This article explores the relationship between the prone position and the physiology of ventilation in both healthy and diseased lungs, and discusses some of the beneficial effects of artificial ventilation in the prone position.
Normal breathing with healthy lungs
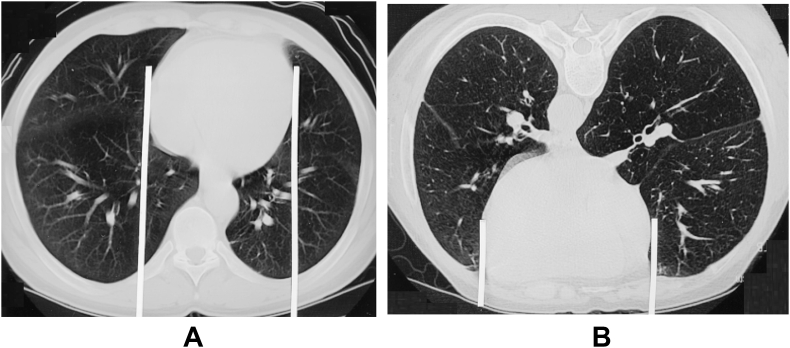
In an awake, spontaneously breathing, non-obese subject, both chest wall and respiratory system mechanics are minimally changed by adopting the prone position. Forced vital capacity and forced expiratory volume in 1 s are similar to those in the supine position. Functional residual capacity (FRC) is increased compared with when supine, but remains less than when upright; this change is presumed to result from altered diaphragm function when prone as a consequence of lower diaphragmatic compliance in the costal/anterior region. An additional explanation is a change in the position of the heart when prone: there is less lung tissue between the pericardium and the anterior chest wall when prone than behind the heart when supine, resulting in the compression of less lung tissue by the heart (Fig. 1).1
Fig 1.
The effect of turning from the supine (A) to prone (B) posture on the heart position within the chest. Note the area of lung behind the heart (between the white lines) is considerably less when prone. Adapted from Albert and Hubmayr1 with permission of the American Thoracic Society. Copyright © 2021 American Thoracic Society. All rights reserved.
The pattern of inspiratory muscle activity is similar to when supine, with two thirds of the tidal volume resulting from intercostal muscle activity, as opposed to upright postures when diaphragmatic action predominates. Maximum voluntary ventilation and peak expiratory flow remain unchanged compared with the supine position.
Ventilation () and perfusion () relationships and gas exchange
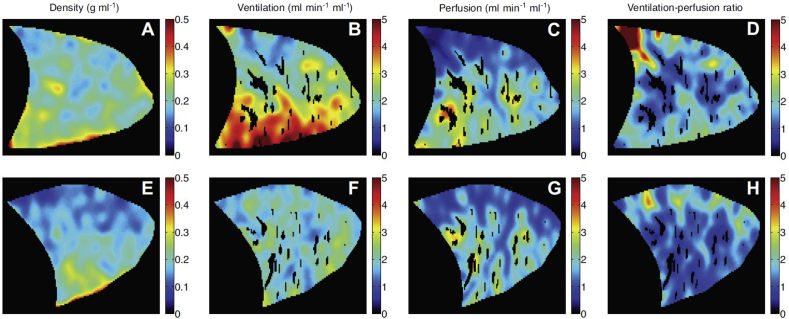
Most land-dwelling vertebrates are quadrupeds and spend life with their lungs in the prone position: the evolution of bipeds who are mostly upright or supine is a recent evolutionary phenomenon for which we were not originally designed. Regional ventilation and perfusion are therefore not perfectly matched, and both are greater in dependent lung regions, with increasing slightly more than such that the / ratio is lower in dependent areas. These changes in regional and result from the effects of gravity on the lungs and from structural variations within lung tissue. Because of this gravitational component a change in posture has an immediate effect on / matching. For example, when moving from the upright to any horizontal posture, when the vertical gradient becomes much smaller, / ratio heterogeneity decreases. When comparing supine and prone positions the changes are more subtle but, predictably, both and remain greater in dependent areas with minimal difference in overall / ratio. However, changes in the distribution of lung density when prone mean that ventilation becomes more uniformly distributed than when supine, whereas regional perfusion heterogeneity remains mostly the same in both positions (Fig. 2).2
Fig 2.
Functional MRI of a healthy subject breathing in supine (A–D) and prone (E–H) positions. See text for details. Republished with permission of the American Physiological Society, from Henderson et al.2; permission conveyed through Copyright Clearance Centre, Inc.
Despite the greater FRC when prone compared with supine, there is a small reduction in diffusing capacity when prone, believed to be caused by altered / relationships secondary to a change in the position of the heart within the chest cavity.
The improved gas exchange consistently seen when prone arises from a combination of increased FRC, less compression of lung tissue behind the heart, and improved / matching because lung density is more uniform.
Artificial ventilation
Mechanical ventilation with healthy lungs
In the supine position the orientation of the ribs causes the ventral chest wall to be more compliant than the dorsal side, which is supported by the spine and bed, and so with IPPV regional ventilation shifts towards non-dependent lung regions. When prone the ventral chest wall is now supported so regional chest wall compliance becomes more even. Overall chest wall compliance is reduced and there is an overall decrease in the pleural pressure gradient between ventral (dependent) and dorsal (non-dependent) lung regions.3 When prone, regional ventilation with IPPV becomes more even than when supine and so better matched to perfusion.
Diaphragm shape is less influenced by position, being more dependent on intra-abdominal pressure secondary to body habitus and, in the prone position, on correct support to lessen the compressive effects of the abdominal organs. In anaesthetised, ventilated subjects turned from supine to prone, regional perfusion also becomes more evenly distributed.4 This observation presumably results from regional variation in local pulmonary vascular resistance as a result of lung inflation and hypoxic pulmonary vasoconstriction.
Mechanical ventilation with injured lungs
Prone IPPV has been established as a treatment for hypoxaemic respiratory failure caused by severe acute lung injury (ALI) for more than 40 yrs. Early trials showed improvement in oxygenation of patients receiving IPPV in the prone position, and the Prone Positioning in Severe Acute Respiratory Distress Syndrome (PROSEVA) trial showed a 16.8% reduction in all-cause mortality at 28 days in patients with early ‘severe’ ALI (severe defined by Pao2:Fio2 < 13.3 kPa).5
In patients with ALI there is a significant increase in lung density in some regions suggesting that the more uniform density of lung when prone will be beneficial. Also, lung collapse in dorsal regions is common in severe ALI, and on turning prone there is dorsal distension and alveolar recruitment, accompanied by some ventral derecruitment, although the former usually prevails.3,6 As a result of these changes to respiratory system mechanics, distending forces in non-dependent alveoli are minimised and it is plausible that the prone position may attenuate volutrauma, atelectrauma and ventilator-induced lung injury.
Regional lung perfusion has not been extensively studied in humans with ALI, but animal models of ALI do suggest that perfusion becomes more uniform than when supine.6 This may be a particular advantage in patients with pneumonia, including COVID-19, when hypoxic pulmonary vasoconstriction is impaired by inflammatory mediators.7
Physiological dead space and CO2 elimination are mostly unchanged when prone such that arterial Pco2 remains unchanged or lower than when supine. In addition to improving oxygenation, better / matching when prone will reduce the areas of / >1 that contribute to alveolar dead space. An increase in arterial Pco2 after proning is associated with poor outcomes, an observation believed to result from the regional alveolar and vascular pathology of advanced ALI, which will be less influenced by the physiological changes of proning.8
Finally, the prone position alters the pattern of secretion movement within the airway, with gravity increasing drainage from dorsal regions towards the central airways. Clearance of secretions in ALI is poor, and prone positioning may reduce the likelihood of developing pneumonia in injured lungs.3
Positive end-expiratory pressure
With healthy lungs, PEEP as part of IPPV in the prone position may be less beneficial than when supine. In anaesthetised humans, PEEP may redistribute perfusion to a greater extent than ventilation, worsening / matching.4 Animal studies have confirmed that PEEP in the prone position had no effect, or even increased, perfusion of non-dependent regions. The same may not be true in injured lungs, when the role of PEEP in recruiting poorly- or non-ventilated lung will override its effects on perfusion. The clinical value of PEEP when prone may therefore be unpredictable, depending on the patient's lung pathophysiology at the time.
Non-invasive respiratory support in a conscious patient in the prone position
Spontaneous breathing
‘Self-proning’ by awake patients with respiratory failure receiving no support other than additional inspired oxygen was widely reported early in the COVID-19 pandemic. The physiology described above suggests this is likely to improve oxygenation, and this was observed in many, but not all patients.9 Whether this, sometimes transient, improvement in oxygenation leads to improved longer-term outcomes remains uncertain; clinical equipoise for this non-invasive and widely practiced intervention is challenging.9
Patient self-inflicted lung injury
Prone positioning in non-intubated patients to delay or avoid tracheal intubation presents multiple challenges. Some patients with respiratory failure have high respiratory drive because of nociceptive feedback from the respiratory system, hypoxic ventilatory drive, and as a psychological response to being acutely ill. This may lead to an intense inspiratory effort, in turn causing excessive transpulmonary and transvascular pressures which are believed to result in further physical lung injury. Severe ALI and COVID pneumonia have both been proposed to result in patient self-inflicted lung injury in some patients.10 In the supine position, large gradients of transpulmonary pressure in the non-dependent regions cause local distension and strain in the lung, predisposing to atelectrauma and negative pressure pulmonary oedema. In theory, this may be attenuated in the prone position by the restrictions on the ventral chest wall preventing excessive pressure gradients in ventral lung regions.
Continuous positive airway pressure
As in the patient whose trachea is intubated, the physiological rationale for CPAP in the prone position is to recruit dorsal lung units and improve / matching by increasing the homogeneity of ventilation throughout the lung. The physiology of CPAP in the prone position has not been studied in either healthy individuals or those with injured lungs. Extrapolation of the preceding sections to the use of CPAP would suggest that an improvement in oxygenation is likely to be seen, as the physiological factors affected by prone positioning will still apply whether the patient is intubated or not.
Published reports of CPAP in the prone position include small numbers of patients with acute respiratory failure secondary to pneumonia or ALI; they consistently show oxygenation and some clinical outcomes to be improved.11 CPAP in the prone position is also an established treatment for refractory hypoxaemia after bilateral lung transplant, with improved oxygenation and resolution of posterior atelectasis on imaging.
Conclusion
Breathing in the prone position, whether naturally or artificially, provides multiple physiological advantages (Table 1). Other than full mechanical ventilation in patients with severe ALI, the clinical benefits of prone breathing remain less clear, and further research is needed on both the mechanisms and its clinical effects. In future, more targeted use of the prone position is likely to become the norm. Patients who may benefit include those with pneumonia, decreased chest wall compliance (e.g. with obesity), and any patient whose pathology causes increased heterogeneity of lung density, particularly when ventilation of dependent regions is poor.
Table 1.
Summary of physiological changes between supine and prone positions in spontaneous breathing and mechanical ventilation. The physiological effects of prone position on ventilation (V̇) and perfusion (Q̇) with IPPV are greater in injured lungs when lung density is increased. Vt, tidal volume
| Spontaneous breathing |
IPPV |
|||
|---|---|---|---|---|
| Supine | Prone | Supine | Prone | |
| FRC | Dependent on body position Minimal when supine, greater when upright. | Midway between upright and supine | Usually reduced, more so if neuromuscular blocking agent used. Dependent on PEEP level | As for supine |
| Respiratory muscles | Supine: two-thirds of Vt from intercostal activity Upright: two-thirds of Vt from diaphragm | As for supine | Muscles inactive | Muscles inactive Chest wall compliance reduced |
| Regional ventilation | Slightly greater in dependent region (supine = dorsal; upright = bases) | More uniform than supine | Predominantly non-dependent (ventral) | Greater in non-dependent (dorsal) Less heterogeneity |
| Regional perfusion | Greater in dependent region (supine = dorsal; upright = bases) | Greater in dependent (ventral) | Predominantly dependent (dorsal) | Greater in dependent (ventral) |
| V̇/Q̇ ratio | Lower in dependent regions | Lower in dependent regions (ventral). Less heterogeneity | High degree of mismatch | Better matching than supine |
Declaration of interests
A.L. is an editorial board member of BJA Education and an associate editor of the British Journal of Anaesthesia. A.W. declares no conflicts of interest.
Biographies
Andy Lumb FRCA is consultant anaesthetist at St James's University Hospital and honorary clinical associate professor at the University of Leeds, UK, specialising in thoracic anaesthesia. His research focuses on respiratory physiology. He teaches at all levels and lectures at postgraduate meetings both in the UK and abroad. He has authored many chapters, reviews, and editorials, and five editions of Nunn's Applied Respiratory Physiology. He is an editorial board member of BJA Education and an associate editor of the British Journal of Anaesthesia.
Alistair White BSc, FRCA, FFICM is a speciality trainee in anaesthesia and intensive care medicine at St James's University Hospital, Leeds.
Matrix codes: 1A01, 2C02, 3C00
References
- 1.Albert R.K., Hubmayr R.D. The prone position eliminates compression of the lungs by the heart. Am J Respir Crit Care Med. 2000;161:1660–1665. doi: 10.1164/ajrccm.161.5.9901037. [DOI] [PubMed] [Google Scholar]
- 2.Henderson A.C., Sá R.C., Theilmann R.J., Buxton R.B., Prisk G.K., Hopkins S.R. The gravitational distribution of ventilation-perfusion ratio is more uniform in prone than supine posture in the normal human lung. J Appl Physiol. 2013;115:313–324. doi: 10.1152/japplphysiol.01531.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gattinoni L., Taccone P., Carlesso E., Marini J. Prone position in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2013;188:1286–1293. doi: 10.1164/rccm.201308-1532CI. [DOI] [PubMed] [Google Scholar]
- 4.Petersson J., Ax M., Frey J., Sánchez-Crespo A., Lindahl S.G., Mure M. Positive end-expiratory pressure redistributes regional blood flow and ventilation differently in supine and prone humans. Anesthesiology. 2010;113:1361–1369. doi: 10.1097/ALN.0b013e3181fcec4f. [DOI] [PubMed] [Google Scholar]
- 5.Guerin C., Reignier J., Richard J.C. Prone positioning in severe acute respiratory distress syndrome (PROSEVA) N Engl J Med. 2013;368:2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 6.Richter T., Bellani G., Harris R.S. Effect of prone position on regional shunt, aeration, and perfusion in experimental acute lung injury. Am J Respir Crit Care Med. 2005;172:480–487. doi: 10.1164/rccm.200501-004OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lang M., Som A., Mendoza D.P. Hypoxaemia related to COVID-19: vascular and perfusion abnormalities on dual-energy CT. Lancet Infect Dis. 2020;20:1365–1366. doi: 10.1016/S1473-3099(20)30367-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gattinoni L., Vagginelli F., Carlesso E. Prone–supine study group. Decrease in PaCO2 with prone position is predictive of improved outcome in acute respiratory distress syndrome. Crit Care Med. 2003;31:2727–2733. doi: 10.1097/01.CCM.0000098032.34052.F9. [DOI] [PubMed] [Google Scholar]
- 9.McNicholas B., Cosgrave D., Giacomini C., Brennan A., Laffey J.G. Prone positioning in COVID-19 acute respiratory failure: just do it? Br J Anaesth. 2020;125:440–443. doi: 10.1016/j.bja.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fan E., Beitler J.R., Brochard L. COVID-19-associated acute respiratory distress syndrome: is a different approach to management warranted? Lancet Respir Med. 2020;8:816–821. doi: 10.1016/S2213-2600(20)30304-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chad T., Sampson C. Prone positioning in conscious patients on medical wards: a review of the evidence and its relevance to patients with COVID-19 infection. Clin Med. 2020;20:97–103. doi: 10.7861/clinmed.2020-0179. [DOI] [PMC free article] [PubMed] [Google Scholar]