Abstract
Primary omental torsion is a rare cause of acute abdomen especially in obese patients with inconsistent history, examination, and laboratory findings. The liberal use of computed tomography in casualties has increased its preoperative diagnosis. Despite the controversy, the non‐operative approach should be attempted as a first line of management while the laparoscopic resection should be only considered after failure of non‐operative management.
Keywords: acute abdomen, non‐operative management, omental torsion
Primary omental torsion is a rare cause of acute abdomen especially in obese patients with inconsistent history, examination, and laboratory findings. The liberal use of computed tomography in casualties has increased its preoperative diagnosis. Despite the controversy, the non‐operative approach should be attempted as a first line of management while the laparoscopic resection should be only considered after failure of non‐operative management.

1. INTRODUCTION
Primary omental torsion represents a rare cause of acute abdomen. Its preoperative diagnosis is challenging owing to its unspecific symptoms and signs. There is no definite consensus for its best management approach. We present a case of primary omental torsion that was successfully managed non‐operatively after a definitive radiological diagnosis.
Differential diagnoses for the acute abdomen are diverse, and primary omental torsion represents one of its rare causes. 1 Traditionally, it was merely intraoperative diagnosis as its preoperative diagnosis was challenging owing to its unspecific symptoms and signs. The preoperative diagnosis has been estimated to be established in less than 5% of all cases. However, the extensive use of different imaging modalities in surgical emergencies has increased the rate of accurate preoperative diagnosis of omental torsion. 2
There is no definite consensus for the best management approach if the omental torsion is preoperatively diagnosed based on imaging studies. 3 Historically, surgical resection has been widely performed as it was usually diagnosed intraoperatively. However, a conservative non‐operative approach can be beneficial in many cases when its diagnosis is confidently established. 3
Herein, we present a young male patient who was preoperatively diagnosed as primary omental torsion based on the characteristic computed tomography (CT) findings and was successfully managed non‐operatively.
2. CASE PRESENTATION
An 18‐year‐old male patient presented to the emergency department, for the second time within 1 week, with recurrent attacks of severe colicky abdominal pain that was associated with nausea, vomiting, and constipation. Initially at the first presentation, the pain was vague, all over the abdomen that was relieved by paracetamol without any imaging modalities. However, the pain started to progressively increase in the 24 h prior to the second presentation and became localized in the right lower quadrant. He had no other relevant symptoms, and his past medical and surgical history was unremarkable.
Upon examination, he looked in pain and had tachycardia of 117 beats/min, low‐grade fever of 37.8°, and a normal blood pressure. He was obese with body mass index of 31.6 Kg/m2 (82 Kg, 1.61 m). His abdomen was tender at the right iliac fossa and supra‐pubic with rebound tenderness at the right iliac fossa and audible normal peristalsis. The rest of the examination was unremarkable. His laboratory investigations were positive for leukocytosis (13.6 × 106/μl) with neutrophilia (79.9%), elevated erythrocyte sedimentation rate (29), and elevated C‐reactive protein (25.39 mg/dl). Other laboratory results including hemoglobin level, renal function, and liver function tests were unremarkable. He underwent multi‐slice CT of the abdomen with intravenous (IV) contrast which showed a right‐sided intraperitoneal concentric‐pattern mass of fat density with whirling appearance, extending from the umbilicus to the right iliac fossa that was suggestive of omental torsion (Figure 1).
FIGURE 1.
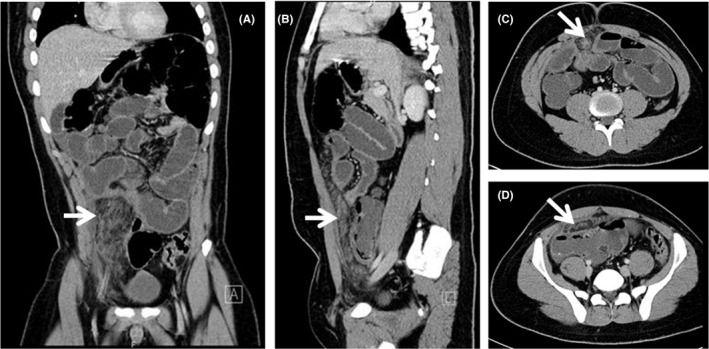
Contrast‐enhanced computed tomography of the abdomen showing (white arrow) a right‐sided intraperitoneal concentric‐pattern mass of fat density with whirling appearance, extending from the umbilicus to the right iliac fossa that was suggestive of omental torsion
Therefore, the patient was admitted for a trial of non‐operative management: Nil per os, IV fluids, analgesia, prophylactic IV antibiotics, and proton pump inhibitors. The antibiotics were ciprofloxacin and metronidazole to cover gram‐negative and anaerobic bacteria. He was closely observed clinically, and, fortunately, his abdominal pain subsided with non‐steroidal anti‐inflammatory drugs. He remained afebrile, with normal vital signs, and his abdominal tenderness gradually improved. Moreover, his leukocytic count, inflammatory markers (CRP, ESR), gradually returned to normal levels. Starting from the third day of admission, he resumed a clear liquid diet which was gradually escalated to a full diet. His condition showed a good improvement on the non‐operative management, and he was discharged home, in a good condition, after 7 days. Upon follow‐up visit after 1, 3, and 6 months, the patient had no symptoms and his clinical examination was unremarkable.
3. DISCUSSION
Omental torsion, first described by Eitel in 1899, is a rare cause of acute abdomen with unknown etiology. 2 , 4 It affects males twice as frequently as females, usually between the fourth and fifth decade of life. It is more common in obese patients. 1 It usually presents with nonspecific symptoms and signs mimicking other abdominal pathologies, especially acute appendicitis. Thus, its diagnosis has been usually made intraoperatively with only 0.6%–4.8% of cases being preoperatively diagnosed. 5 However, its preoperative diagnosis is more commonly established nowadays after the liberal use of computed tomography in the causalities. 3
The omentum is a peritoneal fold hanging between the stomach and the transverse colon. It divides into right and left omentum. The right‐sided omentum is longer, more mobile, and, consequently, more common to be twisted along its blood supply causing omental torsion. Omental fat deposition occurs during childhood and is proportionally related to the overall fat. 1
When the omentum twists around its long axis, it leads to venous obstruction with resultant edema and arterial compromise leading to abdominal manifestations. 5 Omental torsion may lead to omental infarction; however, it is considered a different clinical entity. 6 Omental torsion is classified according to Leitner's classification into primary (idiopathic) and secondary. 7 , 8 , 9 Primary omental torsion occurs without identifiable predisposing abnormalities, while secondary torsion occurred on top of an intra‐abdominal pathology as hernias, omental cysts, tumors, or adhesions. Risk factors for omental torsion include obesity, trauma, anatomical variations, and a sudden increase in intra‐abdominal pressure. 2
Patients with omental torsion usually present with sudden localized abdominal pain aggravated by a sudden movement which may be associated with nausea and vomiting. On examination, there is right‐sided tenderness with rebound tenderness. Temperature, total leukocytic count, and inflammatory markers may be slightly elevated or normal. Otherwise, laboratory findings are nonspecific that may delay the diagnosis and management. Its CT findings include a well‐circumscribed fatty mass with dilated thrombosed veins. 1
Due to its rarity, the treatment of choice remains controversial with no clear consensus or guidelines, especially with absence of prospective comparative studies. 1 , 3 Some authors have recommended surgical management with resection of the twisted omentum. Laparoscopic management is preferred rather than exploration laparotomy as it is associated with better visualization of the abdominal cavity, less postoperative pain, and wound‐related complications. It provides clear precise diagnosis, excludes other differential diagnoses, speeds up the recovery by resecting the affected twisted omentum and eliminating the cause of abdominal pain, and, thus, decreases the hospital stay and costs. 2 However, other experts have suggested the non‐operative management, including analgesia and prophylactic antibiotics, based on the natural history of the disease as a self‐limited benign condition, hence, avoiding the operative complications. 10 They argue that the recent advances and wide availability of multi‐slice CT allow reliable diagnosis, exclusion of other pathologies, and, consequently, substitute the role of diagnostic laparoscopy. 10 , 11 The administration of prophylactic antibiotics is justified to guard against hypothetical possibility of abscess formation. 10 And so, laparoscopic management is only reserved for cases with an unclear diagnosis or cases of failed non‐operative management in form of persistent pain, fever, and elevated inflammatory markers. 1 , 2 , 3 , 10 , 12 , 13 Indeed, it is crucial to mention that the successful non‐operative management depends on the wide use of the CT in casualties, the presence of expert radiologists with reliable exclusion of other diagnoses as well as the sound clinical judgment with a low threshold for prompt diagnostic laparoscopy in non‐responders, cases with doubtful diagnosis, or suspected complications.
A literature review using the search terms ‘omental torsion’, ‘omental infarction’, ‘conservative’, ‘non‐operative’, and ‘adult’ in the title, abstract, and/or keywords of articles indexed in the Medline, Scopus, and Google Scholar databases during the period from 1990 to 2020 revealed 20 articles reporting successful non‐operative management of omental torsion and/or infarction in adult patients. Other articles discussing only pediatric cases were excluded. It is crucial to mention that both terms ‘omental torsion’ and ‘omental infarction’ were interchangeably used in the literature. These cases are summarized in Table 1.
TABLE 1.
Literature review of all adult cases with a diagnosis of omental torsion or omental infarction that were managed non‐operatively
| Year | Author | No of reported cases | Age/gender | Obesity | Presentation | Duration | Temp | SIGNS | WBCs | Inflammatory markers | Initial diagnosis | Imaging modalities | OT/OI | Antibiotics | LoS (days) | Fate | Follow‐up | FU imaging |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1992 | Puylaert 14 , † | 7 |
10–77 5 m–2 f |
NA | Right sided abdominal pain | 1–6 days | NA | NA | 7.6–12 | +++ | Acute appendicitis | US, CT | OT vs OI | ‐ | 8–20 | Improve | 18–44 months | US |
| 1998 | Karak 15 , a | 1 | 50/m | NA | RLQ pain | 18 h | NA | RLQ tenderness | NA | NA | Acute appendicitis, underwent open appendectomy. The appendix was normal | Postop CT | OI | NA | NA | Improve | 6 weeks | CT |
| 1999 | van Breda Vriesman 16 , † | 11 | 6–76 Y | 7 patients | DAP | 0–14 days | NA | Localized tenderness | 5.3 ± 14.8 | + | NA |
US CT |
OI | ‐ | 6–122 | Improve | 24 months | US |
| 2002 | Perelló 17 | 6 | 38/m | NA | DAP | 36 h | NA | NA | NA | NA | NA | CT | OT/OI | NA | 4 days | Improve | 2 months | US/CT |
| 38/m | DAP | 48 h | 4 days | |||||||||||||||
| 34/m | RF and RUQ pain | 72 h | 4 days | |||||||||||||||
| 25/f | RF pain | 72 h | 3 days | |||||||||||||||
| 50/f | DAP | 12 h | 7 days | |||||||||||||||
| 23/m | RF pain | 18 h | 2 days | |||||||||||||||
| 2003 | Xavier 18 | 1 | 30/m | NA | Inguinal hernia | NA | NA | NA | NA | NA | NA | CT | OT | NA | NA | NA | NA | NA |
| 2003 | Paroz 19 | 3 | 59/m | NA | RLQ and RF pain | NA | N | Tenderness | N | +++ | NA | CT | OI | NA | 3–7 days | Improve | NA | NA |
| 34/f | RLQ pain | N | Unremarkable | +++ | OI | |||||||||||||
| 34/m | LUQ pain | ++ | Tenderness | +++ | OI | |||||||||||||
| 2004 | Coulier 20 | 1 | 51/f | NA | Epigastric pain | NA | NA | RT over epigastrium | N | +++ | NA |
US CT |
OI | NA | NA | Improve | 3 weeks | US |
| 2004 | Abadir 21 , b , † | 8 | 11–58 | 7 patients |
RUQ pain 20% LLQ pain 47% RLQ pain 33% |
3–96 h | N 93% | Peritonitis 40% | +++ 33% | NA | NA | CT | OI | +++ 60% | 1–8 days | Improve | NA | NA |
| 2004 | Bachar 22 | 5 | 31/f | NA | RLQ pain | 5 days | N | NA | N | NA | Acute appendicitis |
US CT |
OI | ‐ | 1–6 days | Improve | 3–24 months | NA |
| 75/m | DAP | 2 days | N | |||||||||||||||
| 79/f | RLQ pain | 2 days | N | |||||||||||||||
| 27/f | RLQ pain | 2 days | +++ | |||||||||||||||
| 31/f | RLQ pain | 1 day | +++ | |||||||||||||||
| 2006 | Goh 23 | 1 | 39/m | NA | RUQ pain | 48 h | 38.2 | Tenderness at RUQ, + murphy sign | +++ | NA | Acute cholecystitis | CT | OI | + | 3 days | Improve | 1 month | NA |
| 2007 | Rao 24 | 1 | 29/m | + | RUQ pain | 48 h | N | Tenderness over RUQ | N | NA | NA | CT | OI | ‐ | 1 day | Improve | NA | NA |
| 2010 | Fernández‐Rey 25 | 1 | 43/m | + | RF pain | 48 h | N | Peritoneal irritation at RF | N | NA | Acute diverticulitis |
US CT |
OI | NA | NA | Improve | NA | Resolution of images |
| 2010 | Soobrah 1 | 1 | 20/f | NA | RUQ pain | 1 week | N | Tnederness over RUQ | +++ | +++ | NA | CT | OI | ‐ | 3 days | Improve | NA | NA |
| 2010 | Tandon 26 | 1 | 41/m | NA | RLQ pain | 120 h | 37.9 | Unremarkable | +++ | NA | Acute appendicitis | CT | OT | + | NA | Improve | NA | NA |
| 2011 | Modaghegh 27 | 1 | 74/f | NA | DAP | 96 h | N | RT at RUQ, ill defined fullness | N | NA | NA |
US CT |
OT | + | 9 days | Improve | 6 months | no |
| 2012 | Park 28 | 3 | 56/m | NA | RLQ pain | 72 h | N | Tenderness RLQ | N | Elevated | NA | CT | OI | NA | 5 days | Improve | NA | NA |
| 52/m | Epigastric pain | 48 h | N | Tenderness epigastrium and RUQ | N | Elevated | ‐ | 1 day | 3 days | |||||||||
| 52/m | LF pain | 24 h | N | RT at LF, LLQ | N | +++ | NA | 7 days | NA | |||||||||
| 2012 | Filho 29 | 1 | 36/f | ‐ | DAP and constipation | 5 days | N | Generalized peritonitis | +++ | NA | NA | CT | OI | ‐ | NA | Recurred pain after few days and conservative management continued. He eventually improved. | 1 week | CT |
| 2015 | Rebeca Amo‐Alonso 30 | 1 | 65/f | NA | RUQ pain | NA | 38°C | Painful mass,10 cm, RUQ | +++ | +++ | Ascending colon tumor | CT | OT/OI | NA | 7 days | Improve | 3 months | CT after 15 days |
| 2018 | Udechukwu 31 | 1 | 61/m | + | RUQ pain | 96 h | N | Tenderness over RUQ | N | N | NA | CT | OI | ‐ | NA | Improve | 3 weeks | CT |
| 2019 | Kataoka 2 | 1 | 50/m | ‐ | RLQ pain | 12 h | NA | Unremarkable | N | +++ | NA | CT | OT | + | 5 days preop 9 days postop | Improved symptoms | NA | NA |
Abbreviations: +++, elevated; CT, abdominal computed tomography; DAP, diffuse abdominal pain; LF, left flank; LLQ, left lower quadrant; LUQ, left upper quadrant; N, normal; NA, not available; OI, omental infarction; OT, omental torsion; RF, right flank; RLQ, right lower quadrant; RT, rebound tenderness; RUQ, right upper quadrant; US, ultrasonography of the abdomen.
This reported case was diagnosed as acute appendicitis and underwent open appendectomy. However, the appendix was normal macroscopically and microscopically. Postoperative CT confirmed diagnosis of OI.
This case series included 15 patients (eight OI and seven epiploic appendagitis), but the authors included a table for clinical data of all patients without differentiation between the two pathologies.
In this case, all symptoms were improved. However, laparoscopic omentectomy was performed due to persistent elevated inflammatory markers and worsening of the CT findings.
All articles discussing pediatric cases were excluded. However, these three cases series included pediatric patients and were difficult to exclude these cases in particular.
In our case, the patient presented for the second time within 1 week with on‐and‐off right lower quadrant moderate abdominal pain. He was tachycardic with low‐grade fever, and his abdominal examination was suggestive of acute appendicitis. His laboratory findings showed slightly elevated leukocytosis and inflammatory markers. Our differential diagnosis at that point was acute appendicitis; however, the long duration (4 days) of symptoms was not in line with his examination and laboratory findings. His CT scan confirmed the presence of omental torsion and excluded acute appendicitis and other pathologies. Therefore, we opted to start with a trial of a non‐operative approach with a low threshold to perform laparoscopic resection. We elected to administer wide‐spectrum antibiotics (ciprofloxacin and metronidazole) to cover possible pathogens that may cause abscess. The close follow‐up, by serial examination and laboratory works, was crucial to early pick up any signs of sepsis. Fortunately, he responded well and promptly to the non‐operative management and was discharged within 1 week.
4. CONCLUSION
Primary omental torsion is rare and should be considered in the differential diagnoses of acute abdomen in obese patients with inconsistent history, examination, and laboratory findings. High index of suspicion is important for preoperative diagnosis. The liberal use of CT represents a cornerstone for its preoperative diagnosis. Despite the controversy, the non‐operative approach, which depends on accurate radiological diagnosis, analgesia, prophylactic antibiotics, and close follow‐up, is a valid judicious modality of management and should be attempted as a first line of management even in young healthy patients. Laparoscopic resection should be only considered after failure of non‐operative management.
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTIONS
MF involved in conceptualization and writing. MS and ZA involved in writing—original draft. OA and BA collected the data. HK involved in supervision, conceptualization, and writing—review and editing.
ETHICAL APPROVAL
Case reports are exempted from ethical approval.
ACKNOWLEDGMENT
A written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editor‐in‐chief of this journal on request.
Foula MS, Sharroufna M, Alshammasi ZH, Alothman OS, Almusailh BA, Hassan KA. Non‐operative management of primary omental torsion, a case report and literature review. Clin Case Rep. 2021;9:e04474. 10.1002/ccr3.4474
DATA AVAILABILITY STATEMENT
Further details of the presented case is available from the corresponding upon reasonable request.
REFERENCES
- 1. Soobrah R, Badran M, Smith SG. Conservative management of segmental infarction of the greater omentum: a case report and review of literature. Case Rep Med. 2010;2010:1‐4. 10.1155/2010/765389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kataoka J, Nitta T, Ota M, et al. Laparoscopic omentectomy in primary torsion of the greater omentum: report of a case. Surg Case Rep. 2019;5(1). 10.1186/s40792-019-0618-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Itenberg E, Mariadason J, Khersonsky J, Wallack M. Modern management of omental torsion and omental infarction: a surgeon's perspective. J Surg Educ. 2010;67(1):44‐47. 10.1016/j.jsurg.2010.01.003 [DOI] [PubMed] [Google Scholar]
- 4. Eitel GG. A rare omental tumor. NY Med Rec. 1899;55(20):715‐716. [Google Scholar]
- 5. Dhooghe V, Reynders D, Cools P. Torsion of a bifid omentum as a rare cause of acute abdomen: a case report. J Med Case Rep. 2016;10(1). 10.1186/s13256-016-1070-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tuncer AA, Tuncer N, Cetinkursun S. A rare cause of acute abdomen in children: omental infarction due to segmental omental torsion. J Acad Res Med. 2017;7(3):161‐162. 10.5152/jarem.2017.1275 [DOI] [Google Scholar]
- 7. Leitner MJ, Jordan CG, Spinner MH, Reese EC. Torsion, infarction and hemorrhage of the omentum as a cause of acute abdominal distress. Ann Surg. 1952;135(1):103‐110. 10.1097/00000658-195201000-00014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Coppin T, Lipsky D. Twisting and infarction of the entire greater omentum managed by laparoscopy: a report of two cases. Acta Chir Belg. 2006;106(2):215‐217. 10.1080/00015458.2006.11679874 [DOI] [PubMed] [Google Scholar]
- 9. Anton JI, Jennings JE, Spiegel MB. Primmary omental torsion. Am J Surg. 1945;68(3):303‐317. 10.1016/0002-9610(45)90229-7 [DOI] [Google Scholar]
- 10. Fragoso AC, Pereira JM, Estevão‐Costa J. Nonoperative management of omental infarction: a case report in a child. J Pediatr Surg. 2006;41(10):1777‐1779. 10.1016/j.jpedsurg.2006.05.038 [DOI] [PubMed] [Google Scholar]
- 11. Van Kerkhove F, Coenegrachts K, Steyaert L, Ghekiere J, Gabriel C, Casselman JW. Omental infarction in childhood. JBR‐BTR. 2006;89(4):198‐200. [PubMed] [Google Scholar]
- 12. Estevão‐Costa J, Alvarenga AS, Fragoso AC, Garcia M, Campos M. Omental infarction: a reappraisal of conservative management in children. Acta Méd Port. 2014;27(4):433. 10.20344/amp.4996 [DOI] [PubMed] [Google Scholar]
- 13. Cianci R, Filippone A, Basilico R, Storto ML. Idiopathic segmental infarction of the greater omentum diagnosed by unenhanced multidetector‐row CT and treated successfully by laparoscopy. Emerg Radiol. 2007;15(1):51‐56. 10.1007/s10140-007-0631-z [DOI] [PubMed] [Google Scholar]
- 14. Puylaert JB. Right‐sided segmental infarction of the omentum: clinical, US, and CT findings. Radiology. 1992;185(1):169‐172. 10.1148/radiology.185.1.1523302 [DOI] [PubMed] [Google Scholar]
- 15. Karak PK, Millmond SH, Neumann D, Yamase HT, Ramsby G. Omental infarction: report of three cases and review of the literature. Abdom Imaging. 1998;23(1):96‐98. 10.1007/s002619900294 [DOI] [PubMed] [Google Scholar]
- 16. Vriesman ACVB, Puylaert JBCM. Epiploic appendagitis and omental infarction: pitfalls and look‐alikes. Abdom Imaging. 2002;27(1):20‐28. 10.1007/s00261-001-0056-1 [DOI] [PubMed] [Google Scholar]
- 17. Perelló JM, Aguayo Albasini JL, Soria Aledo V, et al. Omental torsion: imaging techniques can prevent unnecessary surgical interventions. Gastroenterol Hepatol. 2002;25(8):493‐496. [PubMed] [Google Scholar]
- 18. Xavier S, John P. Torsion of the greater omentum with inguinal hernia. Indian J Gastroenterol. 2003;22(5):194‐196. [PubMed] [Google Scholar]
- 19. Paroz A. Idiopathic segmental infarction of the greater omentum: a rare cause of acute abdomen. J Gastrointest Surg. 2003;7(6):805‐808. 10.1016/s1091-255x(03)00139-2 [DOI] [PubMed] [Google Scholar]
- 20. Coulier B, Van Hoof M. Intraperitoneal fat focal infarction of the lesser omentum: case report. Abdom Imaging. 2004;29(4). 10.1007/s00261-003-0140-9 [DOI] [PubMed] [Google Scholar]
- 21. Abadir JS, Cohen AJ, Wilson SE. Accurate diagnosis of infarction of omentum and appendices epiploicae by computed tomography. Am Surg. 2004;70(10):854‐857. [PubMed] [Google Scholar]
- 22. Bachar GN, Shafir G, Postnikov V, Belenky A, Benjaminov O. Sonographic diagnosis of right segmental omental infarction. J Clin Ultrasound. 2005;33(2):76‐79. 10.1002/jcu.20091 [DOI] [PubMed] [Google Scholar]
- 23. Goh BKP, Koong H‐N. Non‐operative management of idiopathic segmental infarction of the greater omentum successfully diagnosed by computed tomography. J Gastroenterol Hepatol. 2006;21(10):1638‐1639. 10.1111/j.1440-1746.2006.04348.x [DOI] [PubMed] [Google Scholar]
- 24. Rao A, Remer EM, Phelan M, Hatem SF. Segmental omental infarction. Emerg Radiol. 2007;14(3):195‐197. 10.1007/s10140-007-0616-y [DOI] [PubMed] [Google Scholar]
- 25. Fernández‐Rey CL. Primary omental infarction as cause of non‐surgical acute abdomen: imaging diagnose. Rev Esp Enfermedades Dig. 2010;102(8). 10.4321/s1130-01082010000800007 [DOI] [PubMed] [Google Scholar]
- 26. Tandon AA, Lim KS. Torsion of the greater omentum: a rare preoperative diagnosis. Indian J Radiol Imaging. 2010;20(4):294. 10.4103/0971-3026.73540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Modaghegh M‐HS, Jafarzadeh R. Primary omental torsion in an old woman: imaging techniques can prevent unnecessary surgical interventions. Case Rep Med. 2011;2011:1‐3. 10.1155/2011/541324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Park TU, Oh JH, Chang IT, et al. Omental infarction: case series and review of the literature. J Emerg Med. 2012;42(2):149‐154. 10.1016/j.jemermed.2008.07.023 [DOI] [PubMed] [Google Scholar]
- 29. Araújo Filho JAB, Martines JAS, Martines BMR, Lourenção RM, Pinto LEA, Castro CC. Segmental omental infarction: an unusual cause of acute abdomen. Autops Case Rep. 2012;2(2):43‐47. 10.4322/acr.2012.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Amo Alonso R, Arenal Vera JJ, de la Peña Cadenato J, Loza Vargas A, Santos Santamarta F, Sánchez‐Ocaña Hernández R. Infarction of the greater omentum. Case report. Rev Española Enfermedades Dig. 2015;107. 10.17235/reed.2015.3754/2015 [DOI] [PubMed] [Google Scholar]
- 31. Udechukwu NS, D'Souza RS, Abdulkareem A, Shogbesan O. Computed tomography diagnosis of omental infarction presenting as an acute abdomen. Radiol Case Rep. 2018;13(3):583‐585. 10.1016/j.radcr.2018.02.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Further details of the presented case is available from the corresponding upon reasonable request.


