Abstract
Background:
Helminth infections can modulate immunity to Mycobacterium tuberculosis (Mtb). However, the effect of helminths, including Schistosoma mansoni (SM), on Mtb infection outcomes is less clear. Furthermore, HIV is a known risk factor for tuberculosis (TB) disease and has been implicated in SM pathogenesis. Therefore, it is important to evaluate whether HIV modifies the association between SM and Mtb infection.
Setting:
HIV-infected and HIV-uninfected adults were enrolled in Kisumu County, Kenya between 2014 and 2017 and categorized into three groups based on Mtb infection status: Mtb-uninfected healthy controls (HC), latent TB infection (LTBI), and active TB disease. Participants were subsequently evaluated for infection with SM.
Methods:
We used targeted minimum loss estimation and super learning to estimate a covariate-adjusted association between SM and Mtb infection outcomes, defined as the probability of being HC, LTBI or TB. HIV status was evaluated as an effect modifier of this association.
Results:
SM was not associated with differences in baseline demographic or clinical features of participants in this study, nor with additional parasitic infections. Covariate-adjusted analyses indicated that infection with SM was associated with a 4% higher estimated proportion of active TB cases in HIV-uninfected individuals and a 14% higher estimated proportion of active TB cases in HIV-infected individuals. There were no differences in estimated proportions of LTBI cases.
Conclusions:
We provide evidence that SM infection is associated with a higher probability of active TB disease, particularly in HIV-infected individuals.
Keywords: HIV, tuberculosis, schistosomiasis, machine learning, causal inference, Kenya
Introduction
Mycobacterium tuberculosis (Mtb) is a serious public health concern, infecting a quarter of the world, leading to ten million cases of tuberculosis (TB) disease and over one million deaths annually.1 Mtb infection results in a spectrum of clinical states ranging from clearance, to latent infection (LTBI), to subclinical and active TB disease.2 The mechanisms that underlie these disparate outcomes are not well understood; however, co-infections, such as with human immunodeficiency virus (HIV), and co-morbidities, such as diabetes, are known risk factors.1 Helminths are co-endemic with Mtb and known to be immunomodulatory.3,4 As such, determining the impact of helminths on Mtb infection outcomes is important and may identify potential risk factors for the development of TB disease.
While the negative impact of helminths on immunity to Mtb infection, by either suppressing or skewing type 1 immunity, is well documented,5 the consequence of helminth infection on the development of TB disease is less clear. Some studies have reported higher prevalence of intestinal helminth infections in individuals with active TB as compared with healthy controls.6–9 Others, however, have found no significant differences in the prevalence of helminth infections between individuals with TB and healthy controls.10 In addition, two longitudinal studies found no increase in TB incidence among individuals infected with intestinal helminths in either HIV-uninfected,11 or HIV-infected individuals.12 This variation is particularly evident in a recent meta-analysis of epidemiological studies of individuals co-infected with Mtb and intestinal helminths, which found that prevalence of co-infection as well as measured associations between helminth and Mtb infections varies greatly between studies, as well as between helminth species.13 These findings may indicate that associations for a single helminth species are not broadly applicable to all helminth species. Moreover, it is not clear that these results apply when considering helminths that do not reside in the intestine, such Schistosoma mansoni (SM).14
Infection with SM or other schistosome worms leads to the clinical disease schistosomiasis, which affects 240 million people globally.14 In Sub-Saharan Africa, approximately one quarter of the population is estimated to be infected with SM.15 Schistosome infections are estimated to cause 280,000 deaths in Sub-Saharan Africa per year.16 Despite this high disease burden, few studies have measured the association between SM and TB disease. Some evidence suggests that SM-infected individuals are at higher risk of developing TB disease and that SM infection may impact the clinical manifestations of TB disease.9,12 However, others have reported decreased odds of TB disease in SM-infected individuals.6 Importantly, there has not been a comprehensive analysis of SM infection on Mtb infection outcomes that includes both LTBI and active TB.
There are also limited data on the impact of SM and HIV co-infection on Mtb infection outcomes. This is of particular interest, not only because HIV is the greatest risk factor for TB disease,17 but also due to the bi-directional effects of SM and HIV. Schistosomiasis is suspected to play a role not only in susceptibility to HIV, but also in higher viral load set point and worse HIV disease progression.18 HIV in turn has been shown to reduce egg shedding from SM adult worms, which makes detecting infection more difficult and can result in increased pathogenesis due to higher internal egg burden.19 Thus, the combination of these three infections could have distinct clinical outcomes and treatment implications.
The inability to perform randomized controlled trials of SM infection makes it challenging to definitively evaluate the impact of SM on Mtb infection outcomes. Nevertheless, we used data from an observational cohort coupled with modern causal inference and machine learning methodology to estimate a covariate-adjusted association between SM infection and Mtb infection outcomes. This allowed us to estimate the distribution of Mtb infection outcomes in an observed population under counterfactual conditions, that is if all individuals in the observed population were infected with SM compared to if no individuals were infected with SM. We further evaluated whether HIV infection modified this association. Our analysis suggests that SM infection is associated with a higher probability of active TB but not LTBI, and that this is exacerbated by HIV.
Methods
Study Population:
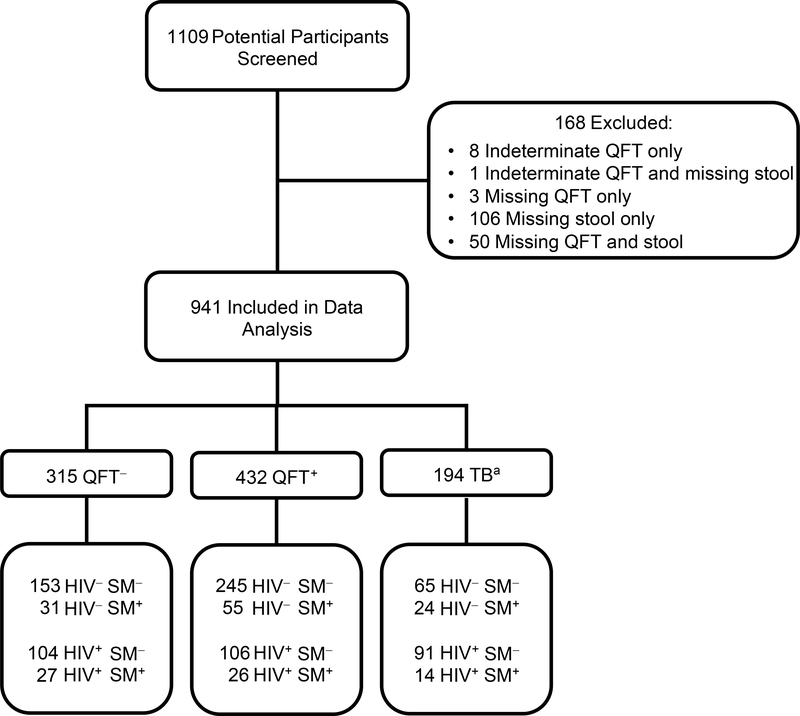
This study was part of a larger case-control study analyzing cellular immune responses to Mtb. Individuals ≥18 years of age residing in Kisumu County in western Kenya were recruited from two community based health clinics located in Kisumu City and in Kombewa.20 Participants were screened and enrolled between 2014 and 2017 based on Mtb infection status and then evaluated for HIV and SM infection. Participants were excluded only if they were missing data in either the outcome or exposure variables. Of 1109 participants screened for this study, 941 had complete Mtb, HIV, and SM study records and were therefore included in the analysis (Figure 1).
Figure 1: Study Participant Flow Diagram.
Abbreviations: Mtb, Mycobacterium tuberculosis; SM, Schistosoma mansoni; QFT, QuantiFERON-TB Gold.
a 20 TB participants had missing or negative Mtb culture results
Laboratory Results:
Mtb infection status was defined as active TB disease (TB), latent TB infection (LTBI), or Mtb-uninfected Healthy Control (HC) based on the following criteria. TB participants were identified as referrals from satellite public health clinics in Kisumu County who had an initial positive sputum smear or GeneXpert MTB/RIF result. Upon enrollment in the study, another sputum sample was collected and evaluated for Mtb by fluorescence microscopy, GeneXpert MTB/RIF, HAIN MTBDR, and MGIT culture. Individuals with active TB were evaluated within the first seven days of initiating the standard six-month course of TB treatment, which was provided according to Kenyan national health guidelines. Healthy asymptomatic individuals with no previous history of TB disease or treatment were identified as community contacts from index TB cases. They were evaluated by QuantiFERON-TB Gold (QFT) assay using the cutoffs and designations specified by the manufacturer (Qiagen) and as previously described.21 LTBI were defined as those with a positive QFT result (TB Ag-Nil ≥0.35 IU IFNγ/mL). HC were defined as those with a negative QFT result (TB Ag-Nil <0.35 IU IFNγ/mL). Chest x-rays were performed on individuals in the LTBI and HC groups.
Helminth infection was determined using standard Kato Katz microscopy. Two thick Kato Katz smears were prepared from stool samples collected on two separate days. Slides were analyzed by experienced lab technicians who recorded the presence of eggs belonging to SM, hookworm, Ascaris lumbricoides, and Trichuris trichuria. SM-infected individuals were defined as having at least one egg present in at least one slide examined. The number of SM eggs were counted and recorded as eggs per gram (epg) for SM-infected individuals. All helminth-infected individuals were referred for treatment, according to Kenya Ministry of Health guidelines.
Serologic testing for HIV antibodies was done for all individuals using the rapid Diagnostic Kit for HIV (1+2) Antibody V2 (KHB® Shanghai Kehua Bio-engineering Co., Ltd). Plasma HIV viral load and CD4 T cell counts were measured for HIV-infected individuals. All HIV-infected individuals were referred for antiretroviral therapy (ART) according to Kenya Ministry of Health guidelines.
Women of childbearing age were tested for pregnancy using test strips for detection of hCG in urine. Individuals were tested for malaria using a malaria rapid diagnostic test (SD BIOLINE Malaria Ag P.f/Pan test from Abbott) and referred for treatment when positive.
Ethics Statement:
This study was conducted in accordance with the principles expressed in the Declaration of Helsinki. All participants provided written informed consent for the study, which was approved by the KEMRI Scientific and Ethics Review Unit, in addition to the institutional review boards at Emory University and U.S. Centers for Disease Control and Prevention.
Statistical Analysis:
Participants’ demographic and clinical characteristics were summarized using descriptive statistics based on SM and Mtb infection status. Groups of individuals were compared based on their SM infection status using a Kruskal-Wallis test to evaluate differences for continuous measures, with pairwise comparisons adjusting for multiple testing using the Benjamini & Hochberg method in the case of three or more groups. Comparisons of categorical data were made using either a χ2 or Fisher’s exact test.
Our primary analysis examined differences in Mtb infection outcomes across the entire study population, and separately amongst HIV-infected and HIV-uninfected individuals. To control for potential confounders of SM and Mtb outcomes, we adjudicated a pre-specified list of potential confounders (Table 1). We used these data to estimate the covariate-adjusted probability of outcomes under each SM infection state using targeted minimum loss estimation (TMLE). TMLE is a doubly-robust method that requires estimates of the probability of SM infection as a function of covariates (a propensity score) and the probability of Mtb infection outcome as a function of SM infection status and covariates.22 These estimates were both obtained using super learning. Super learning entails pre-specifying multiple candidate regression models and uses cross-validation to build a combination of the various models that provides the best estimated fit to the observed data.23 Pre-specified regressions and covariates are indicated in Supplementary Figure 1. Wald tests with a significance level of 0.05 were used to test the null hypothesis of no difference in proportion of Mtb outcomes between SM groups. Standard error estimates were obtained using estimated influence functions and the delta method.
Table 1:
Characteristics of Study Population
| SM− n=764 |
SM+ n=177 |
|
|---|---|---|
| Age: median (IQR)a | 30 (23 – 40) | 30 (23 – 36) |
| Sex: n (%)a | ||
| Female | 472 (61.8%) | 95 (53.7%) |
| Male | 292 (38.2%) | 82 (46.3%) |
| Race: n (%) | ||
| Black African | 764 (100%) | 177 (100%) |
| Recruitment Site: n (%)a | ||
| Kisumu City (urban) | 426 (59%) | 103 (60%) |
| Kombewa (rural) | 296 (41%) | 68 (40%) |
| Hemoglobin g/dL: median (IQR)a | 12.7 (11.4 – 13.9) | 13·0 (11.7 – 14.1) |
| Pregnant: n (%)a | 1 (0.23%) | 0 (0%) |
| Malaria: n (%)a | 2 (0.37%) | 0 (0%) |
| Any Helminth (not including SM): n (%)a | 77 (10.1%) | 19 (10.7%) |
| Ascarisa | 13 (1.7%) | 1 (0.6%) |
| Trichurisa | 16 (2.1%) | 5 (2.8%) |
| Hookworma | 52 (6.8%) | 14 (7.9%) |
| Helminth Species (not including SM): n (%)a | ||
| 0 | 687 (89.9%) | 158 (89.3%) |
| 1 | 73 (9.6%) | 18 (10.2%) |
| 2 | 4 (0.52%) | 1 (0.56%) |
| SM Features | ||
| epg: median (IQR) | NA | 48 (24 – 144) |
| Light Intensity (1–99 epg): n (%) | NA | 122 (68.9%) |
| Moderate Intensity (100–399 epg): n (%) | NA | 41 (23.2%) |
| Heavy Intensity (400+ epg): n (%) | NA | 14 (7.9%) |
| HIV Features | ||
| Positive: n (%)a | 301 (39.4%) | 67 (37.9%) |
| Among Positive | ||
| Viral Load: median (IQR)a | 30058 (1775 – 150 826) | 18879 (2442 – 101 875) |
| Suppressed Viral Load: n (%) | 25 (8.3%) | 5 (7.5%) |
| CD4 Count (cells/μL): median (IQR) | 395 (184 – 600) | 467 (299 – 646) |
| On ART: n (%) | ||
| Yes | 50 (16.6%) | 6 (9.0%) |
| No | 203 (67.5%) | 55 (82.0%) |
| Unknown | 48 (15.9%) | 6 (9.0%) |
| Tuberculosis Features | ||
| QFT IFNγIU/mL (TB Antigen-Nil): median (IQR) | ||
| HC | 0.00 (0.00 – 0.05) | 0.00 (0.00 – 0.04) |
| LTBI | 7.00 (2.12 – 9.57) | 7.07 (1.76 – 9.53) |
| Abnormal Chest x-ray: n (%) | ||
| HC | 3 (1.3%) | 0 (0%) |
| LTBI | 8 (2.5%) | 2 (2.7%) |
: Included in propensity score and outcome regression models.
Abbreviations: IQR, Interquartile Range; epg, Eggs Per Gram; QFT, QuantiFERON-TB Gold.
Our secondary analysis evaluated whether HIV modified the effect of SM infection on Mtb infection outcomes. We tested the null hypothesis that the difference in the probability of each Mtb infection outcome between SM-uninfected and SM-infected groups was equivalent between HIV-uninfected and HIV-infected groups. We then performed a sensitivity analysis to evaluate the impact of adjusting for CD4 T cell counts, measured among HIV-infected individuals. We also performed a sensitivity analysis including study participants with indeterminate QFT results. All primary and secondary statistical analyses were carried out with R software, using the SuperLearner and drtmle packages.23,24
Results
Of the 941 individuals included in the analysis, 177 (18.81%) tested positive for SM (Table 1). The median egg burden for SM-infected individuals was 48 epg, with 122 individuals categorized as having a light intensity infection (1–99 epg), 41 a moderate intensity infection (100–399 epg), and 14 a heavy intensity infection (>399 epg) according to WHO standards.14
Participants in each SM group were similar with regard to demographic and clinical parameters (Table 1). Few participants had additional parasitic infections, the majority of which were hookworm infections. Furthermore, the frequency of both malaria and additional helminth infections was equivalent between SM-uninfected and SM-infected groups. The proportion of HIV-infected individuals in each group was equivalent and had similar clinical features with regard to viral load and CD4 count between SM-uninfected and SM-infected individuals. There were no differences in median quantitative QFT response or the percentage of abnormal chest x-rays between SM-uninfected and SM-infected individuals.
Participants in Mtb infection groups were different with regard to both clinical and demographic measures (Table 2). HC individuals were younger than individuals in both the LTBI and TB group. There were more males and more individuals from Kisumu City in the TB group compared to the LTBI and HC group. In addition, TB participants had lower hemoglobin levels compared to LTBI and HC individuals. The LTBI group had the lowest frequency of HIV-infected individuals. This group also had the lowest median viral load and the highest median CD4 T cell counts. Importantly, very few HIV-infected HC and LTBI individuals were receiving ART treatment compared to 35.2% of TB individuals who were receiving ART at the time of screening. The prevalence of additional helminth infections was higher in the LTBI and HC than in the TB groups.
Table 2:
Study Characteristics by Mtb Infection Status
| HC n=315 |
LTBI n=432 |
TB n=194 |
P-value | |
|---|---|---|---|---|
| Age (years): median (IQR)a | 25.0 (20.0 – 34.0) | 31.0 (24.0 – 41.2) | 33.0 (26.2 – 40.0) | <0.001b |
| Sex: n (%)a | <0.001c | |||
| Female | 212 (67.3%) | 276 (63.9%) | 79 (40.7%) | |
| Male | 103 (32.7%) | 156 (36.1%) | 115 (59.3%) | |
| Race: n (%) | 1c | |||
| Black African | 315 (100%) | 432 (100%) | 194 (100%) | |
| Recruitment Site: n (%)a | <0.001c | |||
| Kisumu City (urban) | 150 (50%) | 250 (59.2%) | 129 (75.4%) | |
| Kombewa (rural) | 150 (50%) | 172 (40.8%) | 42 (24.6%) | |
| Clinical Information | ||||
| Hemoglobin (g/dL): median (IQR)a | 12.9 (11.8 – 13.9) | 13.2 (11.9 – 14.2) | 11.2 (9.80 – 12.3) | <0.001b |
| Pregnant: n (%)a | 0 (0%) | 1 (0.38%) | 0 (0%) | 1d |
| Malaria: n (%)a | 1 (0.47%) | 1 (0.38%) | 0 (0%) | 1d |
| Any Helminth (not including SM): n (%)a | 39 (12.4%) | 46 (10.6%) | 11 (5.67%) | 0.048c |
| Ascarisa | 2 (0.63%) | 11 (2.55%) | 1 (0.52%) | 0.060d |
| Trichurisa | 11 (3.49%) | 5 (1.16%) | 5 (2.58%) | 0.087d |
| Hookworma | 28 (8.89%) | 33 (7.64%) | 5 (2.58%) | 0.020d |
| Number of Helminth Species (not including SM): n (%)a | 0.131d | |||
| 0 | 276 (87.6%) | 386 (89.4%) | 183 (94.3%) | |
| 1 | 37 (11.7%) | 43 (9.95%) | 11 (5.67%) | |
| 2 | 2 (0.63%) | 3 (0.69%) | 0 (0%) | |
| HIV Clinical Features | ||||
| Positive: n (%)a | 131 (41.6%) | 132 (30.6%) | 105 (54.1%) | <0.001c |
| Among Positive | ||||
| Viral Load (copies/mL): median (IQR) a | 52004 (6100 – 145968) | 14856 (1810 – 54166) | 41728 (355 – 376951) | 0.022b |
| Suppressed Viral Load: n (%)e | 6 (4.6%) | 8 (6.1%) | 16 (15.2%) | 0.007d |
| CD4 Count (cells/μL): median (IQR) | 466 (292 – 646) | 518 (356 – 720) | 172(78 – 386) | <0.001b |
| On ART: n(%) | <0.001d | |||
| Yes | 6 (4.6%) | 10 (7.6%) | 40 (38.1%) | |
| No | 105 (80.2%) | 104 (78.8%) | 49 (46.7%) | |
| Unknown | 20 (15.3%) | 18 (13.6%) | 16 (15.2%) | |
| Tuberculosis Clinical Features | ||||
| QFT IFNγ IU/mL: median (IQR) | 0.00 (0.00 – 0.04) | 7.07 (2.09–9.57) | ND | <0.001b |
| Abnormal Chest x-ray: n (%) | 3 (1.05%) | 10 (2.5%) | ND | <0.001d |
: Included in propensity score and outcome regression models
: Kruskall-Wallis
: χ2 test
: Fisher’s exact test
: <20 copies HIV-1 RNA/ml plasma
Abbreviations IQR: Interquartile Range QFT: QuantiFERON Gold ND: Note Done
To estimate a covariate-adjusted association between SM and Mtb infection outcomes, we utilized machine learning to build regressions for both the propensity score and the outcome regression. These models were built using the combined HIV-uninfected and HIV-infected data sets and pre-specified regressions and covariates with the SuperLearner package in R (Supplementary Figure 1). We then used TMLE to evaluate the impact of SM infection on Mtb infection outcomes in HIV-uninfected and HIV-infected individuals. This allowed us to estimate and compare the distribution of Mtb infection outcomes – defined as the probability of being Mtb-uninfected (HC), LTBI, or TB – under the counterfactual conditions of all participants being SM-infected or all participants being SM-uninfected.
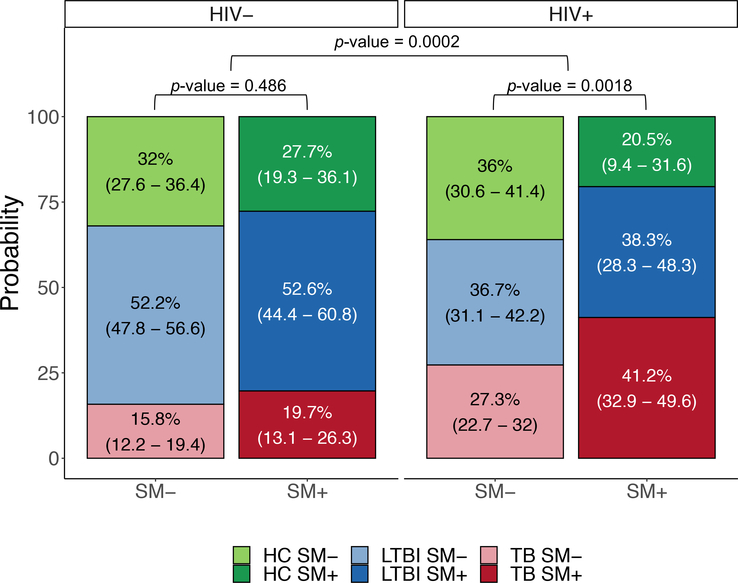
We found that the estimated distribution of Mtb infection outcomes beween SM-infected and SM-uninfected groups was different in HIV-infected individuals compared to HIV-uninfected individuals (p=0.0002, Figure 2). The covariate-adjusted estimate of proportion of HIV-uninfected individuals with active TB was modestly higher in SM-infected as compared to SM-uninfected (SM-infected: 19.7%; SM-uninfected: 15.8%), although the estimated distribution of Mtb infection outcomes was not different between SM groups (p=0.486, Figure 2). By contrast, within the HIV-infected group, the estimated distribution of Mtb infection outcomes differed between SM-infected and SM-uninfected groups (p=0.0018, Figure 2). The difference was driven by higher estimates of active TB in the SM-infected group when compared to the SM-uninfected group (SM-infected: 41.2%; SM-uninfected: 27.3%). Interestingly, the estimated proportion of HIV-infected individuals with LTBI was similar between groups (SM-infected: 38.3%; SM-uninfected: 36.7%).
Figure 2: Estimated Distribution of Mtb Infection Outcomes.
Probabilities are derived from TMLE estimation and are represented as stacked bar plots ± 95% confidence interval. Standard error estimates were obtained using estimated influence functions and the delta method. Significance level was calculated using Wald tests. The estimated distribution of Mtb infection outcomes differs between SM− and SM+ HIV+ individuals. The difference in the estimated proportion of Mtb infection outcomes beween SM+ and SM− groups differs between HIV+ and HIV− individuals.
Sensitivity analysis adjusting for CD4 count led to an attenuation of the association of SM on the probability of active TB in HIV-infected individuals. The estimated distribution of Mtb infection outcomes between SM-uninfected and SM-infected groups still differed between HIV-uninfected and HIV-infected individuals (p=0.0051; Supplementary Figure 2). Sensitivity analysis including individuals with indeterminate QFT status did not affect the observed results (data not shown).
Discussion
In this study we used a robust machine learning-based strategy to evaluate the association of SM infection on Mtb infection outcomes among HIV-infected and HIV-uninfected individuals in western Kenya. Our results suggest that co-infection with SM and HIV may perturb the distribution of Mtb infection outcomes and drive a higher proportion of active TB disease than might be expected through HIV infection alone.
Our data provide evidence that SM is associated with higher probability of active TB disease, after controlling for common covariates and additional helminth infections. This is consistent with findings from previous observational studies which evaluated SM as well as gastro-intestinal helminths, despite differences in study design and setting.9,12 The higher proability of active TB in SM-infected individuals is likely due to impaired or altered CD4 T cell responses, which are necessary for control of Mtb infection,25 as opposed to innate immune responses, since similar proportions of LTBI were observed between SM-uninfected and SM-infected groups. While helminths in general have been shown to impair Mtb immunity by compromising TH1 responses,5 this has not been observed for SM in humans.20 As such, the means by which SM might contribute to active TB disease remain unclear. In addition, we cannot determine whether active TB disease in the setting of SM infection is due to primary Mtb infection or reactivation of LTBI. This is further confounded in the setting of HIV, which results in profound CD4 T cell depletion, including memory CD4 T cells.26 Helminth infections, which induce TH2 responses, may lead to further dysregulation of TH1 immunity and therefore exacerbate HIV infection and perturb Mtb immunity.18,19 Alternatively, HIV has been shown to worsen SM pathology which may contribute to overall disease burden, resulting in susceptibility to the development of TB disease.18,19 Lastly, HIV and SM may simply impair Mtb immunity through independent mechanisms that both contribute to increased disease burden. Further studies are needed to ascertain the mechanism by which co-infection with SM and HIV increases the probability of active TB disease.
The strong association of SM with active TB among HIV-infected but not HIV-uninfected individuals suggests that co-infection with HIV and SM may be a greater risk factor than either infection alone. This is consistent with a study conducted in Uganda that reported an increased incidence of active TB amongst SM-infected HIV-infected individuals compared with SM-uninfected HIV-infected individuals.12 The data regarding the impact of SM infection and treatment on virological outcomes in the setting of HIV mono-infection has been conflicting.18,19,27,28 Testing and treatment of SM among HIV-infected individuals may, however, be useful as a strategy for preventing TB, particularly in high-burden settings.
The main strengths of this study are a large sample size and the use of a robust analytic method. While this cohort had a large number of coinfected individuals, SM was likely underdiagnosed in the HIV-infected group. HIV is known to reduce egg burden in stool, which was the diagnostic criterion utilized in this study.29 Despite this, we still found that HIV modifies the association between SM and active TB. Our findings therefore support robust testing to evaluate SM infection amongst HIV-infected individuals in future studies. While we found little evidence of confounding, we were underpowered to further stratify our analysis to test for interactions with measured characteristics such as biological sex. In addition, there is a possibility of bias by unmeasured confounding such as socioeconomic status, occupational risk, and previous SM infection and/or treatment. This study was also limited by the inability to determine the order or timing of infection, which would be crucial to derive causal conclusions about the direction of effects in this setting. Epidemiologically, people living in western Kenya often become infected with SM in early childhood with prevalence reaching a peak of around 60% in early adolescence.30 While mass drug administration has been very successful in this region, reinfection does occur in both children and adults.31 This suggests that individuals likely experience repeated SM infections prior to HIV and Mtb infection. One study in Uganda which reported increased TB incidence in SM-infected individuals compared with SM-uninfected individuals supports the notion that prior SM infection can increase the risk of active TB disease.12 Future studies, however, would benefit from evaluating Mtb infection outcomes over time among SM-infected individuals with and without HIV infection. This would be of particular interest in the setting of anthelminthic treatment and ART.
The interpretation of our results is influenced by the definitions used for Mtb infection status, which are based on imperfect diagnostic tools. There is currently no gold standard for diagnosing LTBI.32 The test utilized in this study, QuantiFERON-TB Gold (QFT), is an IFNγ release assay (IGRA) based on an immune response to Mtb antigens and does not differentiate LTBI from subclinical or active TB.33 The diagnosis of active pulmonary TB relies on a combination of symptoms and microbiological tests, the sensitivity of which can range from 50–90%.25 The diagnosis of active TB is even more challenging in HIV-infected individuals who are more likely to have negative microbiological tests.34
In high pathogen burden regions such as western Kenya, individuals may be infected with multiple microbes at any given time. It is therefore important to understand the interplay between these infections, not only to appropriately treat each individual, but also to manage public health initiatives. We provide evidence from machine learning-based approaches that SM infection is associated with significant alteration of Mtb infection outcomes in HIV-infected individuals. Further research is needed to establish the underlying mechanisms by which this occurs, and to compare SM-induced immune regulation in HIV-uninfected and HIV-infected individuals. If supported by prospective studies, these findings could have implications to the control of TB in SM-endemic areas of the world. Our findings suggest that treatment of SM with praziquantel should be considered for the clinical prevention of active TB in HIV-infected patients. Furthermore, regular praziquantel treatment of HIV-infected individuals who are at risk for recurring SM infection could be used as an additional low-cost component of TB control programs. Such consideration when designing treatment and prevention strategies could reduce the burden of TB disease at the population level.
Supplementary Material
Acknowledgements
We thank Dr. Kevin Cain for advice on the recruitment and enrollment of study participants with Mtb infection and TB disease in Kisumu, Kenya. We also thank Dr. W. Evan Secor for advice on testing and interpretation of helminth infections in study participants. We thank many additional members of the Kenya Medical Research Institute (KEMRI)/Centers for Disease Control and Prevention (CDC) team who helped with enrollment and evaluation of participants, and the participants themselves.
Conflicts of Interest and Source of Funding: This work was supported by the National Institute of Allergy and Infectious Diseases (5R01AI111948 to CLD and U19AI111211 to JDA, DK, JR, JDE, HMB, LAW, NRG, and CLD). NRG is supported by a Midcareer Investigator Award from the National Institute of Allergy and Infectious Diseases (K24AI114444). For the remaining authors, no conflicts of interest were declared.
References
- 1.Global Tuberculosis Report 2019. World Health Organization;2019. [Google Scholar]
- 2.Lin PL, Flynn JL. The End of the Binary Era: Revisiting the Spectrum of Tuberculosis. J Immunol. 2018;201(9):2541–2548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brooker S, Hotez PJ, Bundy DA. The global atlas of helminth infection: mapping the way forward in neglected tropical disease control. PLoS neglected tropical diseases. 2010;4(7):e779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maizels RM, McSorley HJ. Regulation of the host immune system by helminth parasites. J Allergy Clin Immunol. 2016;138(3):666–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Babu S, Nutman TB. Helminth-Tuberculosis Co-infection: An Immunologic Perspective. Trends Immunol. 2016;37(9):597–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elias D, Mengistu G, Akuffo H, Britton S. Are intestinal helminths risk factors for developing active tuberculosis? Tropical medicine & international health : TM & IH. 2006;11(4):551–558. [DOI] [PubMed] [Google Scholar]
- 7.Hailu AW, S GS, Merid Y, Gebru AA, Ayene YY, Asefa MK. The case control studies of HIV and Intestinal parasitic infections rate in active pulmonary tuberculosis patients in Woldia General Hospital and Health Center in North Wollo, Amhara Region, Ethiopia. Int J Pharma Sci. 2015;5(3):1092–1099. [PMC free article] [PubMed] [Google Scholar]
- 8.Tristao-Sa R, Ribeiro-Rodrigues R, Johnson LT, Pereira FE, Dietze R. Intestinal nematodes and pulmonary tuberculosis. Rev Soc Bras Med Trop. 2002;35(5):533–535. [DOI] [PubMed] [Google Scholar]
- 9.Mhimbira F, Hella J, Said K, et al. Prevalence and clinical relevance of helminth co-infections among tuberculosis patients in urban Tanzania. PLoS neglected tropical diseases. 2017;11(2):e0005342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abate E, Belayneh M, Gelaw A, et al. The impact of asymptomatic helminth co-infection in patients with newly diagnosed tuberculosis in north-west Ethiopia. PLoS One. 2012;7(8):e42901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chatterjee S, Kolappan C, Subramani R, et al. Incidence of active pulmonary tuberculosis in patients with coincident filarial and/or intestinal helminth infections followed longitudinally in South India. PLoS One. 2014;9(4):e94603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brown M, Miiro G, Nkurunziza P, et al. Schistosoma mansoni, nematode infections, and progression to active tuberculosis among HIV-1-infected Ugandans. Am J Trop Med Hyg. 2006;74(5):819–825. [PubMed] [Google Scholar]
- 13.Taghipour A, Mosadegh M, Kheirollahzadeh F, et al. Are intestinal helminths playing a positive role in tuberculosis risk? A systematic review and meta-analysis. PLoS One. 2019;14(10):e0223722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.WHO. Schistosomiasis: Progress Report 2001–2011, Strategic Plan 2012–2020. http://www.who.int/schistosomiasis/resources/9789241503174/en/. Published 2019. Accessed June 14, 2019.
- 15.Hotez PJ, Kamath A. Neglected tropical diseases in sub-saharan Africa: review of their prevalence, distribution, and disease burden. PLoS neglected tropical diseases. 2009;3(8):e412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van der Werf MJ, de Vlas SJ, Brooker S, et al. Quantification of clinical morbidity associated with schistosome infection in sub-Saharan Africa. Acta Trop. 2003;86(2–3):125–139. [DOI] [PubMed] [Google Scholar]
- 17.Narasimhan P, Wood J, Macintyre CR, Mathai D. Risk factors for tuberculosis. Pulm Med. 2013;2013:828939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Secor WE. The effects of schistosomiasis on HIV/AIDS infection, progression and transmission. Current opinion in HIV and AIDS. 2012;7(3):254–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Secor WE. Interactions between schistosomiasis and infection with HIV-1. Parasite Immunol. 2006;28(11):597–603. [DOI] [PubMed] [Google Scholar]
- 20.McLaughlin TA, Khayumbi J, Ongalo J, et al. CD4 T Cells in Mycobacterium tuberculosis and Schistosoma mansoni Co-infected Individuals Maintain Functional TH1 Responses. Frontiers in immunology. 2020;11:127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mazurek GH, Jereb J, Vernon A, et al. Updated guidelines for using Interferon Gamma Release Assays to detect Mycobacterium tuberculosis infection - United States, 2010. MMWR Recomm Rep. 2010;59(RR-5):1–25. [PubMed] [Google Scholar]
- 22.van der Laan MJR,D. Targeted Maximum Likelihood Learning. The International Journal of Biostatistics. 2006;2(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van der Laan MJ, Polley EC, Hubbard AE. Super learner. Statistical applications in genetics and molecular biology. 2007;6:Article25. [DOI] [PubMed] [Google Scholar]
- 24.Benkeser D, Carone M, Laan MJV, Gilbert PB. Doubly robust nonparametric inference on the average treatment effect. Biometrika. 2017;104(4):863–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pai M, Behr MA, Dowdy D, et al. Tuberculosis. Nat Rev Dis Primers. 2016;2:16076. [DOI] [PubMed] [Google Scholar]
- 26.Okoye AA, Picker LJ. CD4(+) T-cell depletion in HIV infection: mechanisms of immunological failure. Immunol Rev. 2013;254(1):54–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Colombe S, Machemba R, Mtenga B, et al. Impact of schistosome infection on long-term HIV/AIDS outcomes. PLoS neglected tropical diseases. 2018;12(7):e0006613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stete K, Glass TR, van Dam GJ, et al. Effect of schistosomiasis on the outcome of patients infected with HIV-1 starting antiretroviral therapy in rural Tanzania. PLoS neglected tropical diseases. 2018;12(10):e0006844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Karanja DM, Colley DG, Nahlen BL, Ouma JH, Secor WE. Studies on schistosomiasis in western Kenya: I. Evidence for immune-facilitated excretion of schistosome eggs from patients with Schistosoma mansoni and human immunodeficiency virus coinfections. Am J Trop Med Hyg. 1997;56(5):515–521. [DOI] [PubMed] [Google Scholar]
- 30.Sakari SSW, Mbugua AK, Mkoji GM. Prevalence of Soil-Transmitted Helminthiases and Schistosomiasis in Preschool Age Children in Mwea Division, Kirinyaga South District, Kirinyaga County, and Their Potential Effect on Physical Growth. J Trop Med. 2017;2017:1013802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mwandawiro C, Okoyo C, Kihara J, et al. Results of a national school-based deworming programme on soil-transmitted helminths infections and schistosomiasis in Kenya: 2012–2017. Parasit Vectors. 2019;12(1):76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Salgame P, Geadas C, Collins L, Jones-Lopez E, Ellner JJ. Latent tuberculosis infection--Revisiting and revising concepts. Tuberculosis (Edinb). 2015;95(4):373–384. [DOI] [PubMed] [Google Scholar]
- 33.Pai M, Riley LW, Colford JM Jr. Interferon-gamma assays in the immunodiagnosis of tuberculosis: a systematic review. Lancet Infect Dis. 2004;4(12):761–776. [DOI] [PubMed] [Google Scholar]
- 34.Getahun H, Harrington M, O’Brien R, Nunn P. Diagnosis of smear-negative pulmonary tuberculosis in people with HIV infection or AIDS in resource-constrained settings: informing urgent policy changes. Lancet. 2007;369(9578):2042–2049. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.