Abstract
In the current study, we aimed to investigate the network structure of COVID-19 symptoms and its related psychiatric symptoms, using a network approach. Specifically, we examined how COVID-19 symptoms relate to psychiatric symptoms and highlighted potential pathways between COVID-19 severity and psychiatric symptoms. With a sample of six hundred seventy-five recovered COVID-19 patients recruited 1 month after hospital discharge, we respectively integrated COVID-19 symptoms with PTSD, depression, and anxiety symptoms and analyzed the three network structures. In all three networks, COVID-19 severity and ICU admission are not linked directly to COVID-19 symptoms after hospitalization, while COVID-19 severity (but not ICU admission) is linked directly to one or more psychiatric symptoms. Specific pathways between COVID-19 symptoms and psychiatric symptoms were discussed. Finally, we used directed acyclic graph estimation to show potential causal effects between COVID-19 related variables and demographic characteristics.
Keywords: COVID-19; Symptom network; Anxiety, Depression; PTSD
1. Introduction
Patients of COVID-19 may have a series of symptoms after hospital discharge. Along with the COVID-19 symptoms, patients infected by COVID-19 may experience a variety of stressors and traumatic events, such as difficulty gaining admission to hospital wards, social and physical isolation, and deaths of other patients and/or family members. Furthermore, treatment for COVID-19 may have adverse effects on mental health and contribute to problems such as anxiety and insomnia (Zhao, Guo, & Li, 2020). Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) might also infect the brain, which could directly cause and have adverse effects on brain function and mental health (Holmes, et al., 2020). Previous studies following severe acute respiratory syndrome (SARS) infected patients in 2003 found that the prevalence of PTSD (post-traumatic stress disorder) in SARS survivors was respectively 46.2% and 38.8% at 3 months and 12 months after discharge (Gao, et al., 2020). A recent study found that 96.2% clinically stable COVID-19 patients reported clinically significant symptoms of PTSD (Bo et al., 2020).
The network approach is particularly useful for analyzing and visualizing complex relationships among psychopathology symptoms that would otherwise be difficult to disentangle using traditional approaches. From a network perspective, disorders are conceptualized as systems of causally connected symptoms rather than effects of a common latent factor. In recent years, the network approach has been applied to investigate the complex structure of a growing number of mental disorders, ranging from posttraumatic stress disorder (Birkeland et al., 2020), to depression (Fried et al. 2016), schizophrenia (Isvoranu et al., 2016), and anxiety (Beard et al. 2016). From a network perspective, it is conceivable that core symptoms might be more important than peripheral symptoms in the etiology and maintenance of mental disorders.
To date however, we are not aware of any research using the network approach to study COVID-19 and its related psychiatric symptoms. Further, there is little information about how COVID-19 symptoms relate to psychiatric symptoms. This study thus aims to fill in this gap in the literature, by respectively integrating COVID-19 symptom networks with PTSD, depression, and anxiety symptoms, in an effort to identify pathways between COVID-19 severity and psychiatric symptoms. Further, the data described here is made publicly available on https://osf.io/vufj4/
2. Method
2.1. Study design
The study protocol was approved by the research ethics committee of Renmin University of China on March 20, 2020. Nurses described the survey to each participant and obtained their oral consent. The participants completed the survey either online at home (with nurses by side offline) or offline at temporary quarantine places. For those at home, the nurses revisited them and sent an online link to complete. Only a small proportion of patients completed the link without nurses by side. The study is a cross-sectional survey conducted from April 11 to April 22, 2020.
2.2. Participants
675 recovered COVID-19 patients were included in the sample. All participants were recovered COVID-19 patients who had been discharged from hospitals, with an average discharge time of 36.75 days. The discharge date ranged from January 27, 2020 to April 21, 2020. According to the treatment guidelines in China, COVID-19 patients had to be isolated in quarantine places for 14 days after hospital discharge and then isolated in their homes for another 14 days afterward. Nurses distributed the questionnaires online or gave them when doing follow-up home visits after discharge. An estimate of 90% of patients visited responded to the survey. We examined the medical records of the patients later. The included patients have no psychiatry disorder history.
2.3. Demographic variables
Demographic data were self-reported by the participants, including occupation (hospital staff or not), sex (male or female), age, marital status, educational level (high school degree or lower, educational specialist diploma, Bachelor's degree, or Master's degree or higher, scores were respectively coded as from 1 to 4), income level (2000-5000 yuan, 5,000-10,000 yuan, 10,000-20,000 yuan, and more than 20,000 yuan per month, scores were respectively coded as from 1 to 4). (1000 yuan convert to US$141 as of May 2020.) Participants were also asked about whether they currently live with parents or children, whether any of their family members were infected, and whether these family members died from COVID-19.
2.4. Illness severity, symptoms, treatment
The questionnaire elicited self-reports of key clinical variables, including ICU admission, severity level of COVID-19 pneumonia (mild, moderate, severe, and critically ill), admission date, discharge date, current symptoms after hospital discharge (cough, chest distress, chest pain, dizziness, fatigue, dyspnea etc.), IMV treatment (invasive mechanical ventilator), ICU (intensive care unit), corticosteroids treatment, presence of chronic underlying disease (e.g. diabetes, hypertension).
2.5. Outcomes
Anxiety, depression, and post-traumatic stress disorder (PTSD) were evaluated using Chinese versions of validated measurement tools. Specifically, the 7-item Generalized Anxiety Disorder scale (GAD-7; range, 0-21) (Kroenke et al., 2001; He et al., 2010), the 9-item Patient Health Questionnaire (PHQ-9; range, 0-27) (Spitzer et al., 2006; Zhang, et al., 2013), and the 20-item PTSD Checklist for DSM-5 (PCL-5; range, 0-80) (Blevins et al., 2015; Wang et al., 2015) were used to assess the severity of symptoms of anxiety and depression in the past two weeks, and PTSD in the past month. Higher scores on the items and/or test score indicate more severe symptomatology. The reliabilities of GAD-7, PHQ-9 and PCL-5 were respectively .890, .875, .948.
2.6. Statistical analysis
Markov Random Fields. In light of the employed sample size, we opted for estimating more stable network models and thus included nodes per disorder rather than all nodes in one large network structure. We constructed Markov Random Fields (MRFs) which are the main type of networks studied in network psychometrics (Robinaugh et al., 2020). A MRF is model in which variables are represented by nodes (circles), which are connected with edges (lines) if sufficient evidence is found that two variables are associated after controlling for all other variables in the dataset (Epskamp et al., 2018). Edges in a MRF may be indicative of causal relationships, but can also be interpreted to show predictive relationships: the nodes that are connected to a node of interest would likely also be substantial/significant predictors of that node in a multiple (generalized) regression model (Epskamp et al., 2018). Because the data contained both continuous and binary variables, we estimated mixed graphical models (MGM)—a type of MRF that supports variables with different distributions. We estimated the MGM models using the mgm package (version 1.2.12; Haslbeck and Waldorp, 2020) for R (version 4.0.5; R Core Team 2020). This package estimates a network model by performing regularized generalized regressions for each variable, estimating edges connected to that variable. Regularization uses a tuning parameter, which we selected using EBIC model selection with , which is generally conservative and does not often falsely include edges (Isvoranu and Epskamp, 2021). Because each edge is estimated twice (once for each node an edge is connected to), we used an OR-rule, indicating that an edge was included in our network if it was included at least once in the performed regression models. In each of the three MGM models, we included COVID-19 severity (continuous), ICU admission (binary), IMV treatment (binary), corticosteroid treatment (binary), family infection (binary), death in family (binary), COVID-19 symptoms after discharge (binary), and anxiety/depression/PTSD symptoms (continuous). We also included age (as continuous variable) and sex (binary; men = 1 women = 2)
The treatment variables for IMV usage and corticosteroid usage featured missing datapoints (18.5% and 31.7% respectively), which the mgm package cannot handle. To this end, we used the mice package (version 3.13.0; van Buuren and Groothuis-Oudshoorn, 2011) to impute missing data using multiple imputation. We imputed the data 10 times, and only retained edges in our final network that were included in the estimated networks based on at least 9 out of 10 imputed datasets. To check for accuracy of estimations, we performed 1,000 non-parametric bootstraps as recommended in the network psychometrics literature (Epskamp, Borsboom, et al., 2018). We included the multiple imputation strategy in the bootstrapping procedure. We did not investigate the centrality of the network structure, as our intent was discovering potential pathways between COVID-19 symptoms, severity and psychiatric symptoms.
Directed Acyclic Graphs. To investigate potential causal directions between COVID-19 disease-specific variables, as well as demographic characteristics, we estimated directed acyclic graphs (DAGs; (Kalisch and Ch, 2007; Pearl, 2000), using the stable PC-algorithm (Colombo and Maathuis, 2014; Kalisch et al., 2012) via the bnlearn R package (version 4.6.1; Scutari, 2010). Unlike the mgm package, the bnlearn package is capable of handling ordered categorical variables. We included the variables age (because bnlearn supports ordinal variables, we made age ordinal with levels 0-17, 18-34, 35-64, 65+ to allow for nonlinear effects), income (ordinal), severity (ordinal), sex (categorical), education (categorical), medical staff (categorical), married (categorical), smoking (categorical), underlying disease (categorical), ICU admission (categorical), IMV treatment (categorical), corticosteroid treatment (categorical), family infection (categorical), death in family (categorical), and the sum-scores of the anxiety, depression and PTSD symptoms (continuous). Here we chose to include the sum-scores rather than the symptom scores to reduce model complexity. We handled the missing data in the same manner as in the undirected network model estimation above: using the R package mice we imputed 10 datasets, and we only retained the edges that were included at least 9 times. The pc-algorithm returns both directed edges and undirected edges (when the algorithm cannot distinguish between direction of effect). To check for stability in the estimation, we performed 1,000 non-parametric bootstraps, and investigated the proportion of times each directed or undirected edge was included in the network.
Of note, DAG estimation is typically not recommended for network analysis of symptoms (Epskamp et al., 2018), as the assumption of acyclicity is often not tenable. We chose to perform DAG estimation on these variables, as acyclicity is much more likely to hold in these cases. For example, background variables such as underlying illnesses, education and sex clearly cannot be caused by a more recent ICU admission. To aid the algorithm, we blacklisted several edges from being included in the model: (1) all edges towards age and sex, as age and sex can be regarded as exogenous variables that cannot be caused by other variables in the analysis, (2) edges from corticosteroid treatment, IMV treatment, ICU admission, and COVID19-severity towards underlying illness, (3) edges from corticosteroid treatment, IMV treatment, and ICU admission to COVID-19-severity, as we can assume severity of COVID-19 causes its treatment, not the other way around, (4) IMV treatment to ICU admission, as IMV is only administered at the ICU, and finally (5) all edges from treatment variables, ICU admission and COVID-19 severity to income and smoking, as due to the short time between hospitalization and administration, we can assume little to no effect on these long-term variables. No edges were whitelisted, meaning that all edges included in the model were discovered by the algorithm.
3. Results
MRF Analyses. The estimated undirected network models are shown in Figs. 1 , Fig. 2, Fig. 3 for anxiety, depression and PTSD data respectively, and bootstrapped accuracy plots can be seen in the online supplementary materials on the Open Science Framework (link: https://osf.io/vufj4/). As the scale of edges differs in MGM models depending on the type for each node (e.g., edges between continuous nodes cannot be stronger than 1, but edges between binary nodes have no upper limit), we highlighted edges above 0.2. To this end, the strong edges between binary variables (COVID-19 symptoms) are not necessarily stronger than edges between continuous variables (psychiatric symptoms). The supplementary materials show that all networks were relatively stable, with larger sampling variation among edges connected to binary variables than edges connected to continuous variables.
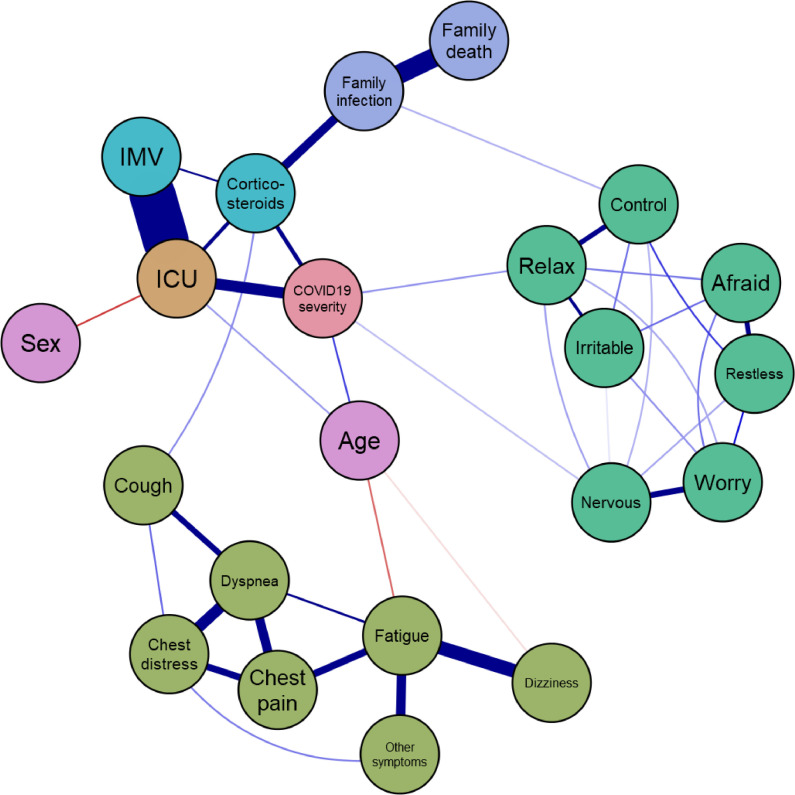
Fig. 1.
Graphical representation of the estimated mixed graphical model for anxiety data. Teal nodes represent anxiety symptoms, green nodes represent residual COVID-19 symptoms after hospitalizations, purple nodes family relations, blue nodes treatment variables, orange indicates ICU admission, red indicates COVID-19 severity, and pink indicates covariates. The qgraph package (version 1.7.1; Epskamp et al., 2012) was used to visualize the result. Blue links indicate positive effects and red links negative effects. The cut argument, used to split scaling of width and color, was set to 0.2, to highlight edges above 0.2.
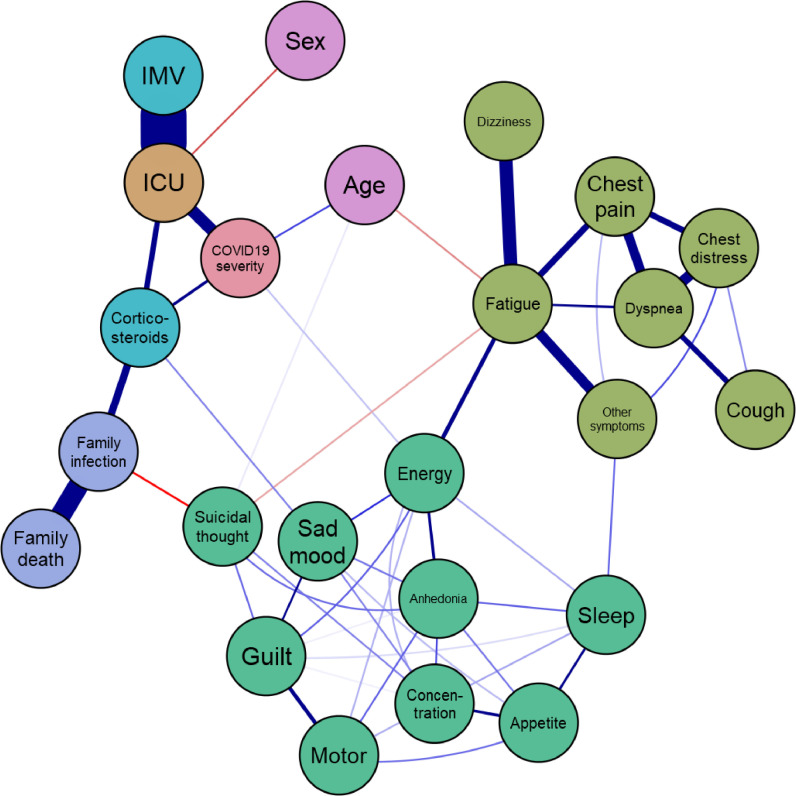
Fig. 2.
Graphical representation of the estimated mixed graphical model for depression data. Teal nodes represent depression symptoms, green nodes represent residual COVID-19 symptoms after hospitalizations, purple nodes family relations, blue nodes treatment variables, orange indicates ICU admission, red indicates COVID-19 severity, and pink nodes are covariates. The qgraph package (version 1.7.1; Epskamp et al., 2012) was used to visualize the result. Blue links indicate positive effects and red links negative effects. The cut argument, used to split scaling of width and color, was set to 0.2, to highlight edges above 0.2.
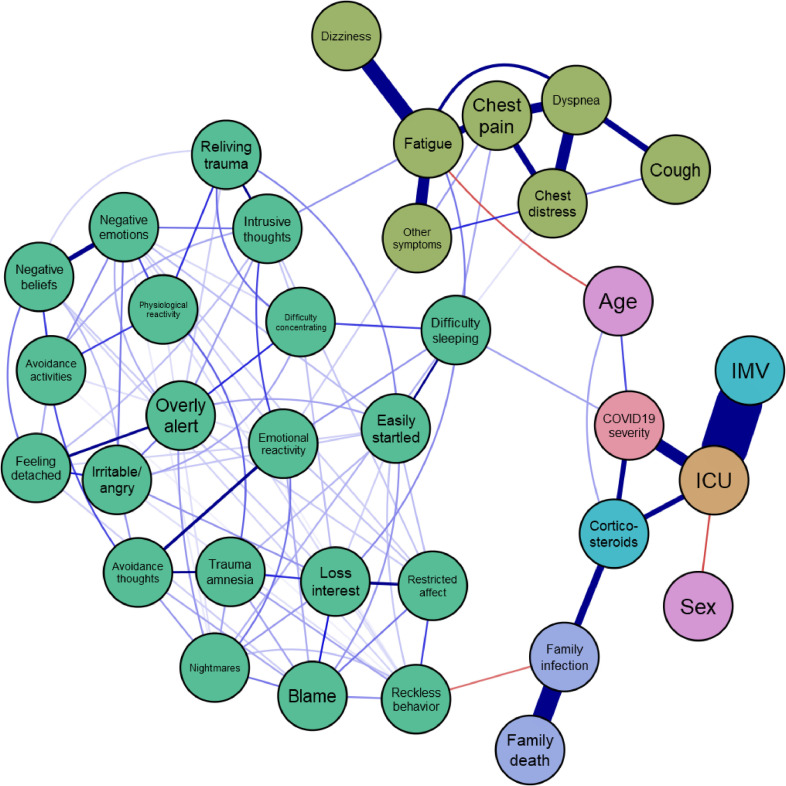
Fig. 3.
Graphical representation of the estimated mixed graphical model for PTSD data. Teal nodes represent PTSD symptoms, green nodes represent residual COVID-19 symptoms after hospitalizations, purple nodes family relations, blue nodes treatment variables, orange indicates ICU admission, red indicates COVID-19 severity, and pink nodes are covariates. The qgraph package (version 1.7.1; Epskamp et al., 2012) was used to visualize the result. Blue links indicate positive effects and red links negative effects. The cut argument, used to split scaling of width and color, was set to 0.2, to highlight edges above 0.2.
All three networks show roughly the same pattern:2 COVID-19 severity and ICU admission are not linked directly to COVID-19 symptoms after hospitalization, COVID-19 severity (but not ICU admission) is linked directly to one or more psychiatric symptoms, family infection is linked to a psychiatric symptom, some residual COVID19 symptoms are linked to psychiatric symptoms, older participants more often had higher COVID-19 severity and ICU admission and lower levels of fatigue as residual COVID-19 symptom, and men were more often admitted to the ICU than women. While some of the edges were common to all networks, other edges were specific to the network structure analyzed, as described below.
First, in the anxiety network, COVID-19 severity is directly linked to the “relax” and “nervous” nodes, indicating that subjects with higher levels of COVID-19 had a harder time relaxing and were more nervous. Family infection was linked to “control”, indicating that subjects with infections in the family showed higher levels of feeling lack of control of worries. None of the COVID19 residual symptoms were linked to anxiety symptoms.
Second, the depression network showed a link between COVID-19 severity and the node “energy”, indicating that more severe COVID-19 cases more often endorsed loss of energy. Corticosteroid treatment was linked to “sad mood.” Not surprisingly, the “fatigue” COVID-19 symptom was linked to the “energy” depression symptom. There is a link between other COVID-19 symptoms and sleep. Striking were two negative edges connected to suicidal thought: the COVID-19 symptom fatigue and infection in the family. This indicated that infections in the family may lead to a lower level of suicidal thought, and that higher levels of fatigue are associated with lower levels of suicidal thought. Further investigation revealed that marginal tetrachoric correlations (correlations without partialling out other variables) were also negative: based on 10,000 bootstrap samples, the 95% confidence interval of the tetrachoric correlation between suicidal thought and family infection was -0.466 to -0.232, and for the tetrachoric correlation between suicidal thought and fatigue -0.341 to -0.0228. A common effect interpretation (De Ron et al., 2019; Epskamp et al., 2018) of these negative edges can be disregarded, as there are no clear common effects of two nodes that are negatively linked in the network, and the marginal correlations were also negative. Of note, however, is that “age” was linked positively to both “suicidal thought” COVID-19 severity.
Third, the PTSD network showed a direct link between COVID-19 severity and “difficulty sleeping”, indicating that more severe COVID-19 cases had more difficulty sleeping. Difficulty sleeping was also linked to several of the COVID-19 residual symptoms. The residual COVID-19 symptom “fatigue” was linked to “intrusive thoughts.” A final thing to note in the PTSD network was that family infection was negatively linked to reckless behavior, suggesting that subjects may be generally more cautious when one or more family members were infected with COVID-19.
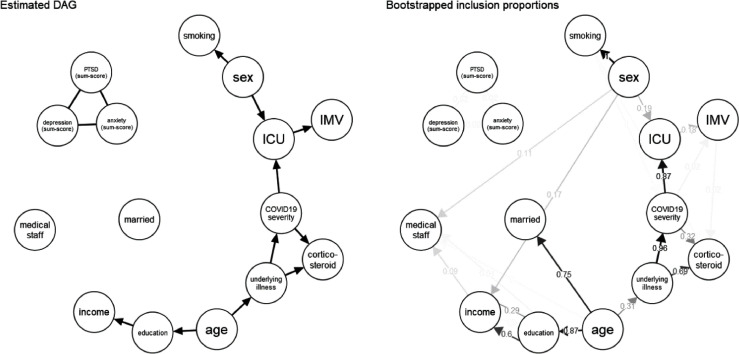
DAG Analysis. The estimated DAG structure and inclusion proportions of each edge can be seen in Fig. 4 . This figure shows that the recovered DAG structure was quite stable, as most edges were retained in many of the bootstrap replications. A first thing to note is that the anxiety, depression and PTSD sum-score variables were not connected to the other variables, indicating that at the disorder level there is no strong evidence for links between COVID-19-severity and treatment and heightened numbers of psychiatric symptoms. The algorithm could not distinguish direction of effect between these disorder-level variables, and the bootstraps showed that edges between the disorder level variables were only rarely included. Focusing on the main connected component on the graph, the model predicted that COVID-19 severity was heightened by underlying illness, that ICU admission was caused by COVID-19 severity, that men were admitted more than women, and IMV treatment was caused by ICU admission. Of note, the model also predicted that age causes education (subjects between 18 and 35 had higher levels of education than younger and older subjects), education causes income (higher educated subjects had higher incomes), and sex causes smoking.
Fig. 4.
Directed Acyclic graph (DAG) estimation results. The network structure was estimated using the stable PC-algorithm implemented in the bnlearn package, using mice for multiple imputation and only retaining edges that were included in nine out of ten imputed datasets. The left panel shows the estimated DAG structure, and the right panel shows the inclusion proportion of each edge based on 1,000 bootstrap replications. An undirected edge indicates that the algorithm could not determine the direction of effect.
4. Discussion
In this study, we present data of recovered COVID-19 patients, including medical and psychiatric symptom variables. We explored the data using undirected and directed network models, estimating individual network models on subsets of the variables.
The undirected network models showed several striking effects. First, residual COVID-19 symptoms were not linked to COVID-19 severity levels during hospitalization, nor were they linked to ICU admission and different treatment variables, with the exception of coughing being linked to corticosteroid treatment. This indicates that more severe COVID-19 cases do not necessarily feature more or less COVID-19 symptoms after hospitalization. Second, COVID-19 severity was consistently linked to at least one psychiatric symptom in all three models: inability to relax and feeling nervous in the anxiety network, lower energy in the depression network, and difficulty sleeping in the PTSD network. Of note, these effects are present after controlling for ICU admission and IMV and corticosteroid treatment. This indicates that higher severe COVID-19 cases may feature some psychiatric symptoms after hospitalizations, which may in turn affect other symptoms as per the network perspective (Borsboom, 2017). Third, some residual COVID-19 symptoms after hospitalization were also linked to psychiatric symptoms, although most of these can be readily explained (e.g., fatigue being linked to a loss of energy). Finally, some striking links were found between infection in the family and psychiatric symptoms: family infections were negatively linked to suicidal thought and reckless behavior, possibly due to subjects having more accompanies during the quarantine periods.
With regard to the directed network analysis, at the disorder level no connections were found between COVID-19 severity and treatment to psychiatric scale sum-scores. However, we identified relationships in the DAG, such as age causing underlying illnesses, underlying illnesses causing COVID-19 severity, and COVID-19 severity causing ICU admission, which all make sense from a theoretical point of view. While several edges were blacklisted (not allowed to be included), no edges were whitelisted. This means that all edges were discovered by the estimation method. As such, while the presented DAG doesn't necessarily include relationships not already known in the literature, the model is exemplary of showcasing that DAG estimation can lead to sensible results and may therefore be a promising avenue for future research. Here, it should be noted that sum-scores likely poorly capture the complexity underlying symptom dynamics (Fried and Nesse, 2015), and directed acyclic graphs themselves may poorly represent interactions that may lead to comorbidity (Cramer et al., 2010). To this end, the found results of no identified direction of effect between psychiatric sum-scores and the limited linkage to other variables3 is in line with the network perspective (Borsboom, 2017). The usage of undirected network structures and symptom-level data may therefore be a much better approach for identifying potential pathways between different levels of symptomatology.
Several limitations are important to be noted. First, the multiple imputation strategy used for imputing data is not yet commonly used in network analysis and has not been validated. We don't expect the imputation strategy to impact our results very much, as only two variables featured missing data and we were conservative on including edges given the imputation strategy. Second, the mgm R-package used does not handle ordered categorical variables, and as such psychiatric symptom variables were treated as continuous. Third, the sample size is relatively high, but higher sample sizes may be warranted for such high-dimensional methods. In particular, we did not perform a network analysis including all variables, nor did we investigate moderation effects (Haslbeck et al., 2019). While the mgm method is relatively conservative, a limited sample size may mean a lack of statistical power (sensitivity) to detect edges, and as such we may have missed on edges to be included in the network models. This is exemplified by the edge between corticosteroid treatment and coughing, which was included in the anxiety and depression networks, but not in the PTSD network (which featured more nodes). Further, while DAG estimation routines allow for detecting direction of effects, the DAG methodology features strong assumptions unlikely to hold (e.g., acyclicity). Finally, all analyses were highly exploratory, and as such should be interpreted as hypothesis generating rather than confirming effects.
5. Conclusion
To conclude, we carried out network analyses on recovered COVID-19 hospitalized subjects and anxiety, depression and PTSD symptoms and revealed several pathways from COVID-19 severity to psychiatric symptom networks. In addition, we showcased potential causal effects between COVID-19 related variables and demographic characteristics, highlighting how the use of directed acyclic graph estimation can lead to interpretable and stable results. DAG estimation as a tool may be useful in identifying specific causal relations, however we note that sum-scores are likely to poorly capture the complexity underlying symptom, and DAGs themselves may poorly represent interactions that may lead to comorbidity, as we may expect comorbidity to result from more complex cyclic interactions instead. Finally, we invite other researchers to further analyze the data presented here, which we made freely available at https://osf.io/vufj4/.
Author statement
Sacha Epskamp, Dong Liu, Adela-Maria Isvoranu contributed to the concept, design, analysis, writing, or revision of the manuscript. Caixia Chen, Wenjun Liu, Xinyi Hong contributed to the data collection and management process.
Funding
None.
Declaration of Competing Interest
All authors declare that they have no conflicts of interest.
Acknowledgements
None.
Footnotes
Note: Some overlap is expected, as several variables are the same in all three networks. To this end, the similar patterns are not replications.
While the undirected networks showed edges between COVID-19 severity and some psychiatric symptoms, the DAGs did not show links from COVID-19 severity to disorder level variables. These results align, as we would expect COVID-19 severity to be connected to far more psychiatric symptoms if it would also be linked to the aggregate sum-score variable.
References
- Birkeland MS, Greene T, Spiller TR. The network approach to posttraumatic stress disorder: a systematic review. Eur. J. Psychotraumatol. 2020;11(1) doi: 10.1080/20008198.2019.1700614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D. A network theory of mental disorders. World Psychiatry. 2017;16(1):5–13. doi: 10.1002/wps.20375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colombo D, Maathuis MH. Order-independent constraint-based causal structure learning. J. Mach. Learn. Res. 2014;15(1):3741–3782. [Google Scholar]
- Cramer AOJ, Waldorp LJ, van der Maas HLJ, Borsboom D. Comorbidity: a network perspective. Behav. Brain Sci. 2010;33(2–3):137–150. doi: 10.1017/S0140525X09991567. [DOI] [PubMed] [Google Scholar]
- Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: a tutorial paper. Behav. Res. Methods. 2018;50(1):195–212. doi: 10.3758/s13428-017-0862-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S, Cramer AOJJ, Waldorp LJ, Schmittmann VD, Borsboom D, Waldrop LJ, Schmittmann VD, Borsboom D. qgraph : network visualizations of relationships in psychometric data. J. Stat. Softw. 2012;48(4):1–18. http://www.jstatsoft.org/v48/i04 [Google Scholar]
- Epskamp S, Maris GKJ, Waldorp LJ, Borsboom D. In: The Wiley Handbook of Psychometric Testing, 2 Volume Set: A Multidisciplinary Reference on Survey, Scale and Test Development. Irwing P., Hughes D., Booth T., editors. Wiley; 2018. Network Psychometrics.http://arxiv.org/abs/1609.02818 [Google Scholar]
- Epskamp S, Waldorp LJ, Mõttus R, Borsboom D. The Gaussian graphical model in cross-sectional and time-series data. Multivariate Behav. Res. 2018;53(4):453–480. doi: 10.1080/00273171.2018.1454823. [DOI] [PubMed] [Google Scholar]
- Fried EI, Nesse RM. Depression sum-scores don’t add up: why analyzing specific depression symptoms is essential. BMC Med. 2015;13(1):72. doi: 10.1186/s12916-015-0325-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haslbeck JMB, Borsboom D, Waldorp LJ. Moderated network models. Multivariate Behav. Res. 2019:1–32. doi: 10.1080/00273171.2019.1677207. [DOI] [PubMed] [Google Scholar]
- Haslbeck JMB, Waldorp LJ. MGM: Estimating time-varying mixed graphical models in high-dimensional data. J. Stat. Softw. 2020;93(1):1–46. doi: 10.18637/jss.v093.i08. [DOI] [Google Scholar]
- He XY, Li CB, Qian J, Cui HS, Wu WY. Reliability and validity of a generalized anxiety scale in general hospital outpatients. Shanghai Arch. Psychiatry. 2010;22(4):200–203. doi: 10.3969/j.issn.1002-0829.2010.04.002. [DOI] [Google Scholar]
- Isvoranu AM, van Borkulo CD, Boyette LL, Wigman JT, Vinkers CH, Borsboom D, Investigators Group. A network approach to psychosis: pathways between childhood trauma and psychotic symptoms. Schizophr. Bull. 2016;43(1):187–196. doi: 10.1093/schbul/sbw055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isvoranu, A. M., & Epskamp, S. (2021). Continuous and ordered categorical data in network psychometrics: which estimation method to choose? Deriving guidelines for applied researchers. https://psyarxiv.com/mbycn/. [DOI] [PubMed]
- Kalisch M, Ch BME. Estimating high-dimensional directed acyclic graphs with the PC-algorithm Peter B ¨ uhlmann. J. Mach. Learn. Res. 2007;8:613–636. [Google Scholar]
- Kalisch M, Mächler M, Colombo D, Maathuis MH, Bühlmann P. Causal inference using graphical models with the R package pcalg. J. Stat. Softw. 2012;47(11):1–26. [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9. J. Gen. Intern. Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearl J. Cambridge Univ Press; 2000. Causality: Models, Reasoning and Inference (Vol. 29) [Google Scholar]
- R Core Team . R Foundation for Statistical Computing; 2020. R: A Language and Environment for Statistical Computing. [Google Scholar]
- Robinaugh D.J., Hoekstra R.H., Toner E.R., Borsboom D. The network approach to psychopathology: a review of the literature 2008–2018 and an agenda for future research. Psychol. Med. 2020;50(3):353–366. doi: 10.1017/S0033291719003404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scutari M. Learning Bayesian networks with the bnlearn R package. J. Stat. Softw. 2010;35(3):1–22. [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch. Intern. Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- van Buuren S, Groothuis-Oudshoorn K. mice: multivariate imputation by chained equations in R. J. Stat. Softw. 2011;45(3):1–67. doi: 10.18637/jss.v045.i03. [DOI] [Google Scholar]
- Zhang YL, Liang W, Chen ZM, et al. Validity and reliability of patient health questionnaire-9 and patient health questionnaire-2 to screen for depression among college students in China. Asia Pac. Psychiatry. 2013;5(4):268–275. doi: 10.1111/appy.12103. [DOI] [PubMed] [Google Scholar]