Abstract
Background:
Understanding the perception and concerns of people about COVID-19 vaccine in developing and populous country like India will help in understanding demand for the vaccine and further tailoring out public health information and education activities. The study was carried out to assess the present state of knowledge people have about the probable vaccine for COVID-19, to know the preferences of respondents about this vaccine and to learn the expectations and apprehensions of people about features of this prospective COVID-19 vaccine residing in the capital city of India.
Methods:
This cross-sectional study was conducted amongst the residents of Delhi, India from July to October 2020. Both offline and online interview method was used to collect date from 513 participants representing various occupational strata. Data were collected on sociodemographic variable, vaccine acceptance and concerns regarding COVID-19 vaccine.
Results:
Among the study population, 79.5% said they will take the vaccine while 8.8% said they were not going to take the vaccine and remaining 11.7% had not yet decided about it. More than 50% were willing to pay for the vaccine and 72% felt vaccine should first be given to health workers and high-risk group.
Conclusion:
The following study has helped to understand the percentage of people who are hesitant to take the vaccine and also the concerns regarding the vaccine. Also since half of the population is willing to pay for the vaccine, a strategic approach considering the various economical classes of people could be applied in a developing country like India.
Keywords: COVID-19, India, New Delhi, vaccine acceptance
Introduction
COVID-19, as we know today, is one of the biggest challenges mankind has faced in the century. The disease has jolted the entire world with 111.2 million cases occurring worldwide and more than 2 million deaths till 20 February 2021.[1] India reported 11 million cases and 156,000 deaths as on 20 February 2021.[2] There has been extensive global efforts to combat the pandemic. Efforts in resource-constrained setting like India have also been multidimensional.[3] However, the disease has caused huge economic loss and has left the entire world socially crippled.
As mentioned by various epidemiologists, the virus is here to stay. In such situations, acquiring immunity against the virus becomes essential. Immunity can be acquired in two ways, either naturally or through vaccine. In the current pandemic, the role of safe and effective COVID-19 vaccine will be very vital in the fight against COVID-19. Many epidemiologists and medical experts have raised doubts and question over emergency authorization of COVID-19 vaccine, yet people are hopeful about the vaccine.[4] Preliminary findings show that a vaccine developed by Pfizer and BioNTech can prevent more than 90% of people from getting COVID-19 and Moderna vaccine has claimed 94.5% efficacy in its interim analysis.[5]
India launched Covaxin and Covisheild vaccine and has started immunizing. A year has passed since India recorded its first case in January 2020, and vaccination for COVID-19 is now gradually picking up in India. India has now become the fastest in the world to give more than 4 million vaccine doses. However, the efficacy, frequency, safety, preferences and precautions are some such queries that every individual whoever counts on the hope of vaccine advent harbours in his mind.
Advent of any vaccine confronts plenty of issues. Vaccine acceptance is a social tool which plays an important role for advent, implementation and continuation of any vaccination programme.[6,7] India's vaccination programme for childhood vaccination has been applauded for its wide coverage and success. Considering the population size and varied socio-demographic scenario, India's COVID-19 vaccine drive will be the largest amongst all countries and will definitely be more challenging.
Accounting for the perception of people about COVID-19 vaccine, advent will give empirical details about their aspirations and apprehensions. Considering factors like willingness to pay will help in considering the financial constraints and economies into consideration before a large-scale bulk production. Thus, this study is being conducted with the objectives to assess the present state of knowledge people have about the probable vaccine for COVID-19, to know the preferences of respondents about this vaccine and to learn the expectations and apprehensions of people about features of this prospective COVID-19 vaccine residing in the capital city of India.
Materials and Methods
Study design, setting and participants
The cross-sectional quantitative study was carried out among the residents of Delhi, North India from July to October 2020.
Various sections of society were taken:
Occupation such as all staff in health work force including doctors, nurses, paramedics and health workers
Staff in corporate sectors including engineers, technicians, managers and leaders
Business class including shopkeepers, owners, delivery boys, managers etc.
Education sector which constitutes a major chunk and plays major role in taking care of young ones like teachers, principal and tutors
Sample size
In such a dynamic scenario where figures escalate and slump on a day-to-day basis, considering the rule of assumptions, a prevalence of 50% was considered and Schwartz formula was applied. At 90% power and 95% confidence interval (CI), the sample size came out to be 400. Considering a nonresponse rate of 10%, sample size of 440 was obtained and further rounded of to 500. A total of 513 participants responded.
Procedure
Respondents above 18 years of age, who consented, were included in the study, which was either conducted physically as an interview or using online technique, depending on the respondent's convenience.
For the physical interview method, individuals were selected by simple random sampling from among these strata so as to reach our estimated sample size. After a brief training, the interviewer collected data from these subjects by a semistructured questionnaire which was pretested and expert validated.
Online method: For those individuals who consented but had time constraint, we wilfully administered the questionnaire to them in Microsoft forms and awaited response from them via the link provided. The terms not understood by them were clarified and explained to them over phone. All terms of ethical consideration, beneficence, autonomy and confidentiality were followed.
The questionnaire was semi-structured and contained the socio-demographic details, respondent's perception and knowledge about the prospective COVID-19 vaccine, questions regarding their expectations, fears, barriers and apprehensions about such a vaccine. The last part included questions regarding their promptness to be part of any such vaccine trials for the benefit of mankind.
The questions were validated by experts and repeat consultations and modifications done as required after an initial pilot study. A link was created to be able to reach professionals who consented to be part of the study but owing to time constraint preferred to respond to it as per their own convenience.
The preference of individuals for vaccine in the terms of its availability, efficacy, intake and cost mounted on a likelihood scale with 1 depicting least likely and 6 depicting most likely was taken up as the dependant variables. Sociodemographic details like age, caste, job profile, knowledge about the vaccine's safety, efficacy, time of advent, adequacy etc., the willingness to be part of trial, preferences for route of administration, readiness to spend and take booster doses were also analysed.
Data analysis
The completed questionnaire was checked for completeness and consistency. Collected data were entered in the MS Excel spreadsheet, coded appropriately and later cleaned for any possible errors in a Statistical Package for Social Studies for Windows version 21.0. Categorical data were presented as percentage. Pearson's Chi-square test was used to evaluate differences between groups for categorized variables. In case, the expected cell count was found to be less than 5 in >20% cells, we used Fisher's exact test. Normally distributed data were presented as means and standard deviation with 95% CIs. All tests were performed at a 5% level significance, and thus the value less than 0.05 (P value < 0.05) was taken as significant association.
Ethics statement
Permission to conduct the study was taken from the Research Proposal Advisory Committee and approval was taken from the Institutional Ethics Committee. Informed consent in writing was taken from respondents who participated through physical interview and online consent was taken by participants who filled the form online. There were no conflict of interest and all measures of autonomy and confidentiality were strictly maintained.
Results
A total of 513 participants responded. Amongst all the participants, almost equal participation was there from males (50.9%) and females (48.3%). Most of the participants were middle aged (41.7%), Hindu by religion (65.9%) and currently married (57.7%). Most of the study participants (88.5%) were either in college or had completed college. Among occupation of participants, most of them were healthcare workers like doctor/nurse/paramedic/ auxiliary nurse midwife (ANM) (42.7%), 23.2% were students and rest were from other service sectors.
Based on the history of COVID-19 infection among the study participants, 2.5% had COVID-19 infection in the past, and 1.4% said there was mortality due to COVID-19 in their family. Around three-fourth had a moderate-to-strong feeling that they may catch the infection anytime, while almost two-third of those who had COVID-19 infection in past think that reinfection can happen. Most of them were afraid of dying after getting COVID-19 [Table 1].
Table 1.
COVID-19-related experiences and perceptions among the study population
| Variables | Frequency n=513 | Percentage |
|---|---|---|
| Did you have COVID-19 in the past | ||
| Yes | 13 | 2.5 |
| No | 500 | 97.5 |
| Did anyone in family COVID-19 in the past | ||
| One person | 26 | 5.1 |
| More than one person | 23 | 4.5 |
| None | 464 | 90.4 |
| Did anyone in family died due to COVID-19 | ||
| Yes | 7 | 1.4 |
| No | 42 | 8.2 |
| No COVID in family | 464 | 90.4 |
| How likely do you feel that you can get COVID-19 anytime@ | ||
| Not at all | 26 | 5.3 |
| Some time | 109 | 22.0 |
| Moderately feeling | 295 | 59.6 |
| Strong feeling | 65 | 13.1 |
| How likely do you feel you can get COVID-19 reinfection# | ||
| Not at all | 2 | 15.4 |
| Some time | 3 | 23.1 |
| Moderately feeling | 4 | 30.8 |
| Strong feeling | 4 | 30.8 |
| How likely do you feel that you may die from COVID-19^ | ||
| Not at all | 90 | 17.8 |
| Some time | 271 | 53.5 |
| Moderately feeling | 132 | 26.0 |
| Strong feeling | 14 | 2.8 |
@Total 495, #Total 13 (if previously infected), ^Total 507
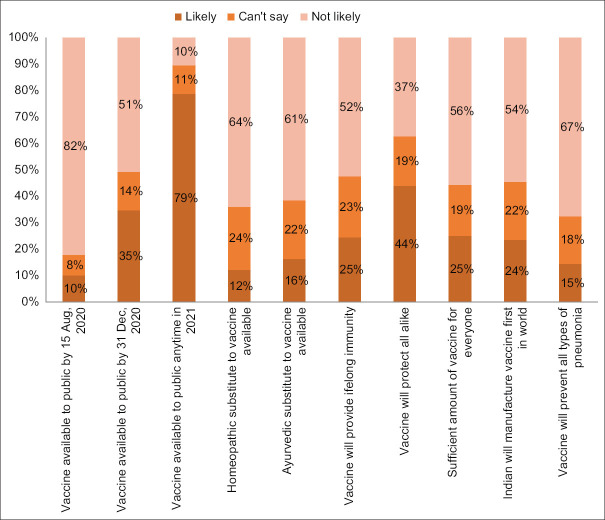
Figure 1 shows COVID-19 vaccine acceptance. It was observed that 79.5% would take the vaccine whenever available, while 8.8% said they would turn it down and remaining 11.7% had not yet decided about it. Figure 2 shows knowledge and attitude of study population about the COVID-19 vaccine. Most of them believed that vaccine would be available to public next year (78.8%), but at the same time half of them believe that it may not be in sufficient amount for everyone to get (50.1%) and 52.4% did feel it will not prevent the COVID-19 disease for lifelong. Majority knew that the COVID-19 vaccine would not prevent all types of pneumonia (67.4%).
Figure 1.
Vaccine acceptance response among the study population
Figure 2.
Vaccine-related knowledge and attitude among the study population
As per Table 2, the study shows that participants were willing to take COVID-19 vaccine by any route in any number of doses, but preferably with a good effectiveness and rare side adverse reaction. People were willing to get the vaccine even if they need to pay for it (84.4%) and had to get vaccinated every year (75.6%).
Table 2.
Vaccine-related preferences among the study population
| Variables | Frequency n=513 | Percentage |
|---|---|---|
| Preferred route | ||
| Any route | 207 | 40.4 |
| Any form of injection | 152 | 29.6 |
| Oral drops/jet | 104 | 20.3 |
| Inhalation by nose | 42 | 8.2 |
| Skin patch | 8 | 1.6 |
| Preferred dose | ||
| Any number of doses | 167 | 32.6 |
| Four doses | 30 | 5.8 |
| More than four doses, but less than seven | 21 | 4.1 |
| Three doses | 165 | 32.2 |
| Two doses | 130 | 25.3 |
| Minimum acceptable effectiveness | ||
| More than 90% | 122 | 23.8 |
| 80-90% | 199 | 38.8 |
| 60-79% | 148 | 28.8 |
| 40-59% | 35 | 6.8 |
| Even below 40% | 9 | 1.8 |
| Least tolerable side effect for you | ||
| Fainting | 206 | 40.2 |
| Fatigue | 32 | 6.2 |
| Fever | 49 | 9.6 |
| Injection-site pain | 131 | 25.5 |
| Rash | 54 | 10.5 |
| Sleepiness | 41 | 8.0 |
| Acceptable adverse reaction | ||
| No risk is acceptable to me | 89 | 17.3 |
| Worse disease 1 in 100 vaccinated | 17 | 3.3 |
| Worse disease 1 in 1000 vaccinated | 19 | 3.7 |
| Worse disease 1 in 1000 vaccinated | 50 | 9.7 |
| Worse disease 1 in 1 lakh vaccinated | 141 | 27.5 |
| Worse disease 1 in 10 lakhs vaccinated | 197 | 38.1 |
| Preferred price for COVID vaccine | ||
| Will accept if it’s free | 80 | 15.6 |
| 100-500 INR | 197 | 38.4 |
| 500-2000 INR | 188 | 36.6 |
| Will take even if >2000 INR | 48 | 9.4 |
| Preferred place where you like to get it | ||
| Anywhere | 90 | 17.5 |
| From any health facility | 276 | 53.8 |
| From our house physician | 45 | 8.8 |
| Through campaign | 41 | 8.0 |
| At our home, by a trained person | 42 | 8.2 |
| Self-administration | 19 | 3.7 |
| If required, will you take the vaccine every year | ||
| No | 125 | 24.4 |
| Yes | 388 | 75.6 |
| Have you taken yearly flu vaccine | ||
| Never | 316 | 61.6 |
| Once | 81 | 15.8 |
| Occasionally | 91 | 17.7 |
| Regularly, each year | 25 | 4.9 |
| Is your child immunized | ||
| Yes, fully vaccinated as per age | 297 | 57.9 |
| Missed some doses | 12 | 2.3 |
| No, don’t believe in vaccines | 3 | 0.6 |
| I have no kid | 201 | 39.2 |
| Would you volunteer for human challenge study | ||
| No | 316 | 61.6 |
| Yes | 197 | 38.4 |
| Who should get the vaccine first | ||
| Healthcare workers | 261 | 50.9 |
| Elderly | 48 | 9.4 |
| People with diseases like diabetes | 59 | 11.5 |
| Children less than five | 37 | 7.2 |
| Essential service | 27 | 5.3 |
| Everyone should get at same time | 81 | 15.8 |
Table 3 shows associations of COVID-19 vaccine acceptance response with demographic factors. It was seen that lower age, females, Hindu by religion, secondary or higher educated, currently not married and students would accept the vaccine most in their categories if offered to them. It was observed the participants who were of lower age, Hindu by religion, currently not married and students were significantly associated with being more acceptable to COVID-19 vaccine uptake.
Table 3.
Associations of vaccine acceptance response with sociodemographic factors
| Variables | Vaccine acceptance response | P | ||
|---|---|---|---|---|
| Will accept | Not yet decided | Refuse | ||
| Age | ||||
| <35 | 227 (84.7%) | 26 (9.7%) | 15 (5.6%) | F=14.93 |
| 35-54 | 160 (74.8%) | 26 (12.1%) | 28 (13.1%) | P=0.004 |
| ≥55 | 21 (67.7%) | 8 (25.8%) | 2 (6.5%) | |
| Gender | ||||
| Male | 200 (76.6%) | 31 (11.9%) | 30 (11.5%) | F=6.142 |
| Prefer not to say | 3 (75.0%) | 1 (25.0%) | 0 (0%) | P=0.151 |
| Female | 205 (82.7%) | 28 (11.3%) | 15 (6.0%) | |
| Religion | ||||
| Hindu | 282 (83.4%) | 33 (9.8%) | 23 (6.8%) | F=15.565 |
| Muslim | 102 (75.0%) | 16 (11.8%) | 18 (13.2%) | P=0.003 |
| Others | 24 (61.5%) | 11 (28.2%) | 4 (10.3%) | |
| Education | ||||
| Illiterate | 4 (66.7%) | 1 (16.7%) | 1 (16.7%) | F=6.214 |
| Primary | 5 (62.5%) | 3 (37.5%) | 0 (0.0%) | P=0.296 |
| Secondary | 38 (84.4%) | 4 (8.9%) | 3 (6.7%) | |
| College | 361 (79.5%) | 52 (11.5%) | 41 (9.0%) | |
| Marital status | ||||
| Married | 219 (74.0%) | 44 (14.9%) | 33 (11.1%) | χ2=13.220 |
| Current not married | 189 (87.1%) | 16 (7.4%) | 12 (5.5%) | P=0.001 |
| Occupation | ||||
| Healthcare worker | 164 (74.9%) | 26 (11.9%) | 29 (13.2%) | χ2=20.925 |
| Others | 107 (78.1%) | 18 (13.1%) | 12 (8.8%) | P=0.001 |
| Student | 109 (91.6%) | 8 (6.7%) | 2 (1.7%) | |
| Unemployed | 28 (73.7%) | 8 (21.1%) | 2 (1.7%) | |
Discussion
This study is first of its kind done in India with the objective to assess the knowledge, preferences, expectations and apprehensions about the probable vaccine for COVID-19 among residents of Delhi. It was observed that overall participants were quite aware about the COVID-19 vaccine and likely to get a vaccine if it were available.
Among the respondents, 79.5% were willing to accept the COVID-19 vaccine if it is available, 11.7% were not sure at the time of survey while 8.8% refused to take it. This acceptability rates in our study are higher in comparison to previous researches from other developing as well as developed countries. A study from Nigeria reported acceptability at 29%, in Saudi Arabia it was 65%, in Indonesia it varied between 67% and 93%, while in China it was 72.5% among the general population.[8,9,10,11] Among developed countries, a study in the United States reported 67% would accept a COVID-19 vaccine, while researchers in France documented about 25% of respondents would not use the vaccine when it is available.[12,13,14] The scepticism was also reported in Larson's Vaccine confidence Project which documented one-fifth of Swiss and 18% of French would refuse a COVID-19 vaccine.[14] In a US poll, only half of the people said they will take a COVID-19 vaccine and 20% turned it down, while in a UK poll, the refusal rate was about one in six.[15,16] A multicentric study conducted in seven European countries found acceptance rate at 73.9%, while 7.2% desired not to get vaccinated.[17] In June 2020, Lazarus et al.[18] surveyed 13,426 people in 19 countries to determine potential acceptance rates and factors influencing acceptance of a COVID-19 vaccine. Of these, 71.5% of participants reported that they would be very or somewhat likely to take a COVID-19 vaccine. In a systematic search of the 31 peer-reviewed studies which assessed COVID-19 vaccine acceptance rates from 33 different countries, it was found that amongst the adults representing the general public, the highest COVID-19 vaccine acceptance rates were found in Ecuador (97.0%), Malaysia (94.3%), Indonesia (93.3%) and China (91.3%). However, the lowest COVID-19 vaccine acceptance rates were found in Kuwait (23.6%), Jordan (28.4%), Italy (53.7), Russia (54.9%), Poland (56.3%), the United States (56.9%) and France (58.9%). Only eight surveys among healthcare workers (doctors and nurses) were found, with vaccine acceptance rates ranging from 27.7% in the Democratic Republic of the Congo to 78.1% in Israel. In the majority of survey studies among the general public stratified per country (29/47, 62%), the acceptance of COVID-19 vaccination showed a level of ≥70%. Low rates of COVID-19 vaccine acceptance were reported in the Middle East, Russia, Africa and several European countries.[19] Another recent multicentric Ipsos survey, conducted on behalf of the World Economic Forum, observed that overall three quarters of adults agreed to get vaccinated when available.[20] In the same survey, India with 87% acceptance rate was among countries where COVID-19 vaccination intent is highest.[20] The higher acceptability in the study reflects good public confidence in COVID-19 vaccine. It may be due to many reasons which are seen in Indian subcontinent. First, the overall immunization coverage and vaccine acceptability in Indian is higher due to efforts of government of India in collaboration with UNICEF and GAVI in providing free as well as universal vaccination. Second, the misinformation being spread by the Anti-Vaxx movement prevalent in developed countries is not so common in India.[21] While good acceptance rate in our study depicts the positive attitudes towards a vaccine in India, we should also pay attention to portion who have not yet decided. These are the potential candidates for intervention for increasing vaccination acceptance among community.
In regards to factors effecting vaccine acceptance, it was observed the future COVID-19 vaccine acceptance was relatively higher among younger age group (84.7% among 34 or lower), females (82.7%), currently not married (87.1%), students (91.6) and participants with secondary education level (84.4%). Except gender and education level, all these associations were significant in statistical analysis. These finding were in contrast to study from the United States and Saudi Arabia where they observed acceptance higher among older adults.[19,20] Apart from different demography, social structure and political engagement, the vaccine acceptance was also different from our study, leading to different findings.
In the study, it was observed that people have mixed expectation from the research team working on COVID-19 vaccine candidates. While the Indian Council of Medical Research claimed of early release of vaccine, it created doubts and pessimistic views of people about its efficacy and safety.[22] Although the respondents had been eagerly waiting for vaccine, they knew that it would be far from the perfect one. Most of them desired not to volunteer to participate in ‘human challenge’ study which could accelerate its development. More than half were in the view that vaccine would provide lifelong immunity and it would not be sufficient for everyone when it will be available. About one-third said it would not protect all alike, while some of the respondents were searching alternatives to vaccine in homeopathy (12.3%) and Ayurveda (16.4%). Perception that vaccine would not be sufficient for everyone and may not protect all with lifelong immunity could affect the vaccine acceptance rate in community. Although we observed handful proportion of sample searching alternatives to vaccine, a recent report by Wellcome Trust observed that almost all Indian (98%) agree that vaccines are important for children.[23]
Almost one-third were willing to have any number of doses, while other one-third were only willing to take a maximum number of three doses. The least accepted side effect for the participant was fainting (40%). This finding is important concern for vaccine candidate profile because it has been documented that most common reason for not getting COVID-19 vaccine was concerned about potential side effects.[17,20] Almost two-fifth would immunize themselves only if the vaccine is at least 80–90% efficacious while rest one-fourth opt for at least 60% efficacy. Similarly, a study from Indonesia reported 93.3% of respondents agreed for vaccination with 95% effective vaccine, but 67.0% accepted for a vaccine with 50% effectiveness.[24]
Most of them were willing to take the vaccine every year and would pay for it too. Almost same proportion of respondent were willing to pay Rs. 100–500 and between Rs. 500 and 2000 from their pocket for the vaccine, while about 16% would be vaccinated only if it was provided for free. These are similar to the findings from other developing countries.[24]
More than half of the respondents said that they would like to get the COVID-19 vaccine from any health facility. Utilizing existing vaccine-distribution infrastructure is also a preferred approach in planning COVID-19 vaccine distribution. Indians have good trust in doctors and health system as reported by recent report by Welcome Trust.[23] This is predominantly due to large numbers of community health workers which again build the confidence of community in the health system. This would be helpful in planning COVID-19 vaccination. The participants were aware that healthcare workers are the most at-risk population for getting COVID-19, more than half advocated that healthcare workers should get the COVID-19 vaccines first, while there were few who said that the vaccine should be given to all at the same time. As a low-middle-income country with limited health budget, India cannot run the rat race of vaccine nationalism where developed countries are hedging their bets to secure potential vaccine supplies to their citizen; our focus should be on establishing a framework for the equitable allocation of COVID-19 vaccines including prioritizing high-risk groups.[25]
Limitations: Only a subsample of the population could be included in the study. Large-scale studies from whole of India are needed to understand the knowledge, expectation and apprehension for the vaccine. Another limitation of the study was that it did not have equal representative from various economic and occupational strata of society which could bias the result.
Conclusion
The study shows that COVID-19 vaccine hesitancy which is currently the concern in other countries is not an issue in India. Also with the launch of vaccine, vaccine misinfodemics will have to be tackled. Primary care physicians will also play a big role in prevention of COVID-19 by providing proper knowledge regarding COVID-19 vaccine and can help in breaking the vaccine hesitancy; this will help to improve the uptake of COVID-19 vaccine and will lead to overall immunization programme strengthening, with scientific evidences, clear and consistent communication and improved health literacy of both the community as well as the service providers.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.WHO Coronavirus Disease (COVID-19) Dashboard [Internet] [Last accessed on 2020 Nov 17]. Available from: https://covid19.who.int .
- 2.Govt of India COVID-19 Dashboard [Internet] [Last accessed on 2020 Nov 17]. Available from: https://www.mohfw.gov.in .
- 3.GRID COVID-19 Study Group. Combating the COVID-19 pandemic in a resource-constrained setting: Insights from initial response in India. BMJ Glob Health. 2020;5:e003416. doi: 10.1136/bmjgh-2020-003416. doi: 10.1136/bmjgh-2020-003416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Office USGA. Artificial intelligence in health care: Benefits and challenges of machine learning in drug development [Reissued with revisions on Jan. 31, 2020.] [Last accessed on 2020 Nov 17]. 2020, Jan 21, (GAO-20-215SP) Available from: https://www.gao.gov/products/GAO-20-215SP .
- 5.COVID vaccine excitement builds as Moderna reports third positive result. [Last accessed on 2020 Nov 17]. Available from https://www.nature.com/articles/d41586-020-03248-7 . [DOI] [PubMed]
- 6.Harapan H, Fajar JK, Sasmono RT, Kuch U. Dengue vaccine acceptance and willingness to pay. Hum Vaccin Immunother. 2016;13:786–90. doi: 10.1080/21645515.2016.1259045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Streefland P, Chowdhury AM, Ramos-Jimenez P. Patterns of vaccination acceptance. Soc Sci Med. 1999;49:1705–16. doi: 10.1016/s0277-9536(99)00239-7. [DOI] [PubMed] [Google Scholar]
- 8.Fu C, Wei Z, Pei S, Li S, Sun X, Liu P. Acceptance and preference for COVID-19 vaccination in health-care workers (HCWs) medRxiv. doi: https://doi.org/10.1101/2020.04.090.20060103. [Google Scholar]
- 9.Reuben RC, Danladi MM, Saleh DA, Ejembi PE. Knowledge, attitudes and practices towards COVID-19: An epidemiological survey in North-Central Nigeria? J CommunityHealth. 2020;7:1–14. doi: 10.1007/s10900-020-00881-1. doi: 10.1007/s10900-020-00881-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harapan H, Wagner AL, Yufika A, Winardi W, Anwar S, Gan AK, et al. Acceptance of a COVID-19 vaccine in Southeast Asia: A cross-sectional study in Indonesia. Front Public Health. 2020;8:381. doi: 10.3389/fpubh.2020.00381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Padhi BK, A. Almohaithef M. Determinants of COVID-19 vaccine acceptance in Saudi Arabia: A web-based national survey. medRxiv. doi: 10.2147/JMDH.S276771. doi: https://doi.org/10.1101/2020.050.27.20114413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Malik AA, McFadden SM, Elharake J, Omer SB. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020;26:100495. doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ward J, Alleaume C, Peretti-Watel P COCONEL Group. The French public's attitudes to a future COVID-19 vaccine: The politicization of a public health issue. Soc Sci Med. 2020;265:113414. doi: 10.1016/j.socscimed.2020.113414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gellin B. Why vaccine rumours stick—and getting them unstuck. Lancet. 2020;396:303–4. [Google Scholar]
- 15.Expectations for a COVID-19 Vaccine. AP-NORC. [Last accessed on 2020 Nov 17]. Available from: https://apnorc.org/projects/expectations-for-a-covid-19-vaccine/
- 16.You Gov & Centre for Countering Digital Hate (CCDH) Survey results. 2020. [Last accessed on 2020 Aug 10]. Available from: https://docs.cdn.yougov.com/5mkju0kxbj/CCDH_RESULTS_062620_PR%20%28002%29.pdf .
- 17.Neumann-Böhme S, Varghese NE, Sabat I, Barros PP, Brouwer W, van Exel J, et al. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur J Health Econ. 2020;21:977–82. doi: 10.1007/s10198-020-01208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2021;27:225–8. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sallam M. COVID-19 vaccine hesitancy worldwide: A concise systematic review of vaccine acceptance rates. Vaccines (Basel) 2021;9:160. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Global Attitudes on a COVID-19 Vaccine.pdf. [Last accessed on 2020 Nov 17]. Available from: https://www.ipsos.com/sites/default/files/ct/news/documents/2020-09/global-attitudes-on-a-covid-19-vaccineipsos-survey-for-wef-2020.pdf .
- 21.Burki T. The online anti-vaccine movement in the age of COVID-19. Lancet Digit Health. 2020;2:e504–5. doi: 10.1016/S2589-7500(20)30227-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Coronavirus vaccine: ICMR plans August 15 launch for COVAXIN-The Week. [Last accessed 2020 Nov 17]. Available from: https://www.theweek.in/news/health/2020/07/03/coronavirusvaccine-icmr-plans-august-15-launch-for-covaxin.html .
- 23.Well come-global-monitor-2018.pdf. [Last accessed on 2020 Nov 17]. Available from: https://wellcome.org/sites/default/files/wellcome-global-monitor-2018.pdf .
- 24.Harapan H, Wagner AL, Yufika A, Winardi W, Anwar S, Gan AK, et al. Willingness-to-pay for a COVID-19 vaccine and its associated determinants in Indonesia. Hum Vaccin Immunother. 2020;16:3074–80. doi: 10.1080/21645515.2020.1819741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fidler DP. Vaccine nationalism's politics. Science. 2020;369:749. doi: 10.1126/science.abe2275. [DOI] [PubMed] [Google Scholar]