Abstract
Background:
Health can be defined as more than an absence or lack of disease. It is generally related to personal, physical, social, along with spiritual wellness. However, the importance of good health is comparable with a progressive physical and cognitive limitations due to aging and hence, its clear definition is not possible. Hence, most of the important aims or goals in aging are unrelated to finding a cure but rather toward achieving an optimal function. Thus, a healthy aging process that encompasses physical, mental, psychological, and spiritual well-being is always much desired.
Aim and Objectives:
The aim and objective of this study is to assess the oral health status and degree of cognitive impairment along with dementia, if present.
Materials and Methods:
This is a prospective and cross-sectional analysis comprising of 300 study participants of which 150 are males while 150 are females. Cognitive ability is assessed using the Standardized Mini-Mental State Examination (SMMSE) scoring test. A score value lesser than or equal to 23 is considered as low, whereas a score of 24 and above represents normal cognitive abilities. Subjects with low score are selected for the study. Oral health status is assessed by examining a) total numbers of teeth present; b) presence or absence of denture use; and c) capacity for masticatory or chewing ability (recorded as yes or no). Demographic variables parameters include age, gender, and presence of smoking habit. Clinical parameters or variables are analyzed by employing the independent t-test and Chi-square test. Pearson's correlation analysis is used to test a correlation between impairment of cognitive capacity, oral health status, masticatory capability, and use of dentures, if present. Two-tailed t-test is used to derive a P value for significance.
Results:
The total numbers of teeth present are significantly correlated with a lower SMMSE score (R = + 0.56; P = 0.03) while a significant association is noted between ability for mastication and lower SMMSE score (P = 0.05).
Conclusion:
This study concluded that loss of cognition or dementia is closely related to a poor oral health status.
Keywords: Cognitive, dementia, elders, oral health, teeth
Introduction
Oral health-related quality-of-life (QoL) is a subjective measure used for assessment of an individual's perception regarding oral health status. Alzheimer's disease is a disorder with neurodegenerative changes. It accounts for 60% to 80% of all dementia conditions affecting the elderly population.[1] Its pathophysiology is associated with the extracellular deposition of amyloid-β protein products in brain. This results in disruption of synaptic transmission and hyperphosphorylation of “tau” protein, which causes intracellular entanglement of neurofilaments. The pathophysiological alterations result in loss of nerves and continuous atrophy in cortex of brain. As the disease progresses, there is an increase in impairment of morbidities related to this disease, which is expressed as loss of physical and cognitive ability in day-to-day or routine activities. Dementia can be defined as a “disease which causes the loss of functioning of cognition and interference with ability in performing daily life activities and participation in social activities. It is an autosomal dominant trait that accounts for 60%–70% of disease etiology.”[2] It is an umbrella terminology employed for symptoms affecting a patient's cognitive function. Its clinical manifestations include impairment or loss of memory, alterations in capacity of thinking, reduced focus, and poor judgment skills and reasoning capacity.
QoL has been described by the World Health Organization as a subject's perception of their oral health. This has a significant relation to overall QoL in patients with limitations on neuromuscular and cognitive capabilities; maintenance of oral health becomes a challenging task. Due to this, maintenance of oral hygiene becomes equally challenging resulting in dental caries and periodontal disease leading to loss of teeth. This can significantly compromise the masticatory efficiency as well as speech, therefore affecting one's social life and nutritional status. Thus, a decrease in oral health status-related QoL and concomitant significant deterioration in an individual's cognitive functioning takes place. Thus, the use of indicators for a measurement tool helps in assessing an individual's satisfaction. Various tools have been used to assess such changes in the geriatric population. One such tool is the “Geriatric Oral Health Assessment Index,” which has been widely validated. This analytical tool provides a sustainable and reliable measurement of perception of oral health-related QoL in terms of function, presence, or absence of morbidities inducing pain along with significant discomfort. Assessment of oral health includes measuring function, pain, impact on psychological status, and impairment in social life and related handicap.[1] Over many years, due to the availability of better treatment options, the teeth are retained in the older age groups. Thus, the incidence of oral health-related issues is also increasing steadily as an individual crosses over into the geriatric age group range.[3]
The diagnosis of dementia has been associated with discontinued dental clinic visits that accumulate to result in poor oral health. Subjects suffering from mixed type of dementia or Parkinsonism with dementia or severe and rapid impairment of cognitive functions show significant decrease in utilization of dental care services. Poor dental and oral health status adversely impacts nutritional status and speech patterns. These abnormalities can further cause worsening of cognitive and general physical health in patients suffering from dementia. Additionally, it has been shown that elderly patients suffering from dementia when living on their own, tend to neglect their oral health more frequently.[4,5,6]
Incidence of dementia worldwide approximately 7.7 million cases per year, i.e., there is one newly diagnosed case at every 4-second interval. Dementia is often associated with problems related to behavior, for example, aggressiveness and combative nature. This may results in difficulty in providing oral healthcare by dental healthcare professionals. Thus, it is quite clear that oral health status in these patients may be improved by educating the healthcare providers with the knowledge pertaining to such subjects.[7]
Decrease in cognitive functioning is seen in older-aged patients. It is considered an early presentation of progressive dementia disorders. Poor oral health risk increases with an increase in disease score related to cognitive functioning. Loss of cognitive functioning may be governed by level and quality of education and socioeconomic status. Utilization of dental care services acts as a moderating factor between cognition and oral health status.[8] Most of the oral and dental health problems can be prevented if they are detected at an early stage and are usually not age-related. These are comprised of usually the plaque-associated diseases like dental caries and periodontal diseases, which can be prevented through early intervention. Although this oral condition does not directly result in any morbidity, but can significantly hamper the management on a variety of medical conditions. For example, the chronic inflammatory process in periodontal disease increases the risk of cardiovascular complications leading to cardiac arrest and sometimes a stroke.[9,10,11,12]
Oral mucosal lesions are frequently reported in elder population. Among these, denture-associated lesions such as angular cheilitis, stomatitis, ulcerations, and candidiasis are most commonly seen. In instances where there is reduction in cognitive abilities along with reduction in self-care, these lesions may get worsened in their manifestations.[13,14]
As per the United Nations, number of individuals over 60 years will constitute 32% of entire world population across the globe, by the middle of 21st century. Since there is no known cure for uncognitive function or dementia, an understanding related to early decline in symptoms and other diseases is important.[15]
Based upon the above background, the aim of the study was to assess the oral health status and treatment needs in geriatric patients with varying degrees of impairment in cognitive function and dementia.
Materials and Methods
Study Design
This prospective, cross-sectional study comprised of 300 geriatric patients of which 150 were males while 150 were females. Inclusion criteria of the study was 1) all study participants were 60 years and above; 2) informed written consent was to be obtained after explaining the study objectives in the native and easily understandable language; and 3) individuals were clinically diagnosed with dementia or similar neurodegenerative disorder. Exclusion criteria of the study were 1) subjects with diseases or any systemic disorders which might interfere with assessment of psychometric functions like inability to hear properly, blindness, and terminal illness; 2) any past episodes of depression; and 3) medical history of a cardiovascular event or stroke.
Criteria for Measurement
Assessment of cognitive mental capacity: The Standardized Mini-Mental State Examination (SMMSE) test was used to measure a subject's cognitive functioning. It analyzed the degree of orientation, capability of retaining short-term memory, use of language, comprehension skills, and registration and basic motor skills. Scoring was performed as under a) score of less than or equal to 23 was considered as low and b) score of 24 and above represented normal cognitive ability.
Assessment of parameters dealing with oral health: Oral health was assessed by judging a) total number of teeth present; b) presence or absence of denture use; and c) capacity for mastication or chewing ability which was recorded as yes/no.
Other variables that were recorded included collection of data pertaining to demographic characteristics which comprised of age, sex, level of education, and any life-style changes such as presence of smoking habit and alcohol consumption.
Statistical Analysis
Statistical analysis was performed by utilizing the SPSS version 24.0. All clinical parameters were analyzed by using the independent t-test and the Chi-square test. Pearson's correlation analysis was employed to test any correlation between impairment of cognitive capacity, oral health status, masticatory capability, and presence or absence of dentures. The two-tailed t-test was used to derive the P value or significance in which values lower than 0.5 was set as statistically significant.
Ethical approval
This study was conducted in compliance with the protocol; ethical approval was obtained from the Institutional ethical committee (EE/088/21) dated 08/01/2019.
Results
The study participants were categorized into two broad groups depending on their score through SMMSE measurement tool. Demographic data have been depicted in Table 1 while the variables related to oral health and low SMMSE test score are demonstrated in Table 2. Graph 1 demonstrate SMMSE score and oral health status in individuals with cognitive function loss and dementia.
Table 1.
Demonstrating demographic data collected in the study
| Male participants (n=150) | Female participants (n=150) | Low SMMSE score | Pearson’s r | Obtained P | |
|---|---|---|---|---|---|
| Age | 68.2±4.4 | 65.3±3.2 | 74.2±10.2 | -0.345 | 0.06 |
| Education | 0.5 | 0.001 | |||
| Uneducated | 30.3±8.2 | 35.4±6.1 | 54.8±6.2 | ||
| Educated | 69.7±2.4 | 64.6±3.2 | 32.1±2.5 | ||
| Positive history of smoking habit | 22% | 15% | 0.2 | 0.11 | 0.5 |
Table 2.
Oral health status and low Standardized Mini-Mental State Examination score
| Male participants | Female participants | Low SMMSE score | Pearson’s r | Obtained P | |
|---|---|---|---|---|---|
| Remaining teeth | |||||
| 0-10 | 15% | 10% | 87.2 | 0.56 | 0.03 |
| 11-21 | 47% | 49% | 55.5 | ||
| 22-32 | 55% | 58% | 37.2 | ||
| Masticatory efficiency | |||||
| Impairment | 25.2% | 79.1% | - | 0.4 | 0.05 |
| Competence | 62.4% | 46.2% |
Graph 1.
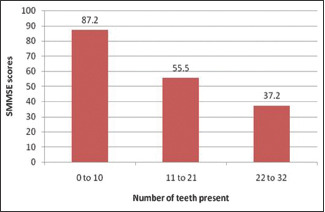
Graph demonstrating SMMSE score and oral health status in individuals with cognitive function loss and dementia
On applying statistical tools, it was seen that the number of teeth present was significantly correlated with lower SMMSE score (R = +0.56; P = 0.03) while a significant association was noted between ability for mastication and lower SMMSE score (r = 0.4; P = 0.05) with 62.4% and 46.2% of males and females exhibiting masticatory competency, respectively, while 25.2% and 79.1% of male and female study participants demonstrating impaired mastication [Table 2]. However, no significance was noted between use of denture in either males or females and low SMMMSE score (P = 0.7).
Discussion
Cognitive impairment (CI) has been found to be common among older aged adult population. It is of common observation that as a person suffers from impairment of cognitive abilities, and their dependence on other individual increases with decline in overall oral health.[16] Recent years have shown growing numbers of analytical studies that have been primarily done in developed nations to be focused upon the relationship between oral health and dementia or progressive cognitive decline. However, few studies have also shown a negative relationship between oral health status and cognitive disease or dementia. Most of the studies have used the baseline number of teeth to predict dementia reporting at an early stage or a late onset or progressive decline in cognition. Hence, the number of teeth has been typically coded as one of the categorical variables which can be assessed by means of various studies. In our study also, the number of teeth present at the time of measurement of dementia and cognitive disability has been used as an indicator of oral health status.
Dementia is a clinical syndrome resulting in loss of intellectual capability and is common among the elderly population. Because of impaired memory and disturbed executive functioning, patients often have difficulty in performing oral hygiene practice and are at high risk of dental caries and periodontal diseases. Dental healthcare practitioners can formulate effective strategies for the elderly patients to reduce their risk of dental diseases. One of these strategies is to integrate 5S into oral hygiene practice. It includes i) sorting to remove unnecessary items, ii) setting-in-order to place the items in order of flow, iii) maintenance of the environment, iv) standardizing to establish discipline for good oral hygiene habits, and v) sustaining to keep 5S going by auditing and improving the environment and oral hygiene practice.[17]
Current study observations have demonstrated that a low SMMSE score, which is an assessment of cognitive ability, is associated with less numbers of teeth present in elderly patients with dementia or cognitive dysfunction. Also, a statistically significant difference was observed between masticatory capacity efficiency among male and female study participants in individuals with cognitive disabilities and dementia. Our findings were supported by Wu et al. who demonstrated that the older individuals suffering from lower cognitive function scores demonstrate higher deterioration in oral health in terms high periodontitis and dental caries scores.[18]
In our study, no significant association was found between association between smoking habit and low SMMSE score or dementia. Our finding is supported by Lee et al. who found in their observation analysis that the risk of dementia is highest in the upper middle socioeconomic group and also, the rural population. They also found that individuals who smoke and consume alcohol were less likely to develop dementia. Also, diabetic patients were observed to suffer from dementia when compared to those with hypertension.[2]
Martande in their observational study found that periodontal disease increased in severity with deteriorating cognitive functioning.[19]
Lopez-Jornet et al. conducted a case control study to evaluate the effect of dementia on oral health. It was observed that the patients with more severe disease were significantly more likely to have fewer natural teeth, a higher plaque index, and a greater bleeding index than the control group. It was suggested that elder adults suffering with dementia had deficient oral health status.[20]
Chen et al. evaluated the oral hygiene among the elderly patients and investigated the possible factors associated with oral health and the effect of CI on it in geriatric care facilities (GCF). It was concluded that oral health status among aged residents in GCFs was worse among individuals with CI.[21]
Similarly, observations derived from various studies have demonstrated high oral disease rates due to dysfunction in salivary glands resulting in periodontal and dental caries in subjects suffering from dementia when compared to normal subjects.[22,23,24,25] It was opined by Singhrao et al. that the periodontal pathogen, Porphyromonas gingivalis, bears a direct link between periodontal disease and Alzheimer's disease due to inflammation causing potential development of neurodegenerative disease process.[26] However, it is unclear if oral health status in geriatric population results in impairment in cognitive functions.[27]
Lauritano et al. studied the prevalence and the characteristics of oral pathology in a demented elderly population and further evaluated the association between different degree of dementia and the oral health condition in each patient. It was found that in elderly patients with dementia, the prevalence of bone resorption was greater than the prevalence of periodontal disease and the persisting mucosal lesions.[28]
Maeda et al. conducted a retrospective observational study on geriatric patients and assessed the nutritional status, daily working activities, CI, and comorbidities. It was observed that the poorest oral health at admission was related to old age, malnutrition, decreased activities of daily living (ADL), and impaired cognition. Poor oral health in older adult patients at the time of hospitalization was associated with in-hospital mortality.[29]
Implications for Clinical Practice
The deterioration of cognitive functions and that of motor and communication skills in dementia patients makes the correct execution of daily oral hygiene maneuvers difficult. The elderly with dementia may present behavioral disorders, with aggressive or opposing attitudes towards the medical–nursing staff of the residential care institutions thus preventing the possibility of being assisted. A common condition among subjects suffering from dementia is, therefore, a poor oral hygiene. It is therefore of primary importance to educate the nursing staff, in order to meet the special dental needs of patients with dementia.[28] Nursing staff should be well aware regarding possible strategies for oral health maintenance in patients with special needs in order to ensure adequate care.[30]
It has been observed that as a person's age advances, there is an increase in frequency and amount of sugar consumption. This factor greatly increases the risk of developing dental caries and which subsequently, leads to loss of teeth coupled with thus, most of the drugs prescribed cause reduction in flow of saliva, which additionally increases the risk of dental disease.[3]
Conclusion
There is a paucity of studies that have analyzed any association between loss of teeth and impairment in cognitive functions among Indian population. In our study, results have demonstrated that loss of teeth is an important risk factor for assessment of cognitive abilities or dementia. The results obtained from our study have shown that presence of more number of teeth is associated with better levels of cognitive functioning and the participants with less or few numbers of teeth show a much faster pace of loss of cognition among older Indian adult population, regardless of gender. These findings might have clinical impact on overall improvement in oral health status and regaining of cognitive functions and abilities. However, more studies are required to examine any link between loss in cognition and oral health status from analyzing more extensive clinical data.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ming Y, Hsu S-W, Yen Y-Y, Lan SJ. Association of oral health-related quality of life and Alzheimer disease: A systematic review. J Prosthet Dent. 2020;124:168–75. doi: 10.1016/j.prosdent.2019.08.015. [DOI] [PubMed] [Google Scholar]
- 2.Lee KH, Choi YY. Association between oral health and dementia in the elderly: A population-based study in Korea. Sci Rep. 2019;9:14407–15. doi: 10.1038/s41598-019-50863-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wyatt CCL, Kawato T. Changes in oral health and treatment needs for elderly residents of long-term care facilities over 10 years. J Can Dent Assoc. 2019;85:j7–13. [PubMed] [Google Scholar]
- 4.Fereshtehnejad SM, Garcia-Ptacek S, Religa D, Holmer J, Buhlin K, Eriksdotter M, et al. Dental care utilization in patients with different types of dementia: A longitudinal nationwide study of 58,037 individuals. Alzheimers Dement. 2018;14:10–9. doi: 10.1016/j.jalz.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 5.Marino RJ, Kan AR, Tham R, Khew CW, Stevenson C. Pattern and factors associated with utilization of dental services among older adults in rural Victoria. Aust Dent J. 2014;59:504–10. doi: 10.1111/adj.12216. [DOI] [PubMed] [Google Scholar]
- 6.Chen X, Clark JJ, Chen H, Naorungroj S. Cognitive impairment, oral self-care function and dental caries severity in community-dwelling older adults. Gerodontology. 205;;2:53–61. doi: 10.1111/ger.12061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Manchery N, Subbiah GK, Nagappan N, Premlatha P. The oral health education for caries effective in the oral hygiene management of elderly with dementia? A systematic review. Dent Res J (Isfahan) 2020;17:1–9. [PMC free article] [PubMed] [Google Scholar]
- 8.Chalmers JM, Carter KD, Spencer AJ. Oral health of Adelaide nursing home residents- A longitudinal study. Australias J Ageing. 2004;23:63–70. [Google Scholar]
- 9.Chelmers JM, Pearson A. Oral hygiene care for residents with dementia: A literature review. J Adv Nursing. 2005;52:410–9. doi: 10.1111/j.1365-2648.2005.03605.x. [DOI] [PubMed] [Google Scholar]
- 10.Niedzielka I, Janu T, Cierpka S, Swietochowska E. The effect of chronic periodontitis on the development of atherosclerosis: Review of literature. Med Sci Monit. 2008;14:RA103–6. [PubMed] [Google Scholar]
- 11.Mustapha IZ, Debrey S, Oladubu M, Ugarte R. Markers of systemic bacterial exposure in periodontal disease and cardiovascular disease risk: A systematic review and meta-analysis. J Periodontol. 2007;78:2289–302. doi: 10.1902/jop.2007.070140. [DOI] [PubMed] [Google Scholar]
- 12.Yao SG, Fine JB. Dementia and oral health: Is there a connection? Dent Open J. 2018;5:34–40. [Google Scholar]
- 13.Lauritano D, Moreo G, Vella FD, Stasio DD, Carinci F, Lucchese A, et al. Oral health status and need for oral care in an aging population: A systematic review. Int J Environ Res Public Health. 2019;16:4558–81. doi: 10.3390/ijerph16224558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Evan V, Staines K. Diagnosis and management of oral mucosal lesions for older people: A review. Rev Clin Gerodontol. 2008;18:115–28. [Google Scholar]
- 15.Seraj Z, Al-Najjar D, Akl M, Aladle N, Atlijaul Y, Zaki A, et al. The effect of number of teeth and chewing ability on cognitive function of elderly in UAE: A pilot study? Int J Dent. 2017;2017:5732748. doi: 10.1155/2017/5732748. doi: 10.1155/2017/5732748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Johnson VB, Schoenfelder DP. Oral hygiene care for functionally dependent and cognitively impaired older adults. J Gerodontol Nurs. 2012;38:11–20. doi: 10.3928/00989134-20121003-02. [DOI] [PubMed] [Google Scholar]
- 17.Gao SS, Chu CH, Young FYF. Integrating 5S methodology in to oral hygiene practice for elderly with Alzheimer's disease. Dent J (Basel) 2020;8:29. doi: 10.3390/dj8020029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu B, Plassman BL, Crout RJ, Liang J. Cognitive function and oral health among community dwelling older adults. J Gerodontol. 2008;63:495–500. doi: 10.1093/gerona/63.5.495. [DOI] [PubMed] [Google Scholar]
- 19.Martande SS. Periodontal health condition in patients with Alzheimer's disease. Am J Alzheimers Dis Other Demen. 2014;29:498–502. doi: 10.1177/1533317514549650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lopez-Jornet P, Zamora Lavella C, Pons-Fuster Lopez E, Tvarijonaviciute A. Oral health status in older people with dementia: A case-control study. J Clin Med. 2021;10:477. doi: 10.3390/jcm10030477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen L, Gu L, Li X, Chen W, Zhang L. Oral health matters in cognitive impaired aged residents in geriatric care facilities: A cross-sectional survey. Nurs Open. 2021;8:792–8. doi: 10.1002/nop2.683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ribeiro GB, Costa JL, Ambrosano GM, Garcia RC. Oral health of the elderly with Alzheimer's disease. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114:338–43. doi: 10.1016/j.oooo.2012.03.028. [DOI] [PubMed] [Google Scholar]
- 23.Ship JA. Oral health of patients with Alzheimer's disease. J Am Dent Assoc. 1992;123:53–8. doi: 10.14219/jada.archive.1992.0005. [DOI] [PubMed] [Google Scholar]
- 24.Ship JA, Puckett SA. Longitudinal study on oral health in subjects with Alzheimer's disease. J Am Geriatr Soc. 1994;42:57–63. doi: 10.1111/j.1532-5415.1994.tb06074.x. [DOI] [PubMed] [Google Scholar]
- 25.Jones JA, Lavallee N, Alman J, Sinclair C, Garcia RI. Caries incidence in patients with dementia. Gerodontol. 1993;10:76–82. doi: 10.1111/j.1741-2358.1993.tb00086.x. [DOI] [PubMed] [Google Scholar]
- 26.Singhrao SK, Harding A, Poole S, Kesavalu L, Crean SJ. Porphyromonas gingivalis periodontal infection and its putative links with Alzheimer's disease? Mediators Inflamm. 2015;2015:137357. doi: 10.1155/2015/137357. doi: 10.1155/2015/13757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nangle MR, Richer J, Grainger SA, Mancherry M, Sachdev PS, Henry JD. Oral health and cognitive function in older adults: A systematic review. Geriodontol. 2019;65:659–72. doi: 10.1159/000496730. [DOI] [PubMed] [Google Scholar]
- 28.Lauritano D, Moreo G, Carinci F, Borgia R, Lucchese A, Contaldo M, et al. Aging and oral care: An observational study of characteristics and prevalence of oral diseases in an Italian Cohort. Int J Environ Res Public Health. 2019;16:3763. doi: 10.3390/ijerph16193763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maeda K, Mori N. Poor oral health and mortality in geriatric patients admitted to an acute hospital: An observational study. BMC Geriatr. 2020;20:1–7. doi: 10.1186/s12877-020-1429-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yoon MN, Compton SM. Building professional competence in dental hygiene students through a community-based practicum. Int J Dent Hyg. 2017;15:e119–27. doi: 10.1111/idh.12233. [DOI] [PubMed] [Google Scholar]


