During the COVID-19 pandemic in King County, WA, declines were observed in both county sexually transmitted infection cases and sexual health clinic visits following stay-at-home orders in Washington.
Background
In response to the COVID-19 pandemic, Washington State's Stay Home, Stay Healthy (SHSH) order was implemented on March 24, 2020. We hypothesized that pandemic mitigation measures might reduce sexually transmitted infection (STI) screening and/or transmission.
Methods
We used King County, WA STI surveillance and sexual health clinic (SHC) data from January 1, 2019, to July 31, 2020. We calculated mean weekly case counts for gonorrhea, primary and secondary (P&S) syphilis, male urethral gonorrhea, and early latent (EL) syphilis for 3 periods in 2020: pre-SHSH (January 1–March 23), SHSH (March 24–June 5), and reopening (June 6–July 31). Primary and secondary syphilis and male urethral gonorrhea were used as proxies for sexual behavior, and EL syphilis was used as a proxy for STI screening. We compared SHC visits (2019 vs. 2020) and SHC gonorrhea treatment practices (across 2020 periods).
Results
Compared with January to July 2019, from January to July 2020, reported cases of gonorrhea, male urethral gonorrhea, P&S syphilis, and EL syphilis decreased by 9%, 5%, 16%, and 22%, respectively. Mean weekly case counts of gonorrhea, male urethral gonorrhea, and EL syphilis decreased pre-SHSH to SHSH, but all returned to pre-SHSH levels during reopening. Sexual health clinic visits during SHSH were 55% lower in 2020 than in 2019. In the SHC during SHSH, ceftriaxone treatment of gonorrhea decreased, whereas cefixime/cefpodoxime treatment and gonorrhea treatment with no testing increased.
Conclusions
Decreases in reported STIs concurrent with COVID-19 SHSH may reflect a true decline in STI transmission. However, the larger decreases in asymptomatic infections indicate that much of the observed decrease was likely due to decreased screening.
On January 20, 2020, the first SARS-CoV-2 infection diagnosed in the United States was reported in Everett, WA, in the Seattle metropolitan area.1 On February 29, 2020, first US death from SARS-CoV-2 occurred in King County, WA,2 and the governor declared a State of Emergency in Washington State.3 Pandemic mitigation measures went into place in King County soon after, with a ban on gatherings of more than 250 people announced March 11, 2020, and statewide school closures on March 13, 2020. The governor's Stay Home, Stay Healthy (SHSH) order for Washington State announced on March 23, 2020, mandated (1) Washington residents stay home except for essential activities; (2) a ban on gatherings for social, spiritual, and recreational purposes; and (3) the closure of restaurants, bars, gyms, bathhouses, sex clubs, and other businesses considered nonessential.4
Washington State implemented measures restricting nonurgent medical procedures in late February to conserve personal protective equipment, hospital beds, and health care personnel.5 Subsequently, the Public Health—Seattle & King County (PHSKC) Sexual Health Clinic (SHC) instituted changes to reduce the number of in-person patient visits, including deferring routine sexually transmitted infection (STI) screening, reducing hours, and conducting patient visits by telephone or telemedicine.6 Because the PHSKC prioritized COVID-19 control, public health staff from all sections of the health department, including the SHC, were deployed to assist with COVID-19 work. This reprioritization resulted in fewer partner services interviews for people newly diagnosed with STIs, limiting data collected about sexual behavior among reported cases.
Although we began to observe declining numbers of people newly reported with STI in King County as early as March 2020, it was unclear whether this was a result of changes in sexual behavior, reduced care-seeking behavior, or changes in STI care or diagnosis. To better understand the observed trends in STI reports, we conducted analyses to assess whether the trends in King County during the pandemic were the results of changes in sexual behavior or in STI screening practices. Our analyses included both asymptomatic and symptomatic infections as proxies for these screening and behavior changes. Washington State began to lift some pandemic mitigation measures in early June 2020, so we compared STI trends during the SHSH period (with the strictest measures) with those during the Safe Start reopening.7 This work adds to our understanding of the impacts of the COVID-19 pandemic on concurrent STI epidemics and informs future public health practice related to STIs if the pandemic and related mitigation efforts continue.
METHODS
We used STI surveillance data for King County, WA, from January 1, 2019, to July 31, 2020, and PHSKC SHC electronic medical record data for the same period. For both surveillance and clinic data, we compared 2020 with the same period in 2019. We also divided 2020 into 3 periods corresponding to prepandemic and the Washington State SHSH orders. The 3 periods were as follows: before the COVID-19 pandemic SHSH order (period 1: pre-SHSH; January 1–March 23), the period when the SHSH order was in effect in King County (period 2: SHSH; March 24–June 5), and the time after which components of the SHSH order were lifted in King County (period 3: Safe Start reopening; June 6–July 31).
Laboratories and medical providers are required to report gonorrhea and syphilis cases to the PHSKC within 3 days of diagnosis. The PHSKC STI case report form includes anatomic site of infection, demographics, diagnosis date, and treatment information. Syphilis stage is indicated by providers on the case report form but may be revised by PHSKC staff after review. We present data for cases of gonorrhea, urethral gonorrhea among men (defined by gender or sex reported on case report form), and syphilis presented as primary and secondary (P&S) syphilis, early latent or early nonprimary nonsecondary syphilis (EL), and early syphilis, which includes P&S and EL syphilis. Analyses of total early syphilis and gonorrhea cases were used to understand the overall reported STI trends. Primary and secondary syphilis and urethral gonorrhea cases among men,8,9 which are generally symptomatic infections, were used as proxies for changes in sexual behavior, whereas EL syphilis cases, an asymptomatic infection, was used as a proxy for changes in STI screening, due to either health care service availability or health care seeking behavior.
Sexual health clinic visits were conducted predominantly in-person before the coronavirus pandemic. In March 2020, clinic practices shifted to defer routine visits for HIV or STI screening of asymptomatic persons who did not have a known sex partner with HIV or STI. At this time, providers also began providing other services by telephone. In addition, routine in-person visits for patients receiving preexposure prophylaxis (PrEP) through the PHSKC SHC clinic were postponed or completed as telephone check-ins. The visit type (in-person vs. telephone) was not monitored prepandemic. Daily telephone and in-person visit numbers were tracked by clinic epidemiologists using the electronic medical record clinic schedule from the start of the telephone visit option in March 2020. We present data for the number of visits overall for 2019 and 2020. We present clinic visits with gonorrhea treatment indicated, including ceftriaxone, cefixime, and cefpodoxime, and visits with one of these treatments received and no corresponding gonorrhea test results for 2020 only. PHSKC SHC is a provider responsible for diagnosing a substantial number of King County STI cases, and visit trends can be used to assess changes in health care seeking behavior during the pandemic. Analyses were descriptive and completed with SAS version 9.4.10 This analysis was considered a public health surveillance activity and was not subject to human subjects review.
RESULTS
Compared with the same period in 2019, from January 1 to July 31, 2020, reported cases of gonorrhea (Fig. 1A), urethral gonorrhea among men (Fig. 1B), P&S syphilis (Fig. 1C), and EL syphilis (Fig. 1D) in King County, WA, all decreased (Table 1). Overall reported cases of gonorrhea decreased by 9% (n = 2683 vs. n = 2431), and urethral gonorrhea cases among men decreased by 5% (n = 961 vs. n = 915). Early syphilis cases overall decreased by 19% (n = 475 vs. n = 384), P&S cases decreased by 16% (n = 229 vs. n = 193), and EL cases decreased by 22% (n = 246 vs. n = 191).
Figure 1.
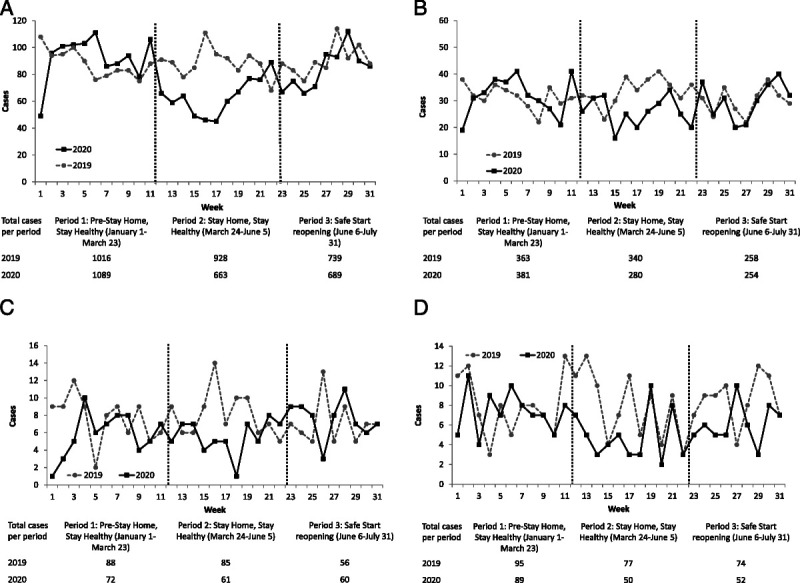
A, Weekly gonorrhea cases reported in King County, WA, comparing 2019 (dashed line) and 2020 (solid line) across 3 COVID-19 pandemic mitigation periods: prepandemic, stay-at-home order (Stay Home, Stay Healthy), and reopening (Safe Start). During Stay Home, Stay Healthy, gonorrhea cases in 2020 were lower than the same period in 2019. B, Weekly urethral gonorrhea cases among men reported in King County, WA, comparing 2019 (dashed line) and 2020 (solid line) across 3 COVID-19 pandemic mitigation periods: prepandemic, stay-at-home order (Stay Home, Stay Healthy), and reopening (Safe Start). During Stay Home, Stay Healthy, urethral gonorrhea cases in 2020 were lower than the same period in 2019 but had returned to same level in Safe Start. C, Weekly primary and secondary (P&S) syphilis, reported in King County, WA, comparing 2019 (dashed line) and 2020 (solid line) across 3 COVID-19 pandemic mitigation periods: prepandemic, stay-at-home order (Stay Home, Stay Healthy), and reopening (Safe Start). During Stay Home, Stay Healthy, P&S syphilis cases in 2020 were lower than the same period in 2019 but were slightly higher during Safe Start. D, Weekly early latent/early nonprimary nonsecondary syphilis reported in King County, WA, comparing 2019 (dashed line) and 2020 (solid line) across 3 COVID-19 pandemic mitigation periods: prepandemic, stay-at-home order (Stay Home, Stay Healthy), and reopening (Safe Start). During Stay Home, Stay Healthy, and Safe Start, early latent cases in 2020 were lower than the same period in 2019.
TABLE 1.
Reported Gonorrhea and Syphilis Cases and Visits to Public Health—Seattle & King County Sexual Health Clinic, King County, WA; January 1 to July 31, 2019 and 2020
| Period 1: Pre–Stay Home, Stay Healthy (January 1–March 23) | Period 2: Stay Home, Stay Healthy (March 24–June 5) | Period 3: Safe Start Reopening (June 6–July 31) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 2019 | 2020 | % Change | 2019 | 2020 | % Change | 2019 | 2020 | % Change | |
| Gonorrhea cases | 1016 | 1089 | 7 | 928 | 663 | −29 | 739 | 689 | −7 |
| Urethral gonorrhea cases among men | 363 | 381 | 5 | 340 | 280 | −18 | 258 | 254 | −2 |
| Primary and secondary syphilis cases | 88 | 72 | −18 | 85 | 61 | −28 | 56 | 60 | 7 |
| Early latent (early nonprimary nonsecondary) syphilis cases | 95 | 89 | −6 | 77 | 50 | −35 | 74 | 52 | −30 |
| Clinic visits | 2523 | 2249 | −11 | 2349 | 1068 | −55 | 1814 | 1203 | −34 |
From period 1 to period 2, in 2020, mean weekly gonorrhea and male urethral gonorrhea case counts fell from 92 to 60 and from 32 to 26, respectively (Fig. 2A). However, by period 3, the mean weekly gonorrhea case count was 84, similar to period 1, and the mean weekly male urethral gonorrhea count was the same as period 1. For P&S and EL syphilis in 2020 (Fig. 2B), trends were somewhat divergent. Mean weekly case counts for P&S syphilis remained stable from period 1 to period 2, and then rose slightly in period 3. Mean weekly EL syphilis case counts decreased from 7 in period 1 to 5 in period 2 but increased to 6 in period 3.
Figure 2.
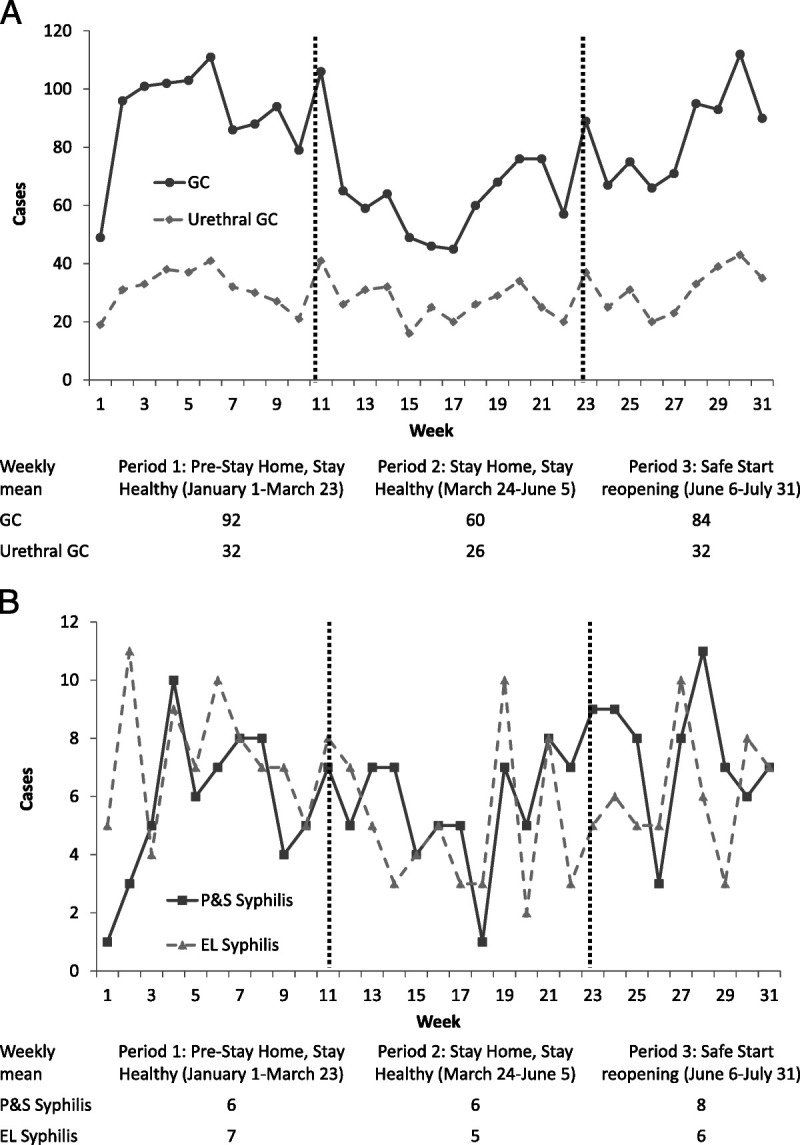
A, Weekly gonorrhea (solid line) and urethral gonorrhea cases among men (dashed line) reported in King County, WA, comparing 2020 across 3 COVID-19 pandemic mitigation periods: prepandemic, stay-at-home order (Stay Home, Stay Healthy), and reopening (Safe Start). During Stay Home, Stay Healthy, weekly mean gonorrhea and urethral gonorrhea cases among men significantly declined compared with prepandemic and were not significantly different in reopening compared with prepandemic. B, Weekly early syphilis, including primary, secondary, or early latent/early nonprimary nonsecondary syphilis (solid line), and early latent/early nonprimary nonsecondary syphilis (dashed line) reported in King County, WA, comparing 2020 across 3 COVID-19 pandemic mitigation periods: prepandemic, stay-at-home order (Stay Home, Stay Healthy), and reopening (Safe Start). During Stay Home, Stay Healthy, weekly mean early syphilis and early latent syphilis cases significantly declined compared with prepandemic and were not significantly different in reopening compared with prepandemic.
From January to July, the overall number of SHC visits was 32% lower in 2020 (n = 4720) than in 2019 (n = 6686; Fig. 3A). Although the decline in clinic visits in 2020 is evident before the official SHSH began, SHC visits in period 2 of 2020 (n = 1068) were 55% lower than the same period in 2019 (n = 2349). In period 3 (n = 1203), weekly clinic visits started to increase from period 2 but were still 34% lower than same period in 2019 (n = 1814). In period 2, 49% (n = 524) of SHC visits were telephone visits, which decreased to 4% (n = 51) in period 3.
Figure 3.
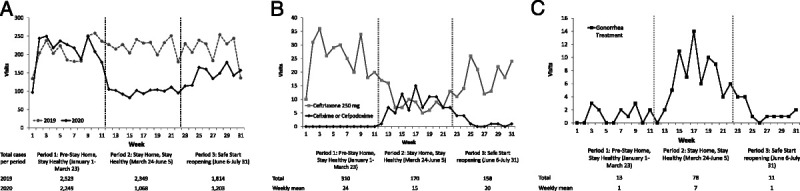
A, Weekly visits at the Public Health—Seattle & King County Sexual Health Clinic comparing 2019 (dashed line) and 2020 (solid line) across 3 COVID-19 pandemic mitigation periods: prepandemic, stay-at-home order (Stay Home, Stay Healthy), and reopening (Safe Start). During Stay Home, Stay Healthy, and Safe Start, clinic visits in 2020 were lower than the same period in 2019. B, Weekly visits with prescribed gonorrhea treatment at the Public Health—Seattle & King County Sexual Health Clinic comparing 2020 across 3 COVID-19 pandemic mitigation periods: prepandemic, stay-at-home order (Stay Home, Stay Healthy), and reopening (Safe Start). Because clinic policy changed during Stay Home, Stay Healthy, oral (black line) gonorrhea treatments (cefixime or cefpodoxime) increased in use and ceftriaxone (gray line) decreased. C, Weekly visits with prescribed gonorrhea treatment without laboratory testing at the Public Health—Seattle & King County Sexual Health Clinic comparing 2020 across 3 COVID-19 pandemic mitigation periods: prepandemic, stay-at-home order (Stay Home, Stay Healthy), and reopening (Safe Start). Because clinic policy changed during Stay Home, Stay Healthy, gonorrhea treatment without laboratory confirmation increased.
Weekly visits during which patients received gonorrhea treatment varied during the 2020 periods (Fig. 3B). In period 1, ceftriaxone was the only gonorrhea treatment used in the SHC, with no use of oral treatments (cefixime or cefpodoxime). In period 2, weekly visits (which included telemedicine visits) with prescribed oral gonorrhea treatment increased, accounting for 52% of visit with gonorrhea treatment and visits with patients receiving ceftriaxone decreased. As the reopening began in period 3, the trends in visits during which patients received ceftriaxone and oral treatments were reversed. Sexual health clinic visits with prescribed gonorrhea treatment without laboratory testing increased during period 2 compared with both period 1 and period 3 (Fig. 3C). In periods 1 and 3, the mean number of weekly visits during which patients received the treatment of gonorrhea with no gonorrhea testing was 1, whereas in period 2, the mean was 7.
DISCUSSION
During the first 4 months of the COVID-19 pandemic, we observed changes in reported gonorrhea and early syphilis cases in King County, WA, that suggested both changes in sexual behavior leading to reduced STI acquisition and changes in screening, likely due to lack of available services combined with declines in seeking health care services. In our analysis, we examined EL syphilis, an asymptomatic infection, to detect changes in screening patterns, and P&S syphilis and urethral gonorrhea infection among men, symptomatic infections to detect changes in recent sexual behavior. Compared with the prepandemic period in 2020 and the corresponding period in 2019, reported gonorrhea and early syphilis cases decreased during the SHSH period. However, behavioral changes may have been brief, as mean weekly cases of all STIs included in our analyses returned to levels observed during the prepandemic period during reopening. Larger differences from 2019 to 2020 were observed in EL syphilis, an asymptomatic infection, compared with P&S syphilis and urethral gonorrhea among men, typically symptomatic infections that lead patients to seek care. Observed declines in SHC visits in 2020 are largely explained by reduced clinical services, with the postponement of routine screening visits and limited PrEP visits, or reluctance to seek care at the SHC as observed in period 3, with visits still lower than expected after the expansion of clinical services. Along with our finding that EL syphilis cases showed the largest decline from 2019 to 2020, this further supports that the declines in STIs during the pandemic were largely influenced by declines in screening of asymptomatic infections.
Nationally, COVID-19 forced STD clinics to close or greatly reduce clinical capacity, especially for screening, and many reported changing the way services were offered, whether through increased telemedicine or moving to appointment only,11 or reduced numbers of visits.12 Increasing telehealth visits and continuing to provide care for symptomatic individuals are vital strategies for continuation of key sexual health services during times when other health services may be limited.13 At the PHSKC SHC, telephone visits increased to continue to provide STI care services at a distance.6
Changes to clinic policy during the pandemic affected both diagnosis and reporting of STI infections. Following the SHSH orders, treatment of gonorrhea with oral medications and presumptively treating patients for gonorrhea without laboratory testing increased at the SHC. Although presumptive treatment over the telephone is a safer option for continuing to provide STI clinical care during the pandemic, this may result in cases missed by county STI surveillance with no laboratory testing to confirm diagnoses. We are unable to assess whether other clinics providing STI treatment services were offering similar treatment options during this time and cannot quantify how many potential cases may have not been reported. Online surveys have documented the challenges patients have encountered accessing services, including impacting the ability of men who have sex with men (MSM) to access PrEP, STI, and HIV testing,14 but the pandemic has resulted innovative practices to provide sexual health services without requiring in-person visits, including mailing test kits to patients' homes.15,16
Similar decreases in reported STIs during stay at home orders have been observed in other jurisdictions in the United States,17–19 and the COVID-19 pandemic has impacted every aspect of STI diagnosis and control, including public health practices. Although King County typically has a robust behavioral surveillance framework in place, as in many other jurisdictions,11 PHSKC staff deployments to the COVID-19 response impacted the completion of partner services interviews for STI cases. Thus, we are not able to directly assess changes in sexual behavior between the 3 pandemic-related periods in 2020, hence our reliance on symptomatic infections as a surrogate marker. Although sexual behavior data were available for SHC patients for all 3 periods, changes to clinic policies and procedures made these data difficult to assess, as patients receiving services during the pandemic represent a different population than those in the prepandemic times. However, multiple surveys of MSM from around the world have shown reductions in number of sex partners during the COVID-19 pandemic, although reductions in sexual risk behaviors may have only been short lived during the early stages of the pandemic.14,20–23 It is unknown to what extent decreased partner services interviews will impact ongoing STI transmission in King County. Indeed, one study projected that long clinical service interruptions combined with a return to normal levels of sexual activity could result in thousands of excess STI cases over the next several years among MSM in Atlanta.24
The decreases in reported STIs we observed concurrent with COVID-19 social distancing polices may reflect some level of true decline in STI transmission. However, the impact of the COVID-19 pandemic on health care seeking behavior is unknown, and a limitation of our analysis is not being able to assess whether the continued decreased visits to the SHC were due to fewer patients with sexual health needs, patients seeking services from other providers, or avoiding seeking care because of potential COVID-19 exposure in a health care facility. Cases were likely underdiagnosed during this time because of a combination of these factors. As such, the impacts of the COVID-19 pandemic on STI epidemics are likely to be long lasting, as persons with undiagnosed STIs, especially those with asymptomatic infections, are likely to contribute to further STI transmission. In addition, deployment of clinicians and public health staff to COVID-19 activities may have slowed the process of case reporting in King County. However, at the end of our study period, COVID-19 cases were declining in King County, lessening the burden of this work somewhat at that time, and we feel that sufficient time has passed to allow all cases in the study period to be reported. Although this article was under review, we were able to examine trends for August to December 2020 and found that gonorrhea, urethral gonorrhea among men, EL syphilis, and SHC visits decreased by 10%, 11%, 20%, and 35%, respectively, compared with this period in 2019. Primary and secondary syphilis increased by 13% compared with 2019. Increased workloads and deployment of public health staff to the pandemic response present continued challenges to an already fatigued public health workforce. The impact of COVID-19 on public health is not limited to its direct impact on morbidity and mortality but will likely reverberate across multiple sectors of public health, including STI control, for many months or years to come.
Footnotes
Conflict of Interest and Sources of Funding: None were declared. Funding was received from STD Surveillance Network (CDC/NCHHSTP 1 NH25PS005185-01-00).
Data presented in part at the STD Prevention Conference, 2020 (virtual).
Contributor Information
Christina S. Thibault, Email: Christina.Thibault@kingcounty.gov.
Lindley A. Barbee, Email: lbarbee@u.washington.edu.
Matthew R. Golden, Email: golden@u.washington.edu.
Christine Khosropour, Email: ckhosro@medicine.washington.edu.
Roxanne P. Kerani, Email: rkerani@uw.edu.
REFERENCES
- 1.Holshue ML DeBolt C Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med 2020; 382:929–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention . CDC, Washington State Report first COVID-19 Death. Available at: https://www.cdc.gov/media/releases/2020/s0229-COVID-19-first-death.html.
- 3.Washington Governor . Inslee issues COVID-19 emergency proclamation (Office of the Governor website). Available at: https://www.governor.wa.gov/news-media/inslee-issues-covid-19-emergency-proclamation. Accessed January 1, 2021.
- 4.Washington Governor . Inslee announces “Stay Home, Stay Healthy” order (Office of the Governor website). Available at: https://www.governor.wa.gov/news-media/inslee-announces-stay-home-stayhealthy%C2%A0order. Accessed January 1, 2021.
- 5.Washington Governor . Restrictions on non urgent medical procedures (Office of the Governor website). Available at: https://www.governor.wa.gov/sites/default/files/proclamations/20-24%20COVID-19%20non-urgent%20medical%20procedures%20%28tmp%29.pdf?utm_medium=email&utm_source=govdelivery. Accessed January 1, 2021.
- 6.Barbee LA Dombrowski JC Hermann S, et al. “Sex in the time of COVID”: Clinical guidelines for sexually transmitted disease management in an era of social distancing. Sex Transm Dis 2020; 47:427–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Washington Governor . Inslee issues Safe Start proclamation for county approach to re-opening (Office of the Governor website). Available at: https://www.governor.wa.gov/news-media/inslee-issues-safe-start-proclamation-county-approach-re-opening. Accessed January 1, 2021.
- 8.Ong JJ Fethers K Howden BP, et al. Asymptomatic and symptomatic urethral gonorrhoea in men who have sex with men attending a sexual health service. Clin Microbiol Infect 2017; 23:555–559. [DOI] [PubMed] [Google Scholar]
- 9.Brill JR. Diagnosis and treatment of urethritis in men. Am Fam Physician 2010; 81:873–878. [PubMed] [Google Scholar]
- 10.SAS. Version 9.4. Cary, NC: SAS Institute, 2020. [Google Scholar]
- 11.National Coalition of STD Directors . COVID-19 & the State of the STD Field (NCSD Website). Available at: https://www.ncsddc.org/resource/covid-19-and-the-state-of-the-std-field/. Accessed December 21, 2020.
- 12.Tao J Napoleon SC Maynard MA, et al. Impact of the COVID-19 pandemic on sexually transmitted infection clinic visits. Sex Transm Dis 2020; 47:431–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Napoleon SC Maynard MA Almonte A, et al. Considerations for STI clinics during the COVID-19 pandemic. Sex Transm Dis 2020; 47:431–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pampati S Emrick K Siegler A, et al. Changes in sexual behavior, PrEP adherence, and access to sexual health services because of the COVID-19 pandemic among a cohort of PrEP-using MSM in the South. J Acquir Immune Defic Syndr 2021; 87:639–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Melendez JH Hamill MM Armington GS, et al. Home-based testing for sexually transmitted infections: Leveraging online resources during the COVID-19 pandemic. Sex Transm Dis 2021; 48:e8–e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carnevale C Richards P Cohall R, et al. At-home testing for sexually transmitted infections during the COVID-19 pandemic. Sex Transm Dis 2021; 48:e11–e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blank S. Impact of COVID-19 on STI Services, New York City, 2020. Presented at: 2020 STD Prevention Conference; 2020; Virtual.
- 18.Bolan G Weinstock H Harvey D, et al. 2020STD Prevention Conference: Roundtable Discussion for Journalists (CDC Web site). Available at: https://www.cdc.gov/nchhstp/newsroom/2020/2020-std-prevention-conference.html. Accessed December 21, 2020.
- 19.Menza TW Zlot AI Garai J, et al. The impact of the SARS-CoV-2 pandemic on human immunodeficiency virus and bacterial sexually transmitted infection testing and diagnosis in Oregon. Sex Transm Dis 2021; 48:e59–e63. [DOI] [PubMed] [Google Scholar]
- 20.Sanchez TH Zlotorzynska M Rai M, et al. Characterizing the impact of COVID-19 on men who have sex with men across the United States in April, 2020. AIDS Behav 2020; 24:2024–2032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reyniers T Rotsaert A Thunissen E, et al. Reduced sexual contacts with non-steady partners and less PrEP use among MSM in Belgium during the first weeks of the COVID-19 lockdown: Results of an online survey. Sex Transm Infect 2020; sextrans-2020-054756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van Bilsen WPH Zimmermann HML Boyd A, et al. Sexual behavior and its determinants during COVID-19 restrictions among men who have sex with men in Amsterdam. Acquir Immune Defic Syndr 2021; 86:288–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hammoud MA Maher L Holt M, et al. Physical distancing due to COVID-19 disrupts sexual behaviors among gay and bisexual men in Australia: Implications for trends in HIV and other sexually transmissible infections. J Acquir Immune Defic Syndr 2020; 85:309–315. [DOI] [PubMed] [Google Scholar]
- 24.Jenness SM Le Guillou A Chandra C, et al. Projected HIV and bacterial sexually transmitted infection incidence following COVID-19-related sexual distancing and clinical service interruption. J Infect Dis 2021; 223:1019–1028. [DOI] [PMC free article] [PubMed] [Google Scholar]


