Abstract
Pre-exposure prophylaxis (PrEP) uptake remains woefully low among U.S. women at high risk for HIV acquisition. We evaluated a pilot intervention which involved Peers providing brief PrEP education and counseling at mobile syringe exchange sites and at sex worker and syringe exchange drop-in centers followed by navigation to PrEP care. Peers recruited English-proficient, self-identified women (i.e., cisgender and transgender women and persons with other transfeminine identities) over a 3-month period and delivered the intervention to 52 HIV-negative/status unknown participants. Thirty-eight participants (73.1%) reported PrEP interest, 27 (51.9%) accepted the offer of a PrEP appointment, 13 (25.0%) scheduled a PrEP appointment, 3 (5.8%) attended an initial PrEP appointment, and none were prescribed PrEP. We found a gap between PrEP interest and connecting women to PrEP care. Further study is needed to understand this gap, including exploring innovative approaches to delivering PrEP care to women at highest risk for HIV.
Keywords: Women, HIV, Pre-exposure prophylaxis, Syringe exchange programs, Sex work
Introduction
Pre-exposure prophylaxis (PrEP) reduces the risk of HIV acquisition for cisgender and transgender women [1–5]. Although PrEP does not prevent against non-HIV sexually transmitted infections (STIs), PrEP is a user-controlled method, and it may be an especially important HIV prevention strategy for women as it can be used at a woman’s own discretion and without having to negotiate for safer sex with a sexual partner. However, cisgender and transgender women face a number of barriers to PrEP uptake [6–9], and available data indicate that PrEP uptake in the United States (U.S), particularly among cisgender and transgender women, has remained persistently low since the approval of emtric-itabine-tenofovir disoproxil fumarate for PrEP in 2012, the only drug approved for PrEP in both cisgender and transgender women [10–15]. Moreover, striking racial/ethnic inequities exist with PrEP uptake being lowest among Black and Latina women [14], who account for almost 59% and 16% of new HIV diagnoses among U.S. cisgender women, respectively, and 44% and 26% of U.S. HIV-positive transgender women, respectively [16, 17].
Given “Ending the HIV Epidemic: A Plan for America”, the national plan to reduce new HIV infections by 90% by 2030, there is an urgent need to develop and implement evidence-based interventions to increase PrEP uptake among cisgender and transgender women at high risk for HIV infection [18]. Women at high risk include those who live in areas of high HIV prevalence and engage in condomless sex and/or exchange sex, and/or those who inject drugs [19]. It is not exchanging sex in and of itself that places women at risk, but rather the complex environments (e.g., housing insecurity, gender-based violence) that make it challenging to negotiate condom use and place women at risk [20]. Moreover, focusing HIV prevention interventions on cisgender and transgender women placed at highest risk for HIV has the potential to be a cost-effective approach [21]. However, to our knowledge, no published interventions are designed to increase PrEP uptake among U.S. women at high risk for HIV. Moreover, inclusive women’s programming—in other words, interventions that include both cisgender and transgender women and persons with other transfeminine identities—represents a cutting-edge HIV prevention approach. Cisgender and transgender women are not typically grouped together in HIV prevention intervention studies; in fact, it is more common to see men who have sex with men and transgender women simultaneously targeted by an HIV prevention intervention. However, cisgender and transgender women at high risk for HIV face many shared vulnerabilities based on their gender identity including similar social and economic conditions (e.g., poverty, gender-based violence, lack of access to quality health care) which act in concert to increase their risk of HIV [22–26]. Additionally, social stigma and transphobia further amplify transgender women’s risk of HIV [22, 24].
A growing body of literature has identified barriers to and facilitators of PrEP uptake among cisgender and transgender women. Contributors to low PrEP uptake among women include lack of PrEP awareness [15, 27, 28], misinformation about PrEP eligibility and appropriateness [29, 30], concerns about side effects and cost [6, 8, 30, 31], PrEP-related stigma [31–33], and medical mistrust [6], including mistrust due to transphobia experienced by women of trans experience [34]. Facilitators of PrEP uptake for women include learning about PrEP from a trusted source [35], having a welcoming, client-centered, culturally appropriate environment, and having positive interactions with PrEP clinical providers and other trusted medical and community-based providers [30, 35, 36]. Interventions that mitigate barriers, enhance facilitators and that can be easily adopted and scaled up have the potential to fill an important gap.
Peer outreach and navigation represents a potentially effective approach to increasing PrEP uptake among women at high risk for HIV. This approach has frequently been used in the context of HIV medical care to engage with and connect individuals, often from marginalized populations, to health care and social services [37–39]. It has been increasingly used in clinical practice to connect individuals to PrEP care. A review of the published literature from 2012 to 2017 of models of PrEP care found that peers and community-based organizations (CBOs) played an important role in engaging with and navigating individuals at highest risk to PrEP care [40]. Peers are often considered by clients to be reliable sources of information due to their shared experience and nonjudgmental approach to providing information [41]. Peer navigation can help facilitate linkage to a culturally competent clinical site and help mitigate socio-structural barriers to PrEP care. CBOs often have intimate knowledge of and contact with individuals from marginalized populations and may offer peer outreach and navigation services. Collaboration with CBOs can also help leverage the CBO’s existing services to address structural barriers to PrEP care such as assistance obtaining health insurance coverage and referrals to mental health or housing services.
To address the absence of evidence-based and evidence-informed interventions to increase PrEP uptake among women, we designed, implemented and evaluated PrEP-UP, a novel PrEP peer outreach and navigation intervention for women at high risk for HIV infection. This paper describes PrEP-UP, the socio-demographic, behavioral, and psychosocial characteristics of the women enrolled, and outcomes from a single-arm pilot study of PrEP-UP’s implementation.
Methods
Setting
We partnered with an established, long-standing CBO that provides harm reduction services in East Harlem and the Bronx, NY, two regions of New York City with high HIV prevalence [42]. The CBO provides a comprehensive set of services that include peer outreach and navigation; harm reduction (e.g., condoms, HIV testing, and syringe exchange); case management; mental health care; referrals to substance use treatment programs; housing placement assistance, and benefits assistance. The majority of the CBO’s harm reduction services are delivered by peer outreach workers (Peers). Services are offered at the CBO’s two brick-and-mortar drop-in centers, one of which includes a Friday evening drop-in center specifically for women involved in exchange sex, and at nine mobile syringe exchange sites located throughout East Harlem and the Bronx. At the mobile syringe exchange sites, services are provided at established street-side locations often out of a mobile unit such as a van. They include syringe exchange and injection drug use supplies, as well as other harm reduction services such as pipes for smoking drugs such as crack cocaine and/or methamphetamines, testing for HIV and hepatitis C, opioid overdose prevention services, condoms and information on biomedical HIV prevention.
Clients are navigated to services at one of the CBO’s brick-and-mortar locations if they want or need additional services such as case management, housing placement assistance and benefits assistance. The CBO uses a peer outreach and navigation model whereby Peers assist in linking clients to general and HIV primary care via case management (appointment reminders and accompaniment, supportive counseling, etc.). If a Peer engages a client at a mobile syringe exchange site who needs additional services, the Peer can then accompany the client to one of the CBO’s two brick-and-mortar locations or can meet the client at one of the two locations at a subsequently scheduled time.
For this study, participants were linked to a clinic in the South Bronx which was accessible by public transportation from the CBO’s mobile syringe exchange sites and two brick-and-mortar drop-in centers. The clinic offers primary and subspecialty care; buprenorphine treatment; HIV and Hepatitis C Virus treatment; gender-affirming care and services, and referrals to outpatient and inpatient substance use treatment. The clinic is also a federally-qualified health center which means it provides these services regardless of ability to pay or insurance status. Its primary care physicians are experienced in PrEP care, follow PrEP clinical guidance from the Centers for Disease Control and Prevention, the New York State Department of Health’s AIDS Institute, and the New York City Department of Health and are familiar with other PrEP indications as identified in the literature (e.g., intimate partner violence) [19, 43, 44]. The clinic also has a dedicated PrEP patient navigator who calls patients with appointment reminders; follows up with patients after missed visits; links patients to relevant social services in the community, and assists with insurance coverage issues.
Intervention Description
The intervention, PrEP-UP, was integrated into the CBO’s existing peer-facilitated service delivery model and included: (1) PrEP education, (2) PrEP counseling, and (3) navigation to PrEP care. The Information-Motivation-Behavioral Skills (IMB) model of HIV preventive behavior [45] posits that the determinants of effectively carrying out HIV preventive behaviors include: (1) HIV prevention information which can be feasibly enacted, (2) motivation to engage in HIV preventive behavior and (3) behavioral skills to engage in HIV preventive acts.
Guided by the IMB model, we designed PrEP-UP to (1) provide relevant, actionable information about PrEP, (2) increase personal motivation to use PrEP, and (3) enhance perceived self-efficacy and objective behavioral skills needed to effectively use PrEP. The education component consisted of providing the basic facts about PrEP (i.e., what PrEP is, how it works, what PrEP does not do, side effects, and what is involved in taking PrEP). The counseling component utilized motivational interviewing techniques to address attitudes about and behavioral intentions towards initiating and engaging in PrEP care and taking PrEP. Education and counseling were delivered in an initial brief encounter (i.e., 10–15 min) with the participant and then as needed during subsequent interactions between participant and Peer. Information was also tailored to address concerns that might be specific to transgender women (e.g., potential interactions of PrEP with gender-affirming hormone therapy). Intervention content incorporated adult learning theories including transformative learning (e.g., seeking to engage participants where they are; building on prior knowledge and introducing new information) and experiential learning (e.g., providing information that can be used immediately) [46]. This component was followed by asking the participant if she was interested in learning more about PrEP. If the participant responded affirmatively, she was then offered a PrEP care appointment at a nearby clinic, in addition to any other needed health (e.g., primary care, obstetrics/gynecology) and social services (e.g., housing, mental health services, substance use treatment, case management) appointments. If the encounter occurred during business hours, the participant was given the date and time of the PrEP clinic appointment on the spot. If the encounter occurred after business hours, the clinic’s PrEP navigator contacted the participant the following business day with the date and time of a scheduled PrEP care appointment. On the day of the PrEP care appointment, the Peer would then meet the participant at the clinic or at one of the CBO’s brick-and-mortar locations or mobile syringe exchange sites from where the participant was initially recruited, whichever the participant’s preference. The Peer would then give the participant a roundtrip Metrocard for travel via public transportation (value $5.00). If the Peer met the participant at the one of the CBO’s brick-and-mortar locations or at a mobile syringe exchange site, the Peer would then travel via public transportation with the participant to the clinic which was located nearby. The linkage and navigation component also included assistance with subsequent appointment scheduling, appointment reminders, and transportation (i.e., Metrocards), as well as appointment accompaniment (i.e., accompanying the participant to clinic visits) for the first three to four visits (~4–12 weeks).
Two Peers—one transgender woman and one cisgender woman—who shared similar life experiences to the target population (e.g., history of exchange sex and/or substance use) were hired and trained to deliver the intervention. Over a three-week period, Peers received approximately 30 h of training on participant recruitment, PrEP education and counseling, linkage and navigation strategies, harm reduction, and participant confidentiality. This included nine sessions delivered by study staff as well as PrEP and motivational interviewing-specific trainings delivered online or in-person by the New York City and New York State Departments of Health which are provided free of cost [47, 48]. Sessions involved role-playing with case vignettes, pre-and post-tests and training in recording data in peer logs. Peers toured the clinic and met with core clinic staff including the PrEP navigator. Peers were supervised by the study’s project manager who throughout the study also observed the Peers delivering the intervention to participants. Realtime feedback was provided when necessary. The study team met weekly to troubleshoot any issues with the protocol and provide opportunities for the Peers to enhance their skills, including engaging in additional role-playing exercises. Peers were provided with resources such as flash cards with key messages to help facilitate delivery of the intervention.
Study Population
Participant recruitment and enrollment took place from November 2017 to February 2018 at the CBO’s two brick-and-mortar drop-in centers as well as at its nine mobile syringe exchange sites. Participants were eligible if they (1) self-identified as a woman (included cisgender women, transgender women and persons with other trans feminine identities), (2) were 18 years or older, (3) proficient in English, and (4) were receiving services at the CBO’s mobile syringe exchange sites and/or sex worker/harm reduction drop-in centers. We kept the eligibility criteria broad given that women using these services were likely to be at high risk of HIV acquisition due to related activities (e.g., condomless sex, sex work, drug use) and because we wanted to minimize the likelihood of potential participants providing socially desirable responses to meet study eligibility. While interacting with CBO clients, the Peers briefly described the study and invited clients to participate. If interested, clients were screened, and written informed consent was obtained from all individual participants included in the study. The study was approved by Albert Einstein College of Medicine’s Institutional Review Board (IRB).
Data Collection
Data collection took place at the mobile syringe exchange sites and the CBO’s drop-in centers. Peers collected participants’ names and contact information (i.e., phone numbers, email addresses). Baseline quantitative survey data were collected prior to intervention delivery and measured the following domains: socio-demographic characteristics (age, race/ethnicity, gender identity, sexual orientation, relationship status, education, housing status, and insurance status) [49, 50], self-reported HIV status (positive, negative, unknown), sexual and substance use behaviors (whether they had main partner, likelihood of main having other partners, likelihood of main partner injecting drugs, condomless vaginal sex, condomless anal sex, any condomless sex, and exchange sex) [51], symptoms of depression and anxiety (Patient Health Questionnaire 2-item [PHQ-2] and Generalized Anxiety Disorder Scale 2-item [GAD-2]) [52, 53], intimate partner violence (Hit, Insult, Threaten, Scream Took for Intimate Partner Violence Screening [HITS]) [54], PrEP-and HIV-related psychosocial measures (ever heard of PrEP; ever asked a health care provider about PrEP; ever talked to a health care provider about PrEP; ever prescribed PrEP; know some who has taken PrEP; perceived PrEP safety and effectiveness; level of HIV-related worry; likelihood of acquiring HIV in the next year; and self-perceived risk of one’s own sexual behaviors) [55], and healthcare engagement (place of health care, whether they have a personal health care provider, and whether they had a visit to a health care provider in the last one to three months [55]. The survey took approximately 10–15 min to complete and was administered by study staff using the REDCap mobile application via an iPad computer tablet. Participants who self-reported their HIV status as positive on the baseline survey were offered the CBO’s usual Peer-facilitated HIV linkage and navigation services. Those who self-reported their HIV status as negative or unknown were offered the PrEP-UP intervention. For participants who received PrEP-UP, quantitative data were collected through the use of Peer activity logs; this included engagement in the stages of PrEP-UP intervention cascade: (1) interest in PrEP; (2) acceptance of a PrEP care appointment offer; (3) receipt of a scheduled PrEP appointment; (4) attendance at a PrEP care appointment, and (5) receipt of a PrEP prescription. Participant personal information (e.g., contact information) was kept in a separate database from other study-related data. Unique participant identifiers linking these two databases were kept in a separate secure, password-protected database only accessible to study staff. Identifiers were used in all datasets and in peer logs. A certificate of confidentiality was obtained for the study and participants were told about the certificate and its purpose during the written informed consent process. Participants received a $40 gift card for completing the baseline survey and received roundtrip Metrocards at each PrEP care appointment.
Statistical Analyses
We began by describing socio-demographic characteristics, sexual and drug use behaviors and PrEP- and HIV-related psychosocial measures for the study sample and for engagement outcomes along the PrEP-UP intervention cascade. To explore differences in participants’ characteristics, behaviors and psychosocial measures by PrEP interest and by PrEP appointment acceptance, we conducted Chi-square tests for binary or categorical variables and t-tests for continuous variables. Fisher’s Exact and Wilcoxon rank-sum tests were used in the case of small sample size or non-normal distribution. All analyses were done in SAS 9.4 (SAS Institute, Cary NC).
Results
Seventy-two people were screened, of whom 66 were eligible to enroll. Lack of English proficiency was the primary reason for ineligibility. All 66 women consented to participate and enrolled in the study. Of these 66 participants, 64 completed the baseline survey. Those participants who reported they were HIV-negative or status unknown (n = 56) were eligible to receive the PrEP-UP intervention. Fifty-two participants ultimately received PrEP-UP and were included in the analyses. Tables 1 and 2 contain data about the study sample’s socio-demographic and behavioral characteristics as well as the associations of these characteristics with PrEP interest and PrEP appointment acceptance, respectively.
Table 1.
Associations of socio-demographic and behavioral characteristics with PrEP interest (n = 52)
| Characteristic | Total (n = 52) | Interested in PrEP (n = 38) | Not interested in PrEP (n = 14) | Chi-squared statistic (degrees of freedom) | p |
|---|---|---|---|---|---|
| Age, years, n (%) | |||||
| 20–35 | 13 (25.0%) | 8 (21.1%) | 5 (35.7%) | 0.30c | |
| 36–50 | 17 (32.7%) | 11 (29.0%) | 6 (42.9%) | 0.51c | |
| ≥50 | 22 (42.3%) | 19 (50.0%) | 3 (21.4%) | χ2 (1) = 0.42 | 0.06 |
| Race/ethnicity, n (%) | |||||
| Latina/Hispanic | 27 (51.9%) | 20 (52.6%) | 7 (50.0%) | χ2 (1) = 0.03 | 0.87 |
| Non-Hispanic Black | 18 (34.6%) | 12 (31.6%) | 6 (42.9%) | 0.52c | |
| Non-Hispanic White/Other | 7 (13.5%) | 6 (15.8%) | 1 (7.1%) | 0.66c | |
| Current gender identity, n (%) | |||||
| Cisgender woman | 46 (88.5%) | 33 (86.8%) | 13 (92.9%) | 1.00c | |
| Transgender woman | 6 (11.5%) | 5 (13.2%) | 1 (7.1%) | ||
| Sexual orientation, n (%) | |||||
| Gay/Lesbian/Bisexual/Other | 22 (42.3%) | 17 (44.7%) | 5 (35.7%) | χ2 (1) = 0.34 | 0.56 |
| Heterosexual/Straight | 30 (57.7%) | 21 (55.3%) | 9 (64.3%) | ||
| Non-partnered relationship status, n (%) | 33 (63.5%) | 25 (65.8%) | 8 (57.1%) | χ2 (1) = 0.33 | 0.57 |
| Education, n (%) | |||||
| Some high school | 18 (34.6%) | 16 (42.1%) | 2 (14.3%) | 0.10 | |
| High school diploma or GED | 19 (36.5%) | 10 (26.3%) | 9 (64.3%) | χ2 (1) = 6.36 | 0.01 |
| Some college or more | 15 (28.9%) | 12 (21.6%) | 3 (21.4%) | 0.73 | |
| Housing insecure, n (%) | 25 (40.1%) | 18 (47.4%) | 7 (50.0%) | χ2 (1) = 0.03 | 0.87 |
| Insurance status/cost, n (%) | |||||
| Has health insurance | 47 (90.4%) | 34 (89.5%) | 13 (92.9%) | 1.00c | |
| Unable to see a healthcare provider due to cost | 11 (21.6%) | 7 (18.9%) | 4 (28.6%) | ||
| Sexual behavior (in last 30 days), n (%) | |||||
| Any vaginal or anal sex | 39 (75%) | 32 (84.2%) | 7 (50.0%) | χ2 (1) = 6.39 | 0.01 |
| Condomless vaginal sex | 19 (36.5%) | 17 (44.7%) | 2 (14.3%) | χ2 (1) = 4.09 | 0.04 |
| Condomless anal sex | 7 (13.5%) | 6 (15.8%) | 1 (7.1%) | 0.66c | |
| Any condomless sex | 23 (44.2%) | 20 (52.6%) | 3 (21.4%) | χ2 (1) = 4.04 | 0.04 |
| Sex with exchange partner | 15 (28.9%) | 14 (36.8%) | 1 (7.1%) | 0.04c | |
| Had main sexual partner | 30 (57.7%) | 23 (60.5%) | 7 (50.0%) | χ2 (1) = 0.46 | 0.50 |
| Main partner “definitely” or “probably” has other sex partner(s)a | 12 (40.0%) | 10 (43.4%) | 2 (28.6%) | 0.66c | |
| Main partner “definitely” or “probably” injects with othersa | 10 (33.3%) | 8 (34.8%) | 2 (28.6%) | 1.00b | |
| Substance use (in last 30 days), n (%) | |||||
| Any substance use | 42 (80.8%) | 33 (86.8%) | 9 (64.3%) | χ2 (1) = 3.35 | 0.07 |
| Injected drugs | 14 (26.9%) | 11 (29.0%) | 3 (21.4%) | 0.73c | |
| Positive screen for anxiety, n (%) | 32 (61.5%) | 24 (63.2%) | 8 (57.1%) | χ2 (1) = 0.16 | 0.69 |
| Positive screen for depression, n (%) | 23 (44.2%) | 17 (44.7%) | 6 (42.9%) | χ2 (1) = 0.01 | 0.90 |
| Positive screen for IPV, n (%) | 13 (25.0%) | 10 (26.3%) | 3 (21.4%) | 1.00c | |
| HIV-related psychosocial measures | |||||
| HIV-related worry (“some” or “all the time”), n (%) | 31 (59.6%) | 26 (68.4%) | 5 (35.7%) | χ2 (1) = 5.09 | 0.02 |
| HIV risk perception | |||||
| Likelihood of getting HIV in the next year (%), mean (SD) (out of 100%) | 17.9(± 27.9) | 23.1(± 30.2) | 3.7(± 13.3) | − 2.3ld | 0.03 |
| “Somewhat risky” or “very risky” sexual behavior, n (%) | 23 (44.2%) | 19 (50.0%) | 4 (28.6%) | χ2 (1) = 1.90 | 0.17 |
| PrEP-related psychosocial measures | |||||
| Heard of PrEP, n (%) | 26 (50.0%) | 15 (39.5%)b | 11 (78.6%)b | χ2 (1) = 6.26 | 0.01 |
| Asked HCP about PrEPb | 10 (38.5%) | 7 (46.7%) | 3 (27.3%) | χ2 (1) = 1.01 | 0.32 |
| Had HCP talk to them about PrEPb | 11 (42.3%) | 5 (33.3%) | 6 (54.6%) | 0.43c | |
| Been prescribed PrEPb | 4 (15.4%) | 3 (20.0%) | 1 (9.1%) | 0.45c | |
| Know someone who has taken PrEPb | 12 (46.2%) | 6 (40.0%) | 6 (54.6%) | 0.43c | |
| PrEP effectiveness (10-point scale, 1 = not at all, 10 = extremely), median, IQR | 8 (7–10) | 9 (7–10) | 8 (7–9) | − 0.94d | 0.36 |
| PrEP safety (10-point scale, 1 = not at all, 10 = extremely), median, IQR | 9 (7–10) | 9 (7–10) | 9 (7–10) | 0.17d | 0.86 |
| Place of health care, n (%) | |||||
| Primary care clinic/community health center | 45 (86.5%) | 33 (86.8%) | 12 (92.3%) | 1.00c | |
| Emergency Department/Urgent Care/Other | 5 (9.6%) | 4 (10.5%) | 1 (7.1%) | ||
| Personal health care provider, n (%) | 44 (84.6%) | 32 (84.2%) | 12 (85.7%) | 0.66 | |
| Last visit to a HCP within the last 1–3 months, n (%) | 41 (78.8%) | 28 (73.7%) | 13 (92.9%)a | 0.05 |
IPV intimate partner violence, HCP health care provider, Non-partnered single, casual, or non-monogamous. Housing insecure housing status other than living in own house or apartment
Asked only of participants who responded “yes” to having a main partner
Only asked of participants who responded “yes” to having heard of PrEP
Indicates that Fisher Exact test p value is presented due to small expected cell counts under Chi- Squared test
Indicates that a t-test p was run for continuous data
Table 2.
Associations of socio-demographic and behavioral characteristics with PrEP appointment acceptance (n = 52)
| Characteristic | Total (n = 52) | Accepted PrEP appointment (n = 27) | Declined PrEP appointment (n = 25) | Chi-squared statistic (degrees of freedom) | p |
|---|---|---|---|---|---|
| Age, years, n (%) | |||||
| 20–35 | 13 (25.0%) | 7 (25.9%) | 6 (24.0%) | χ2 (2) = 0.24 | 0.89 |
| 36–50 | 17 (32.7%) | 8 (29.6%) | 9 (36.0%) | ||
| ≥50 | 22 (42.3%) | 12 (44.4%) | 10 (40.0%) | ||
| Race/ethnicity, n (%) | |||||
| Latina/Hispanic | 27 (51.9%) | 16 (59.3%) | 11 (44.0%) | χ2 (1) = 1.21 | 0.27 |
| Non-Hispanic Black | 18 (34.6%) | 8 (29.6%) | 10 (40.0%) | χ2 (1) = 0.62 | 0.43 |
| Non-Hispanic White/Other | 7 (13.5%) | 3 (11.1%) | 4 (16.0%) | 0.70c | |
| Current gender identity, n (%) | |||||
| Cisgender woman | 46 (88.5%) | 23 (85.2%) | 23 (92.0%) | 0.67c | |
| Transgender woman | 6 (11.5%) | 4 (14.8%) | 2 (8.0%) | ||
| Sexual orientation, n (%) | |||||
| Gay/Lesbian/Bisexual/Other | 22 (42.3%) | 12 (44.4%) | 10 (40.0%) | χ2 (1) = 0.11 | 0.75 |
| Heterosexual/Straight | 30 (57.7%) | 15 (55.6%) | 15 (60.0%) | ||
| Non-partnered relationship status, n (%) | 33 (63.5%) | 18 (66.7%) | 15 (60.0%) | χ2 (1) = 0.25 | 0.62 |
| Education, n (%) | |||||
| Some high school | 18 (34.6%) | 9 (33.3%) | 9 (36.0%) | χ2 (2) = 0.58 | 0.75 |
| High school diploma or GED | 19 (36.5%) | 9 (33.3%) | 10 (40.0%) | ||
| Some college or more | 15 (28.9%) | 9 (33.3%) | 6 (24.0%) | ||
| Housing insecure, n (%) | 25 (40.1%) | 13 (48.2%) | 12 (48.0%) | χ2 (1) = 0.001 | 0.99 |
| Insurance status/cost, n (%) | |||||
| Has health insurance | 47 (90.4%) | 24 (88.9%) | 23 (92.0%) | 1.00c | |
| Unable to see a healthcare provider due to cost | 11 (21.6%) | 7 (26.9%) | 4 (16.0%) | 0.50c | |
| Sexual behavior (in last 30 days), n (%) | |||||
| Any vaginal or anal sex | 39 (75%) | 22 (81.5%) | 17 (68.0%) | χ2 (1) = 1.26 | 0.26 |
| Had main sexual partner | 30 (57.7%) | 15 (55.6%) | 15 (60.0%) | χ2 (1) = 0.11 | 0.75 |
| Main partner “definitely” or “probably” has other sex partner(s)a | 12 (40.0%) | 5 (33.3%) | 7 (50.0%) | χ2 (1) = 0.83 | 0.36 |
| Main partner “definitely” or “probably” injects with othersa | 10 (33.3%) | 6 (40.0%) | 4 (26.7%) | 0.70 c | |
| Condomless vaginal sex | 19 (36.5%) | 11 (40.7%) | 8 (32.0%) | χ2 (1) = 0.43 | 0.51 |
| Condomless anal sex | 7 (13.5%) | 5 (18.5%) | 2 (8.0%)) | 0.42c | |
| Any condomless sex | 23 (44.2%) | 14 (51.9%) | 9 (36.0%) | χ2 (1) = 1.32 | 0.25 |
| Sex with exchange partner | 15 (28.9%) | 11 (40.7%) | 4 (16.0%) | 0.07 c | |
| Substance use (in last 30 days), n (%) | |||||
| Any substance use | 42 (80.8%) | 22 (81.5%) | 20 (80.0%) | χ2 (1) = 0.02 | 0.89 |
| Injected drugs | 14 (26.9%) | 7 (25.9%) | 7 (28.0%) | χ2 (1) = 0.03 | 0.87 |
| Positive screen for anxiety, n (%) | 32 (61.5%) | 17 (63.0%) | 15 (60.0%) | χ2 (1) = 0.05 | 0.83 |
| Positive screen for depression, n (%) | 23 (44.2%) | 12 (44.4%) | 11 (44.0%) | χ2 (1) = 0.001 | 0.97 |
| Positive screen for IPV, n (%) | 13 (25.0%) | 8 (29.6%) | 5 (20.0%) | χ2(1) = 0.64 | 0.42 |
| HIV-related psychosocial measures | |||||
| HIV-related worry (“some” or “all the time”), n (%) | 31 (59.6%) | 18 (66.7%) | 13 (52.0%) | χ2 (1) = 1.59 | 0.21 |
| HIV risk perception | |||||
| Likelihood of getting HIV in the next year (%), mean (SD) (out of 100%) | 17.9 (± 27.9) | 19.5 (± 24.9) | 16.8 (± 31.3) | − 0.44d | 0.67 |
| “Somewhat risky” or “very risky” sexual behavior, n (%) | 23 (44.2%) | 16 (59.3%) | 7 (28.0%) | χ2 (1) = 5.14 | 0.02 |
| PrEP-related psychosocial measures, n(%) | |||||
| Heard of PrEP, n (%) | 26 (50.0%) | 10 (37.0%) | 16 (64.0%) | χ2 (1) = 3.77 | 0.05 |
| Asked HCP about PrEPb | 10 (38.5%) | 4 (40.0%) | 6 (37.5%) | 1.00c | |
| Had HCP talk to them about PrEPb | 11 (42.3%) | 2 (20.0%) | 9 (56.3%) | 0.11c | |
| Been prescribed PrEPb | 4 (15.4%) | 1 (10.0%) | 3 (18.8%) | 1.00c | |
| Know someone who has taken PrEPb | 12 (46.2%) | 3 (30.0%) | 9 (56.3%) | 0.23c | |
| PrEP effectiveness (10-point scale, 1 = not at all, 10 = extremely), median, IQR | 8 (7–10) | 9 (7–10) | 8 (7–10) | − 1.27 d | 0.22 |
| PrEP safety (10-point scale, 1 = not at all, 10 = extremely), median, IQR | 9 (7–10) | 9 (7–10) | 9 (8–10) | 0.75 d | 0.50 |
| Place of health care, n (%) | |||||
| Primary care clinic/community health center | 45 (86.5%) | 24 (88.9%) | 21 (87.5%) | 1.00c | |
| Emergency Department/Urgent Care/Other | 5 (9.6%) | 3 (11.1%) | 2 (8.0%) | ||
| Personal health care provider, n (%) | 44 (84.6%) | 23 (85.2%) | 21 (84.0%) | 1.00c | |
| Last visit to a HCP within the last 1–3 months, n (%) | 41 (78.8%) | 21 (77.8%) | 20 (83.3%) | 0.73c |
IPV intimate partner violence, HCP health care provider, Non-partnered single, casual, or non-monogamous, Housing insecure housing status other than living in own house or apartment
Asked only of participants who responded “yes” to having a main partner
Only asked of participants who responded “yes” to having heard of PrEP
Indicates that Fisher Exact test p value is presented due to small expected cell counts under Chi-Squared test
Indicates that a t- test was run for continuous data
Socio-demographic Characteristics
Mean age was 44.7 years old (SD ± 12.0). Six women (11.5%) were transgender, and forty-five participants (86.5%) were Latina or non-Latina Black. Twenty-two participants (42.3%) identified as gay, lesbian or bisexual and thirty-three (63.5%) did not have a main partner. Eighteen participants (34.6%) reported having less than a high school education and 25 (40.1%) reported housing insecurity (i.e., not having their own apartment or house).
Behavioral Characteristics
Thirty-nine participants (75.0%) reported being sexually active within the last 30 days. Nineteen participants (36.5%) reported condomless vaginal sex, 7 (13.5%) condomless anal sex, and 23 (44.2%) any condomless sex. Fifteen (28.9%) reported having an exchange sex partner and 30 (57.7%) reported having a main sexual partner, with all but one reporting a partner with male gender identity. Of the 30 participants with a main sexual partner, 12 (40.0%) thought their main partner was “definitely” or “probably” having sex with someone else.
Forty-two participants (80.8%) in the total sample reported substance use in the last 30 days (inclusive of injection and non-injection drug use) and fourteen (26.9%) reported injection drug use during that period. The most common substances used by participants were alcohol (51.9%) followed by cocaine or crack (40.4%) and heroin (38.5%).
Psychosocial Characteristics
Thirty-two women (61.5%) screened positive for anxiety and 23 (44.2%) screened positive for depression. Thirteen (25.0%) screened positive for intimate partner violence with their most recent partners.
Thirty-one participants (59.6%) reported worrying about HIV “some of the time” or “all of the time”. Twenty-three participants (44.2%) considered their sexual behavior “somewhat risky” or “very risky”. Twenty-six (50.0%) participants reported that they had heard of PrEP prior to study enrollment. Of those 26 participants, 10 (38.5%) had asked a healthcare professional about PrEP, 11 (42.3%) had a healthcare professional talk to them about PrEP, 4 (15.4%) had been prescribed PrEP, and 12 (46.2%) had known someone who had taken PrEP. Of those who had previously heard of PrEP, in response to how well PrEP works in preventing HIV infection (on a 10-point scale from “not at all well” to “extremely well”), perceived effectiveness was high: 8 out of 10 (IQR 7–10). Similarly, in response to how safe is PrEP on a 10-point scale from “not at all safe” to “extremely safe”, PrEP was perceived as very safe: 9 out of 10 (IQR 7–10), respectively.
Health Care Engagement
Most participants reported having health insurance (90.4%) and typically getting their health care at a primary care clinic or community health center (86.5%). The vast majority reported having someone they identified as their personal health care provider (84.6%) and having a visit with a health care provider in the last one to three months (78.8%).
PrEP-UP Intervention Cascade Engagement
All but five participants had a self-disclosed PrEP indication based on existing guidance [19, 43, 44]: 23 (44.2%) reported any condomless sex; 12 of the 30 (40%) with a main partner reported that their main partner definitely or probably has other partners; 13 (25.0%) screened positive for intimate partner violence; 42 (80.8%) reported active substance use, and 14 (26.9%) reported injection drug use. Of the 52 participants, 38 (73.1%) reported interest in learning more about PrEP, 27 (51.9%) accepted the offer of a PrEP care appointment, 13 (25.0%) were scheduled for PrEP care appointment, 3 (5.8%) attended an initial PrEP care appointment, and no participant received a PrEP prescription (Fig. 1). All three participants who attended an initial PrEP care appointment had an indication for PrEP based on existing guidance. Of participants who accepted a PrEP care appointment, but who did not receive a scheduled appointment (n = 14), 11 (78.6%) were engaged outside of clinic hours and the study team was unable to contact them to give them a scheduled appointment (e.g., participants’ phone out of service, participant did not return call). Thirty-six (69.2%) were referred to other needed health and social services, including social work/case management (29.5%), women’s reproductive health (26.2%), and mental health services (19.7%).
Fig. 1.
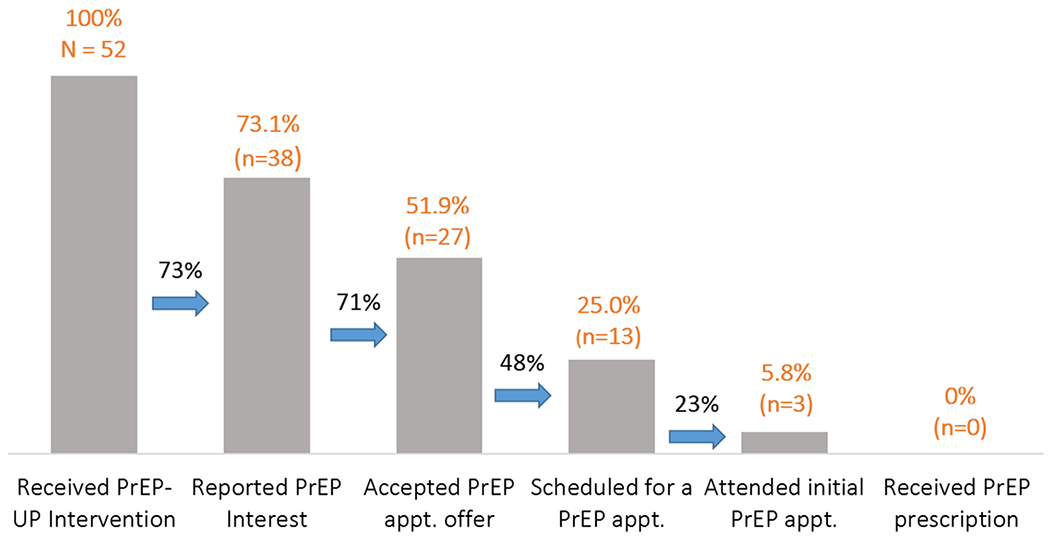
PrEP-UP Intervention Cascade. Percentages above each bar represent the proportion of the total sample (N = 52); percentages between bars represent the proportion retained at each step of the cascade
Exploratory Analyses of Participant Characteristics and Association with PrEP Interest and PrEP Appointment Acceptance
Compared with participants who did not report PrEP interest, participants with PrEP interest were more likely to report recent vaginal or anal sex (84.2% vs. 50.0%, χ2(1) = 6.39; p = 0.01), condomless vaginal sex (44.7% vs. 14.3%, χ2(1)=4.09; p = 0.04), any condomless sex (52.6% vs. 21.4%, χ2(1) = 4.04; p = 0.04) and recent exchange sex (38.8% vs. 7.1%; p = 0.04). Compared with those who declined a PrEP care appointment, those who accepted an appointment were also more likely to report recent exchange sex as (40.7% vs. 16.0%; p = 0.07). Additionally, those with PrEP interest were more likely to report HIV worry “some of the time” or “all of the time” (68.4% vs. 35.7%, χ2(1) = 5.09; p = 0.02) and to have a higher perceived likelihood of getting HIV in the next year (23.1%±30.2% vs 3.7% ± 13.3%; p = 0.03). Compared to those who declined a PrEP appointment, those who accepted a PrEP appointment were more likely to report their own sexual behavior as “somewhat risky” or “very risky” (59.3% vs. 28.0%, χ2(1) = 5.14; p = 0.02). Participants with PrEP interest and those who accepted an appointment were less likely to have heard of PrEP previously (39.5% vs. 78.6%, χ2(1) = 6.26; p = 0.01 and 37.0% vs. 64.0%, χ2(1) = 3.77; p = 0.05, respectively). Those who were interested in PrEP were also less likely to have seen a health care provider in the last three months (73.7% vs. 92.9%; p = 0.05).
Discussion
We conducted a pilot study of a novel PrEP peer outreach and navigation intervention for women based at mobile syringe exchange sites and sex worker and syringe exchange drop-in centers. We found it feasible for Peers to recruit a cohort of women at high risk for HIV at these sites and to provide brief PrEP-related education and counseling in these settings. Study participants were primarily Latina and non-Latina Black self-identified women at high risk for HIV based on sexual and drug use behaviors who lived in an area of high HIV prevalence. Despite reporting a high level of HIV-related worry and access to health care, self-perceived HIV risk was low and only half were previously aware of PrEP. However, we found linkage to PrEP care challenging. Although a majority of participants reported PrEP interest and accepted a PrEP appointment, and a sizeable minority were scheduled for an appointment, very few ultimately attended a PrEP appointment, and none received a PrEP prescription.
Our findings contribute to the limited evidence base for strategies and approaches to promoting PrEP uptake among women at risk. They highlight how Peers, syringe exchange sites and drop-in centers may be leveraged to provide PrEP education and counseling. Prior research has shown that discussions about HIV prevention at syringe exchange programs were associated with higher PrEP awareness among women who injected drugs [27]. PrEP interest and appointment acceptance were high suggesting missed opportunities for PrEP education and counseling at these sites. However, moving along the PrEP-UP intervention cascade, we saw a more substantial drop-off in participants receiving a scheduled PrEP appointment which was a particular challenge when women who were engaged outside of clinic hours. Moving further down the cascade, women experienced additional challenges with attendance at the scheduled appointment; only three women attended a PrEP appointment, suggesting that it may be difficult for women to attend appointments. This could be because of transportation issues or women may need more flexible scheduling hours. Given these findings, one potential solution may be to bring PrEP care to women in their current environments, by providing PrEP onsite at mobile syringe sites and at syringe exchange and sex worker drop-in centers instead of requiring women to travel to a separate location. Offering same-day PrEP starts may also help to seize a window of opportunity when women have expressed interest in PrEP and could help minimize appointment burden, as well as allowing for walk-in hours. Provision of substance use treatment (e.g., medication assisted treatment) and HIV treatment on mobile clinic units has been found to be feasible and acceptable [19, 56–60], indicating that provision of PrEP on mobile clinic units may be successful as well. However, it is also possible that participants may have given socially desirable responses to Peers’ question about interest in PrEP and their offer of a scheduled PrEP appointment and, therefore, actual PrEP interest may be lower. Planned follow-up in-depth interviews will help to understand participants’ motivations for enrolling and further elucidate barriers to engagement in various stages of the PrEP-UP intervention cascade.
Results of our exploratory analyses revealed potential insights for next steps for PrEP interventions tailored for women. Women with self-perceived and objective high risk for HIV were more likely to report PrEP interest and/or accept offer of a PrEP care appointment. This may indicate that women who are at high risk for HIV are aware of their risk and may see the potential utility of PrEP in decreasing their risk. It is possible that focusing on women with high levels of HIV-related worry and self-perceived risk and/or those who engage in condomless sex or exchange sex, with careful attention to other intersections that have been associated with risk such as drug use, may result in greater engagement in the intervention and ultimately PrEP uptake [56, 61–64]. It was surprising that women who had previously heard of or used PrEP as well as those who had recently seen a health care provider were less likely to report PrEP interest and/or accept a PrEP appointment. One potential explanation is that providers may not be doing an adequate job of assessing, educating, or referring women for PrEP, and that interactions with health care providers around PrEP may actually be discouraging PrEP use. Past research has demonstrated inequities in PrEP prescribing, and that women, especially Black and Latina women, are less likely to receive PrEP [65], and that physicians are less willing to prescribe PrEP to persons who inject drugs [66]. In addition, a survey among medical students found that physicians were less willing to prescribe PrEP to patients who did not report consistent condom use and patients who had multiple partners, indicating that prescribing PrEP did not match the actual need for PrEP [67]. More research is needed to understand how existing PrEP knowledge or perceptions as well as interactions with health care providers may influence PrEP uptake and the role of Peers in addressing misconceptions about PrEP as well as helping clients advocate for themselves in patient-health care providers interactions.
Despite its strengths, our study has several limitations. First, our intervention was only offered in English which limited the inclusion of monolingual Spanish-speaking participants, who represent about 10% of our partner CBO’s clients. Second, given that we recruited a convenience sample of a specific population, our findings may not be generalizable to other populations of women. Third, most of the women of trans experience recruited were HIV-positive and so we ended up with a small number of trans women receiving the intervention and are, therefore, unable to evaluate differences in engagement in the intervention between cis and trans women. Although, the PrEP-UP intervention was designed to be inclusive of trans women, cis and trans women have different lived realities and these differences could affect interest or engagement in PrEP care. Follow-up interviews with participants who were trans women may help to elucidate unique barriers to engagement in the PrEPUP intervention. Our findings also highlight the urgency of developing and implementing effective culturally responsive interventions to engage trans women in both HIV prevention and treatment.
Conclusions
We designed and implemented an innovative PrEP peer outreach and navigation intervention for women. Peers were able to successfully recruit a cohort of women at high risk for HIV at mobile syringe exchange sites and sex worker and syringe exchange drop-in centers and to deliver brief PrEP education and counseling. However, we found a gap between PrEP interest and being able to connect women to a PrEP care appointment and, ultimately, PrEP. Further study is needed to understand this gap, including exploring innovative ways to deliver PrEP care to women at highest risk for HIV.
Acknowledgements
We are grateful to Tonia Poteat, PhD, PA-C, MPH, and Hilary Surratt, PhD for insightful discussions during the early stages of this project and to Axcel Barboza for his input into planning and implementation phases of this study. The authors would also like to thank colleagues at NDRI for their assistance with Peer training. This project was supported by a Centers for Disease Control and Prevention Minority HIV/AIDS Research Initiative Grant (1U01PS005111-01).
Footnotes
Compliance with Ethical Standards
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the Albert Einstein College of Medicine IRB and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- 1.Deutsch MB, Glidden DV, Sevelius J, Keatley J, McMahan V, Guanira J, et al. HIV pre-exposure prophylaxis in transgender women: a subgroup analysis of the iPrEx trial. Lancet HIV. 2015;2(12):e512–e519519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thomson KA, Baeten JM, Mugo NR, Bekker L-G, Celum CL, Heffron R. Tenofovir-based oral preexposure prophylaxis prevents HIV infection among women. Curr Opin HIV AIDS. 2016;11(1):18–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baeten JM, Donnell D, Ndase P, Mugo NR, Campbell JD, Wangisi J, et al. Antiretroviral prophylaxis for HIV prevention in hetero-sexual men and women. N Engl J Med. 2012;367(5):399–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thigpen MC, Kebaabetswe PM, Paxton LA, Smith DK, Rose CE, Segolodi TM, et al. Antiretroviral preexposure prophylaxis for heterosexual HIV transmission in Botswana. N Engl J Med. 2012;367(5):423–34. [DOI] [PubMed] [Google Scholar]
- 5.Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Auerbach JD, Kinsky S, Brown G, Charles V. Knowledge, atti-tudes, and likelihood of pre-exposure prophylaxis (PrEP) use among US women at risk of acquiring HIV. AIDS Patient Care STDs. 2015;29(2):102–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sevelius JM, Keatley J, Calma N, Arnold E. ’I am not a man’: trans-specific barriers and facilitators to PrEP acceptability among transgender women. Glob Public Health. 2016;11(7–8):1060–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Flash CA, Stone VE, Mitty JA, Mimiaga MJ, Hall KT, Krakower D, et al. Perspectives on HIV prevention among urban Black women: a potential role for HIV pre-exposure prophylaxis. AIDS Patient Care STDs. 2014;28(12):635–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sevelius JM, Deutsch MB, Grant R. The future of PrEP among transgender women: the critical role of gender affirmation in research and clinical practices. J Int AIDS Soc. 2016;19(6):21105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eaton LA, Matthews DD, Driffin DD, Bukowski L, Wilson PA, Stall RD, et al. A multi-US city assessment of awareness and uptake of pre-exposure prophylaxis (PrEP) for HIV prevention among Black men and transgender women who have sex with men. Prev Sci. 2017;18:505–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Grant RM, Anderson PL, McMahan V, Liu A, Amico KR, Mehrotra M, et al. Uptake of pre-exposure prophylaxis, sexual practices, and HIV incidence in men and transgender women who have sex with men: a cohort study. Lancet Infect Dis. 2014;14(9):820–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mera Giler R, Magnusen D, Trevor H, editors. Changes in Truvada for HIV pre-exposure prophylaxis utilization in the USA: 2012–2016. 9th International AIDS Society Conference on HIV Science (2017). [Google Scholar]
- 13.Wu H, Mendoza MC, Huang YIA, Hayes T, Smith DK, Hoover KW. Uptake of HIV preexposure prophylaxis among commercially insured persons—United States, 2010–2014. Clin Infect Dis. 2016;64(2):144–9. [DOI] [PubMed] [Google Scholar]
- 14.Ya-lin AH. HIV preexposure prophylaxis, by race and ethnicity—United States, 2014–2016. MMWR Morb Mortal Wkly Rep. 2018;67:1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kuhns LM, Reisner SL, Mimiaga MJ, Gayles T, Shelendich M, Garofalo R. Correlates of PrEP indication in a multi-site cohort of young HIV-Uninfected Transgender Women. AIDS Behav. 2015;20:1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. HIV Surveillance Report, 2018 (Updated); vol.31. https://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published May 2020. Accessed July 13 2020. [Google Scholar]
- 17.Becasen JS, Denard CL, Mullins MM, Higa DH, Sipe TA. Estimating the prevalence of HIV and sexual behaviors among the US transgender population: a systematic review and meta-analysis, 2006–2017. Am J Public Health. 2019;109(1):e1–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fauci AS, Redfield RR, Sigounas G, Weahkee MD, Giroir BP. Ending the HIV epidemic. JAMA. 2019;321(9):844. [DOI] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention: US Public Health Service: Preexposure prophylaxis for the prevention of HIV infection in the United States—2017 Update: a clinical practice guideline. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf. Published March 2018.
- 20.Walters SM, Rivera AV, Reilly KH, Anderson BJ, Bolden B, Wogayehu A, et al. Exchange sex among persons who inject drugs in the New York metropolitan area: the importance of local context, gender and sexual identity. AIDS Behav. 2018;22:2773. [DOI] [PubMed] [Google Scholar]
- 21.Juusola JL, Brandeau ML, Owens DK, Bendavid E. The cost-effectiveness of preexposure prophylaxis for HIV prevention in the United States in men who have sex with men. Ann Intern Med. 2012;156(8):541–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Herbst JH, Jacobs ED, Finlayson TJ, McKleroy VS, Neumann MS, Crepaz N. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav. 2008;12(1):1–17. [DOI] [PubMed] [Google Scholar]
- 23.Blackstock OJ, Frew P, Bota D, Vo-Green L, Parker K, Franks J, et al. Perceptions of community HIV/STI risk among U.S women living in areas with high poverty and HIV prevalence rates. J Health Care Poor Underserved. 2015;26(3):811–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.De Santis JP. HIV infection risk factors among male-to-female transgender persons: a review of the literature. J Assoc Nurses AIDS Care. 2009;20(5):362–72. [DOI] [PubMed] [Google Scholar]
- 25.Adimora AA, Schoenbach VJ, Taylor EM, Khan MR, Schwartz RJ, Miller WC. Sex ratio, poverty, and concurrent partnerships among men and women in the United States: a multilevel analysis. Ann Epidemiol. 2013;23(11):716–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li Y, Marshall CM, Rees HC, Nunez A, Ezeanolue EE, Ehiri JE. Intimate partner violence and HIV infection among women: a systematic review and meta-analysis. J Int AIDS Soc. 2014;17(1):18845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Walters SM, Reilly KH, Neaigus A, Braunstein S. Awareness of pre-exposure prophylaxis (PrEP) among women who inject drugs in NYC: the importance of networks and syringe exchange programs for HIV prevention. Harm Reduct J. 2017;14(1):40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wilson EC, Jin H, Liu A, Raymond HF. Knowledge, indications and willingness to take pre-exposure prophylaxis among transwomen in San Francisco, 2013. PLoS ONE. 2015;10(6):e0128971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bazzi AR, Biancarelli DL, Childs E, Drainoni M- L, Edeza A, Salhaney P, et al. Limited knowledge and mixed interest in pre-exposure prophylaxis for HIV prevention among people who inject drugs. AIDS Patient Care STDs. 2018;32:529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Park CJ, Taylor TN, Gutierrez NR, Zingman BS, Blackstock OJ. Pathways to HIV pre-exposure prophylaxis among women prescribed PrEP at an urban sexual health clinic. J Assoc Nurses AIDS Care. 2019;30:321. [DOI] [PubMed] [Google Scholar]
- 31.Rael CT, Martinez M, Giguere R, Bockting W, Maccrate C, Mellman W, et al. Barriers and facilitators to oral PrEP use among transgender women in New York city. AIDS Behav. 2018;22:3627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Park C, Taylor T, Rios N, Khedimi R, Weiss C, Dolce E, et al. , (eds). Perspectives of women prescribed HIV pre-exposure proph-ylaxis (PrEP). Open forum infectious diseases. Oxford: Oxford University Press; 2017. [Google Scholar]
- 33.Braksmajer A, Senn TE, McMahon J. The potential of pre-exposure prophylaxis for women in violent relationships. AIDS Patient Care STDs. 2016;30(6):274–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sevelius JM, Keatley J, Calma N, Arnold E. ‘I am not a man’: trans-specific barriers and facilitators to PrEP acceptability among transgender women. Glob Public Health. 2016;11(7–8):1060–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bradley E, Forsberg K, Betts JE, DeLuca JB, Kamitami E, Por-ter SE, et al. Factors affecting pre-exposure prophylaxis implementation for women in the United States: a systematic review. J Women’s Health. 2019;28:1272. [DOI] [PubMed] [Google Scholar]
- 36.Aaron E, Blum C, Seidman D, Hoyt MJ, Simone J, Sullivan M, et al. Optimizing delivery of HIV preexposure prophylaxis for women in the United States. AIDS Patient Care STDs. 2018;32(1):16–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bradford JB, Coleman S, Cunningham W. HIV system navigation: an emerging model to improve HIV care access. AIDS Patient Care STDs. 2007;21(s1):S49–S58. [DOI] [PubMed] [Google Scholar]
- 38.Higa DH, Marks G, Crepaz N, Liau A, Lyles CM. Interventions to improve retention in HIV primary care: a systematic review of U.S. studies. Curr HIV/AIDS Rep. 2012;9(4):313–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rajabiun S, Cabral H, Tobias C, Relf M. Program design and evaluation strategies for the special projects of National Significance Outreach Initiative. AIDS Patient Care STDs. 2007;21(s1):9–19. [DOI] [PubMed] [Google Scholar]
- 40.Mayer KH, Chan PA, Patel R, Flash CA, Krakower DS. Evolving models and ongoing challenges for HIV pre-exposure prophylaxis implementation in the United States. J Acquir Immune Deficienc Syndr (1999). 2018;77(2):119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.AIDS United. Best practices for integrating peer navigators into HIV models of care. 2015. https://www.aidsunited.org/data/files/Site_18/PeerNav_v8.pdf.
- 42.HIV Epidemiology Program. HIV Surveillance Annual Report, 2018. New York City Department of Health and Mental Hygeine: New York, NY: November 2019. https://www1.nyc.gov/assets/doh/downloads/pdf/dires/hiv-surveillance-annualreport-2018.pdf. [Google Scholar]
- 43.Daskalakis DC, Blackstock OJ, Askew GL. New York City Health Department urges medical providers to expand the offer of PrEP (pre-exposure prophylaxis) to HIV-negative women. https://www1.nyc.gov/assets/doh/downloads/pdf/hcp/prepforwomen.pdf. Updated February 2018.
- 44.New York State Department of Health AIDS Institute. Clinical Guidelines Program. PrEP to Prevent HIV and Promote Sexual Health. 2019. https://www.hivguidelines.org/prep-for-prevention/?smau=iVVRJrsR2D665MJQ. Accessed July 13 2019.
- 45.DiClemente RJ, Crosby RA, Kegler MC. Emerging theories in health promotion practice and research. Hoboken: Wiley; 2009. [Google Scholar]
- 46.Merriam SB, Bierema LL. Adult learning: linking theory and practice. Hoboken: Wiley; 2013. [Google Scholar]
- 47.New York City Health Training. T-Tap Course Directory. 2020. https://nychealthtraining.org/ttap-training-course-directory. Accessed 13 July 2013.
- 48.New York State Department of Health. HIV Education and Training. 2020. https://www.health.ny.gov/diseases/aids/general/about/education.htm. Accessed 13 July 2013.
- 49.Golub S (2016). Understanding Implementation of HIV Prevention Navigation in STD Clinics [National Institutes of Health; Grant R01MH106380-02S1]. [Google Scholar]
- 50.The Center Advancing LGBT Health Colorado (2014) Colorado Transgender Health Survey [Google Scholar]
- 51.National Institute on Drug Abuse. HIV Risk Behaviors/ Perception of Risks Questionnaire [Seek, Test, Treat and Retain for Vulnerable Populations: Data Harmonization Measure] (2015).
- 52.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41:1284–92. [DOI] [PubMed] [Google Scholar]
- 53.Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder. Arch Intern Med. 2006;166(10):1092. [DOI] [PubMed] [Google Scholar]
- 54.Shakil A, Bardwell J, Sherin K, Sinacore JM, Zitter R, Kindratt TB. Development of Verbal HITS for intimate partner violence screening in family medicine. Fam Med. 2014;46(3):180–5. [PubMed] [Google Scholar]
- 55.Golub S. Intervention to Enhance PrEP Uptake and Adherence in a Community-based Setting [National Institutes of Health Grant R01AA022067] (2012). [Google Scholar]
- 56.Chinazo OC, John-Paul S, Xuan L, Daliah H, Nancy LS. Medical and support service utilization in a medical program targeting marginalized HIV-infected Individuals. J Health Care Poor Underserved. 2008;19(3):981–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Greenfield L, Brady JV, Besteman KJ, De Smet A. Patient retention in mobile and fixed-site methadone maintenance treatment. Drug Alcohol Depend. 1996;42(2):125–31. [DOI] [PubMed] [Google Scholar]
- 58.Hall G, Neighbors CJ, Iheoma J, Dauber S, Adams M, Culleton R, et al. Mobile opioid agonist treatment and public funding expands treatment for disenfranchised opioid-dependent individuals. J subst Abuse Treat. 2014;46(4):511–5. [DOI] [PubMed] [Google Scholar]
- 59.Maru DSR, Bruce RD, Walton M, Mezger JA, Springer SA, Shield D, et al. Initiation, adherence, and retention in a randomized controlled trial of directly administered antiretroviral therapy. AIDS Behav. 2008;12(2):284–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Roth AM, Aumaier BL, Felsher MA, Welles SL, Martinez-Donate AP, Chavis M, et al. An exploration of factors impacting preexposure prophylaxis eligibility and access among syringe exchange users. Sex Transm Dis. 2018;45(4):217–21. [DOI] [PubMed] [Google Scholar]
- 61.Strathdee SA, Sherman SG. The role of sexual transmission of HIV infection among injection and non-injection drug users. J Urban Health. 2003;80(3):7–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kral AH, Bluthenthal RN, Lorvick J, Gee L, Bacchetti P, Edlin BR. Sexual transmission of HIV-1 among injection drug users in San Francisco, USA: risk-factor analysis. Lancet. 2001;357(9266):1397–401. [DOI] [PubMed] [Google Scholar]
- 63.Hill MJ, Holt M, Hanscom B, Wang Z, Cardenas-Turanzas M, Latkin C. Gender and race as correlates of high risk sex behaviors among injection drug users at risk for HIV enrolled in the HPTN 037 study. Drug Alcohol Depend. 2018;183:267–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Neaigus A, Reilly KH, Jenness SM, Hagan H, Wendel T, Gelpi-Acosta C. Dual HIV risk: receptive syringe sharing and unprotected sex among HIV-negative injection drug users in New York City. AIDS Behav. 2013;17(7):2501–9. [DOI] [PubMed] [Google Scholar]
- 65.Caponi M, Burgess C, Leatherwood A, Molano LF. Demographic characteristics associated with the use of HIV pre-exposure prophylaxis (PrEP) in an urban, community health center. Prev Med Rep. 2019;15:100889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Edelman EJ, Moore BA, Calabrese SK, Berkenblit G, Cunningham C, Patel V, et al. Primary care physicians’ willingness to prescribe HIV pre-exposure prophylaxis for people who inject drugs. AIDS Behav. 2016;21:1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Calabrese SK, Earnshaw VA, Underhill K, Krakower DS, Magnus M, Hansen NB, et al. Prevention paradox: medical students are less inclined to prescribe HIV pre-exposure prophylaxis for patients in highest need. J Int AIDS Soc. 2018;21(6):e25147. [DOI] [PMC free article] [PubMed] [Google Scholar]


