Abstract
OBJECTIVES:
To examine how medical complexity modifies the relationship between enrollment in Department of Veterans Affairs (VA) home-based primary care (HBPC) and hospitalization for ambulatory care–sensitive conditions (ACSC) for veterans with diabetes mellitus and whether the effect of HBPC on hospitalizations varies according to clinical condition.
DESIGN:
Retrospective cohort study.
SETTING:
VA and non-VA hospitals.
PARTICIPANTS:
VA beneficiaries aged 67 and older with diabetes mellitus and enrolled in Medicare (N = 364,972).
MEASUREMENTS:
Instrumental variables regression models were used to estimate the effect of HBPC enrollment on hospitalization for ACSCs (defined according to the Agency for Healthcare Research and Quality Prevention Quality Indicators) overall and in subgroups stratified according to medical complexity. Models were also estimated for each ACSC to determine which conditions were most sensitive to HBPC. Distance from the veteran’s residence to the nearest HBPC site was used as the instrumental variable.
RESULTS:
HBPC was associated with fewer ACSC hospitalizations (odds ratio (OR) = 0.35 per person-month, 95% confidence interval (CI) = 0.30–0.42). For veterans in the highest quartile of medical complexity, HBPC enrollment was associated with fewer ACSC hospitalizations (OR = 0.43, 95% CI = 0.19–0.93), whereas for those in the lowest quartile, HBPC was associated with more ACSC hospitalizations (OR = 33.2, 95% CI = 4.6–240.1). HBPC enrollment was associated with fewer hospitalizations for a range of ACSCs.
CONCLUSION:
HBPC enrollment was associated with fewer hospitalizations for a range of ACSCs in veterans with diabetes mellitus but only in the most medically complex individuals. This demonstrates the importance of appropriate targeting and suggests that the effect of HBPC is attributable to its comprehensive approach rather than condition-specific interventions.
Keywords: frail elderly adults, home care services, chronic disease, person-centered care, policy
Older adults with multiple chronic diseases are frequently hospitalized and account for a large proportion of healthcare costs.1,2 As the number of older Americans increases, hospital care for high-risk older adults will account for a growing share of healthcare spending. A frequently promoted solution is to intensify outpatient care for these individuals with the hope that this will prevent avoidable hospitalizations and there by reduce costs.3 Decisions about which people to target can determine whether a program will reduce overall spending.4
Department of Veterans Affairs Home-Based Primary Care (HBPC) is an integrated primary care model for older adults at high risk of hospitalization that provides comprehensive, longitudinal primary care by a physician-supervised interdisciplinary team of VA staff in the homes of veterans with complex, chronic, disabling disease.5 Enrollment in VA HBPC is associated with a significant reduction in hospitalization risk,6,7 and early evaluation of the Independence at Home demonstration of HBPC for Medicare beneficiaries demonstrated overall cost savings,8 but there is substantial variation in practice characteristics and participant selection within and between HBPC pro-grams.9,10 Although most HBPC enrollees are elderly, have multiple chronic conditions, and are homebound, it is not known which benefit the most from enrollment or which chronic conditions are most affected.
This study examined how hospitalization risk, determined according to medical complexity, modified the association between VA HBPC enrollment and hospitalizations for ambulatory care–sensitive conditions (ACSCs; hospitalizations that are potentially avoidable with timely and appropriate ambulatory care) in a cohort of older adults with diabetes mellitus. Which ACSC hospitalizations VA HBPC affected most was further investigated. The objective was to facilitate cost-effective targeting and design of HBPC and intensive ambulatory care models more broadly.
METHODS
Study Design and Data Sources
This was a national retrospective cohort study of HBPC use in older veterans with diabetes mellitus. To assess how medical complexity modifies the effect of HBPC on ACSC hospitalizations, a model was first developed to predict ACSC hospitalization risk based on comorbidity scores. The cohort was then divided into quartiles based on this risk score, and the effect of HBPC enrollment on ACSC hospitalizations was estimated in each quartile. Finally, separate models were developed for each ACSC hospitalization in the entire cohort, controlling for comorbidities, to better understand which conditions HBPC had the greatest effect on.
Data were used from VA outpatient visit, hospitalization, and pharmacy data files, as well as Medicare claims, because VA beneficiaries also use non-VA facilities,11 The VA Boston and VA Portland Healthcare System institutional review boards approved the study protocol.
Cohort
All veterans who received a prescription for diabetes mellitus medication (metformin, any sulfonylurea, any thiazolidinedione, any formulation of insulin) through the VA in 2005 or 2006, which was considered the baseline year, were identified. The follow-up period was specified as starting at the end of the baseline year (January 1, 2006, for Baseline Year 2005 participants; January 1, 2007, for Baseline Year 2006 participants) and ending on December 31, 2010. The analysis was focused on veterans with diabetes mellitus because it is common in the population and in HBPC enrollees (48% of enrollees) and is associated with greater healthcare use. Additionally, appropriate ambulatory management of diabetes mellitus and diabetes mellitus–related cardiovascular complications can prevent hospitalization.12–14 Veterans who were aged 67 and older, were traditional Medicare beneficiaries, and primarily used a VA Medical Center that offered HBPC were included. Those who lived farther than 500 miles from the nearest VA providing HBPC were excluded.
Home-Based Primary Care
HBPC is a national, intensive, interdisciplinary home care program. Designed to meet the needs of veterans who cannot practically receive care in an ambulatory setting, HBPC typically targets older adults with multiple medical conditions and functional disability at high risk of being institutionalized. Primary care physicians typically refer individuals to HBPC, or they are referred at hospital discharge, and HBPC clinicians consider whether to enroll referred individuals based on personal factors, program capabilities, and program capacity.
HBPC enrollment was defined as a minimum of two HBPC encounters during the follow-up period with the first HBPC encounter occurring within 6 months of the baseline year to ensure that the baseline-measured comorbidities were current at the time of HBPC enrollment. Because the goal was to compare new HBPC enrollees with non-HBPC individuals, individuals who received HBPC during the baseline year were excluded.
Risk Adjustment Covariates
Additional control variables computed during the baseline year were age, sex, race, and VA service connection status (presence of disability incurred during military service), which can affect VA benefit eligibility. Comorbidities included 29 Elixhauser indicators of physical and mental health conditions15 and eight indicator variables for the components of the Young Diabetes Complications Severity Index.16
Outcome
The outcome of interest was ACSC hospitalizations. Using the Agency for Healthcare Research and Quality prevention quality indicators,17,18 admissions to VA and non-VA hospitals for an ACSC in VA and Medicare claims during the follow-up period were analyzed. All ACSC hospitalizations were analyzed as a composite measure, and each ACSC hospitalization was examined separately.
Instrumental Variable Analysis
Selection bias is a threat to the validity of analyses, because people are referred to HBPC for factors that put them at risk of hospitalization. Information on some of these factors, such as age and prevalence of comorbidities, was available for analysis, but metrics for functional impairment, healthcare trajectory, and severity of illness were not available in the data. Without controlling for unmeasured confounding, it is possible to conclude that HBPC enrollment is associated with greater hospitalization risk, when this actually reflects that HBPC enrollees are sicker than controls in unmeasured ways, so it was decided to use an instrumental variable analysis.
An instrumental variable (or instrument) is a factor that is highly associated with treatment (HBPC) but is unrelated to the outcome (hospitalization) except through the treatment and unrelated to any measured or unmeasured confounders. In the first stage of an instrumental variable analysis, the variation in treatment due to the instrument is estimated, and the second stage estimates the association between treatment and outcome, explicitly controlling for the influence of unmeasured confounders. Distance from the Veteran’s residence to the nearest HBPC program was used as the instrument, because it was hypothesized that this would be highly related to HBPC enrollment but random in relation to hospitalization risk and the prevalence of measured and unmeasured confounders.
To ensure that the instrument was valid, a logistic regression that evaluated the association between distance from the veteran’s residence to the nearest HBPC site and HBPC enrollment was first performed.19 The further a veteran lived from an HBPC site, the less likely they he or she was to be enrolled in HBPC (Table 1). Then measured comorbidities stratified according to median distance from the nearest HBPC site were examined (Table 2), and no systematic relationship was found. In addition, the rate of ACSC hospitalizations of participants who lived less than the median distance of 28.4 miles from the nearest HBPC program (13.8%) was similar to the rate of those who lived 28.4 miles or more from the nearest program (13.7%) (≥1 ACSC hospitalizations in 1 year).
Table 1.
Association Between Distance from Veteran’s Residence to Nearest Home-Based Primary Care (HBPC) Program and HBPC Enrollment
| Miles (Reference <5) | Odds of HBPC Enrollment (95% Confidence Interval) |
|---|---|
| 5–9 | 0.85 (0.78–0.92) |
| 10–29 | 0.55 (0.51–0.59) |
| 30–49 | 0.20 (0.18–0.22) |
| 50–99 | 0.10 (0.09–0.11) |
| ≥100 | 0.03 (0.03–0.03) |
Adjusted for participant demographic characteristics, Veterans Affairs facility, service connection, month, and year.
Table 2.
Participant Characteristics According to Home-Based Primary Care (HBPC) Enrollment and Median Distance from Nearest HBPC Program
| No HBPC, n = 360,399 | HBPC, n = 4,573 | <28.4 Miles from Nearest HBPC, n = 182,453 | ≥28.4 Miles from Nearest HBPC, n = 182,519 | |
|---|---|---|---|---|
| Age, mean | 70.9 | 76.0 | 70.9 | 71.1 |
| Male, % | 98.1 | 96.9 | 97.8 | 98.4 |
| Comorbidity, % | ||||
| Congestive heart failure | 18.4 | 39.9 | 18.1 | 19.3 |
| Cardiac arrhythmia | 23.9 | 38.6 | 24.1 | 24.1 |
| Cardiac valve disease | 10.8 | 14.6 | 10.7 | 11.0 |
| Pulmonary circulatory disorder | 2.0 | 4.6 | 1.94 | 2.0 |
| Hypertension | 85.9 | 89.4 | 85.8 | 86.0 |
| Paralysis | 1.8 | 8.0 | 2.0 | 1.8 |
| Other neurological disorder | 6.2 | 16.5 | 6.5 | 6.1 |
| Chronic pulmonary disorder | 26.4 | 41.0 | 25.1 | 28.1 |
| Hypothyroidism | 9.6 | 11.8 | 9.5 | 9.7 |
| Renal failure | 10.9 | 20.5 | 11.6 | 10.4 |
| Liver disease | 2.9 | 3.5 | 3.3 | 2.6 |
| Peptic ulcer disease | 2.4 | 3.6 | 2.4 | 2.5 |
| Acquired immunodeficiency syndrome | 0.3 | 0.1 | 0.4 | 0.2 |
| Lymphoma | 1.0 | 1.1 | 1.0 | 0.9 |
| Cancer: metastatic | 1.2 | 1.6 | 1.3 | 1.2 |
| Cancer: solitary tumor | 17.8 | 21.3 | 18.4 | 17.2 |
| Rheumatoid arthritis | 2.8 | 3.4 | 2.8 | 2.9 |
| Coagulopathy | 4.4 | 8.6 | 4.7 | 4.3 |
| Obesity | 20.9 | 23.3 | 21.1 | 20.7 |
| Weight loss | 3.0 | 8.0 | 3.3 | 2.8 |
| Fluid or electrolyte disorder | 12.2 | 27.6 | 12.7 | 12.0 |
| Blood loss anemia | 1.5 | 2.5 | 1.5 | 1.5 |
| Iron-deficiency anemia | 18.5 | 34.0 | 19.8 | 17.6 |
| Alcohol abuse | 3.9 | 4.1 | 4.6 | 3.2 |
| Drug abuse | 2.1 | 1.6 | 2.7 | 1.4 |
| Psychosis | 12.6 | 23.9 | 14.5 | 11.0 |
| Depression | 15.0 | 29.5 | 15.2 | 15.1 |
Statistical Models
Outcomes were analyzed using a two-stage discrete-time survival model with an instrumental variable. The first stage was a logistic regression that predicted HBPC enrollment in a given month and distance from the veteran’s primary residence to the nearest VA facility that provides HBPC. The second stage was a logistic regression that predicted hospitalization for an ACSC in a given month based on demographic characteristics, comorbidities, and HBPC enrollment, controlling for unobserved factors from the first stage. Participants were censored after enrollment in Medicare Advantage or death. Month and year fixed effects were included to account for seasonal changes and secular trends, and VA Medical Center was included as a fixed effect to account for facility effects. Because the outcome equations were nonlinear, the two-stage residual inclusion technique was used for instrumental variable estimation.20,21 As an additional sensitivity analysis, a single-stage multivariable logistic regression was performed using HBPC enrollment as the independent variable and ACSC hospitalization as the outcome (Table S1). Analyses were performed using Stata (Stata Corp, College Station, TX).
Risk Score
After building the two-stage model for the entire sample, a risk score for ACSC hospitalization was developed based on Elixhauser comorbidities using the results of the second-stage model. For each Elixhauser comorbidity, the beta coefficient was multiplied by 10 and rounded to the nearest integer (Table S2), which generated a score with a range of −2 to 27. The cohort was then stratified into quartiles based on this risk score. To assess the effect of HBPC on ACSC hospitalization at different levels of medical complexity, the second-stage regression predicting hospitalization for ACSCs in each quartile was reestimated. In this model, participant demographic characteristics, service connected status, year, and month, but not Elixhauser comorbidities, were included.
RESULTS
Participant Characteristics
Three hundred sixty-four thousand nine hundred seventytwo veterans with a total of 16,587,706 person-months of follow-up were identified for analysis; 4,573 of these were enrolled in HBPC, and 360,399 were not (Table 2). HBPC enrollees were older (mean 76.0 vs 70.9) and had more coexisting conditions, including congestive heart failure (CHF) (39.9% vs 18.4%), chronic pulmonary disorder (41.0% vs 26.4%), renal failure (20.5% vs 10.9%), and paralysis (8.0% vs 1.8%) (Table 2). HBPC enrollees also had a higher prevalence of mental illness, including psychosis (23.9% vs 12.6%) and depression (29.5% vs 15.0%).
ACSC Risk Score Development
The Elixhauser comorbidities that were most strongly associated with ACSC hospitalization were CHF (odds ratio (OR) = 1.86, 95% confidence interval (CI) = 1.86–1.92), chronic pulmonary disease (OR = 1.86, 95% CI = 1.79–1.84), and pulmonary circulatory disorder (OR = 1.30, 95% CI = 1.26–1.34). Significant negative predictors of ACSC hospitalization included hypertension (OR = 0.96, 95% CI = 0.94–0.98) and obesity (OR = 0.97, 95% CI = 0.96–0.99). Second-stage regression results and ACSC risk score calculations are presented in Table S1.
ACSC Risk Score and Stratified Participant Characteristics
ACSC risk scores ranged from −2 to 27 (median 1, interquartile range (IQR) 0–7). Median risk score was 7 (IQR 10–12) for HBPC enrollees and 1 (IQR 0–6) for non-HBPC enrollees. Risk score quartile ranges, median risk score according to quartile and HBPC status, and participant characteristics stratified according to risk score quartile are presented in Table 3. Participants in the first quartile were older than those in higher risk strata, nearly all had hypertension, and few had a third comorbidity, most commonly obesity or solitary tumor. In the second quartile, many participants also had mental health diagnoses, iron-deficiency anemia, and cardiac arrhythmias. In the third quartile, a higher proportion of participants had multiple comorbidities, but some participants also had several new conditions such as chronic pulmonary disease and drug abuse. In the fourth quartile, a high proportion of participants had multiple comorbidities, and a large majority had CHF and chronic pulmonary disease. Half of HBPC-enrolled participants were in the highest-risk quartile.
Table 3.
Ambulatory-Care Sensitive Conditions Risk Score and Selected Participant Characteristics Stratified According to Risk Score Quartile
| Characteristic | Quartile 1 |
Quartile 2 |
Quartile 3 |
Quartile 4 |
||||
|---|---|---|---|---|---|---|---|---|
| No HBPC, n = 83,345 | HBPC, n = 286 | No HBPC, n = 102,904 | HBPC, n = 791 | No HBPC, n = 84,775 | HBPC, n = 1,165 | No HBPC, n = 89,375 | HBPC, n = 2,300 | |
| Age, mean | 71.1 | 77.1 | 69.4 | 75.4 | 70.5 | 75.3 | 72.7 | 76.4 |
| Number of comorbidities, mean | 1.52 | 1.59 | 2.30 | 2.81 | 3.67 | 4.38 | 6.05 | 6.77 |
| Comorbidity, % | ||||||||
| Congestive heart failure | 0.0 | 0.0 | 0.0 | 0.0 | 11.1 | 12.3 | 63.8 | 72.5 |
| Cardiac arrhythmia | 0.0 | 0.0 | 11.9 | 9.2 | 25.5 | 31.9 | 58.3 | 56.7 |
| Hypertension | 99.9 | 100.0 | 72.8 | 85.5 | 84.0 | 87.1 | 88.9 | 90.3 |
| Chronic pulmonary disorder | 0.0 | 0.0 | 0.0 | 0.0 | 37.4 | 18.9 | 71.0 | 71.4 |
| Renal failure | 4.2 | 6.6 | 6.1 | 9.0 | 10.6 | 17.5 | 22.3 | 27.4 |
| Obesity | 19.9 | 21.0 | 19.7 | 20.5 | 21.3 | 19.8 | 23.5 | 27.0 |
| Fluid or electrolyte disorder | 0.0 | 0.0 | 2.9 | 5.0 | 14.6 | 23.8 | 31.8 | 41.0 |
| Deficiency anemia | 0.0 | 0.0 | 14.7 | 17.1 | 21.4 | 30.7 | 36.6 | 44.9 |
| Drug abuse | 0.0 | 0.0 | 0.0 | 0.0 | 4.7 | 1.5 | 3.9 | 2.4 |
| Psychosis | 0.0 | 0.0 | 15.7 | 24.0 | 16.2 | 27.5 | 18.1 | 25.5 |
| Depression | 0.0 | 0.0 | 17.2 | 22.7 | 18.7 | 30.2 | 23.6 | 35.4 |
Model also included age, demographic characteristics, service connection, Veterans Affairs facility, month, year, and the Elixhauser comorbidities pulmonary circulatory disorder, paralysis, other neurological condition, hypothyroidism, liver disease, peptic ulcer disease, acquired immunodeficiency syndrome, lymphoma, metastatic cancer, solitary tumor, rheumatoid arthritis, weight loss, blood loss anemia, and alcohol abuse.
HBPC = Home-Based Primary Care.
HBPC Enrollment and Risk of ACSC Hospitalization
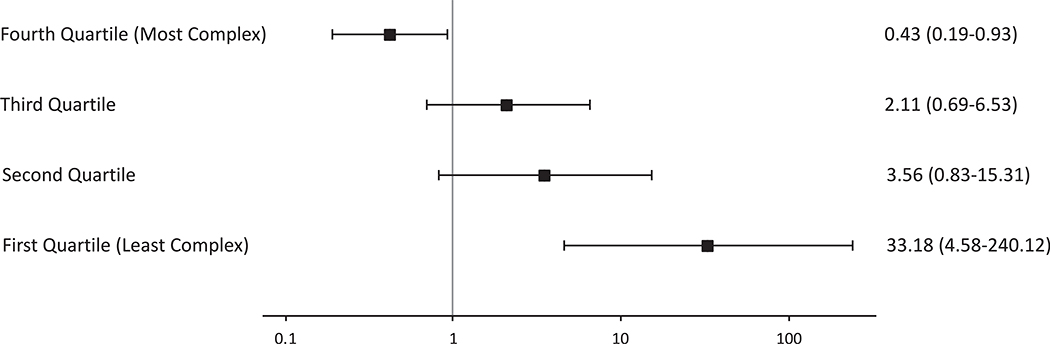
HBPC enrollment was associated with significantly lower odds of ACSC hospitalization (OR = 0.35, 95% CI = 0.30–0.42). The magnitude and significance of HBPC as a predictor of ACSC hospitalization stratified according to risk score quartile is presented in Figure 1. In the first, or least-complex, quartile, HBPC enrollment was associated with significantly greater odds of ACSC hospitalization (OR = 33.18, 95% CI = 4.58–240.12). In the second and third quartiles, no significant association was observed (second quartile OR = 3.56, 95% CI = 0.83–15.31, third quartile OR = 2.11, 95% CI = 0.69–6.53). In the highest quartile, HBPC enrollment was associated with significantly lower odds of hospitalization (OR = 0.43, 95% CI = 0.19–0.93).
Figure 1.
Effect of HBPC on total ACSC Hospitalizations, by quartile of ACSC risk score. *Results presented as adjusted odds ratios (95% confidence intervals) representing relative probability of hospitalization with versus without HBPC, within risk quartiles. HBPC, Home-Based Primary Care; ACSC, Ambulatory Care Sensitive Conditions.
Risk of Hospitalization for Individual ACSCs
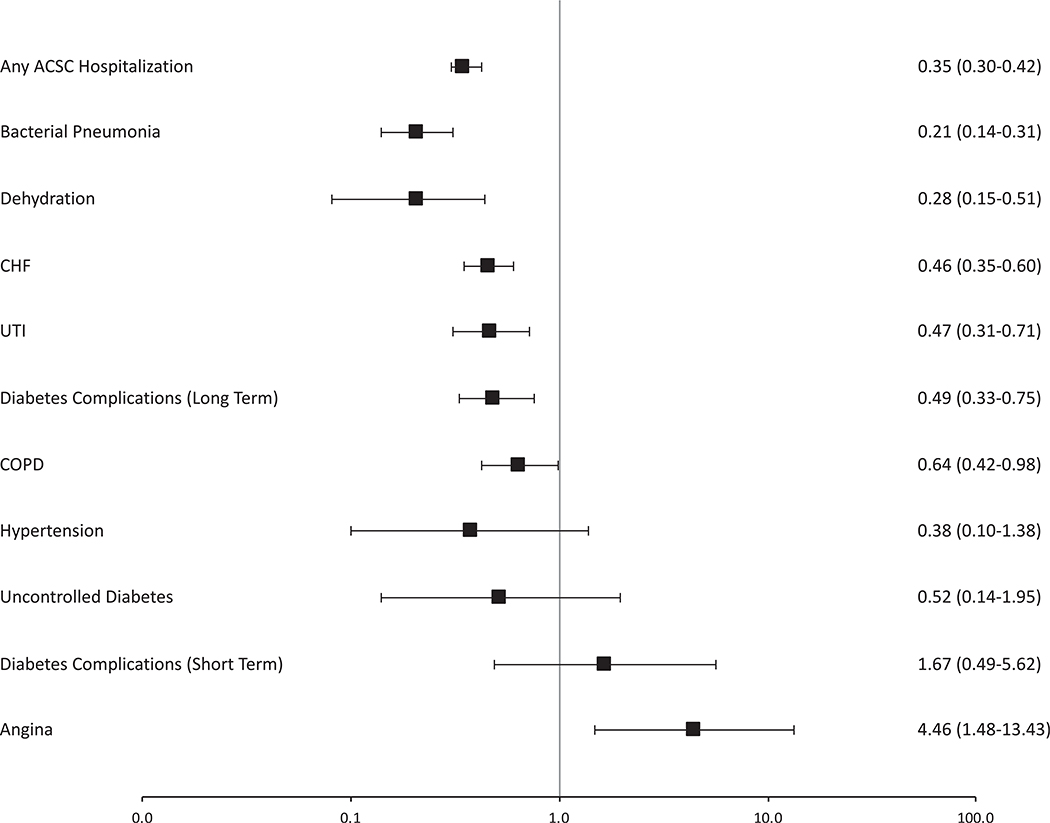
The effects of HBPC on hospitalization for each ACSC are presented in Figure 2. HBPC was associated with significant lower odds of hospitalization for CHF, bacterial pneumonia, chronic pulmonary disease, long-term diabetes mellitus complications, urinary tract infection, and dehydration. HBPC enrollment was associated with significant greater odds of hospitalization for angina pectoris (OR = 4.46, 95% CI = 1.48–13.43). HBPC enrollment was associated with nonsignificantly greater odds of hospitalization for short-term diabetes mellitus complications and nonsignificantly lower odds of hospitalization for uncontrolled diabetes mellitus and perforated appendix. There were inadequate events to model the effect of HBPC on hospitalization for lower extremity amputation or asthma.
Figure 2.
Effect of HBPC enrollment on individual ACSC hospitalizations. *Each row represents a separate model with each listed ACSC hospitalization serving as dependent variable, controlling for demographics, Elixhauser comorbidities, service connected status, month and year. Results presented as odds ratios with 95% confidence intervals. HBPC, Home-Based Primary Care; ACSC, Ambulatory Care Sensitive Conditions; CHF, Congestive Heart Failure; UTI, Urinary Tract Infection; COPD, chronic obstructive pulmonary disease; DM, diabetes mellitus.
DISCUSSION
This analysis of the effect of HBPC on hospitalizations for ACSC conditions uncovered several important relationships. First, most participants enrolled in HBPC were in the highest quartile of medical complexity, had multiple chronic conditions, and had CHF and chronic pulmonary disease. Second, HBPC was associated with significantly lower odds of ACSC hospitalizations overall when controlled for comorbidities, although in the stratified analysis, the effect of HBPC on reducing ACSC hospitalizations was restricted to the highest quartile of risk. Third, for participants in the lowest quartile of risk, HBPC enrollment was associated with greater odds of ACSC hospitalization. Finally, the observed lower odds of ACSC hospitalizations was seen for nearly all diagnostic categories with the exception of angina pectoris.
This study is consistent with and extends prior work. A previous study demonstrated that, in veterans in the highest decile of Centers for Medicare and Medicaid Services hierarchical condition category (HCC) scores, HBPC was associated with a larger reduction in total healthcare costs than in participants in lower deciles.7 Similarly, in a HBPC program in Washington, District of Columbia, enrollment was associated with 17% lower total healthcare costs and 9% fewer hospitalizations for the highestcost Medicare beneficiaries.22,23 The current work corroborates the concept that HBPC may be most effective in reducing costs in these sickest individuals and that there is no evidence of a ceiling effect, where high medical complexity exceeds the capacity of HBPC to prevent hospital admissions.
Conversely, in the lowest quartile of risk, HBPC enrollment was associated with greater odds of hospitalization. This group had relatively few HBPC enrollees and a lower hospitalization rate, leading to a less-precise, but still statistically significant estimate of the effect of HBPC. The participants in this group were elderly but had few other chronic conditions than diabetes mellitus, the most common being hypertension and obesity. This could be interpreted in several ways. First, exposure to a moreintense care model with more-frequent contacts may give healthcare providers the opportunity to identify new problems and disease exacerbations that otherwise would have gone undiscovered, leading to hospitalizations. Hence these hospitalizations may represent appropriate and high-quality care. Alternatively, it is possible that more exposure to healthcare providers through HBPC induced hospitalizations that may not have been necessary. Overall, targeting the most medically complex individuals at the highest risk of hospitalization is associated with larger and more-consistent reductions in hospitalizations for ACSCs.
To be enrolled in HBPC, individuals are referred by their primary care physician or upon hospital discharge and are subsequently evaluated for admission by HBPC staff using a standardized screening tool. Physician referral can be a suboptimal method of identifying high-risk individuals, because referral decisions can be inconsistent,24 and physicians often refer individuals who are less medically complex than those identified using other methods, such as prediction models.25,26 The current study data demonstrate that, in a sample of older veterans with diabetes mellitus, a majority of HBPC enrollees are in the highest risk quartile for ACSC hospitalization and that, for these individuals, HBPC enrollment is associated with lower odds of hospitalization. This suggests that overall HBPC enrollment procedures are identifying most individuals appropriately, but better enrollee selection methods could increase the effect of HBPC on ACSC hospitalizations.
Examining the individual ACSC diagnostic categories shows that HBPC is associated with fewer ACSC hospitalizations, including exacerbations of chronic conditions such as CHF and chronic pulmonary disease and infectious diseases such as bacterial pneumonia and urinary tract infection. There is increasing evidence that the current health system’s focus on individual diseases leads to poor coordination and integration of care and that an increased focus on comprehensive management of multimorbidity is needed.27–29 The current study data demonstrate that comprehensive care programs such as HBPC affect a range of hospitalizations with varied etiologies. Significantly greater odds of hospitalization for angina pectoris was associated with HBPC enrollment. Chest pain is a potentially life-threatening symptom, and differentiating acute coronary syndromes from less-serious conditions requires advanced diagnostic tools often available only in a hospital. Hence, the greater frequency of participant contact in HBPC may have led to hospital referral for chest pain, and less-severe cases may have been coded as angina pectoris. Additionally coding changes over time for angina pectoris had led to AHRQ dropping this measure from the prevention quality indicators in future years.
This work has some limitations. Although the instrumental variable approach has been validated previously6 and appeared valid in the current study, an unknown association between the instrument and hospitalizations for an ACSC in principle could threaten the validity of the findings. Second, the analysis is restricted to individuals with diabetes mellitus. Although this work shows lower odds of hospitalization for chronic conditions other than diabetes mellitus, we cannot directly comment on the effect of HBPC in a population without diabetes mellitus. Additionally, VA HBPC may differ from community-based HBPC practices in financing, organization, and service delivery,10 which may limit the generalizability of these results, although appropriate participant selection is relevant for a variety of high-intensity primary care models.22 Finally, although the analysis demonstrates that individuals with more chronic conditions benefit more from HBPC, the specific combinations or minimum number of clinical conditions at which HBPC is most effective is not known. In addition, because many non-medical factors such as income and social isolation affect hospitalization risk,30 it is not known how HBPC addresses these risk factors and whether this contributes to its effect on reducing hospitalizations.
In conclusion, HBPC is effective in reducing hospitalization for ACSCs in older adults with diabetes mellitus. It is most efficacious in individuals with the highest medical complexity, whereas in less medically complex individuals, HBPC is less effective in preventing hospitalizations and may increase hospitalization rates in some low-risk groups. HBPC reduces a range of different kinds of hospitalizations, reinforcing the concept that comprehensive care models are more effective in preventing hospital use than models focused on a single medical condition. Intensive care models like HBPC, when targeted at the appropriate population, have an important role in the management of medically complex older adults.
Supplementary Material
Table S1. Comparison of multivariable regression and instrumental variable analysis of the impact of HBPC and selected comorbidities on the odds of hospitalization of an hospitalization for an ambulatory care sensitive condition.
Table S2. Selected second stage regression results, and risk score calculations.
ACKNOWLEDGMENTS
We thank Donglin Li for programming support on this project and the members of the VA HBPC Research Interest Group for their feedback on earlier versions of this work. This work was a plenary presentation at the Society for General Internal Medicine National meeting in Hollywood, Florida, May 13, 2016.
Footnotes
Conflict of Interest: None.
Financial Disclosure: Funded by the Department of Veterans Affairs.
Sponsor’s Role: None.
REFERENCES
- 1.Zulman DM, Pal Chee C, Wagner TH et al. Multimorbidity and healthcare utilisation among high-cost patients in the US Veterans Affairs Health Care System. BMJ Open 2015;5:e007771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lehnert T, Heider D, Leicht H et al. Review: Health care utilization and costs of elderly persons with multiple chronic conditions. Med Care Res Rev 2011;68:387–420. [DOI] [PubMed] [Google Scholar]
- 3.Bodenheimer T, Berry-Millett R. Follow the money—Controlling expenditures by improving care for patients needing costly services. N Engl J Med 2009;361:1521–1523. [DOI] [PubMed] [Google Scholar]
- 4.Mukamel DB, Chou CC, Zimmer JG. The effect of accurate patient screening on the cost-effectiveness of case management programs. Gerontologist 1997;37:777–784. [DOI] [PubMed] [Google Scholar]
- 5.Home-Based Primary Care Program. Department of Veterans Affairs. Veterans Health Administration Handbook 114.01 [on-line]. Available at http://www1.va.gov/vhapublications/ViewPublication.asp?pub_ID=1534 Accessed August 1, 2016.
- 6.Edwards ST, Prentice JC, Simon SR et al. Home-based primary care and the risk of ambulatory care-sensitive condition hospitalization among older veterans with diabetes mellitus. JAMA Intern Med 2014;174:1796–1803. [DOI] [PubMed] [Google Scholar]
- 7.Edes T, Kinosian B, Vuckovic NH et al. Better access, quality, and cost for clinically complex veterans with home-based primary care. J Am Geriatr Soc 2014;62:1954–1961. [DOI] [PubMed] [Google Scholar]
- 8.Center for Medicare and Medicaid Innovation. Independence at Home Demonstration Year 1 Practice Results [on-line]. Available at https://innovation.cms.gov/Files/x/iah-yroneresults.pdf Accessed January 20, 2016.
- 9.Kinosian B, Tompkins H, Edes T. Factors associated with reduction in inpatient days by home based primary care. J Am Geriatr Soc 2008;56: S197–S198. [Google Scholar]
- 10.Leff B, Weston CM, Garrigues S et al. ; the National Home-Based Primary Care and Palliative Care Network. Home-based primary care practices in the United States: Current state and quality improvement approaches. J Am Geriatr Soc 2015;63:963–969. [DOI] [PubMed] [Google Scholar]
- 11.Hynes DM, Koelling K, Stroupe K et al. Veterans’ access to and use of Medicare and Veterans Affairs health care. Med Care 2007;45:214–223. [DOI] [PubMed] [Google Scholar]
- 12.Kim S. Burden of hospitalizations primarily due to uncontrolled diabetes: Implications of inadequate primary health care in the United States. Diabetes Care 2007;30:1281–1282. [DOI] [PubMed] [Google Scholar]
- 13.Huang ES, Laiteerapong N, Liu JY et al. Rates of complications and mortality in older patients with diabetes mellitus: The Diabetes and Aging Study. JAMA Intern Med 2014;174:251–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lipska KJ, Ross JS, Wang Y et al. National trends in US hospital admissions for hyperglycemia and hypoglycemia among Medicare beneficiaries, 1999 to 2011. JAMA Intern Med 2014;174:1116–1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Elixhauser A, Steiner C, Harris DR et al. Comorbidity measures for use with administrative data. Med Care 1998;36:8–27. [DOI] [PubMed] [Google Scholar]
- 16.Young BA, Lin E, Von Korff M et al. Diabetes complications severity index and risk of mortality, hospitalization, and healthcare utilization. Am J Manag Care 2008;14:15–23. [PMC free article] [PubMed] [Google Scholar]
- 17.Agency for Healthcare Research and Quality, Department of Health and Human Services. Guide to Prevention Quality Indicators, 3rd Ed. 2007:1–59 [on-line]. Available at http://www.qualityindicators.ahrq.gov/Downloads/Modules/PQI/V31/pqi_guide_v31.pdf Accessed on 5th January, 2017. [Google Scholar]
- 18.Nyweide DJ, Anthony DL, Bynum JPW et al. Continuity of care and the risk of preventable hospitalization in older adults. JAMA Intern Med 2013;173:1879–1885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Patient Centered Outcomes Research Institute Methodology Standards [on-line]. Available at http://www.pcori.org/research-results/research-methodology/pcori-methodology-standards Accessed August 1, 2016.
- 20.Terza JV, Basu A, Rathouz PJ. Two-stage residual inclusion estimation: Addressing endogeneity in health econometric modeling. J Health Econ 2008;27:531–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pizer SD. An intuitive review of methods for observational studies of comparative effectiveness. Health Serv Outcomes Res Method 2009;9:54–68. [Google Scholar]
- 22.De Jonge KE, Jamshed N, Gilden D et al. Effects of home-based primary care on Medicare costs in high-risk elders. J Am Geriatr Soc 2014;62:1825–1831. [DOI] [PubMed] [Google Scholar]
- 23.Kinosian B, Taler G, Boling P et al. Projected savings and workforce transformation from converting independence at home to a Medicare benefit. J Am Geriatr Soc 2016;64:1531–1536. [DOI] [PubMed] [Google Scholar]
- 24.Forrest CB, Nutting PA, von Schrader S et al. Primary care physician specialty referral decision making: Patient, physician, and health care system determinants. Med Decis Making 2006;26:76–85. [DOI] [PubMed] [Google Scholar]
- 25.Freund T, Gondan M, Rochon J et al. Comparison of physician referral and insurance claims data-based risk prediction as approaches to identify patients for care management in primary care: An observational study. BMC Fam Pract 2013;14:157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gharacholou SM, Hellkamp AS, Hernandez AF et al. Use and predictors of heart failure disease management referral in patients hospitalized with heart failure: Insights from the Get With the Guidelines Program. J Card Fail 2011;17:431–439. [DOI] [PubMed] [Google Scholar]
- 27.Starfield B, Lemke KW, Bernhardt T et al. Comorbidity: Implications for the importance of primary care in “case” management. Ann Fam Med 2003;1:8–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barnett K, Mercer SW, Norbury M et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: A cross-sectional study. Lancet 2012;380:37–43. [DOI] [PubMed] [Google Scholar]
- 29.Tinetti ME, Fried TR, Boyd CM. Designing health care for the most common chronic condition—multimorbidity. JAMA 2012;307:2493–2494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Barnett ML, Hsu J, McWilliams JM. Patient characteristics and differences in hospital readmission rates. JAMA Intern Med 2015;175:1803–1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Comparison of multivariable regression and instrumental variable analysis of the impact of HBPC and selected comorbidities on the odds of hospitalization of an hospitalization for an ambulatory care sensitive condition.
Table S2. Selected second stage regression results, and risk score calculations.