Abstract
We aim to highlight the importance of using a process-level view in analyzing distributed healthcare tasks through a case study analysis of medication management (MM). MM during older adults’ hospital-to-skilled-home-healthcare (SHHC) transitions is a healthcare process with tasks distributed across people, organizations, and time. MM has typically been studied at the task level, but a process-level is needed to fully understand and improve MM during transitions. A process-level view allows for a broader investigation of how tasks are distributed throughout the work system through an investigation of interactions and the resultant emergent properties. We studied MM during older adults’ hospital-to-SHHC transitions through interviews and observations with 60 older adults, their 33 caregivers, and 79 SHHC providers at 5 sites associated with 3 SHHC agencies. Study findings identified key cross-system characteristics not observable at the task-level: (1) identification of emergent properties (e.g., role ambiguity, loosely-coupled teams performing MM) and associated barriers; and (2) examination of barrier propagation across system boundaries. Findings highlight the importance of a process-level view of healthcare delivery occurring across system boundaries.
Keywords: Process, Sociotechnical system, Work system, Medication management, System boundaries, Transitional care, Frail elderly, Home care agencies
1. Introduction
Recent years have seen a substantial increase in research focused on improving the safety of transitions of care, particularly for older adults. Despite these efforts, transitions remain a high-risk healthcare process. In particular, unsuccessful medication management (MM) is a persistent contributing factor to suboptimal outcomes for older adults receiving skilled home healthcare (SHHC) services (e.g., nursing, physical therapy) after hospital discharge (Coleman et al., 2005; Schoenborn et al., 2013). MM refers to the ability to successfully obtain, administer, and take medications according to a prescribed regimen. Historically, medication management has been studied at the task level. However, for older adults transitioning to SHHC services after hospital discharge, MM tasks are distributed across people, organizations, and time. To improve MM for these vulnerable older adults, a process-level view of MM is needed.
Carayon (2006) described a process as “a series of tasks performed by individuals using various tools and technologies in a specific environment” (p.17) (Carayon, 2006). Expanding that view to encompass processes within the distributed context of healthcare delivery, Walker and Carayon (2009) underscored the distinction between tasks and processes in the following way:
“Task-focused care is centered on the provider or facility rather than on the patient. The focus on tasks (and payment for isolated tasks) is a fundamental cause of the fragmentation, low quality, and high cost of U.S. health care. On the other hand, process-focused care is centered on the patient. It coordinates the work of many care team members (including patients, physicians, nurses, midlevel providers, lay caregivers, clinical educators, pharmacists, case managers, and call-center personnel) to provide each patient with high-quality, efficient care across time and across all venues of care” (p. 468). (Walker and Carayon, 2009)
This is not to say that we espouse a process-level view to the exclusion of analyzing task interactions. Multiple levels of analysis are critical to understanding the work that occurs within a complex sociotechnical system (Hendrick and Kleiner, 2002; Karsh and Brown, 2010; Kleiner, 2006). Rather, we aim to highlight the importance of using a process-level view in analyzing the distributed tasks associated with healthcare delivery through a case study analysis of a healthcare delivery activity (i.e., MM) typically studied at the task level. In particular, we aim to emphasize the importance of accounting for the distributed nature of healthcare delivery activities in human factors and ergonomics analysis (Walker and Carayon, 2009). The analysis should capture the distribution of tasks as they occur across traditionally-defined system boundaries (i.e., temporal, organizational, person/team. (Carayon, 2006).
The level of interaction within a system often guides how boundaries are defined (Wilson, 2000, 2014; Karsh et al., 2014). Levels of interaction encompass both micro-level interactions (between humans and machines, i.e., cognitive and physical ergonomics), and macro-level interactions (between humans and organizations, e.g., macroergonomics). Carayon (2006) highlighted how the study of interactions across “organizational, geographical, cultural and temporal boundaries increas[es] the number and type of interactions between systems, and therefore amplify[ies] the complexity of work systems” (p. 526) (Carayon, 2006). As work spans system boundaries, the increasing complexity of interactions poses a challenge to identifying and defining the boundaries of the system under investigation. Taking a process-level view may serve to bound the system analysis as complexity increases across system boundaries.
1.1. The importance of accounting for the distributed nature of medication management from the hospital to skilled home healthcare
Previous research has used a task-level view to evaluate MM in single healthcare settings (Meredith et al., 2001; Faye et al., 2010; Caroff et al., 2015; Carayon et al., 2015). However, from a patient-centered perspective, MM activities are distributed and include interactions with various healthcare providers, organizations, and tasks over time. Communication is integral to successful MM and is a process-level activity distributed across people, time, and tasks. Carayon and Wood (2009) referred to this patient-centered view of healthcare delivery as a “patient journey” in which patient care “interactions occur over time, and therefore produce transitions of care that influence each other and accumulate over the journey of the patient care process. (p.29) (Carayon and Wood, 2009).” The hospital-to-SHHC transition highlights the distributed nature of MM tasks. MM occurs across system boundaries over several days and involves multiple organizations (e.g., the hospital, the older adult’s home, the community pharmacy), and occurs over multiple days.
Work often occurs across predefined system boundaries (Carayon, 2006; Olson and Olson, 2000). These boundaries include temporal, geographical, organizational, and cultural boundaries. Boundary-spanning work can have a significant effect on both the work performed and the individuals performing the work (Carayon, 2006; Karsh et al., 2014). Choosing how to define system boundaries is a challenge that has the potential to either facilitate or hinder the design of the boundary-spanning work being studied (Rivera-Rodriguez et al., 2013).
We propose that studying MM at the process level as it occurs across system boundaries will produce insights into optimizing work system design that would be indiscernible with a task-level approach. When we refer to a process-level view, we conceptualize a distributed process that has the following characteristics: 1) unfolds over time; 2) involves the dynamic interaction of multiple system elements (e.g., individuals, tasks, organizational structure, technologies, etc.) (Wilson, 2014; Carayon et al., 2006); 3) has both loosely- and tightly-coupled (Weick,1976) non-linear sub-processes; and 4) occurs across multiple system boundaries (Carayon, 2006). Key tenets of sociotechnical system design such as the emergent properties of systems, identification of variances [i.e., divergences from a standard/normal process or procedure] or barriers [conditions or properties within the system that make work performance challenging, distressing, or unfeasible] (Holden et al., 2013a) distributed interactions, and propagation of variances are not necessarily detectible at the task level of analysis (Hendrick and Kleiner, 2002; Cherns, 1976; Herbst, 1974). Thus, we use MM as a case study to highlight the critical significance of analyzing the distributed tasks of healthcare from a process-level view.
1.2. Case study domain
Skilled home health care (SHHC) is one of the most commonly utilized and poorly understood healthcare delivery models (Carayon, 2012). SHHC is a formal, regulated program of care providing a range of healthcare services to patients (e.g., nursing, physical therapy) in the home, such as wound care, physical therapy after a hip replacement, or medication management (MM) for patients with complex medication regimens (Centers Medicare Medicaid Serv., 2014).
Older adults transitioning to SHHC following hospital discharge are among those at highest risk for experiencing adverse outcomes in the post-discharge period (Murtaugh and Litke, 2002). Unsuccessful MM is a persistent contributing factor to suboptimal outcomes (Coleman et al., 2005; Rosati and Huang, 2007; Bruning and Selder, 2011; Dierich et al., 2011) and is associated with readmission within the first 60 days of receiving SHHC (Rosati and Huang, 2007). Older adults are particularly susceptible to problems with MM. They typically follow complex medical regimens and are hospitalized at a higher rate than the general population, leading to further changes in medication regimens (Coleman et al., 2005; Dierich et al., 2011).
It is not yet clear how a process may change as it occurs across predefined system boundaries. The process of MM during older adults’ hospital-to-SHHC transitions from the hospital to SH involves multiple organizations (e.g., hospital, SHHC agency, older adult’s home) and often occurs across over several days. We do not yet know how crossing these temporal and organizational boundaries may affect the fundamental attributes of the process, or how cross-system barriers will affect the process of MM. For example, there is the potential for barrier propagation at an earlier stage of the process to propagate through the later stages of the process across system boundaries. Propagation refers to the proliferation of variances or barriers from one stage of a process to stages downstream in the process (Kleiner, 2006; Herbst,1974). In the case of MM, having an incorrect medication list at hospital discharge has the potential to transform into multiple barriers downstream in the process once the patient is home from the hospital. A process-level view has the potential to improve the identification of the connections between system boundaries, variances, and errors as they occur across a process (Carayon et al., 2015).
The purpose of this study was to investigate MM during older adults’ transitions from hospital to SHHC as an in-depth case study to highlight the importance of studying healthcare tasks distributed across system boundaries at the process level, while identifying key factors contributing to unsuccessful MM during older adults’ hospital-to-SHHC transitions using a process-level view.
2. Methods
2.1. Design
Data collection took place during older adults’ transitions from the hospital to SHHC. We defined the transition time frame as starting just prior to hospital discharge, extending through the first SHHC home visit (24e48 h after hospital discharge), and ending approximately 24e48 h after the home visit. Data collection took place in the hospital, at the SHHC agency, and in the home.
To capture the MM process as it occurred across system boundaries, the researchers interviewed and observed the work of various individuals in multiple organizations. The researchers embedded themselves within SHHC agencies for week-long periods of time. The researchers shadowed SHHC providers (SHHCPs) at the hospital and at the first SHHC visit, termed the start-of-care visit (or resumption-of-care visit if they had received SHHC in the past). The start-of-care visit was primarily for information gathering. The SHHCP performed several tasks during the visit: inform the patient and informal caregiver about SHHC, set up the electronic health record, assist with MM, identify appropriate services and for what duration, identify the physician who will be overseeing SHHC services, and provide emergency contact information. The focus of the present study was the SHHCP’s performance of a thorough medication reconciliation with the patient to assist with MM. Medication reconciliation in the context of our study was the process of creating an accurate list of all medications the patient was taking at home and comparing that list against the hospital discharge orders. The goal of medication reconciliation was to ensure the patient was taking the correct medications (Institute for Healthcare Improvement, 2016).
We conducted 1) contextual inquiry (Beyer and Holtzblatt,1997) of the SHHC initial home visit, during which researchers observed work being performed and asked probing questions (e.g., to clarify or to gain a more in-depth understanding of what was observed); and 2) semi-structured interviews with patients, in combination with their associated informal caregiver(s) (defined as any nonpaid individual that participated regularly in the care of the patient). We conducted separate interviews with the SHHCP assigned to provide care in the home, the hospital-based SHHCP who initiated patients’ transitions from the hospital, and SHHC administrators and staff involved in transitions. Interviews lasted approximately 45 min and were audiotaped and transcribed.
Semi-structured interview guides were informed by the research objectives and the Systems Engineering Initiative for Patient Safety 2.0 (SEIPS 2.0) model. The original SEIPS model (Carayon et al., 2006) was developed as a framework to represent the complex work system of the healthcare environment. SEIPS leveraged Donabedian’s structure-process-outcome model (Donabedian, 1988) familiar to those in the healthcare field as well as being grounded in systems theory such as Carayon and Smith’s balance theory (Smith and Sainfort, 1989). Key tenets of SEIPS (and the 2.0 model) are the need for balance within the system and that any change within the work system affects the processes and thus the outcomes (although these are not the only key messages from the model (Carayon et al., 2006). See Carayon et al., 2006 for a full description of the original model). SEIPS 2.0 expands upon the original SEIPS model in several ways (Holden et al., 2013b). Those that are pertinent to the present study are: the inclusion of patients and families as actors within the work system, the emphasis on the patient work processes of healthcare, the concept of configuration as a process and performance shaping characteristic of the work system, discussion of internal environment and organizational aspects outside of the hospital (e.g., the patient home). Similar to the original SEIPS model, SEIPS 2.0 describes a structured work system that performs processes that lead to outcomes. Outcomes feed back to the work system, and the work system adapts as a result. The work system is comprised of 6 dynamically interacting elements: (1) people (or teams of people)− e.g., SHHCP, patients, caregivers, physicians (2) the tasks people perform; (3) the tools and technology available and needed to complete the tasks; (4) organizational factors shaping the work, such as staffing, policies, teamwork, coordination, communication; (5) factors related to the physical environment in which work is performed; and (6) features of the external environment such as insurance and healthcare policy (Holden et al., 2013b). These elements dynamically interact to comprise processes (e.g., MM) that produce outcomes (e.g., medication adherence, improved health) (Carayon et al., 2006, 2014; Holden et al., 2013b). Interview questions focused on barriers and facilitators to successful MM and the components of the MM process. Questions were developed iteratively through pilot testing and review by research team members.
2.2. Sites and participants
Data collection occurred at 5 sites affiliated with 3 different SHHC agencies (Table 1). The sites were in both rural and urban areas across the United States.
Table 1.
Data collection site characteristics.
| SHHC agency site | Type | Location where data collected | Average daily census | Average monthly admissions | Total number SHHCP participated | Total number patients participated |
|---|---|---|---|---|---|---|
| 1 | Non profit | Urban/Suburban | 750 | 550 | 20 | 22 |
| 2 | For profit | Rural | 98 | 28 | 9 | 5 |
| 3 | For profit | Urban/Suburban | 170 | 51 | 11 | 9 |
| 4 | Non profit | Urban | 1977 | 1280 | 19 | 13 |
| 5 | Non profit | Urban | 3229 | 2152 | 20 | 11 |
SHHC = Skilled Home Health Care; SHHCP = Skilled Home Health Care Provider.
We used a combination of purposive and network sampling (Crabtree and Miller,1999) to identify older adults ≥ 65 years of age referred for SHHC services after hospital discharge for any diagnosis. We obtained consent from both the SHHCP assigned to visit the patient in the home and the patient (or the patient’s legally authorized representative, if applicable). This study was approved by the Johns Hopkins School of Medicine Institutional Review Board and the review boards at participating sites.
2.3. Approach
Using observation notes and interview transcripts, we developed site-specific and composite process maps representing the high-level process of MM across the transition. Process maps were evaluated by research team members (NW, AG, AIA), and through a member-checking process until consensus was reached.
Directed content analysis for barrier identification was guided by both the process map and SEIPS 2.0. We used an iterative approach to create our coding framework and generate themes and subthemes (Lopez et al., 2012; Vashi and Rhodes, 2011). Two researchers (NW, SM) reviewed all transcripts and identified items related to components of MM. Three researchers (NW, SM, AIA) discussed categorization of MM items. We grouped codes by the highest level of the work system (e.g., person, task, etc.). We created codes inductively within each level based on work system-level barriers. We then categorized codes based upon specific attributes of the process and identified emergent themes. Differences were discussed and reconciled by consensus among all members of the research team. ATLAS.ti qualitative data management software was used to facilitate analysis (ATLAS, 2010).
We assessed barrier propagation through the stages of the MM process during the transition using a case analysis approach. For each transition we observed, we compiled data from the following sources: observation notes from two researchers (AIA, NW); interviews with SHHCPs; and interviews with patients and informal caregivers. We identified barriers to the MM process and propagation through the stages of the process. Characteristics of propagation patterns were concatenated into overarching propagation themes.
3. Results
3.1. Participant characteristics
The 60 older adult patients (65% female) had an average age of 75 years (range = 48e94 years; Table 2). The 33 caregivers (66% female) had an average age of 61 years (range = 22e87 years; Table 2).
Table 2.
Patient demographic characteristics.
| Characteristic | Site 1 N = 22 | Site 2 N = 5 | Site 3 N = 9 | Site 4 N = 13 | Site 5 N = 11 | All Sites N = 60 |
|---|---|---|---|---|---|---|
| Patient Age (mean years) | 75 | 78 | 79 | 67 | 72 | 75 |
| Female (%) | 60 | 60 | 71 | 76% | 81 | 65 |
| Race/Ethnicity (%) | % | % | % | % | % | % |
| African American | 9 | - | - | 46 | 18 | 13 |
| Asian | - | - | - | - | 9 | 2 |
| Caucasian | 90 | 80 | 86 | 15 | 27 | 27 |
| Hispanic | - | 20 | - | 23 | 36 | 12 |
| Other | - | - | 14 | 15 | 9 | 10 |
The SHHCPs (N = 79) had an average of 19 years of experience (90% female) (Table 3). Detailed demographic information is provided in Tables 2 and 3.
Table 3.
Skilled home health care provider demographic characteristics.
| Characteristic | Site 1 N = 20 | Site 2 N = 9 | Site 3 N = 11 | Site 4 N = 19 | Site 5 N = 20 | All Sites N = 79 |
|---|---|---|---|---|---|---|
| Female (%) | 100 | 88 | 64 | 100 | 85 | 89 |
| Provider Age (mean years) | N/A | 39 | 44 | 50 | 45 | 44 |
| Race/Ethnicity (%) | ||||||
| African American | N/A | 11 | - | 57 | 35 | 20 |
| Asian | N/A | - | - | 7 | 15 | 5 |
| Caucasian | N/A | 88 | 90 | 50 | 30 | 41 |
| Hispanic | N/A | - | - | 14 | 15 | 6 |
| Other | N/A | - | 9 | - | 5 | 2 |
| Mean years in homecare industry | 14 | 11 | 9 | 16 | 15 | 13 |
| Mean years since professional degree | 24 | 14 | 15 | 23 | 20 | 19 |
| Role (%) | % | % | % | % | % | % |
| RN | 25 | 66 | 27 | 85 | 70 | 58 |
| PT | 20 | 11 | 36 | 5 | 5 | 13 |
| OT | - | - | 9 | - | - | 1 |
| SLP | - | - | 9 | - | - | 1 |
| SW | - | - | - | - | 1 | |
| HCC | 55 | - | 9 | 5 | - | 15 |
| Administrator | - | 22 | 18 | 5 | 20 | 9 |
RN = Registered Nurse; PT = Physical Therapist; OT = Occupational Therapist; SLP = Speech-Language Pathologist; SW = Social Worker; HCC = Home Care Coordinator.
Results are presented as: 1) description of the fundamental attributes of the MM process during the transition; 2) emergent properties identified and the categorization of associated barriers to the successful execution of the process, and 3) characteristics related to the propagation of barriers through the process. The key components of the process, emergent properties, and related barriers did not differ markedly across sites.
3.2. Fundamental attributes of the medication management process
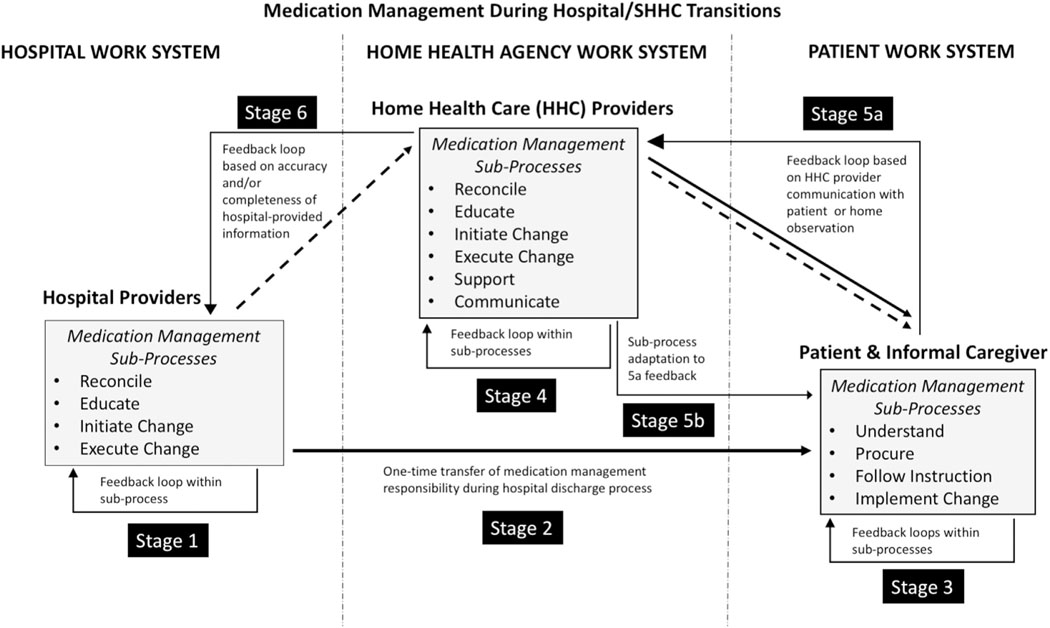
Fig. 1 provides a simplified representation of the high-level stages to completing the process of MM during the transition, rather than a step-by-step process map or task analysis of each subprocess.
Fig. 1.
Simplified representation of the high-level stages of completing the process of medication management during the hospital-to-skilled home healthcare transition.
Each box in Fig. 1 represents the sub-processes that an individual or team must complete for the MM process to be successful during the transition. Tasks within those boxes are not linear per se, but occur within feedback loops that influence the trajectory of the process. Feedback loops represent the iterative nature of the process.
The numbering of the stages in Fig. 1 is not to imply that each sub-process necessarily leads directly to the next stage of the process. In fact, our results revealed that this was not the case. For example, if a patient was unable to procure a medication because they did not have anyone to pick it up and they could not leave the house, the next stage of the process was delayed.
Arrows depict direct communication/transfers of information regarding MM, indirect transfers/communication, or actions. Dashed arrows indicate areas of communication challenge. For example, the arrow depicting MM information transfer between the hospital providers and SHHCPs is dotted and unidirectional because our results suggested there was no direct line of communication; the information received regarding MM was often incomplete or inaccurate. Similarly, the dotted and unidirectional arrow between SHHCPs and patients/informal caregivers indicates that there were communication and information challenges, and SHHCPs typically provided information and initiated communication.
The arrow between the hospital providers and the patient/ informal caregiver is unidirectional and bolded to differentiate it from other communications, as this was a one-time transmission of information occurring during hospital discharge. Angled arrows represent feedback loops where MM tended to get “stuck” and adaptations needed to occur to move to the next stage. But can also represent areas of the process where adaptation can occur.
Dashed vertical lines indicate that system boundaries were not always clear. For example, hospital-based SHHCPs performed MM tasks and sub-processes to facilitate the work of patients and SHHCPs at future stages in the MM process. Hospital-based SHHCPs were typically part of the SHHC agency work system, but they were working within the organizational boundaries of the hospital. Dashed vertical lines denote separate work systems based on organizational boundaries −hospital work system, SHHC agency work system, and the home work system. The process of MM during the transition was an exceedingly complex multi-level process, which involved a series of multiple interdependent sub-processes performed by various roles across systems.
We found the MM process crossed multiple system boundaries. Certain specific sub-processes and tasks occurred within system boundaries, but the MM process as a whole occurred across multiple system boundaries. System boundaries included organizational boundaries (the hospital, SHHC agency, and home/community), temporal boundaries (multiple conceptualizations regarding the length of the MM process), and work boundaries (professional and non-professional work).
The process of MM during the transition also spanned work boundaries, including both professional (i.e., healthcare provider) and nonprofessional (i.e., patient and informal caregiver) work. Successful MM during the transition required hospital and SHHC providers to: (1) successfully reconcile medications prescribed across providers and healthcare settings; (2) educate patients and their informal caregivers about medication regimens; and (3) initiate or execute changes to the medication regimen based on evolution of the patient’s clinical condition or goals of care. These MM sub-processes included the ability of patients and informal caregivers to: (1) successfully understand medication regimens, (2) procure medications, (3) take medications in accordance with the prescribed regimen, and (4) implement changes to the medication regimen as needed.
3.3. Emergent properties of the MM process
Our results revealed three key emergent properties of the MM processes: (1) role and task ambiguity/confusion related to MM were ubiquitous at all process stages for all actors, (2) the process involved individuals performing work across systems in loosely-coupled teams, and (3) cross-boundary spanners played a key role in the execution of the MM processes. Cross-boundary spanners are defined as SHHCP that performed activities related to bridging the communication and information gap that occurred during the hospital-to-SHHC transition. We now describe these emergent properties in detail, including a discussion of the barriers related to each. Illustrative quotations from participants are presented in Table 4 and quotations relevant to specific text are referred to using “QX.” A full list of the barrier categories identified and their descriptions is presented in Table 4.
Table 4.
Fundamental attributes of the process of medication management during hospital/skilled home health care transitions and associated barriers.
| Emergent property of the MM process | Element from SEIPS 2.0 conceptual framework | Barriers identified in MM process during the transition | Description of barrier related to the emergent property | Illustrative quotation |
|---|---|---|---|---|
| Role ambiguity/confusion related to MM were ubiquitous at all process stages and for all actors | Person - Patient and informal caregiver | Level of trust in hospital-based healthcare provider care plan | Patient and/or caregiver may have a low level of trust in hospital providers, leading them to go back to home medication regimens instead of what was prescribed in the hospital | Q1: “Some patients don’t trust their physicians so they kind of just are doing their own thing, they don’t think their doctor really knows what they’re talking about or have their best interest at heart. It’s difficult.” — Setting 4 |
| Ambiguity of role related toMM during the transition | Patient and/or caregiver does not understand what their role should be in MM during the transition | Q2: “There were so many meds that had been changed … and the patient and family were like nobody told us that and here they’re handed a piece of paper that unless someone goes over it with them some of these people aren’t taking the time or aren’t educated enough to read it and understand it. — Setting 1 | ||
| Rapid transfer of roles | Patient and/or caregiver is required to take on full responsibility for MM immediately at the point of discharge | Q3: “[The hospital doctor] prescribed [a] new medication and took me off of some of the old ones because the two don’t work together, so when my [SHHC] nurse comes in I want to actually check ‘em, and she will tell me what to take and what not to take.” — Setting 1 | ||
| Caregiver impact on MM | Caregiver may positively or negatively affect the patient’s ability to perform MM | Q4: “At least [this patient] has someone to give him the medicine, to remind him to follow up with what the [medication regimen] is. There are people who don’t have that support. So then the only support they have is [to go] back to the hospital. — Setting 5 | ||
| The MM process involved individuals performing work across system boundaries in loosely coupled teams | Person - Patient and informal caregiver | Knowledge and skills related to MM | Limited ability to understand and/or implement medication regimen | Q5: “I don’t know how clear it’s made to them when they leave the hospital that they need to stick with what’s on the discharge paperwork.” — Setting 1 |
| Ability to manage medication | Limited ability to cognitively or physically execute the tasks associated with MM | Q6: “At least [this patient] has someone to give him the medicine, to remind him to follow up with what the [medication regimen] is. There are people who don’t have that support. So then the only support they have is [to go] back to the hospital.” — Setting 5 | ||
| Task | Training to perform MM tasks | The level of training to perform MM tasks is not adequate to successfully execute the tasks | Q7: “Personally for me, but I know others struggle with this, the medication part of it [is the transition challenge]. Because we’re just not schooled that much in all the different medications, and reconciling those medications, and that kind of thing … we know cursory information about some of the medications and what they’re for, but when a patient starts asking us something, ‘Now what is this medication for?’ … I don’t want to lead them astray.” — Setting 3 | |
| MM task complexity | Complexity due to the variability, unpredictability, or fluctuating nature of MM tasks | Q8: “You talk [with the hospital] about medications you’re going to take and then when you get the medications back from the drugstore, the names bear no resemblance.” — Setting 5 | ||
| SHHCP Workload | SHHPC workload does not support the current MM process | Q9: “Later on I’m gonna compare that to the paperwork that I have. I’ll probably call [primary care physician] office again and just find out for sure which medications [the patient is on] cause I didn’t have a chance [during the call at the home visit] to put it all together in my head what I wanted to ask him about the medications. — Setting 1 | ||
| Tools | Availability of tools to support teamwork during the transition | Lack of tools to support team-based MM during the transition | Q10: “Yes [the discharge paper] said resume home meds as directed but it doesn’t list them and tell me what she should be taking and what she shouldn’t be taking.” — Setting 1 | |
| Existence of MM artifacts | Tools or technologies developed to support thinking, problem solving, or memory related to MM, e.g., pill planners, reminders, etc. | Q11: “We always want to make sure that our patients have a medication list handy, something they can really read and understand. So actually in our admission packet, we have a patient-friendly medication list. So even though they have one that comes with the discharge papers, and it’s typed up … it may be difficult for them to interpret.” — Setting 5 | ||
| Usefulness of discharge papers to facilitate MM | Discharge tools do not provide enough information on medications, it is difficult to find in the discharge papers, or it conflicts with other medication information | Q12: “We have nothing in the plan of care … there’s 14 medications written on the discharge paper. The patient had 6 prescriptions, [and] the patients don’t always give you accurate information.” — Setting 4 | ||
| Organization | SHHCP working sphere | Barriers related to the nature of the SHHCP’s mobile work environment that lead to isolation and inability to easily communicate when needed | Q13: “If we can’t get orders and we don’t, you know, we can’t just do things, you know. We have to have, we base our care off of doctors orders, so if we don’t have orders to do something we know the patient needs, then you know, our next step if it’s critical, we have to send them to the emergency room.” — Setting 4 | |
| Physical environment | Physical environment to support MM | Safety hazards in the home, including obstacles, sanitation issues, clutter, that impede successful MM | Q14: (from observation notes) “Medication reconciliation is taking a considerable amount of time because of all the medications and the difficulty locating medications in the home.” — Setting 3 | |
| External Environment | Sociocultural factors (e.g., socioeconomic status, culture, community) | Sociocultural factors that may negatively influence perceptions about MM and negatively affect ability to access medications, etc. | Q15: “We do see people who are just there by their self with no support. They’ll come home [from the hospital] but they haven’t had the opportunity to pick up their medicine ‘until my daughter comes to see me tomorrow at 4:00.’ But you’re CHF and you just got out of the hospital, and you need your fluid medicine. [Those are] some struggles that we see … especially in some of the lower socioeconomic [areas].” — Setting 2 | |
| Cross-boundary spanners played a key role in the execution of the MM processes | Person — hospital- and home-based SHHCP | SHHCP execution of perceived ideal role in MM | Tension between SHHCPs’ execution of routine vs. ideal roles in MM, e.g., performing tasks that go beyond the job description, or not being able to perform all ideal tasks due to some kind of restriction based on time, workload, etc. | Q16: “You know, and then they don’t have their medications and they just had open heart surgery. So you know, what do you want me to do, you know … [these types of situations are] really burning us out.” — Setting 4 |
| SHHCP ability to fulfill role in MM | Limited ability of SHHCP to fulfill role, because expectations of what is needed to fulfill role requirements are not met | Q17: “I [follow up with the pharmacy] because I want to make sure that the patient has everything she needs when she’s [home].” — Setting 1 | ||
| Tools | Usefulness of tools available to support MM | Lack of useful tools or technologies to support MM | Q18: “I always tell my patients to write down both names. So that when they go to the doctor they bring that form with them.” — Setting 1 | |
| Organization | Physician accessibility | SHHCP difficulties communicating with physicians involved in medication management decisions (e.g., PCP, hospitalist) | Q19: “One of the biggest issues and problems [SHHCPs] run into is the ability to reconcile medications [due to inability] to reach a physician via the phone when you need to.” — Setting 5 | |
| Communication breakdown during the transition | Ineffective communication and/or a disruption of the expected communication process | Q20: “Another issue is that [the patient] needs someone to bring her medications over to the pharmacy and with the aide not being here, she will need to find another way. She’s actually missed her medications for the entire day because of a miscommunication and misunderstandings related to not having someone clearly write on the discharge summary her complicated medication regimen.” — Setting 4 | ||
| Information underload | SHHCP does not have the information they need to perform MM | Q21: “If I don’t have the correct information … simple things like … the address is completely wrong, the phone number is wrong, the phone number is not in service … then I can spend the day spinning wheels calling here and there, calling emergency numbers and trying to find the patient.” — Setting 1 | ||
| Physical Environment | SHHCP feels safe in the home environment to take the time to perform MM activities | Challenges related to personal safety may lead to less time spent on MM-related tasks | Q22: (from observation notes) “When the SHHCP asks the patient for his medications, he becomes agitated and says “what is all this?” “Why do you need to do all of this?” The mother is also upset and comes into the living room. The patient says “yes mom is here to back me up.” — Setting 3 |
MM: Medication management; PCP: Primary Care Physician; SHHCP: Skilled home health care provider; SEIPS: System Engineering Initiative for Patient Safety.
3.3.1. Role ambiguity/confusion related to MM were ubiquitous at all process stages for all actors
We found that role ambiguity existed at different process stages, e.g., physicians not comfortable accepting responsibility for specific stages of the process without additional information. Role ambiguity also extended to patients not understanding their level of responsibility in MM. For example, patients often waited for the SHHC visit to clarify MM issues, either because they were confused, or because they did not trust hospital provider recommendations. This was a potentially dangerous practice, as SHHC visits did not take place until about 48e72 h post hospital discharge.
3.3.1.1. Barriers related to role ambiguity/confusion.
We identified barriers to the success of the process due to the rapid transfer of roles across work system boundaries when patients were discharged from the hospital. During the hospital stay, healthcare providers maintained full responsibility of MM. At the point of discharge, responsibility was transferred to patients and their informal caregivers. We found that because SHHC services did not start immediately, this sometimes caused insurmountable challenges for patients’ MM during the transition (Q2). SHHCPs expressed the importance of informal caregiver (e.g., family member) roles in MM during transitions (Q4). However, caregivers sometimes questioned prescribed regimens.
Patients often waited for the SHHC visit to clarify MM issues. Discharge (Q3). Some patients returned home and resumed medication regimens prescribed by their primary care physicians (PCP) for several reasons: regimens were more familiar to patients; regimens were already part of their home routine; and regimens were from the PCP, whom patients trusted more than hospital-based physicians (Q1).
3.3.2. The MM process involved individuals performing work across system boundaries in loosely-coupled teams
We found the MM process involved individuals performing work across systems in loosely-coupled teams. Loose coupling can be conceptualized as work that is performed by individuals with a shared goal, but who are not necessarily dependent on other team members to achieve the shared goal. Loosely-coupled team members perform most tasks autonomously and often at disparate times and locations (Olson and Olson, 2000; Weick, 1976).
Loosely-coupled teams occurred as a result of the MM process unfolding across misaligned work systems. For example, multiple individuals were involved in the process of MM during the transition, yet no one person was responsible for all MM, and no one person had knowledge of the entire MM process. Although the process was dependent upon the interaction of multiple loosely-coupled teams, individuals did not necessarily understand that they were part of a team.
3.3.2.1. Barriers related to individuals performing work across system boundaries in loosely-coupled teams.
MM was highly complex and included managing medications with more than one name for each medication (Q8). Complex regimens also included high numbers of medications, often from various prescribers. High complexity of medication regimens led SHHCPs to perform additional or redundant steps for MM, such as placing numerous phone calls to the hospital to clarify prescriptions. The tools available to support MM during the transition reflected the absence of understanding that MM was a team-based process. For example, discharge papers and SHHC documents were tailored to the needs of the organization providing the paperwork, rather than to the needs of all team members across organizational boundaries (Q10), limiting distributed situation awareness.
SHHCPs did not always have the training to handle MM during the transition. For example, physical therapists were deployed by SHHC agencies to perform initial evaluations for a subset of less medically complex patients. Physical therapists were not specifically trained to manage complex medication regimens, but they were sometimes required to do so (Q7) if the patient was more complex than anticipated. Compounding this barrier was that SHHCPs often did not have the time available during the initial home visit to complete MM-related tasks due to other issues the patient was having during the visit (Q9). In addition, SHHCPs were isolated in the field, without easy access to supervisors, team members, or prescribing physicians (Q13).
Many patients did not have the appropriate knowledge and skills to successfully execute MM. SHHCPs believed patients were not receiving the training they needed at hospital discharge to manage MM during the transition (Q5). As a result, many patients relied exclusively on informal caregivers to manage their medications (Q6).
Patients developed their own tools for MM, such as medication lists, to help during the transition (Q13). SHHCPs often found discrepancies between these documents and the medications the patient had in the home (Q11). Discharge instructions were not always useful tools for determining the correct medication regimen. Both SHHCPs and patients described many instances of conflicting information between discharge paperwork and what patients reported being told at discharge (Q12).
Physical environment barriers included cluttered medication storage areas and difficulty finding pills. SHHCPs described medication storage areas that held medications for the entire household. One older stored her medications with her dog’s medications alongside the medications prescribed for her late husband (who had died several years prior). In another household, the informal caregiver could not locate all of the medications for the SHHCP to complete the medication reconciliation because medications were stored in several cluttered areas (Q14). Changes to the physical environment were also a factor in successful MM. Some patients were staying with informal caregivers rather than in their own homes; this change in environment caused disruption to MM routines, such as medications not being stored in the usual areas, and missing the usual environmental cues to taking medications.
Sociocultural factors also played a role in the ability to manage MM during the transition, particularly when patients were unable to obtain help (Q15). Multiple factors contributed to lack of home support, including adult children not able to provide full-time help, inability to afford in-home care, or living in rural areas that were difficult to access.
3.3.3. Cross-boundary spanners played a key role in the execution of the MM processes
The cross-boundary spanner role served as communication and coordination hub for the work that occurred across system boundaries. SHHCPs served as a point of communication and facilitator of information flow, providing feedback to hospitals, clarifying regimens, educating patients and their informal caregivers, and executing medication changes.
Fig. 1 represents SHHCPs as a mediator of the shift in MM responsibility from the hospital providers to the patient and informal caregiver. SHHCPs have the additional responsibilities of communication and support, which was a challenging role. Several communication challenges were noted during the process of MM during the transition. Patients and informal caregivers described communication challenges during hospital discharge, with medications being ordered as they left the hospital or afterwards. SHHCPs described challenges communicating with patients to schedule the first SHHC visit, and SHHCPs often had to show up at homes without appointments. SHHCPs also had challenges communicating with hospital providers during the transition period. Representative across sites, one SHHCP reported needing to contact prescribing providers for MM clarification “40−50% of the time” − (Site 1).
3.3.3.1. Barriers related to cross-boundary spanners played a key role in the execution of the MM processes.
As cross-boundary spanners, hospital-based SHHCPs and those delivering care at home routinely performed tasks that were above and beyond their job description (Q16). SHHCPs reported going to pharmacies to pick up prescriptions, waiting for extended periods at patients’ homes for confirmation that a prescription was ready before leaving, and giving patients money for prescriptions they otherwise could not afford.
Barriers in communication and information management across system boundaries impeded MM (Q17). SHHCPs were consistently working without the information they needed for MM (Q21). Information underload resulted from several factors: missing documentation from the hospital, patients who did not retain discharge instructions, and delayed transfer of documentation from the hospital to the SHHC agency. Further, communication-related barriers were ubiquitous (Q20). SHHCPs reported communication and coordination challenges, such as difficulty accessing and communicating with hospital- or primary care-based physicians (Q19).
Patients became confused when lists from the hospital or pharmacy contained either only the generic or brand names for medications. SHHCPs supported patients in creating medication tools to support MM and updating their tools with current information (Q18). However, some patients were not receptive to SHHCP support. SHHCPs also described instances of not being able to perform MM optimally due to not feeling safe in the home (Q22).
3.4. Barriers propagated across stages of the medication management process
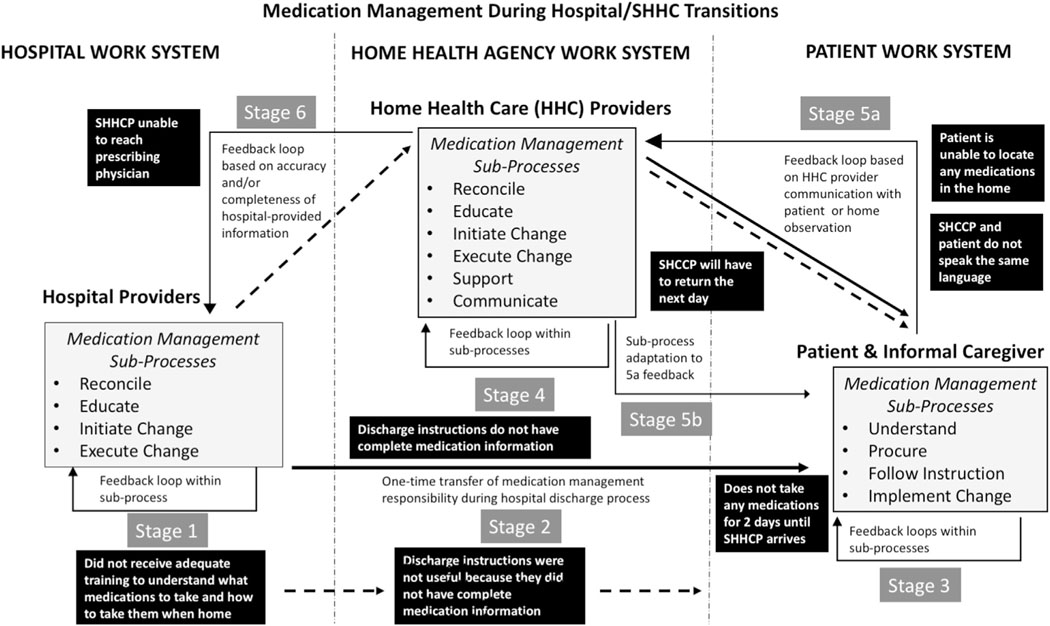
We found four insights related to barrier propagation (Fig. 2). Within Fig. 2 we depict barriers as black boxes, and we provide example barriers as they occurred in one particular MM process:
Fig. 2.
Depiction of barrier propagation through the stages of the medication management process.
Carolina (name has been changed) is a woman over the age of 65 living alone in a subsidized housing apartment in an urban northeastern city in the United States. Her primary diagnosis is chronic obstructive pulmonary disease (COPD) and the SHHC visit occurred following her 3rd hospital admission in a 30-day period. Carolina is from the Dominican Republic, and speaks only Spanish.
3.4.1. Barriers propagated across process stages
First, we found that when a barrier was identified at stage one in the MM process, the barrier would propagate to later stages in the process. Carolina’s case illustrates the propagation of barriers following the occurrence of two barriers at stage 1 of the MM process: 1) lack of usefulness of tools available to support MM, and 2) lack of training to perform MM tasks. The “usefulness of tools” barrier (Table 4) was encountered during stage 1 (Fig. 2)da discharge summary did not provide needed MM information. This barrier was encountered again in stages 3, 4, and so on. As Fig. 2 illustrates, the discharge summary not providing needed information led to the inability for Carolina to take any medications (stage 3). Thus, the patient was not able to complete stage 3. Once the SHHCP arrived, the lack of information on the discharge summary also inhibited the SHHCP from performing stage 4, as she was unable to discern which medications the patient should have been taking. Considerable time was spent in stage 5 as the SHHCP played detective, attempting to find medications in the home, asking the patient questions about what she was told during discharge, and calling the pharmacy. At this point, the SHCCP was frustrated because “all [the documentation] I had walking into this appointment was 4 lines that don’t tell me anything.” (Setting 4) The SHHCP was also unable to reach the prescribing physician due to lack of contact information in the discharge instructions.
3.4.2. Barriers often proliferated at later process stages
Second, we found that the propagation of barriers from stage 1 or stage 2 often resulted in an increase in and transformation of barriers at later process stages as a consequence of the initial barrier. Downstream in the process, the original barrier has transformed. For example, consider again the “usefulness of tools” barrier that occurred in stage 1 of Fig. 2; this barrier became two barriers in stages 5 and 6: communication breakdown and physician accessibility.
3.4.3. Barrier propagation led to process consequences
Third, we found that the propagation of barriers across process stages led to consequences in the execution of MM, and MM would get stuck at a sub-process stage. Consider again the “usefulness of tools” barrier: this early-stage barrier often propagated through the stages of the process until a sub-process continuous feedback loop led to a delay. In Fig. 2, the barrier affecting stage 3 led to an inability for the patient to complete that stage. Once the SHHCP arrived, the process was stuck again at stage 4, as the SHHCP attempted to reconcile the medications. Finally, the SHHCP was unable to execute stage 6 because the prescribing physician could not be reached. The process was unable to move forward due to the stage 1 barrier of lack of information about the medication regimen on the discharge paperwork.
3.4.4. Barrier propagation led to system consequences
Fourth, analyses revealed that barrier propagation was associated with negative work system consequences. As depicted in Fig. 2, barrier propagation led to process delays that were associated with negative consequences for the patient, including missed medication doses and potentially dangerous drug interactions. In addition, there were negative consequences for the SHHCP (e.g., frustration and increased workload), and for the SHHC agency (e.g., staffing issues due to work not being completed).
4. Discussion
Our results provide novel insights into optimizing work system design that would be indiscernible with a task-level approach. A process-level of analysis identified: (1) the key attributes of the process of MM during the hospital-to-SHHC transition, (2) the emergent properties of MM as it occurs across system boundaries and the related barriers, and (3) the patterns of barrier propagation through the MM process. This is the first study to analyze and describe MM at the process level across hospital-to-SHHC transitions, and these descriptions and their resultant insights can be used to guide future work to improve the MM process and to study other distributed healthcare tasks at the process level.
4.1. Insights from, and advantages of, a process-level analysis: implications for the field of human factors and ergonomics
4.1.1. The process-level of analysis provided a framework for bounding sociotechnical system analysis
Our findings suggest the importance of taking a process-level approach to a critical challenge in the field of systems ergonomics e how to define the boundaries of systems we wish to study and improve (Carayon, 2006; Karsh et al., 2014; Rivera-Rodriguez et al., 2013; Flach et al., 2015). Edwards and Jensen (2014) have urged systems ergonomists not to limit the scope of those boundaries, lest there be repercussions in the ability to redesign the system (Edwards and Jensen, 2014). To optimize a process across systems, smaller individual work systems must be designed to align with each other around specific processes. Conceptually, these smaller systems combine during certain processes to make up a larger “mega system.” For example, the hospital and patient work system do not have to be designed such that they are aligned for every process. A critical step is to determine what processes the system needs to be aligned for and how the alignment across those processes should be prioritized.
We acknowledge a potential disadvantage of the process-level view is that it could lead to an overwhelming complexity of numerous interactions, actors, and tasks (Carayon, 2006). However, the process itself serves to restrict the number of variables to those pertinent to the interactions that occur because of the process. For example, focusing on a particular process (i.e., MM) allowed for identification of barriers specific to the process. This may be best explained in terms of configuration (Holden et al., 2013b). In light of their SEIPS 2.0 model, Holden et al (2013a,b) describe configuration as the phenomenon in which,
“… only a subset of all possible interactions is actually relevant in a given work process or situation … Thus, for a particular process or situation, one can distinguish a configuration of a finite number of relevant elements that interact to strongly shape the performance of that process. (p. 6)” (Holden et al., 2013b).
Crossing system boundaries increases the number of potential interacting variables, and thus the complexity of the system analysis (Carayon, 2006). However, if the interactions studied were limited to those specific to the process, this would create a more parsimonious configuration of interactions specifically related to the process, focusing the analysis.
4.1.2. The process-level of analysis allows for identification of properties that would not be uncovered at the task level
Studying MM at the process level allowed us to identify the fundamental attributes of the process. In turn, we identified emergent properties of the MM process we would not have seen at the task level of analysis (Walker and Carayon, 2009; Dekker et al., 2013; Carayon et al., 2013). By definition, “an emergent property … cannot be deduced solely by examining the components of the system in isolation.” (p. 360 (Dekker et al., 2013);) Emergent properties can be either positive or negative in terms of their effect on the work performed; in either case, emergent properties provide critical information about processes and systems (Wilson, 2014; Johnson, 2006). MM does not occur in one organization, and tasks related to MM are not performed by one person.
By viewing MM as a set of distributed tasks (i.e., process-level), rather than only studying parts of the process individually at the task level (i.e., in the pharmacy, then separately in the home), critical properties emerged that can inform redesign. In other words, if our HFE analysis had been bound at the task level (i.e., by individual system constraints) certain emergent properties may not have been revealed, such as the emergence of a boundary-spanning role (Walker and Carayon, 2009).
4.1.3. The process-level of analysis allows for an examination of barrier propagation occurring across system boundaries
Finally, using a process-level view allowed for the identification of the propagation of barriers throughout the MM process (Carayon et al., 2015). Propagation analysis was critical to identifying the antecedents of barriers that occurred across system boundaries. Once a barrier propagated through a process, we found that it could change or propagate to the creation of new barriers. When propagation of a barrier happens in a process, the ability for those downstream in the process to identify the antecedents is substantially decreased (Waterson, 2009).
Propagation analysis also allowed us to consider the antecedents of barriers downstream in the process of MM that led to process variance. Researchers at the Tavistock Institute included identification and analysis of key variances in procedures for sociotechnical system design, and these have been used for decades (Herbst, 1974). Cherns (1976) highlights the identification of variances, “an unprogrammable event … which critically affects outcome” (p. 787), as a key principle of sociotechnical system design (i.e., variances being a result of a barrier within the system) (Cherns, 1976). We have applied these concepts to study the work that occurs across the traditionally-defined system boundaries and focused on the barriers that lead to variances (Hollnagel, 1999).
Future work should investigate barrier propagation across processes by linking specific process variances and errors and modeling the propagation using methods such as neural network or Markov chain models. Carayon et al (2015) applied a Markov chain modeling approach to identify the propagation of medication administration errors within an intensive care unit in a hospital (Carayon et al., 2015). These methods allow for the identification of specific patterns of process variances, barriers, errors, and how feedback at different stages of the process might affect propagation and system adaptation across system boundaries.
4.2. Limitations
This study focused on one type of process (i.e., MM) in one domain (i.e., hospital-to-SHHC transitions). However, the attributes identified may be transferable to other healthcare processes distributed across organizations, people, and time. Because the focus of this study was on the process itself, we did not examine clinical or utilization outcomes, such as adverse events or rehospitalizations related to the process. This would be an area for future study. We also did not interview or observe other stakeholders, such as hospital-based physicians, pharmacists, or PCPs. We chose as a first step to focus on the perspectives of those most immediately involved in the MM process (Schoenborn et al., 2013). Finally, for the purposes of the present analysis, we focused on identifying evidence of common themes across all sites rather than those specific to each site. We found that the key components of the process and key barriers related to MM did not differ markedly across sites. However, an analysis focused specifically on cultural differences at specific sites may be able to uncover differences our analysis did not elucidate.
4.3. Process-level analysis: implications for medication management
4.3.1. Importance of building process feedback across system boundaries
Study findings point to the need for developing feedback mechanisms across system boundaries. Adaptability is a critical characteristic of a sociotechnical system (Carayon et al., 2014; Clegg, 2000). By viewing MM at the process level, we found a lack of infrastructure to provide feedback across organizational boundaries, limiting adaptability. As a result, team members did not have the benefit of seeing the effects or implications of their individual actions on subsequent sub-processes.
To integrate feedback, the systems must be aligned for the process. Given the lack of alignment of the systems involved in the MM process, the only way for team members to become aware of propagated barriers was if a team member downstream notified them. We found team members did not receive feedback in a timely fashion, or at all, which impeded them from making adaptations to their actions that would benefit the process across system boundaries (Holden et al., 2013b). This is particularly concerning as communication issues have been found to a persistent contributing factor to medication-related errors (Armitage and Knapman, 2003; Patterson et al., 2004).
4.3.2. System redesign across system boundaries from a process-level view
Our results suggest the need for system design at the process level specific to the complexities of MM during the hospital-to-SHHC transition. System design must focus on improved teamwork across system boundaries among hospital providers, hospital and home-based SHHCPs, and patients and their informal caregivers, emphasizing communication across organizational boundaries. Loose coupling has implications for the way teams cooperate, as the inherent attributes of loosely-coupled teams have been shown to limit team communication and collaboration (Carter et al., 2004). Hence, loosely coupled teams require formalized strategies and support to facilitate team performance (Olson and Olson, 2000; Pinelle and Gutwin, 2003, 2006; Olson and Teasley, 1996; Neyem et al., 2007; Holmstrom and Boudreau, 2006). To improve the connectedness of teams across system boundaries, systems must be designed to identify feedback mechanisms at each stage. Across organizational boundaries, and over time.
Our results also point to the critical need to design systems to support team members’ situation awareness across system boundaries (Endsley, 1995). As Stanton (2016a,b) emphasized, “Situation awareness holds loosely coupled systems together. It is argued that without this coupling the systems [sic] performance may collapse.” (p.3) (Stanton, 2016a). However, it is not necessary that all team members encompass all knowledge of a patient’s situation. Rather, for MM to be a successful process, a distributed situation awareness is needed, in which systems provide team members only the specific information pertinent to complete their actions in the process (Salmon et al., 2010; Stanton et al., 2006). For example, distributed situation awareness could be improved through the design of technologies that provide each team member with role-specific information (Salmon et al., 2010; Stanton, 2016b).
There are currently a number of interventions available to improve transitions or a specific process related to aspects of MM (Coleman, 2007; Parry et al., 2003, 2006; Bradway et al., 2011; Naylor et al, 2004, 2009; Naylor and Ware, 2007). However, interventions to support MM typically focus on only one part of the MM process in only one work system, such as medication reconciliation in the hospital, or medication adherence in the home. Study findings suggest a need to understand the process as a whole, rather than focusing on only one sub-process/work system for improvement.
4.4. Conclusions
Older adults transition across health care settings with increasing frequency compared to the general population. Complex health care processes such as MM have previously been studied from a task-level view, and as occurring in a single work system. Study findings demonstrate the need for, and advantages of, understanding complex processes from the process level. Care transitions represent a critical point for error recovery (Clancy, 2006), and transitions by definition occur across system boundaries e temporal boundaries (e.g., transitions of care, coordination of care), physical boundaries (e.g., multiple healthcare settings), and cultural boundaries (e.g., professional and non-professional work of managing health) (Arbaje et al., 2014; Coleman and Berenson, 2004).
The process of MM during the hospital/SHHC transition provided an important case study for conducting an in-depth exploration of healthcare processes across system boundaries. A process-level approach allowed for a holistic examination of MM, an understanding of how barriers occur, and how barriers are propagated across systems. Study findings point to the need for, and importance of, using a process-level approach to investigating complex healthcare work across system boundaries.
Acknowledgements
Contributors: We would like to thank Elaine Nguyen and Ashley Hughes for assistance in data coding. We would also like to extend our gratitude to the home health care agencies for their ongoing support of this research, and all of the providers, patients and their caregivers who participated as part of this work.
Funders: This work was supported by funding from the Johns Hopkins University School of Nursing Center for Innovative Care in Aging, the Johns Hopkins Clinical Research Scholar grant (#KL2TR001077), the National Patient Safety Foundation, and the Agency for Healthcare Research and Quality (grant # 1K08HS022916).
The funders had no role in any of the following activities: design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Prior presentations: Abstracts of this work were presented as posters at the Gerontological Society of America annual conference, November 6, 2014, Washington, DC, and the Human Factors and Ergonomics Society Annual Health Care Symposium, April 27, 2015, Baltimore, MD.
Footnotes
Conflicts of interest
The authors have no conflicts of interest to report.
References
- Arbaje AI, et al. , 2014. Regardless of age: incorporating principles from geriatric medicine to improve care transitions for patients with complex needs. J. general Intern. Med 29 (6), 932–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armitage G, Knapman H, 2003. Adverse events in drug administration: a literature review. J. Nurs. Manag 11 (2), 130–140. [DOI] [PubMed] [Google Scholar]
- Beyer H, Holtzblatt K, 1997. Contextual Design: Defining Customer-centered Systems. Interactive Technologies. Morgan Kaufmann, San Francisco, p. 496. [Google Scholar]
- Bradway C, et al. , 2011. A qualitative analysis of an advanced practice nurse-directed transitional care model intervention. Gerontologist 52 (3), 394–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruning K, Selder F, 2011. From hospital to home healthcare: the need for medication reconciliation. Home Healthc. Nurse 29 (2), 81–90. [DOI] [PubMed] [Google Scholar]
- Carayon P, 2006. Human factors of complex sociotechnical systems. Appl. Ergon 37 (4), 525–535. [DOI] [PubMed] [Google Scholar]
- Carayon P. (Ed.), 2012. Handbook of Human Factors and Ergonomics in Health Care and Patient Safety, second ed. CRC Press, Boca Raton, Florida. [Google Scholar]
- Carayon P, Wood KE, 2009. Patient safety. Inf. Knowl. Syst. Manag 8 (1e4), 23e46. [Google Scholar]
- Carayon P, et al. , 2006. Work system design for patient safety: the SEIPS model. Qual. Saf. Health Care 15 (Suppl. 1), i50–i58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, et al. , 2013. Macroergonomics in health care quality and patient safety. Rev. Hum. factors Ergon 8 (1), 4–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, et al. , 2014. Human factors systems approach to healthcare quality and patient safety. Appl. Ergon 45 (1), 14–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, et al. , 2015. Medication error propagation in intensive care units. In: Proceedings of the Human Factors and Ergonomics Society Annual Meeting. SAGE Publications. [Google Scholar]
- Caroff DA, et al. , 2015. A medical resident−pharmacist collaboration improves the rate of medication reconciliation verification at discharge. Jt. Comm. J. Qual. Patient Saf 41 (10), 457–461. [DOI] [PubMed] [Google Scholar]
- Carter S, Mankoff J, Goddi P, 2004. Building connections among loosely coupled groups: Hebb’s rule at work. Comput. Support. Coop. Work (CSCW) 13 (3e4), 305–327. [Google Scholar]
- Centers Medicare Medicaid Serv. 2014. 2004; Available from: http://www.cms.hhs.gov/. [PubMed]
- Cherns A, 1976. The principles of sociotechnical design. Hum. Relat 29 (8), 783e792. [Google Scholar]
- Clancy CM, 2006. Care transitions: a threat and an opportunity for patient safety. Am. J. Med. Qual 21 (6), 415–417. [DOI] [PubMed] [Google Scholar]
- Clegg CW, 2000. Sociotechnical principles for system design. Appl. Ergon 31 (5), 463–477. [DOI] [PubMed] [Google Scholar]
- Coleman E, 2007. The Care Transitions Program. The John A. Hartford Foundation. [Google Scholar]
- Coleman EA, Berenson RA, 2004. Lost in transition: challenges and opportunities for improving the quality of transitional care. Ann. Intern. Med 141 (7), 533–536. [DOI] [PubMed] [Google Scholar]
- Coleman EA, et al. , 2005. Posthospital medication discrepancies: prevalence and contributing factors. Archives Intern. Med 165 (16), 1842–1847. [DOI] [PubMed] [Google Scholar]
- Crabtree BF, Miller WL, 1999. Doing Qualitative Research, second ed. Sage Publications, Newbury Park. [Google Scholar]
- Dekker SW, Hancock PA, Wilkin P, 2013. Ergonomics and sustainability: towards an embrace of complexity and emergence. Ergonomics 56 (3), 357–364. [DOI] [PubMed] [Google Scholar]
- Dierich MT, Mueller C, Westra BL, 2011. Medication regimens in older home care patients. J. Gerontol. Nurs 37 (12), 45–55. [DOI] [PubMed] [Google Scholar]
- Donabedian A, 1988. The Quality of Care: how can it be assessed? J. Am. Med. Assoc 260 (12), 1743–1748. [DOI] [PubMed] [Google Scholar]
- Edwards K, Jensen PL, 2014. Design of systems for productivity and well being. Appl. Ergon 45 (1), 26–32. [DOI] [PubMed] [Google Scholar]
- Endsley MR, 1995. Toward a theory of situation awareness in dynamic systems. Hum. Factors J. Hum. Factors Ergon. Soc 37 (1), 32–64. [Google Scholar]
- Faye H, et al. , 2010. Involving intensive care unit nurses in a proactive risk assessment of the medication management process. Jt. Comm. J. Qual. Patient Saf 36 (8), 376–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flach JM, et al. , 2015. Striving for safety: communicating and deciding in socio-technical systems. Ergonomics 58 (4), 615–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ATLAS.ti: the knowledge workbench, GmbH A.t.S.S.D., Editor. 2010: Berlin. [Google Scholar]
- Hendrick HW, Kleiner B, 2002. Macroergonomics: Theory, Methods, and Applications. CRC Press. [Google Scholar]
- Herbst PG, 1974. Socio-technical Design: Strategies in Multidisciplinary Research. Tavistock London. [Google Scholar]
- Holden RJ, et al. , 2013. Automation and adaptation: nurses’ problem-solving behavior following the implementation of bar-coded medication administration technology. Cogn., Technol. work 15 (3), 283–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holden RJ, et al. , 2013. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics 56 (11), 1669–1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollnagel E, 1999. Accidents and barriers. In: Proceedings of Lex Valenciennes. [Google Scholar]
- Holmström J, Boudreau M-C, 2006. Communicating and coordinating: occasions for information technology in loosely coupled organizations. Inf. Resour. Manag. J 19 (4), 23. [Google Scholar]
- Institute for Healthcare Improvement, 2016. Medication Reconciliation to Prevent Adverse Drug Events [cited 2016; Available from: http://www.ihi.org/topics/adesmedicationreconciliation/Pages/default.aspx.
- Johnson CW, 2006. What are emergent properties and how do they affect the engineering of complex systems? Reliab. Eng. Syst. Saf 91 (12), 1475–1481. [Google Scholar]
- Karsh B-T, Brown R, 2010. Macroergonomics and patient safety: the impact of levels on theory, measurement, analysis and intervention in patient safety research. Appl. Ergon 41 (5), 674–681. [DOI] [PubMed] [Google Scholar]
- Karsh B-T, Waterson P, Holden RJ, 2014. Crossing levels in systems ergonomics: a framework to support ‘mesoergonomic’inquiry. Appl. Ergon 45 (1), 45–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleiner BM, 2006. Macroergonomics: analysis and design of work systems. Appl. Ergon 37 (1), 81–89. [DOI] [PubMed] [Google Scholar]
- Lopez A, et al. , 2012. What patients say about their doctors online: a qualitative content analysis. J. Gen. Intern Med 27 (6), 685–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meredith S, et al. , 2001. Possible medication errors in home healthcare patients. J. Am. Geriatr. Soc 49 (6), 719–724. [DOI] [PubMed] [Google Scholar]
- Murtaugh CM, Litke A, 2002. Transitions through postacute and long-term care settings: patterns of use and outcomes for a national cohort of elders. Med. Care 40 (3), 227–236. [DOI] [PubMed] [Google Scholar]
- Naylor MD, Ware MS, 2007. Transitional Care Model: a Journey in Collaboration. [Google Scholar]
- Naylor MD, et al. , 2004. Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. J. Am. Geriatr. Soc 52 (5), 675–684. [DOI] [PubMed] [Google Scholar]
- Naylor MD, et al. , 2009. Translating research into practice: transitional care for older adults. J. Eval. Clin. Pract 15 (6), 1164–1170. [DOI] [PubMed] [Google Scholar]
- Neyem A, Ochoa SF, Pino JA, 2007. Designing mobile shared workspaces for loosely coupled workgroups. In: International Conference on Collaboration and Technology. Springer. [Google Scholar]
- Olson GM, Olson JS, 2000. Distance matters. Hum.Comput Interact 15 (2), 139–178. [Google Scholar]
- Olson JS, Teasley S, 1996. Groupware in the wild: lessons learned from a year of virtual collocation. In: Proceedings of the 1996 ACM Conference on Computer Supported Cooperative Work. ACM. [Google Scholar]
- Parry C, et al. , 2003. The care transitions intervention: a patient-centered approach to ensuring effective transfers between sites of geriatric care. Home Health Care Serv. Q 22 (3), 1–17. [DOI] [PubMed] [Google Scholar]
- Parry C, Kramer HM, Coleman EA, 2006. A qualitative exploration of a patient-centered coaching intervention to improve care transitions in chronically ill older adults. Home Health Care Serv. Q 25 (3e4), 39–53. [DOI] [PubMed] [Google Scholar]
- Patterson ES, et al. , 2004. Examining the complexity behind a medication error: generic patterns in communication. IEEE Trans. Syst. Man, Cybern.-Part A Syst. Hum 34 (6), 749–756. [Google Scholar]
- Pinelle D, Gutwin C, 2003. Designing for loose coupling in mobile groups. In: Proceedings of the 2003 International ACM SIGGROUP Conference on Supporting Group Work. ACM. [Google Scholar]
- Pinelle D, Gutwin C, 2006. Loose coupling and healthcare organizations: deployment strategies for groupware. Comput. Support. Coop. Work (CSCW) 15 (5e6), 537–572. [Google Scholar]
- Rivera-Rodriguez AJ, et al. , 2013. Multi-level ergonomics determining how to bound your system. In: Proceedings of the Human Factors and Ergonomics Society Annual Meeting. SAGE Publications. [Google Scholar]
- Rosati RJ, Huang L, 2007. Development and testing of an analytic model to identify home healthcare patients at risk for a hospitalization within the first 60 days of care. Home Health Care Serv. Q 26 (4), 21–36. [DOI] [PubMed] [Google Scholar]
- Salmon PM, et al. , 2010. Is it really better to share? Distributed situation awareness and its implications for collaborative system design. Theor. Issues Ergon. Sci 11 (1e2), 58–83. [Google Scholar]
- Schoenborn NL, et al. , 2013. Clinician roles and responsibilities during care transitions of older adults. Journal of the american geriatrics society, 61 (2), 231–236. [DOI] [PubMed] [Google Scholar]
- Smith MJ, Sainfort PC, 1989. A balance theory of job design for stress reduction. Int. J. Ind. Ergon 4, 67–79. [Google Scholar]
- Stanton NA, 2016. Distributed Situation Awareness. Taylor & Francis. [Google Scholar]
- Stanton NA, 2016. Distributed situation awareness. Theor. Issues Ergon. Sci 17 (1), 1–7. [Google Scholar]
- Stanton NA, et al. , 2006. Distributed situation awareness in dynamic systems: theoretical development and application of an ergonomics methodology. Ergonomics 49 (12−13), 1288–1311. [DOI] [PubMed] [Google Scholar]
- Vashi A, Rhodes KV, 2011. “Sign right here and you’re good to go”: a content analysis of audiotaped emergency department discharge instructions. Ann. Emerg. Med 57 (4), 315–322 e1. [DOI] [PubMed] [Google Scholar]
- Walker JM, Carayon P, 2009. From tasks to processes: the case for changing health information technology to improve health care. Health Aff. 28 (2), 467e477. [DOI] [PubMed] [Google Scholar]
- Waterson P, 2009. A critical review of the systems approach within patient safety research. Ergonomics 52 (10), 1185–1195. [DOI] [PubMed] [Google Scholar]
- Weick KE, 1976. Educational organizations as loosely coupled systems. Adm. Sci. Q 1e19. [Google Scholar]
- Wilson JR, 2000. Fundamentals of ergonomics in theory and practice. Appl. Ergon 31 (6), 557–567. [DOI] [PubMed] [Google Scholar]
- Wilson JR, 2014. Fundamentals of systems ergonomics/human factors. Appl. Ergon 45 (1), 5–13. [DOI] [PubMed] [Google Scholar]