Abstract
Minimally invasive operative techniques and enhanced recovery after surgery (ERAS) protocols have transformed clinical practice and made it possible to perform increasingly complex oncologic procedures in the ambulatory setting, with recovery at home after a single overnight stay. Capitalizing on these changes, Memorial Sloan Kettering Cancer Center’s Josie Robertson Surgery Center (JRSC), a free-standing ambulatory surgery facility, was established to provide both outpatient procedures as well as several surgeries that had previously been performed in the inpatient setting, newly transitioned to this ambulatory extended recovery (AXR) model. However, JRSC’s core mission goes beyond rapid recovery, aiming to be an innovation center with a focus on superlative patient experience and engagement, efficiency, and data-driven continuous improvement. Here, we describe JRSC’s genesis, design, care model, and outcome tracking and quality improvement efforts to provide an example of successful, patient-centered surgical care for select patients undergoing relatively complex procedures in an ambulatory setting.
Introduction
An outpatient cancer surgery center at Memorial Sloan Kettering Cancer Center (MSK) was initially proposed in 2010, when growth in surgical case volume was projected to outstrip operating room capacity at the main campus, Memorial Hospital, within the decade. Furthermore, an increasingly high inpatient census dominated by patients undergoing more and more complex medical treatment and surgical procedures made the idea of a short-stay center that could free up hospital beds appealing. The challenge was that the types of cases that needed to be moved were more complicated than those typically performed in the ambulatory setting, with average hospital stays of 2 to 4 days. Thus, a multidisciplinary team was created to plan a dedicated short-stay surgical facility and was first tasked with determining the procedures for which, with appropriate patient selection and management, patients could be safely discharged home after a single overnight stay while maintaining quality and providing an outstanding patient experience. While qualifying as ambulatory or outpatient from a regulatory standpoint, we distinguish these more complex, short-stay “ambulatory extended recovery” (AXR) procedures from conventional outpatient (OP) procedures in which the patient recovers and is discharged home in a few hours.
The freestanding nature and scale of the Josie Robertson Surgery Center (JRSC) provided an opportunity to build a “focused factory” solely dedicated to ambulatory cancer surgery1,2. Further, MSK leadership were committed to using the new facility to pioneer innovative approaches to patient-centered care, using modern principles for building and process design. Guiding questions included, “How can we become national leaders in delivering high-quality and cost-effective day and short-stay surgery? How can we maximally standardize processes and procedures? How do we continually assess progress to innovate and improve? How can we apply new technology to streamline processes and allow staff to focus on patients? What are the optimal roles for nurses and advanced practice providers within this short-stay environment? Most importantly, how can we ensure that the needs and experience of the patient and their loved ones are considered and prioritized in everything we do?”
Organizational Structure
The JRSC is part of MSK and operates as a hospital-associated outpatient clinic, attached to the Memorial Hospital ambulatory license, and all JRSC staff are employed at MSK. As such, patients come to MSK for their cancer care, and if surgery is indicated and the procedure and patient characteristics are appropriate (as described below), surgery may be scheduled at JRSC.
JRSC is staffed by a dedicated core team, as well as nurses, surgeons, and anesthesia providers that rotate from the main hospital campus. The senior leadership and administrative team consist of the Director, Chief of Surgery, Chief of Anesthesia, Director of Perioperative Nursing, Director of Innovation and Informatics, and Director of Logistics, Facility, and Support Services. The local leadership of most clinical and operational departments at JRSC report in a matrixed relationship to the home department at Memorial Hospital. JRSC staff total approximately 450 employees, excluding physicians, and including nurses, surgical technicians, patient care technicians, advanced practice providers, pharmacists, pathology technicians, physical therapists, and radiology technicians. Overnight, JRSC is staffed with an anesthesia provider for airway emergencies, and an in-house physician in case of any postoperative surgical or medical complications or other critical events requiring immediate intervention or hospital transfer.
Facility Design
The JRSC was designed and constructed for the sole purpose of surgical care, and does not contain clinics, offices, or other patient services. The 180,000 square-foot, 15-story facility holds 12 operating rooms, equipped with 4 dual-console surgical robots (Intuitive Surgical, Sunnyvale, CA), and 46 private patient rooms. Of the patient rooms, 18 function as both preoperative and outpatient post-anesthesia care unit (PACU) beds, and 28 are postoperative recovery rooms designed to accommodate overnight patients, featuring private bathrooms and pull-out sleepers for a caregiver (more than 60% of overnight patients at JRSC have a caregiver stay over). All patient rooms are equipped with wall-mounted PACU-level physiologic monitors, including those in which patients stay overnight. The patient makes “one stop post-op” and is cared for by a single, cross-trained team throughout their recovery.
Perioperative floors were designed for efficient workflows and to promote active recovery (Figure 1). Wrap-around floor-to-ceiling windows in private patient rooms allow in natural light and city views. A centralized hall, also referred to as the “oasis,” is a living room-like space where patients and caregivers may congregate and relax outside their individual rooms and access light snacks and drinks from an open pantry. Patients are encouraged to ambulate by the figure eight-shaped path around the oasis in close proximity to nursing staff. A separate family waiting area includes numerous comfortable and private seating arrangements, surgical consultation rooms, Wi-Fi access, charging stations, and a café and gift shop. The patient-centric design aesthetic is clean, modern, and functional.
Figure 1. Guest and patient areas.

Clockwise from top left: photos of the family waiting area, postoperative recovery floor, and representative patient room on one of these floors, and corresponding floor plan. Patient rooms are arranged in pairs with a remote nursing documentation station between to allow the care team to remain close to the bedside.
An important design element was the use of technology to facilitate patient flow, communication, data collection, supply chain, and documentation. Some, such as the real-time locating system (RTLS; Midmark Corp, Traverse City, MI), nurse call system (Rauland, Mt. Prospect, IL), and bedside hemodynamic monitors (GE Healthcare), were hard-wired into the building infrastructure during construction. Others were implementations of enterprise systems used across MSK, such as the EMR and communication systems. These systems were customized and integrated with specialized interfaces to create the functionalities described below.
Establishment of Care Program
The surgical services, surgeons, and procedures performed at JRSC were carefully selected to ensure a high volume of consistently performed procedures with a high probability of successful discharge the day after surgery. The planning committee selected 5 surgical services (Breast, Plastics & Reconstructive Surgery, Urology, Gynecologic Oncology, and Head and Neck Surgery) to develop pilot AXR programs at the main hospital, identifying procedures, standardized management processes, and criteria for appropriate patient selection. These services selected the following initial procedures for transition to AXR: mastectomy with and without immediate tissue expander reconstruction, laparoscopic and robotic prostatectomy, laparoscopic and robotic partial and total nephrectomy, laparoscopic and robotic hysterectomy and pelvic surgeries, and thyroidectomy, parotidectomy, and limited neck dissections. Over the 5 years prior to JRSC’s opening, over 9,000 of these procedures were performed, allowing refinement of processes and continuous tracking of outcomes including on-time discharge, complications, and patient satisfaction. The MSK experience with the transition to AXR for minimally invasive prostatectomies over several years was recently described3.
Within these services, surgeons with sufficient volume of appropriate OP and AXR cases were invited to move one or more of their main campus operating room (OR) schedule blocks to JRSC. The Breast surgery service was moved nearly entirely to JRSC with the exception of cases requiring flap reconstruction, which require a several-day hospital stay and so are performed at the main campus. Since opening, several surgeons from the Gastric and Mixed Tumor Service have also started operating at JRSC, mainly performing melanoma, peripheral sarcoma, and minimally invasive incisional hernia repairs. Traditional OP procedures, performed only by these designated JRSC surgeons, constitute about 64% of JRSC surgical volume.
Patient Selection and Expectation Setting
Determining patient eligibility preoperatively is a key component of safe patient care at a free-standing surgery center, which is undertaken systematically to accommodate as many JRSC-appropriate cases as possible. While we initially specified a number of rigid exclusion criteria, including body mass index (BMI) > 45, presence of an automatic implantable cardioverter-defibrillator, and end-stage renal disease on dialysis, it quickly became apparent that these criteria should instead serve as flags for individualized evaluation4,5. When a surgeon determines that a patient has these or other serious medical co-morbidities, direct communication with the anesthesia team permits early assessment of whether surgery at JRSC is appropriate for the patient, and prompt scheduling at the proper location. Medical comorbidities only prevent a patient from having surgery at JRSC if is anticipated that they will require an extended hospital stay. In particular, patients with complex medical conditions having OP procedures can often be safely cared for because of the option to keep these patients overnight if necessary for additional observation or management.
One key to providing an outstanding experience for patients and their caregivers is education that sets clear, realistic expectations for the procedure and how they will be supported throughout pre- and postoperative management. For patients undergoing AXR procedures, the benefits and success of the short-stay approach are also emphasized. Videos and web-based educational materials further set expectations and prepare the patient for the experience, as well as making the facility seem already familiar when they arrive. We meet regularly with the staff from the surgeons’ offices and the preoperative testing clinic to keep them updated on current practices at JRSC and standardize messaging and language.
All surgical patients are evaluated by nurse practitioners overseen by an anesthesiologist at one of MSK’s several preoperative surgical testing sites. Evaluation includes indicated laboratory testing and specialist consultation based on the patient’s comorbidities and procedure complexity. All patients are evaluated for their risk of obstructive sleep apnea (STOP-Bang criteria4,6), alcohol withdrawal (CAGE assessment7), and postoperative nausea and vomiting (PONV, Apfel score8); standardized pathways include adjustments to manage patients according to their individual risk of complications. After evaluation, an anesthesiologist reviews patient charts and serves as the main gatekeeper for determining if a patient is ultimately appropriate for JRSC, with input from surgeons, surgical physician assistants, and consulting physicians if concerns about patient eligibility arise.
Standardized Pathways and Care Management
JRSC’s efficient operations and its patients’ rapid recovery are enabled by standardized pathways guiding perioperative practices and patient flow. Clinical care standardization spans the surgical care timeline from preoperative evaluation and testing (above) to anesthesia care and surgical instrumentation through postoperative management.
Preoperative evaluation and surgical preparation.
All administrative and clinical requirements are completed prior to the day of surgery to expedite patient flow; for example, insurance coverage and clearance are pre-confirmed and preoperative clinical evaluations (including all lab testing) are completed before the patient’s arrival. A concierge personally escorts patients from the lobby to the waiting area for check-in, where both patient and caregiver receive a RTLS badge used to automate flow and communication, obviating the need for overhead paging. When it is time for the patient to go to the pre-surgical center (PSC), the unit assistant locates them by RTLS and escorts them there.
In the PSC, a perioperative nurse performs a standardized pre-surgical assessment, reviews surgical consent forms, administers day of surgery pre-ordered medications, places an intravenous catheter, and describes the next steps for the patient. During this time, the patient is also interviewed by the anesthesiologist and a member of the surgical team, who marks the surgical site. Nerve blocks, when indicated, are performed in PSC by a dedicated block anesthesiologist supported by trained nurses. As staff enter the room, their name and role are transmitted from the RTLS to the wall-mounted TV to identify them to the patient and family. When the operating room is ready, the perioperative nurse accompanies the patient to the operating room and directly hands-off care to the operating room nurse. As the patient leaves PSC, the RTLS detects the move, marks the room as dirty and notifies the environmental services team that room turnover is needed, alerts the attending anesthesiologist, and logs the “in OR” time in the electronic medical record (EMR). This allows the OR team to focus on welcoming and preparing the patient rather than documenting times and paging staff.
Operative efficiency.
In the operating room, case-specific instrument and supply case carts are prepared in advance and staged in the adjacent sterile core. Standardized case carts help reduce variability, promote timely set-up between cases, and ensure the availability of appropriate equipment. All supplies are tagged with radio-frequency identification (RFID) on arrival to the facility and electronically scanned into each case as they are consumed to facilitate documentation and inventory control (Helios, ARC Healthcare Technologies, Orion, MI). Surgical instrument trays are also tracked electronically for inventory and quality control. Specialty-trained surgical physician assistants further insure that workflows, including pre- and post-op orders, site marking, positioning, draping, and so on, are carried out consistently and efficiently.
Standardized anesthesia care.
Intraoperative anesthetic management is also protocolized according to principles drawn from the enhanced recovery after surgery (ERAS) literature9,10. These pathways aim to minimize use of opioid analgesics, utilize regional anesthesia techniques when feasible, and decrease PONV. Examples of ERAS components include liberalized guidelines regarding preoperative oral intake to promote hydration, administration of PONV prophylaxis in patients at high risk, preoperative paravertebral blocks and oral gabapentin for patients undergoing mastectomy with immediate reconstruction, total intravenous anesthesia including dexmedetomidine to further reduce opioids and PONV for patients who are undergoing tissue expander replacement, and intraoperative fluid management guidelines for patients undergoing robotic-assisted prostatectomy. Compliance with these protocols is monitored and outcome data are regularly reviewed to drive protocol refinement.
Communication with patients and caregivers during surgery.
To put caregivers at ease while their family member is in surgery, a nurse liaison locates them by RTLS and checks in on them to answer questions and provide updates. In addition, patient status boards, with coded patient identifiers known to their family members, provide real-time updates on the patient’s progress through surgery and indicate when visitors may come to the postop room (Figure 2). Caregivers may also provide a mobile phone number so that these updates are automatically texted directly to them.
Figure 2. Patient status board.
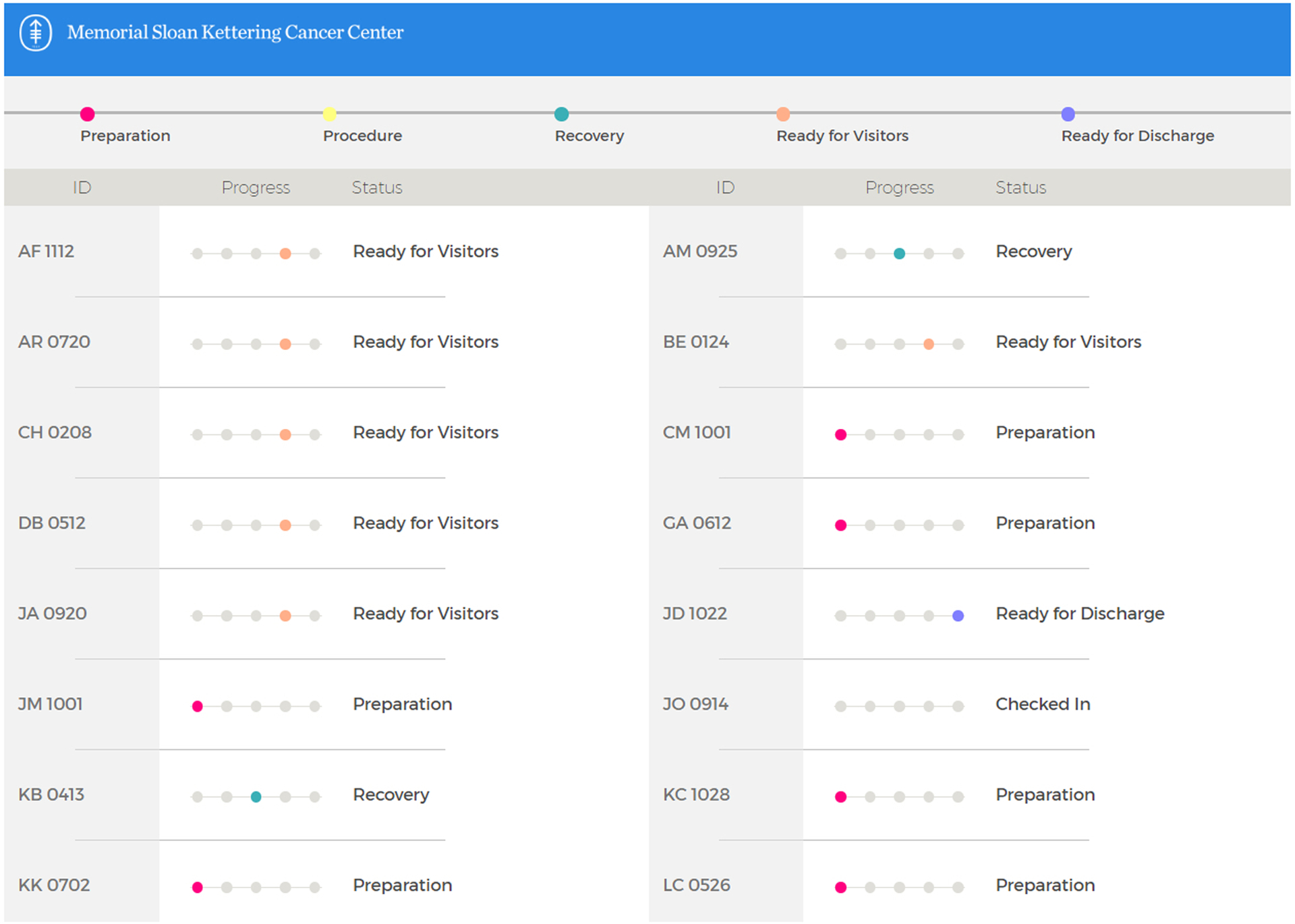
Patients are identified by codes known to their family members.
Postoperative management.
Following completion of surgery, patients are transported to their postoperative room by the anesthesia provider and a member of the surgical team, who transfer care to the recovery room nurse and advanced practice provider. The RTLS system automatically captures the “out of OR” time and, on entry to the postop room, claims the pre-assigned room for the patient, directing the hemodynamic data from the monitor to that patient’s EMR. For AXR procedures, the appropriate care pathway is enabled by a single electronic order and includes standardized medications, laboratory tests, other indicated elements such as physical therapy for mastectomy patients, and timed benchmarks for progress in activity level and diet advancement. Nurses review recovery milestones and goals, emphasizing early ambulation, with the patient and their caregivers to enable participation in their progress towards discharge (Figure 3). All nursing assessments are documented using structured data in the EMR so that patients not meeting benchmarks are immediately flagged in both the EMR and on status boards, enabling the care team to focus on getting them back on track. In addition, the patient’s cumulative distance ambulated is captured by the RTLS system, transmitted to the EMR and displayed on status boards along with other progress indicators. (A system to provide patients with ambulation goals and real-time feedback to “gamify” recovery is under development.)
Figure 3. Example recovery progress plan slide for patient counseling.
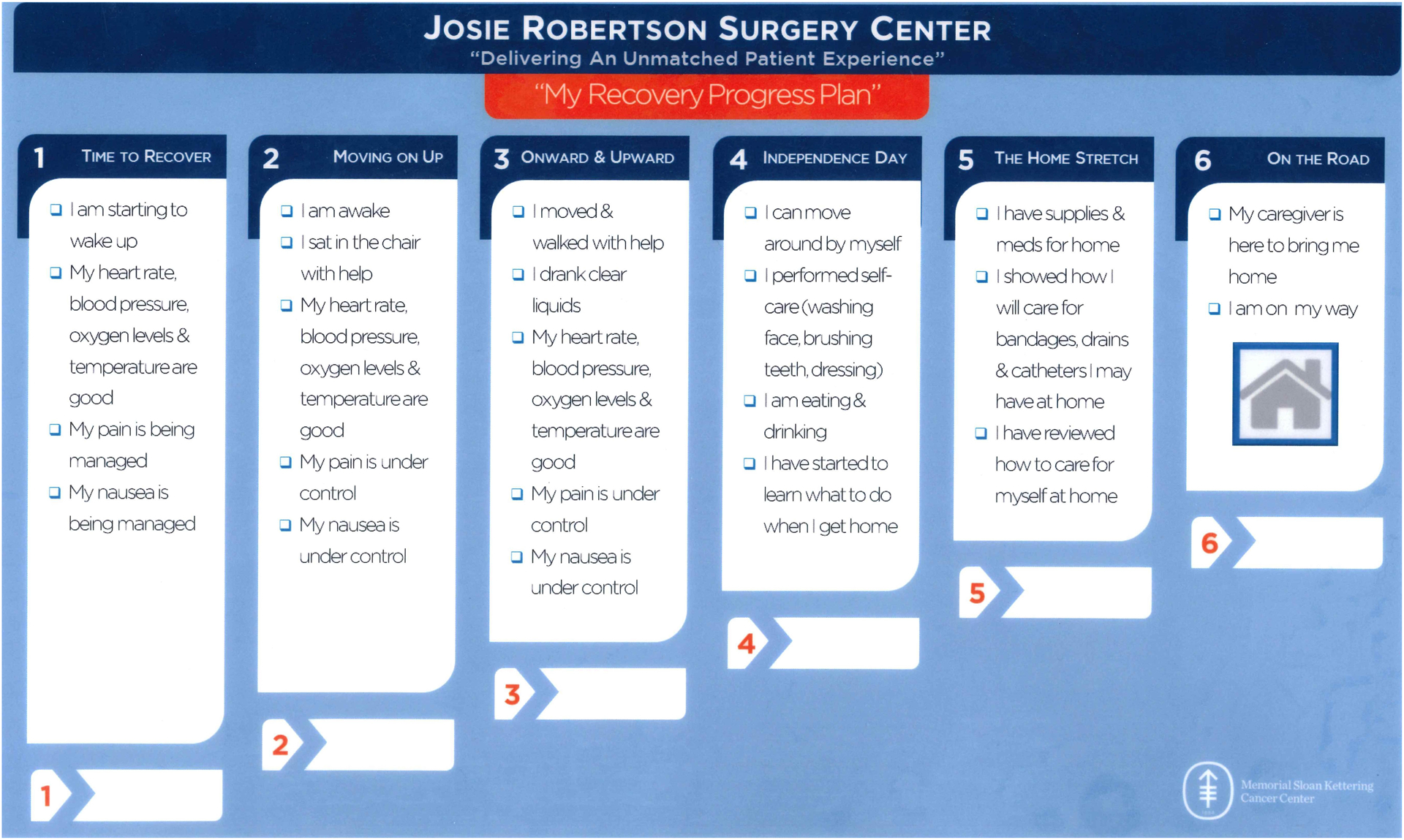
Milestones and goals for the stages of recovery are reviewed with each patient and caregiver to enable participation in their progress toward discharge.
While the majority of AXR patients stay overnight, patients may return home whenever they complete their pathway and meet discharge criteria. Some pathways obligate an overnight stay, such as prostatectomy, which includes a 14-hour postop creatinine test, or mastectomy, for physical therapy the morning after surgery. In the morning, breakfast is not served in bed but is provided as a buffet in the oasis, sending an empowering message that patients can do things for themselves. Patients are discharged the following morning when ready and are not held for a visit by the surgical team, but every room is equipped for tele-visits at the surgeon’s discretion. Any discharge prescription medications can be provided by the JRSC outpatient pharmacy. The median discharge time for overnight AXR patients is approximately 11 am (interquartile range, 10 am-12 pm). (We report discharge time rather than length of stay because this parameter is independent of surgery time11.)
Patients are required to have a responsible adult escort them home, as is usual after outpatient surgery, and are educated by their surgeons’ office practice nurses to arrange for their care needs for the immediate postoperative period. We do not routinely arrange home health care or visiting nurse support, but for patients with particular needs, social work assists in planning.
Postoperative communication—the Recovery Tracker.
The day after discharge, a JRSC nurse telephones the patient to assess their condition, answer any questions, and reinforce key discharge instructions. Patients are also sent daily reminders for 5 to 10 days after surgery (depending on procedure complexity, see below) to complete the Recovery Tracker, a brief electronic survey assessing symptoms such as pain, fatigue, nausea, fever, and wound condition, administered via the MyMSK Patient Portal. Each question/response set has pre-identified thresholds which, if triggered, send a notification to the surgeon’s care team. For intermediate symptoms such as moderate pain or nausea, a “yellow alert” is sent and the office practice nurse contacts the patient during regular business hours for follow-up. For concerning symptoms that should not wait for business hours, such as acute shortness of breath or very severe pain, a “red alert” is sent to the care team but also pops up on the patient’s screen, instructing them to immediately contact the office or, after hours, the call team.
For AXR procedures and selected procedures expected to have a higher symptom burden, the Recovery Tracker includes 14 questions covering 12 symptoms, as well as whether the patient has contacted their physician or visited an emergency room, and is sent each of the 10 days post-discharge. These questions were modified from the Patient-Reported Outcomes version of the Common Terminology Criteria for Adverse Events (PRO-CTCAE) system from the National Cancer Institute12. For less complex procedures, the questionnaire covers 6 symptoms plus emergency room visits and is sent for 5 days. Procedure-specific questions and alert thresholds are regularly reviewed and refined based on feedback from patients, caregivers, and office practice nurses to maximize their relevance and value while minimizing the burden on patients and office staff.
Our early experience with the Recovery Tracker has led to a PCORI (Patient-Centered Outcomes Research Institute)-sponsored randomized trial (NCT03178045) comparing the “team monitoring” response to alerts described above to “enhanced feedback,” where patients receive immediate normative feedback comparing their reported symptoms to what is expected based on other patients undergoing the same procedure (Figure 4)13. The goals of this ongoing trial are to reduce avoidable emergency department visits and enhance patient autonomy, and the results will help inform the appropriate response to these patient-reported data.
Figure 4. Example of enhanced feedback report.
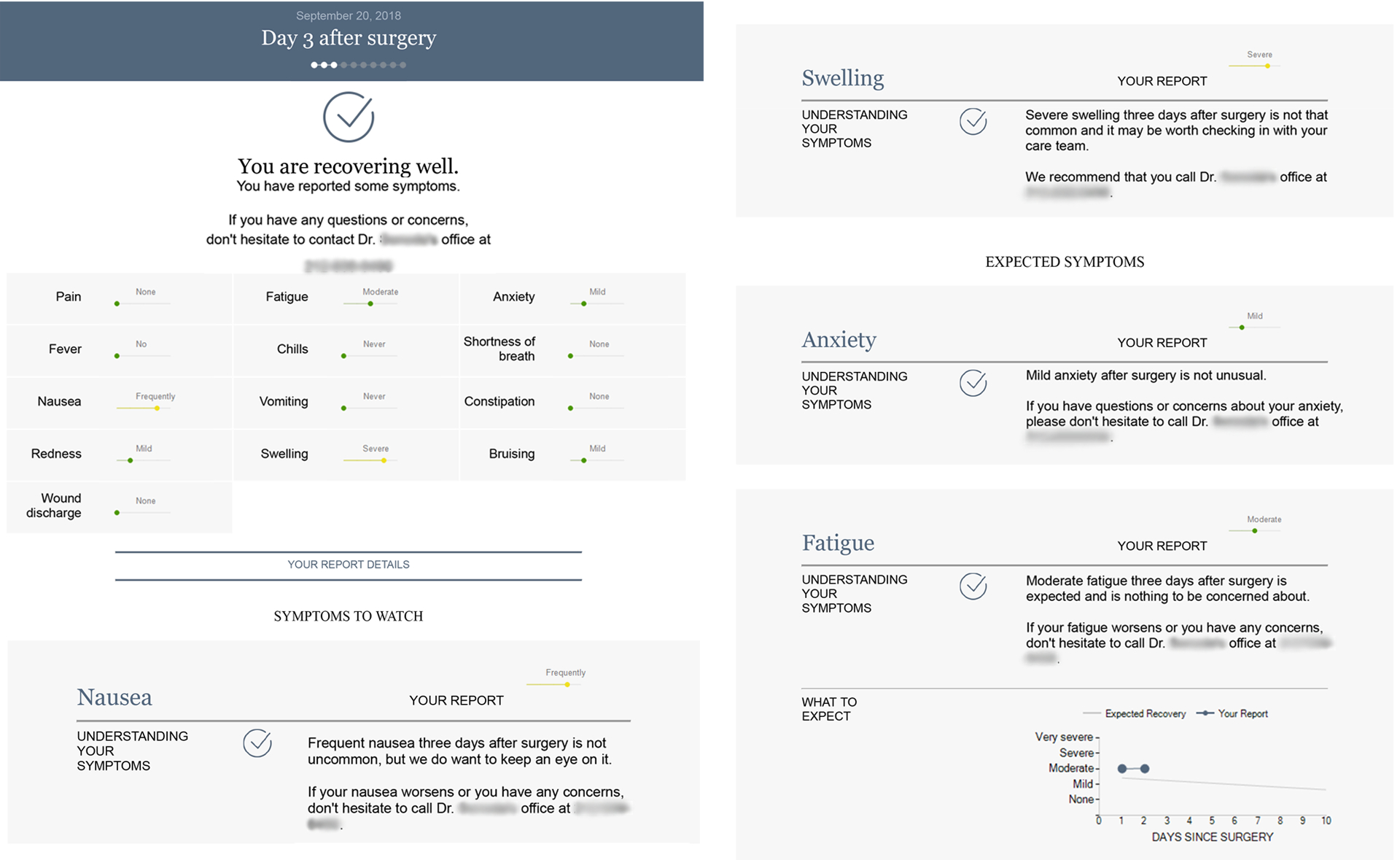
Patients in an ongoing clinical trial are randomized to receive either “team monitoring” or “enhanced feedback” in response to their reported symptoms13. See text for details.
Continuous Quality Improvement
Dedication to continuous learning, improvement, and innovation is part of JRSC’s core mission. To foster transparency and identify opportunities for improvement, the Clinical Operations Working Group, which consists of members of the nursing, anesthesia, surgery, advanced practice providers, and key operations teams, convenes twice monthly to review case volume, quality metrics (e.g. admissions, transfers, re-operations, outpatient extended stay patterns), emergency protocols, case cancellations, and other issues related to screening and management of patients. In particular, systems issues affecting patient care and workflows are reviewed with stakeholders and modified and adapted as needed. A brief weekly huddle with representation from all departments, both clinical and non-clinical, is held to insure all are updated on organizational priorities, trends and changes that impact operations (i.e., facility repairs or maintenance, new clinical programs, informatics upgrades, regulatory priorities, etc.). To plan and implement formal improvement initiatives, ranging from clinical workflow refinement to supply chain efficiency to staff safety, project teams are formed, supported by project facilitators or improvement engineers as needed. Improvement projects are also supported and conceptualized by the Clinical Research Working Group, which meets monthly and encourages involvement of non-physician clinical staff.
An important aspect of our improvement program is staff engagement and development. The Patient Framework Steering Committee, consisting of managers and front-line staff from across the facility, was created to drive initiatives that promote continued engagement and development of staff and to recognize outstanding employees who consistently go above and beyond in providing patient-centered care.
Volumes and Outcomes
In its first 3 years of operation, over 21,000 procedures have been performed at JRSC on 7 services, of which 7,663 (36%) were AXR, 13,525 (64%) outpatient (Table 1), and 3,081 (15%) robotically assisted. Overall, 151 patients (0.7%) underwent immediate (within 36 hours) reoperation, of which approximately 2/3 occurred at JRSC (reoperations after ORs close for the day require transfer to Memorial Hospital). Nearly all (98%) of reoperations were for confirmed or suspected bleeding, most frequently after breast and/or breast reconstructive surgery (94.7%).
Table 1. Case volumes by service 2016–2018.
Data are presented as n (%).
| Service | Cases | OP | AXR |
|---|---|---|---|
| Breast | 10,479 (49.5%) | 7,436 (71.0%) | 3,043 (29.0%) |
| Plastics | 3,682 (17.4%) | 3,605 (95.2%) | 177 (4.8%) |
| Gynecology | 2,844 (13.4%) | 1,646 (57.9%) | 1,198 (42.1%) |
| Urology | 2,543 (12.0%) | 127 (5.0%) | 2,416 (95.0%) |
| Head and neck | 1,260 (5.9%) | 430 (34.1%) | 830 (65.9%) |
| GMT | 369 (1.7%) | 270 (73.2%) | 99 (26.8%) |
| Dental | 11 (0.1%) | 11 (100.0%) | 0 (0.0%) |
| Total | 21,188 (100.0%) | 13,525 (65.4%) | 7,763 (36.6%) |
OP, outpatient; AXR, ambulatory extended recovery; GMT, Gastric and mixed tumor service.
If a patient develops an acute medical condition that requires more advanced treatment than can be provided at JRSC (including cross-matched transfusion), requires extended observation or treatment, or is otherwise unable to be discharged home on the first postoperative day, they must be transferred to an inpatient setting. Transfers to Memorial Hospital or nearby New York Presbyterian Hospital (for acute cardiac or neurologic care) occurred in 162 (0.8%) cases, with rates of 0.3% for OP cases and 1.7% for AXR (Table 2). Of these 162 transfers, the majority (45%) were for confirmed or suspected bleeding, for after-hours reoperation, and/or for cross-matched transfusion. Of these, 40 underwent reoperation and 22 ultimately received a transfusion (1–4 units of blood, average 2.1 units). Only 2 patients received 1 unit each of emergency blood at JRSC. Cardiac (13.3%) and neurologic (10.1%) issues were the next most frequent reasons for transfer, followed by abnormal lab values (5.7%), and severe allergic reactions to isosulphan blue dye used to assist in lymph node detection during breast surgery (6 patients; 3.8%).
Table 2. Transfers, re-operations, and 30-day MSK Urgent Care (UCC) visits and readmissions 2016–2018.
Data are presented as n (%).
| Total (n = 21,188) |
Outpatient (n = 13,525) |
AXR (n = 7,763) |
|
|---|---|---|---|
| Transfer | 162 (0.8%) | 41 (0.3%) | 132 (1.7%) |
| Re-operation | 151 (0.7%) | 54 (0.4%) | 101 (1.3%) |
| 30-day UCC visit | 755 (3.6%) | 26 (1.9%) | 512 (6.6%) |
| 30-day readmission | 339 (1.6%) | 135 (1.0%) | 202 (2.6%) |
Re-operation, return to OR within 36 hours; UCC, MSK Urgent Care Center.
Of note, the AXR transfer rate of 1.7%, which has been essentially unchanged since our opening, is significantly lower than the 7–9% rate3 at which patients in the pilot AXR program failed to be discharged on post-op day 1 (an equivalent metric in the inpatient setting). We attribute this large decrease in part to appropriate patient selection, but most importantly to the much higher physical and psychological barriers to keeping a JRSC patient an extra night. At JRSC, this requires an ambulance transfer, which is potentially stressful and upsetting for the patient and family, and a subsequent team review of the reasons for the transfer. These factors effectively eliminated “soft” reasons for extending stays, such as patient ambivalence about going home, and were accompanied by greatly improved education and expectation setting for patients at pre-surgical office visits.
Within 30 days of surgery at JRSC, 3.6% of patients returned to the MSK Urgent Care Center (UCC) and 1.6% were readmitted (Table 2). Again, these rates were higher for AXR patients (6.6% of whom visited the UCC and 2.6% were readmitted) than for outpatients (1.9% visited UCC and 1.0% were readmitted). Note these rates are only for patients returning to MSK facilities and do not capture patients going to local clinics, emergency rooms, or hospitals, thus underestimate the overall rate of patients’ post-discharge acute care. Two patients died within 30 days of surgery, both of whom had undergone palliative procedures unrelated to their cause of death. Patient satisfaction is measured by the OAS CAHPS (Outpatient and Ambulatory Surgery Consumer Assessment of Healthcare Providers and Systems) survey14, implemented at JRSC in late 2017 and delivered to all patients (75% electronically and 25% paper). For calendar year 2018, OAS CAHPS reports placed JRSC at the 98th percentile of large (greater than 3,000 surgeries) peer group hospitals and 99th percentile of American Nurses’ Credentialing Center (ANCC)-designated Magnet Hospitals for overall patient satisfaction. In November 2019, JRSC was awarded a Press Ganey “Guardian of Excellence” award for placing in the 95th percentile or above for OAS CAHPS-measured overall patient experience for an entire year15.
Key Learning Points
As many organizations build new facilities and redesign existing processes in the service of improving clinical care, quality, efficiency, and the patient experience, we offer a few key learning points from our experience. First, from the outset organizational leadership must be committed to rethink traditional approaches, end-to-end and on all fronts, with a unifying focus on the experience of the patient and their caregivers. Early engagement of clinicians and other stakeholders, including patients, in the care redesign process is also essential. Both clinical and operational processes should be maximally standardized, and technology modified to enable clinicians to prioritize spending time with patients rather than with computers. Finally, systems should be designed to provide granular and actionable data, and those data made readily available to stakeholders, to guide both daily operations and continuous improvement. While we recognize that these concepts may seem obvious to some and unattainable to others, we found that articulating and committing to these principles helped us to drive change and innovation across many fronts simultaneously.
Conclusion
The JRSC is an innovative free-standing ambulatory surgery center designed from the outset for patient-centered care that has provided successful care for a high volume of patients undergoing complex cancer surgery in the past 3 years. JRSC’s patient-centered approach relies on standardized pathways throughout the facility from patient flow to anesthesia, surgical, and postoperative management, and coordinated healthcare teams. Our novel implementation of technology aids in communication and promotes efficiency in a high-turnover surgery center. Continuous improvement activities are embedded in all aspects of clinical, as well as facility and support team, operations. We anticipate that these strategies will enhance patient satisfaction, reduce costs through shorter lengths of stay, decrease the risk of nosocomial infection, and accelerate and promote recovery.
Acknowledgments
The authors thank Jessica Moore for editorial assistance and all the staff of the Josie Robertson Surgery Center and Memorial Sloan Kettering Cancer Center who contributed to the design, implementation, and continuously improving delivery of extraordinary patient care at JRSC.
Glossary of Terms
- ANCC
American Nurses’ Credentialing Center
- AXR
ambulatory extended recovery
- BMI
body mass index
- EMR
electronic medical record
- ERAS
enhanced recovery after surgery
- JRSC
Josie Robertson Surgery Center
- MSK
Memorial Sloan Kettering Cancer Center
- OAS CAHPS
Outpatient and Ambulatory Surgery Consumer Assessment of Healthcare Providers and Systems
- OP
outpatient
- OR
operating room
- PACU
post-anesthesia care unit
- PCORI
Patient-Centered Outcomes Research Institute
- PONV
postoperative nausea and vomiting
- PRO-CTCAE
Patient-Reported Outcomes version of the Common Terminology Criteria for Adverse Events
- PSC
pre-surgical center
- RFID
radio-frequency identification
- RTLS
real-time locating system
- UCC
urgent care center
Footnotes
Conflicts of interest: None
Financial Disclosures: None
References
- 1.Christensen CM, Grossman JH, Hwang J. The Innovator’s Prescription: A Disruptive Solution for Health Care. McGraw-Hill Education; 2008. [Google Scholar]
- 2.Cook D, Thompson JE, Habermann EB, et al. From ‘solution shop’ model to ‘focused factory’ in hospital surgery: increasing care value and predictability. Health Aff (Millwood). 2014;33(5):746–755. [DOI] [PubMed] [Google Scholar]
- 3.Musser JE, Assel MJ, Meeks JJ, et al. Ambulatory Extended Recovery: Safely Transitioning to Overnight Observation for Minimally Invasive Prostatectomy. Urology Practice. 2015;2(3):121–125. [DOI] [PubMed] [Google Scholar]
- 4.Szeto B, Vertosick EA, Ruiz K, et al. Outcomes and Safety Among Patients With Obstructive Sleep Apnea Undergoing Cancer Surgery Procedures in a Freestanding Ambulatory Surgical Facility. Anesth Analg. 2019;129(2):360–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vertosick EA, Assel M, Tokita HK, et al. Suitability of outpatient or ambulatory extended recovery cancer surgeries for obese patients. J Clin Anesth. 2019;58:111–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chung F, Abdullah HR, Liao P. STOP-Bang Questionnaire: A Practical Approach to Screen for Obstructive Sleep Apnea. Chest. 2016;149(3):631–638. [DOI] [PubMed] [Google Scholar]
- 7.Ewing JA. Detecting alcoholism. The CAGE questionnaire. Jama. 1984;252(14):1905–1907. [DOI] [PubMed] [Google Scholar]
- 8.Apfel CC, Laara E, Koivuranta M, Greim CA, Roewer N. A simplified risk score for predicting postoperative nausea and vomiting: conclusions from cross-validations between two centers. Anesthesiology. 1999;91(3):693–700. [DOI] [PubMed] [Google Scholar]
- 9.Kehlet H, Dahl JB. Anaesthesia, surgery, and challenges in postoperative recovery. Lancet. 2003;362(9399):1921–1928. [DOI] [PubMed] [Google Scholar]
- 10.Kehlet H, Wilmore DW. Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg. 2008;248(2):189–198. [DOI] [PubMed] [Google Scholar]
- 11.Assel MJ, Laudone VP, Twersky RS, Vickers AJ, Simon BA. Assessing Rapidity of Recovery After Cancer Surgeries in a Single Overnight Short-Stay Setting. Anesth Analg. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Cancer Institute Division of Cancer Control and Population Sciences. Patient-Reported Outcomes version of the Common Terminology Criteria for Adverse Events (PRO-CTCAE™). https://healthcaredelivery.cancer.gov/pro-ctcae/. Accessed April 3, 2019.
- 13.Stabile C, Temple LK, Ancker JS, et al. Ambulatory cancer care electronic symptom self-reporting (ACCESS) for surgical patients: a randomised controlled trial protocol. BMJ Open. 2019;9(9):e030863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Medicare & Medicaid Services (CMS) and RTI International. Outpatient and Ambulatory Surgery CAHPS Survey. https://oascahps.org/, 2019.
- 15.Press Ganey. Guardian of Excellence Award Winners. 2019; https://www.pressganey.com/about/client-award-program/2019-guardian-of-excellence-award-winners.


