Abstract
Objectives
A multicentre survey was designed to evaluate the impact of COVID-19 outbreak on dental practice worldwide, estimate the COVID-19 related symptoms/signs, work attitudes and behaviour and the routine use of protective measures and Personal Protective Equipment (PPE).
Methods
A global survey using a standardized questionnaire with research groups from 36 countries was designed. The questionnaire was developed and pretested during April 2020 and contained three domains: 1) Personal data; 2) COVID-19 positive rate and symptoms/signs presumably related to the coronavirus; 3) Working conditions and PPE adopted after the outbreak. Countries’ data were grouped by the Country Positive Rate (CPR) during the survey period and by Gross-National-Income per capita. An ordinal multinomial logistic regression model was carried out with COVID-19 self-reported rate referred by dental professionals as dependent variable to assess the association with questionnaire items.
Results
A total of 52,491 questionnaires were returned with a male/female ratio of 0.63. Out of the total respondents, 7,859 dental professionals (15%) reported symptoms/signs compatible with COVID-19. More than half of the sample (n = 27,818; 53%) stated to use FFP2/N95 masks, while 21,558 (41.07%) used eye protection. In the bivariate analysis, CPR and N95/FFP2 were significantly associated (OR = 1.80 95%CI = 1.60/2.82 and OR = 5.20 95%CI = 1.44/18.80, respectively), while Gross-National-Income was not statistically associated with CPR (OR = 1.09 95%CI = 0.97/1.60). The same significant associations were observed in the multivariate analysis.
Conclusions
Oral health service provision has not been significantly affected by COVID-19, although access to routine dental care was reduced due to country-specific temporary lockdown periods. While the dental profession has been identified at high-risk, the reported rates of COVID-19 for dental professionals were not significantly different to those reported for the general population in each country. These findings may help to better plan oral health care for future pandemic events.
Keywords: COVID-19, SARS-CoV-2, Dentistry, Dental professionals, Personal Protective Equipment (PPE), Infection control, Oral Health, Global Health, Public Health Dentistry
1. Introduction
The COVID-19 outbreak worldwide has had severe repercussions on individual behaviours and social interaction. Viral transmission occurs mainly through inhalation/ingestion/direct mucous contact with saliva droplets. Additionally, the virus could stagnate on hands, objects or surfaces for a long time and remain infectious [1].
Among the many potential sources of transmission and spread of SARS-CoV-2, dental services have received high attention [2], [3], [4]. Dental professionals are at the front line of healthcare, working in the mouth, with a potentially increased viral exposure. Indeed, according to the USA's Occupational Safety and Health Administration agency, all dental healthcare personnel (dentist, dental hygienist and dental assistant) are included at the highest risk category for SARS-CoV-2 exposure [4]. The putative risk posed by the dental profession was widely conveyed on mainstream media [5]. Whether this assertion is justified and supported by worldwide data, is elusive. We, therefore, decided to explore this issue through a global multicentre research survey among dental professionals.
During the first months of the COVID-19 pandemic, with extremely high infection rates and relatively high mortality, many national authorities worldwide, including some dental organizations, imposed several restrictive measures on the profession. In most countries, dental care was restricted during the COVID-19 outbreak and limited only to urgent care. Implementation of effective infection control measures was recommended to prevent nosocomial coronavirus infection [6]. Thus, the dental profession was forced to change in March-April 2020 to accommodate to new regulations and guidelines. By the beginning of the pandemic and during lockdown periods, dental treatment has been generally suspended or postponed, except for urgent care. The response of the dental profession to COVID-19 has not been homogeneous. While some countries restricted dental care only to urgencies/emergencies, in others, where the pandemic had subsided or even during the phase of maximum infection rates, dental clinics and offices had returned/continued to also provide non-urgent dental care, but figures from global data are not available. Moreover, limited knowledge at that time, unavailability of tests, availability or incorrect use of Personal Protective Equipment (PPE) and conflicting protocols may have lowered protection among the dental care workforce and patients, potentially increasing the infection rate and transmission [7], [8], [9], [10]. This paper reports findings from the 2020 International Collaborative COVID-19 Disease Study giving, to the best of authors’ knowledge, the only updated worldwide observational epidemiological study on COVID-19 and dental professionals. The study describes morbidity due to COVID-19 among dental personnel in 36 countries/areas from May to August 2020, as well as the approaches to protective measures used to reduce the risk of viral infection and transmission.
The aim of this global survey was to evaluate the impact of the COVID-19 outbreak among dental professionals in different countries worldwide, via an extensive multicentre study. Due to the numerous data collected of this global study, this is the first paper of a series of epidemiological publications of dental professionals regarding COVID-19. The main aims were to estimate the impact of COVID-19 on oral health service provisions, the disease rate among dental professionals globally, describe self-reported symptoms/signs presumably related to COVID-19, and to investigate the adoption of protective measures and the PPE used to reduce the risk of viral infection and transmission.
2. Materials and Methods
2.1. Study design
The structured closed cross-sectional survey was developed with a modified Delphi method using a standardized questionnaire developed and pretested in Italy during April 2020 [9]. Briefly, following the Stehr-Green scale, the questionnaire was built up and structured into three domains: 1) personal data including age, gender, area of living and working, and working status; 2) dental professionals infection rate and symptoms/signs presumably related to the COVID-19; 3) working conditions and PPE adopted after the outbreak of the infection (Appendix 2). A pre-test before the Italian survey was performed with twelve dental professionals, reaching a satisfactory Intra-class Correlation Coefficient (ICC) value of 0.80 for each item.
The protocol of the study was previously described and registered in the World Pandemic Research Network (WPRN) WPRN-486352 [10]. The study follows the CHERRIES guidelines (the checklist is available as supplementary file). Thirty-six collaborating research groups around the world were contacted by the central management team and all agreed to participate. Each research team was instructed on the research protocol, the survey design and the participant search strategies by a central coordinator (GC). Research teams were formed individually in each country and tasks were assigned at their convenience.
2.2. Participants and study size
Dental professionals working in each national health system, either private or public, including general or specialists were enrolled. Each country performed a sample size calculation; the total number of working dental professionals was ascertained, and according to the previously published protocol, at least a high proportion of participants (5-20%) in each country was invited to participate, aiming to reach minimum 5% proportion [10]. In order to reach this purpose, each national team could use the strategies that best suited the context of their country. Study participants were reached in each country via adequate platforms to avoid duplicate answers, and the invites were sent through the national Dental Board systems, official web pages of national Dental Boards and/or social media groups/pages. The number of invited dental professionals ranged from all personnel registered by the national Dental Board to members of the professional social media groups. A mixed strategy was used; direct email to individual dental professionals, invitations to participate through national dental associations and other related organizations and dissemination on social media (i.e. Facebook), so it was not possible to estimate how many invitations had been disseminated in many countries. The number of respondents and relevant demographic data for each country is shown in Table 1 .
Table 1.
Participating Countries survey Information.
| Country | Population size (as of date) | Survey period (2020) | Total new cases in population (survey period) | N° dentists reported by the teams | Responders | % Positive/rate COVID-19 test in population | Oral health service provision/restrictions nationally(survey period) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Private | Public (Hospitals, etc.) | ||||||||||||
| Start | End | Urgent | Routine | None | Urgent | Routine | None | ||||||
| Africa | |||||||||||||
| Egypt | 102,334,404 | 16.07 | 31.07 | 9,827 | 19,111 | 925 | 24.41 | Yes | Yes, only | ||||
| Nigeria | 24,206,644 | 11.06 | 29.07 | 28,340 | 4,000 | 438 | 2.10 | Yes | Yes, only | ||||
| Tunisia | 11,818,619 | 08.07 | 25.07 | 237 | 4,500 | 871 | 1.51 | Yes | Yes | ||||
| America | |||||||||||||
| Argentina | 44,938,712 | 16.06 | 31.07 | 147,419 | 54,000 | 1,422 | 34.43 | Yes, only | Yes, only | ||||
| Brazil | 212,559,417 | 27.07 | 31.07 | 215,589 | 645,889 | 1,837 | 30.15 | Yes, only | Yes, only | ||||
| Chile | 19,116,201 | 20.07 | 01.08 | 26,821 | 21,541 | 2,307 | 10.98 | Yes, only | Yes, only | ||||
| Colombia | 50,882,891 | 19.06 | 24.07 | 212,382 | 36,000 | 5,375 | 26.60 | Yes, only | Yes, only | ||||
| El Salvador | 6,486,205 | 12.07 | 21.07 | 3,065 | 2,100 | 543 | 12.40 | Yes, only | None | ||||
| Peru | 32,971,854 | 25.07 | 31.07 | 38,744 | 30,000 | 1,759 | 23.55 | Yes | None | ||||
| USAa | 39,512,223 | 05.06 | 31.07 | 370,687 | 28,800 | 562 | 7.00 | Yes, only | Yes, only | ||||
| Venezuela | 28,435,940 | 18.07 | 28.07 | 5,134 | 12,000 | 638 | 5.46 | Yes | None | ||||
| Asia and Oceania | |||||||||||||
| Chinab | 58,500,000 | 13.07 | 28.07 | 0 | 7,750 | 1,116 | 0 | Yes | Yes | ||||
| India | 1,380,004,385 | 11.07 | 25.07 | 543,059 | 277,303 | 3,265 | 10.92 | Yes, only | Yes, only | ||||
| Malaysia | 32,365,999 | 01.07 | 15.07 | 92 | 11,108 | 2,904 | 0.09 | Yes | Yes, only | ||||
| Pakistanc | 220,892,340 | 16.07 | 30.07 | 21,633 | 2,226 | 425 | 16.27 | Yes | Yes, only | ||||
| Saudi Arabia | 34,813,871 | 02.07 | 30.07 | 81,767 | 16,752 | 857 | 5.17 | Yes, only | Yes, only | ||||
| Singapore | 5,850,342 | 15.07 | 02.08 | 6,229 | 2,390 | 355 | 7.30 | Yes | Yes | ||||
| Australia | 25,667,000 | 13.07 | 31.07 | 6,750 | 16,861 | 815 | 0.69 | Yes | Yes | ||||
| Europe | |||||||||||||
| Albania | 2,877,797 | 16.07 | 31.07 | 2,850 | 2,776 | 206 | 39.1 | Yes, only | Yes, only | ||||
| Belgium | 115,89,623 | 30.07 | 04.08 | 3,273 | 10,080 | 782 | 2.68 | ||||||
| Bosnia | 3,280,819 | 29.06 | 12.07 | 2,863 | 2,233 | 213 | 17.0 | Yes | Yes | ||||
| Cyprus | 1,207,359 | 16.07 | 31.07 | 62 | 1,017 | 176 | 0.49 | Yes | Yes | ||||
| Georgia | 3,989,167 | 10.07 | 31.07 | 192 | 3,050 | 317 | 1.48 | Yes | Yes | ||||
| Greece | 10,423,054 | 16.07 | 31.07 | 518 | 10,200 | 46 | 0.44 | ||||||
| Germany | 83,783,942 | 04.06 | 16.06 | 4,469 | 70,740 | 3,542 | 0.70 | Yes | Yes | ||||
| Italy | 60461826 | 04.05 | 18.05 | 15,293 | 49,413 | 8,284 | 2.90 | Yes, only | Yes, only | ||||
| Lithuania | 2,722,289 | 12.07 | 24.07 | 99 | 3,800 | 204 | 0.46 | Yes | Yes | ||||
| Macedonia | 2,083,374 | 16.07 | 31.07 | 2,232 | 2,800 | 24 | 10.4 | Yes, only | Yes, only | ||||
| Montenegro | 628,066 | 16.07 | 31.07 | 1,184 | 591 | 110 | 14.84 | Yes | Yes | ||||
| Netherlands | 17,134,872 | 08.07 | 06.08 | 5,724 | 8,600 | 372 | 1.00 | Yes | Yes | ||||
| Romania | 19,237,691 | 16.07 | 31.07 | 16,006 | 16,442 | 1,051 | 4.72 | Yes | Yes | ||||
| Russia | 145,934,462 | 09.06 | 07.26 | 339,047 | 50,000 | 1,011 | 12.55 | Yes, only | Yes, only | ||||
| Serbia | 8,737,371 | 16.07 | 31.07 | 6,230 | 4,677 | 1,460 | 4.06 | Yes | Yes | ||||
| Spain | 46,754,778 | 29.05 | 11.06 | 4,374 | 38,000 | 2,318 | 0.80 | Yes, only | Yes, only | ||||
| Switzerland | 8,654,622 | 02.07 | 15.07 | 1,300 | 5,777 | 1,324 | 1.26 | Yes | Yes | ||||
| UK | 67,886,011 | 01.06 | 04.07 | 31,751 | 39,500 | 4,637 | 1.09 | Until 08.06 | Yes | Yes, only | |||
| TOTAL | 52,491 | ||||||||||||
aUSA/California; bChina/Hubei; cPakistan/Lahore; ^https://www.worldometers.info/coronavirus
2.3. Bias
The platform used to collect data and run the survey in each country was set to avoid duplicate answers. The duration of the survey in each country was at least one week according to the previously published protocol [10] (Table 1). All national research teams sent accurately collected and organized data according to the protocol, with the written report on country level data.
Each country/region translated the questionnaire, performed a pilot test and semantically adjusted the questions, if necessary. The same core questionnaire was mandatorily applied to all participating countries, regardless of optional additional questions incorporated by each national team. The full questionnaire is presented as supplementary material (Appendix 2). A description of the survey's aim along with the link to the questionnaire and an online informed consent were provided to each participant in accordance with the applicable data protection laws of the respective countries. In some countries, the project protocol and the consent form were approved by the local Ethics Committee. Each participant was defined by a unique identification number based on IP address. Participants were allowed to review and correct their answers, but if they did not sign the consent, the questionnaire was automatically closed. Data collection timeframe was from May to August 2020. All data were stored in a repository using a Research Electronic Data Capture (REDCap) account.
2.4. Independent variables and data sources
Data from all the participating countries were stratified in several ways:
-
-
if the dental professionals in the different countries continued to work routinely during the lockdown or limited the clinical activity to emergencies only;
-
-
by the country/region (i.e. California not U.S.A. etc.) community positive rate (CPR) of COVID-19 during the survey period (Table 1) [11]. The CPR were calculated using the Git Hub data [12] and, where internationally available data were not updated, by the national research teams obtaining data from the official national web page reporting COVID-19 statistical recourses in each local language.
-
-
by Gross National Income (GNI) per capita 2019, Atlas method and Purchasing Power Parity (PPP, international dollar) [13].
2.5. Outcome variables
Ordinal multinomial linear regression analysis was run using the COVID self-reported rate as dependent variable to evaluate the association with questionnaire items. COVID self-reported rate was calculated using data derived from the questionnaire, reporting one or more specific or nonspecific COVID symptoms [14,15]. Clinical manifestations of COVID-19 appear after an incubation period of around 5–6 days and most frequently include fever, dry cough, tiredness with the possible onset of sputum production, headache, haemoptysis, diarrhoea, dyspnoea, and/or lymphopenia amongst others [16], [17], [18], [19], [20].
2.6. Statistical Analysis
Data were exported to an Excel (Microsoft Corp., WA, USA) spread sheet and quality-checked to ensure accuracy, sent to the management team (GC, MDB, MGC, TGW) and transferred to STATA16™ (Statacorp, TX, USA) for statistical analysis. The raw data were added as a supplementary file (Appendix 3). Data analysis was performed centrally. Demographic data and the impact of COVID-19 on dental professionals and oral health provision were descriptively presented.
All demographic data were completed without missing data. Missing data were present on the outcome variables and complete case analysis was selected as the primary analysis with no imputation [21,22]. Absolute and relative frequencies were calculated for each item. Differences in proportions were evaluated with χ2 test or Fisher exact test if one cell had a value of less than five. Multiple testing for post hoc estimation, such as the number of observed frequencies, expected frequencies, percentage, and contribution to the chi-square were run. Estimation of a nonparametric test for trend across the areas with different prevalence of COVID self-reported rate and questionnaire items were also calculated. The effect size was calculated using the Cramer's V, as a measure of the strength of association among the levels of the row and column variables. Ordinal multinomial linear regression analysis was run to evaluate the association with questionnaire items.
3. Results
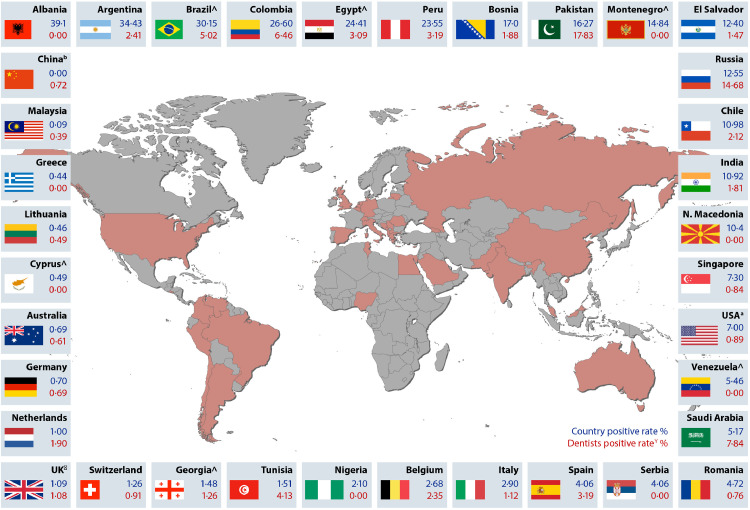
The map of the countries participating in the survey, the Country Positive Rate (CPR) to COVID-19 according to the survey period and COVID self-reported positive rate are displayed in Fig. 1 . A total of 52,491 dental professionals from the 36 countries completed the questionnaires. The total population, survey period (2020), total new cases during the survey period, the positive rate, the type of oral health care provision, the reported number of dental professionals, the hypothetical sample at the 5% level and the number of dental professionals reached in each country by continent, country/area is displayed in Table 1.
Fig. 1.
COVID-19 positive rates by countries. In blue colour, is reported the COVID-19 positive rate of the population (%) at the time point when the survey was conducted, while in red the cumulative COVID-19 positive rate (%) among dental professionals since the beginning of the pandemic.
aUSA/California; bChina/Hubei; cPakistan/Lahore; https://www.worldometers.info/coronavirus
3.1. Descriptive data
In most countries, the dental professionals sex ratio favoured women (i.e. in Russia 100% were women), whilst Switzerland had the highest ratio for males (1.97). More than 50% of the dental professionals in countries such as Argentina, Peru, USA/California, Venezuela, Australia, Albania, Belgium, Cyprus, Chile, Germany, Greece, Italy, Lithuania, Macedonia, Montenegro, Netherlands, Romania, Spain and Switzerland, reported to work as owners of a private practice. Working within a National Health System or at Universities or for administrative staff was reported highly by Nigerian, Chinese (province of Hubei), Malaysian, Singaporean and UK dental professionals. The majority were general dental professionals (43.2% versus 23.61% specialists), one third of the participants did not enter this item.
Table 1 shows the impact of the COVID-19 pandemic on the provision of routine oral health services globally. Only 14 of the 36 countries reported to perform routine cares across both private and public sectors during the survey period. Thirteen countries reported provision of emergency care only. Almost 80% (n = 41,776) of dental professionals continued providing some face-to-face clinical activities, many despite limited access to appropriate PPE.
3.2. Self-reported prevalence of COVID-19 in dental professionals
Overall, 15% of respondents (n = 7,859) reported symptoms/signs pertaining to COVID-19. This was higher in the Americas, in particular, Perú and El Salvador where more than two thirds of the respondents reported experiencing at least one symptom assumed to be from COVID-19. Of those who reported signs of having COVID-19, more than 90% reported to have worked clinically during the outbreak, while the remainder had only community level exposure, many unable to work or working from home offering remote dental advice (Teledentistry) and triage services.
Participating dental professionals were grouped by the positive rates registered at the country level (CPR) and by the COVID self-reported rate (Table 2 ). The COVID self-reported rate ranged between 0% in some Balkan Countries and Nigeria to over 10% in Russia (14.68%) and Pakistan (17.34%). At country level, the community rates of COVID-19 were usually higher than those reported by the dental participants, except for China, Malaysia, Netherlands, Pakistan, Russia, Saudi Arabia and Tunisia, where the results were higher for dental professionals than the CPR.
Table 2.
Dentists positive rate to COVID-19 and work condition in the participating dentists.
| Country | Dentists positive rate | Positive rate COVID-19 % | One or more symptoms | Dentist M/F ratio | Private | Public | Regular working load | Only emergencies |
|---|---|---|---|---|---|---|---|---|
| %¡ | N (%) | N (%) | N (%) | N (%) | N (%) | |||
| Pakistanc | 17.83 | 16.27 | 151 (36.39) | 0.40 | 149 (36.43) | 260 (63.57) | 98 (24.62) | 118 (29.65) |
| Russia | 14.68 | 12.55 | 118 (11.67) | 0.00 | 443 (43.81) | 552 (34.59) | 368 (36.44) | 475 (47.03) |
| Saudi Arabia | 7.84 | 5.17 | 257 (30.09) | 0.86 | 210 (24.59) | 628 (73.54) | 47 (5.52) | 383 (45.06) |
| Colombia | 6.46 | 26.60 | 721 (13.41) | 0.38 | 4327 (100.00) | 0 (0.00) | 126 (2.34) | 1002 (18.64) |
| Brazil^ | 5.02 | 30.15 | 188 (10.22) | 0.25 | 1161 (63.18) | 664 (36.13) | 87 (4.73) | 1057 (57.54) |
| Tunisia | 4.13 | 1.51 | 198 (22.73) | 0.52 | 494 (64.98) | 305 (35.02) | 15 (1.73) | 351 (40.53) |
| Spain | 3.19 | 4.06 | 291 (12.55) | 0.53 | 2073 (89.43) | 245 (10.57) | 18 (0.78) | 916 (39.52) |
| Peru | 3.19 | 23.55 | 1721 (97.84) | 0.60 | 1358 (77.22)° | 720 (40.93) | 42 (2.39) | 1187 (67.48) |
| Egypt^ | 3.09 | 24.41 | 191 (21.08) | 1.31 | 361 (39.99) | 545 (60.15) | 146 (15.79) | 416 (44.97) |
| Argentina | 2.41 | 34.43 | 130 (9.20) | 0.30 | 1166 (82.51) | 247 (17.48) | 20 (1.42) | 557 (39.42) |
| Belgium | 2.35 | 2.68 | 77 (9.51) | 0.73 | 661 (93.95) | 47 (6.05) | 280 (35.90) | 366 (46.92) |
| Chile | 2.12 | 10.98 | 38 (1.65) | 0.49 | 1592 (69.04) | 747 (32.93) | 96 (5.16) | 1047 (56.26) |
| Netherlands | 1.90 | 1.00 | 65 (17.91) | 0.47 | 368 (100.00) | – | 253 (69.70) | 109 (30.03) |
| Bosnia | 1.88 | 17.0 | 52 (24.41) | 0.43 | 123 (57.75) | 90 (42.25) | 13 (6.10) | 85 (39.91) |
| India | 1.81 | 10.92 | 430 (13.97) | 0.86 | 3302 (100.00) | 0 (0.00) | 24 (0.74) | 3240 (99.26) |
| El Salvador | 1.47 | 12.40 | 235 (43.26) | 0.50 | 265 (48.36) | 278 (51.19) | 20 (3.68) | 191 (35.17) |
| Georgia^ | 1.26 | 1.48 | 7 (2.20) | 0.38 | 242 (76.48) | 75 (23.66) | 31 (9.80) | 71 (22.40) |
| Italy | 1.12 | 2.90 | 1346 (16.25) | 0.66 | 7211 (87.05) | 1073 (22.95) | 171 (2.06) | 4075 (49.19) |
| UKÅ | 1.08 | 1.09 | 672 (14.49) | 0.85 | 893 (19.26) | 3738 (80.74) | 2121 (45.74) | 1102 (23.77) |
| Switzerland | 0.91 | 1.26 | 35 (2.65) | 1.97 | 1288 (97.32) | 36 (2.72) | 100 (7.58) | 296 (22.44) |
| USAa | 0.89 | 7.00 | 10 (1.78) | 0.63 | 467 (83.10)° | 95 (16.90) | 226 (40.14) | 222 (39.43) |
| Singapore | 0.84 | 7.30 | 121 (34.03) | 0.41 | 101 (28.44) | 254 (71.56) | 316 (89.01) | 14 (3.94) |
| Romania | 0.76 | 4.72 | 47 (4.47) | 0.26 | 736 (70.03) | 315 (29.97) | 0 (0.00) | 575 (54.71) |
| Chinab | 0.72 | 0.00 | 12 (1.08) | 0.55 | 476 (42.69) | 639 (57.31) | 40 (3.59) | 228 (20.45) |
| Germany | 0.69 | 0.70 | 77 (2.95) | 1.43 | 2619 (99.28) | 37 (0.72) | 170 (6.84) | 2140 (86.15) |
| Australia | 0.61 | 0.69 | 115 (14.11) | 0.63 | 674 (82.85) | 140 (17.15) | 78 (11.32) | 391 (56.75) |
| Lithuania | 0.49 | 0.46 | 13 (6.40) | 0.13 | 138 (67.98) | 25 (12.31) | 4 (1.97) | 42 (20.69) |
| Malaysia | 0.39 | 0.09 | 223 (7.67) | 0.13 | 134 (4.62) | 2770 (95.38) | 2161 (86.47) | 226 (9.04) |
| Albania | 0.00 | 39.14 | 5 (3.29) | 0.52 | 128 (84.21) | 24 (15.79) | 6 (3.95) | 23 (15.13) |
| Montenegro | 0.00 | 14.84 | 1 (1.91) | 1.11 | 104 (94.55) | 6 (5.41) | 18 (16.36) | 42 (38.18) |
| Macedonia | 0.00 | 10.4 | 0 (0.00) | 0.60 | 22 (91.67) | 2 (8.33) | 1 (4.17) | 6 (25.00) |
| Venezuela^ | 0.00 | 5.46 | 132 (20.69) | 0.26 | 614 (96.23) | 144 (3.77) | 17 (2.65) | 503 (78.60) |
| Serbia | 0.00 | 4.06 | 175 (11.99) | 0.35 | 1019 (69.80) | 441 (30.20) | 156 (10.68) | 697 (47.74) |
| Nigeria | 0.00 | 2.10 | 0 (0.00) | 1.62 | 98 (23.62) | 317 (76.39) | 81 (18.54) | 164 (37.53) |
| Cyprus^ | 0.00 | 0.49 | 4 (2.27) | 0.71 | 165 (93.75) | 170 (96.59) | 7 (3.98) | 78 (44.32) |
| Greece | 0.00 | 0.44 | 1 (2.17) | 0.80 | 40 (86.96) | 6 (13.04) | 8 (17.77) | 19 (42.22) |
| p-value | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 |
aUSA/California; bChina/Hubei; cPakistan/Lahore; ^data calculated by the authors, °private, no differentiated;
*In these Countries other dental personnel participate to the survey; their replies are not reported in this table; ¡Positive/Hospitalized, ÅIn UK the survey involved only dentists working in primary care
3.3. Protecting measures for patients and dental professionals
The precautionary measures adopted by dental professionals who continued to work after the COVID-19 outbreak are displayed in Table 3 . More than half of the dental professionals (n = 27,818; 53%) reported the use of FFP2/N95, while 41.07% (n = 21,558) declared the use of eye protection equipment. The percentage of dental professionals who reported routine use of protective mask (FFP2/N95) was notably high in South American countries with low GNI (Brazil, Peru and Colombia with 100%). In most countries, more than half of the dental professionals reduced the number of patient appointments to reduce crowding in the waiting room, with the highest percentage in countries with the highest GNI, i.e. Germany (93.84%). The patients’ health status and body temperature were checked by 57.6% of the respondents, with the highest prevalence in countries with the highest GNI (Australia 99.84% and Germany 91.05%). The use of mouthrinses intended to reduce SARS-CoV-2 salivary load was highly variable, but some trends between countries with different GNI were observed regarding the use of alcohol-containing mouthrinses and essential oils or cetylpyridinium chloride (p = 0.01 and p < 0.01, respectively) (data not tabulated).
Table 3.
Precautionary measures taken by dentists who continued to provide face to face clinical care after the outbreak of COVID-19. Countries were ranked by the COVID-19 positive rate by country. In Fig. 2 the COVID-19 positive rate by country and Dentists positive rates are reported.
| Before the arrival of the patients | In the operating room | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Country | Gross national income | Face-face activity | Phone triage | Appointment numbers reduced | Patients’ health status | Surface disinfection | Eye protection equipment |
N95/FFP2 mask |
TNT disposal gown |
|
| 70% ethyl alcohol | 0.5% sodium hypochlorite | |||||||||
| range | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Egypt | <5,000 | 679 (73.40) | 427 (62.88) | 410 (60.38) | 245 (36.08) | 599 (88.22) | 234 (34.46) | 78 (11.49) | 431 (63.48) | 48 (7.07) |
| El Salvador | <5,000 | 351 (64.64) | 169 (48.15) | 231 (65.81) | 283 (80.63) | 230 (65.53) | 229 (65.24) | 329 (60.58) * | 347 (98.86) | – |
| Georgia | <5,000 | 311 (98.11) | 212 (68.17) | 209 (67.20) | 196 (63.02) | 221 (71.06) | 130 (13.53) | 167 (53.70) | 216 (69.45) | 125 (40.19) |
| India | <5,000 | 3025 (92.65) | 1213 (40.10) | 1021 (33.75) | 1457 (48.17) | 2976 (98.38) | 1851 (61.19) | 1687 (55.77) | 1368 (45.22) | 2562 (84.69) |
| Nigeria | <5,000 | 399 (91.10) | 50 (12.53) | 135 (33.83) | 105 (26.32) | 89 (22.31) | 83 (20.80) | 155 (38.85)* | 120 (30.08) | 63 (15.79) |
| Pakistanc | <5,000 | 272 (64.00) | 222 (81.62) | 52 (19.12) | – | 155 (56.99) | 73 (26.84) | 45 (16.54) | 196 (72.06) | 53 (19.49) |
| Tunisia | <5,000 | 745 (85.53) | 466 (62.55) | 588 (78.93) | 595 (79.87) | 277 (37.18) | 448 (60.13) | 720 (96.64) | 570 (76.51) | – |
| Venezuela | <5,000 | 567 (88.87) | 438 (77.25) | 443 (78.13) | 489 (86.24) | 416 (73.37) | 359 (63.32) | 369 (65.08) | 295 (52.03) | 184 (32.45) |
| Albania | 5,000/<10,000 | 206 (100.00) | 21 (10.19) | 22 (10.67) | 22 (10.68) | 22 (10.68) | 11 (5.34) | 27 (13.11) | 22 (10.68) | 10 (4.85) |
| Argentina | 5,000/<10,000 | 836 (58.79) | 434 (51.91) | 502 (60.05) | 472 (56.46) | 405 (48.44) | 399 (47.73) | 557 (66.63)* | 375 (44.86) | 239 (28.59)§ |
| Bosnia | 5,000/<10,000 | 213 (100.00) | 122 (57.28) | 79 (37.09) | 86 (40.38) | 84 (39.44) | 34 (15.96) | 128 (60.09) | 66 (30.99) | 34 (15.96) |
| Brazil | 5,000/<10,000 | 1270 (69.13) | 684 (53.86) | 1110 (87.14) | 1059 (83.39) | 1152 (90.71) | 462 (36.38) | 127 (100.00) | 1270 (100.00) | 696 (54.80) |
| Colombia | 5,000/<10,000 | 5030 (95.58) | 4137 (97.41) | 4064 (95.69) | 4064 (95.69) | 2929 (68.97) | 2329 (54.84) | 4123 (97.08) | 5030 (100.00) | 1535 (36.14) |
| Macedonia | 5,000/<10,000 | 22 (91.67) | 6 (27.27) | 2 (9.09) | 2 (9.09) | 2 (9.09) | – | 7 (31.82) | 5 (22.73) | 3 (13.64) |
| Montenegro | 5,000/<10,000 | 110 (100.00) | 47 (42.73) | 50 (45.45) | 49 (44.55) | 52(47.27) | 25 (22.73) | 36 (32.73) | 11 (10.00) | 6 (5.45) |
| Peru | 5,000/<10,000 | 1229 (69.87) | 1055 (59.97) | 1337 (76.00) | 1245 (70.77) | 1041 (59.18) | 1028 (58.44) | 1229 (100.00)* | 1229 (100.00) | 1218 (69.24)§ |
| Serbia | 5,000/<10,000 | 742 (50.82) | 553 (74.53) | 652 (87.87) | 665 (89.62) | 725 (97.71) | 363 (48.92) | 742 (100.00) | 284 (38.27) | 76 (10.24) |
| Chile | 10,000 / <20,000 | 1589 (68.88) | 921 (57.96) | 1241 (78.10) | 725 (45.63) | 1086 (68.34) | 573 (36.06) | 1455 (91.57) | 1291 (81.25) | 280 (17.62) |
| Chinab | 10,000 / <20,000 | 269 (14.64) | 128 (47.58) | 196 (72.86) | 214 (79.5) | 175 (65.06) | 88 (32.71) | 230 (85.50) | 230 (85.50) | 117 (43.49) |
| Cyprus | 20,000 / 35,000 | 170 (96.59) | 77 (45.29) | 66 (38.82) | 74 (43.53) | 59 (34.71) | 11 (6.47) | 74 (43.53) | 57 (33.53) | 37 (21.76) |
| Greece | 20,000 / 35,000 | 24 (100.00) | 19 (41.30) | 25 (54.35) | 19 (41.30) | 16 (34.78) | 3 (6.52) | 22 (47.83) | 14 (30.43) | 11 (23.91) |
| Italy | 20,000 / 35,000 | 7521 (90.79) | 4226 (56.19) | 3810 (50.66) | 7452 (99.08) | 5164 (68.66) | 808 (10.74) | 2552 (33.93) | 6562 (87.25) | 940 (12.50) |
| Lithuania | 10,000 / <20,000 | 71 (34.80) | – | 14 (19.72) | 19 (26.76) | 11 (15.49) | 1 (1.41) | 176 (86.70) | 100 (49.26) | 160 (78.82) |
| Malaysia | 10,000 / <20,000 | 2183 (75.17) | 483 (22.13) | 1342 (61.48) | 1383 (63.35) | 1110 (50.85) | 284 (13.01) | 548 (25.10) | 952 (43.61) | 1280 (58.63) |
| Romania | 10,000 / <20,000 | 1016 (96.67) | 51 (5.02) | 46 (4.53) | 44 (4.33) | 33 (3.25) | 21 (2.07) | 58 (5.71) | 45 (4.43) | 13 (1.28) |
| Russia | 10,000/<20,000 | 946 (93.57) | 118 (12.47) | 561 (59.30) | 620 (65.54) | 335 (35.41) | 116 (12.26) | 793 (83.83) | 312 (32.98) | 91 (9.62) |
| Saudi Arabia | 20,000 / 35,000 | 458 (53.44) | 237 (51.75) | 325 (70.96) | 337 (73.58) | 275 (60.04) | 105 (22.93) | 196 (42.79) | 369 (80.57) | 231 (50.44) |
| Spain | 20,000 / 35,000 | 918 (28.53) | 747 (81.37) | 808 (88.02) | 758 (82.57) | 376 (40.96) | 545 (59.37) | 870 (94.77) | 805 (87.69) | 231 (25.16) |
| Australia | >35,000 | 718 (88.10) | 506 (70.47) | 448 (62.40) | 631 (87.88) | 525 (73.12) | 152 (21.17) | 243 (33.84) | 191 (26.60) | 86 (11.98) |
| Belgium | >35,000 | 732 (93.61) | 596 (81.42) | 567 (77.46) | 573 (78.28) | 523 (71.45) | 116 (15.85) | 429 (58.61) | 570 (77.87) | 106 (14.48) |
| Germany | >35,000 | 2510 (70.86) | 2463 (98.13) | 2485 (99.00) | 2023 (80.60) | 2414 (96.18) | 2460 (98.01) | 175 (6.97) | 2319 (92.39) | 841 (33.51) |
| Netherlands | >35,000 | 360 (82.26) | 359 (99.72) | 263 (73.06) | __ | 277 (76.94) | 31 (8.61) | 353 (94.89) | 59 (16.39) | 27 (7.50) |
| Singapore | >35,000 | 315 (88.73) | 149 (47.30) | 141 (44.76) | 311 (98.73) | 275 (87.30) | 19 (6.05) | 145 (46.03)** | 177 (56.19) | 263 (83.49)** |
| Switzerland | >35,000 | 1243 (93.88) | 1085 (87.29) | 1083 (87.13) | 1171 (94.21) | 231 (18.58) | 13 (1.05) | 1154 (92.84) | 696 (55.99) | 57 (4.59) |
| UK | >35,000 | 4264 (91.96) | 2233 (52.37) | 2146 (50.33) | 2404 (56.38) | 1337 (31.36) | 1055 (24.74) | 1553 (36.42) | 262 (6.14) | 120 (2.81) |
| USAa | >35,000 | 462 (82.21) | 361 (78.14) | 387 (83.77) | 451 (97.62) | 155 (33.55) | 58 (12.55) | 84 (18.18) | 48 (10.39) | 106 (22.94) |
| p-value | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | <0.01 | |
aUSA/California; bChina/Hubei; cPakistan/Lahore; *safety glasses or visor; ⁎⁎Reserve for aerosol generating procedures; § Water-repellent gown or disposable sterile microfiber gown; ° Rotating instrument;
When COVID self-reported rate among dental professionals was used as the dependent variable for an ordinal multinomial regression model (Table 4 ), CPR and N95/FFP2 were statistically significantly associated (β = 1.07 and β = -1.46, respectively both p < 0.01). Also, GNI was statistically associated to the test-positive rate among dental professionals ( β = 0.72 p = 0.03). The face-to-face clinical activity and Private Practice Rate (PPr) (<25%) were not statistically associated to the dependent variable.
Table 4.
Ordinal multinomial regression analysis using dentists’ test-positive as dependent variable. For the multivariate analysis the forward stepwise method was used.
| Dentists positive rate | |||
|---|---|---|---|
| Variables | β | Standard Error | p-value |
| GNI (>$35,000 a year) | 0.72 | 0.43 | 0.03 |
| CPR (>10) | 1.07 | 0.24 | <0.01 |
| ffp2/N95 (<25 %) | -1.46 | 0.43 | <0.01 |
| Face-to face | 0.61 | 0.35 | 0.05 |
| PPr (<25%) | 0.32 | 0.21 | 0.59 |
GNI= Gross National Income per capita 2019; CPR=Country Positive Rate % to COVID-19;
ffp2= routine use of ffp2/N95 mask; Face-to-face= Face-to-face clinical activity;
PPr=Private Practice rate
4. Discussion
This is the first global population-based study, to the authors’ knowledge, that describes the effect of COVID-19 on the dental profession, describing self-reported COVID-19 infection and presumably related symptoms/signs suffered, exploring work attitudes and behaviour, and investigating the routine use of protective measures and PPE. The questionnaire used also included other aspects such as COVID-related risk awareness and perception; however, the focus of this project was centred on the dissemination of the infection among dental professionals and the implemented protection measures for dental professionals and patients. The survey included more than 50,000 participants across 36 countries. Findings showed that living in countries with high COVID-19 positive rates increased the probability that the dental professionals became infected, although these higher rates could be related to infection acquired within the community, as well as at work. In terms of protective measures, the use of N95/FFP2 masks significantly reduced the chances of the dental professionals reporting symptoms/signs related to the disease, while the other PPEs seem less relevant for SARS-CoV-2 protection. Overall, the probability of dental professionals becoming infected was associated to the Gross National Income (GNI) of the countries where they work.
The present study offers a global picture of the dental profession and COVID-19, even if the large number of respondents cannot be considered representative of the entire world population of dental professionals; nonetheless, these findings can provide a measurement framework and methods for countries and global stakeholders to better plan health service provision.
Although our study provided relevant information on the effect of COVID-19 on the dental profession, caution is necessary when interpreting the results due to some limitations. First of all, the obvious limitation could be choosing COVID self-reported positive rate as dependent variable as representative of the impact of the disease in the field. In most countries, testing was not available in the earlier stages of the pandemic. Moreover, any person who presented any of the symptoms related to COVID were asked to isolate. These people were, then, certainly impacted by the disease, even if they did not have an official positive testing. In this case, the number of professionals who had symptoms might be higher than the true prevalence of COVID. Also, there is need to highlight the possibility of false negative test results and the necessity to measure clinical sensitivity and specificity of each test according to real-life situations (symptoms, contacts etc) [23]. Further research would be needed to address other outcome data collected during this survey, such as tested “positive for COVID", and "hospitalized for COVID ". On the other hand, there is possibility that the lack of access to testing in low-income countries, may have led to an over-estimation of infection due to reliance on untested symptoms.
Secondly, the time periods for collection of the survey data and independent reports of dental professional infection rates do not coincide since survey was carried out from May to August 2020. The dental professionals reported infection rates from the beginning of the pandemic. However, this does not reduce the relevance of the results, since these data were only used to categorize countries and as a metric for comparing countries. In addition, these data provide useful information on how adequately countries were testing, also in relation to the size of the outbreak and thus facilitating the understanding of how widespread the virus was, in conjunction with confirmed case data [24]. According to World Health Organization (WHO) criteria, a positive testing rate of less than 5% is a reliable indicator that the epidemic is under control [24].
Although these data do not seem to support all the recommended enhanced protective measures, except for higher-rated masks, the results must be interpreted cautiously, nonetheless. The use of higher-rated masks, in itself, may be an indicator of higher levels of protection overall. This survey is based on self-reported information in a large sample of dental professionals from 36 countries. Importantly, the design of this research does not allow inferences to be drawn about cause and effect, therefore, conclusions must be carefully drawn. It is possible that at the individual level, the use of N95/FFP2 masks alone is not a sufficient protection against SARS-CoV-2 infection. It might be speculated that dental professionals wearing N95 masks at work are also more likely to wear them when they are in normal life settings, reducing the risk of community transmission. However, such appealing hypothesis cannot be verified from the present data.
The pandemic of COVID-19 has affected the entire world, with over 150 million cases and more than 3.2 million deaths by May 2021, worldwide [25], and an increasing infection and death rate in developing countries. The dental profession has not had universal guidelines on how to manage the virus, despite being perceived as having extremely high risk for exposure among all professions [2], [3], [4]. However, data from similar studies in Europe and USA showed that the prevalence and the positivity rates among dental professionals/dental hygienists was low, suggesting that current infection control recommendations against COVID-19 could be appropriate [8,9,25,26]. Similarly, our findings follow the same trend for most countries, where infectivity rate during the performance of the survey could be retrieved (Tables 2 and 3). This trend could be at least partially explained by the preventive measures frequently implemented by dental professionals all over the world, that protect the dentist whilst treating symptomatic patients, reducing the risk of infection [27,28].
High variability could be observed among countries, but in general, dental professionals from countries with higher GNI reported lower infection rates, potentially because they were less well protected in lower GNI countries; however, it could also be a reflection on testing protocols in high income countries which may have necessitated that healthcare workers be tested disproportionately more than the general population. In a recent survey among other health professions in the USA, the majority of responders reported to have access to PPEs [27,29], but the situation is different in countries with lower GNI, which may lead to higher infection rates. In eight of the surveyed countries, the dental professionals’ COVID self-reported rate was higher than that of the general population (Pakistan, Russia, Saudi Arabia, Tunisia, Netherlands, Lithuania, Malaysia and China).
When dental professionals continued practicing in countries with higher positive rates, our data showed that this also was associated with a higher COVID self-reported rate than those working in countries with lower rates (Table 4). The results also showed a trend for a higher rate of COVID self-reported infection among dental professionals working in public rather than private practice. It is reasonable to speculate that in hospitals and primary public care centres more people congregate at the same time, reducing time to ventilate rooms between patients, increasing the risk of virus transmission. It is also possible that, in such places, there are higher odds of COVID-19-positive people gathering, among patients, institutional staff and accompanying persons. It has been shown that other health professionals working in health centres are at a higher risk of acquiring the SARS-CoV-2 due to direct contact with positive patients, long working hours, lack of preparation or limited access to PPE [7,27,29]. This higher risk may be also true for community contacts when infection rates are high in the country.
Although droplets of contaminated secretions and direct contact were initially regarded as the main routes for SARS-CoV-2 infection [30], aerosol-generating procedures (AGPs) in contaminated environments is an indisputable route, in addition to exhalation, speaking, sneezing or coughing [3,4,31]. At the present time, nosocomial infection of SARS-CoV-2 through the airborne route has not been reported [32]. The ordinal multinomial logistic regression showed that only the use of N95/FFP2 masks significantly reduced the probability of reporting signs/symptoms of COVID-19. Information was not collected to explain, when N95/FFP2 masks were not used, the reason for this action; it is therefore impossible to know if N95/FFP2 masks were not available to dental professionals or if their non-use was due to cost or because they were not considered more effective than surgical masks. In other words, the use of high-quality masks appears to be the most effective measure to avoid infection by SARS-CoV-2. From the HIV/AIDS onset and the increased awareness of hepatitis B and C in the 1990’s, the dental profession adopted strict infection control measures. Indeed, the Center of Disease Control (CDC) released guidelines for infection control starting to the assumption that every patient in a dental office could be infected with HIV or Hepatitis B viruses [33]. These guidelines were later updated, based on new evidence, but the philosophy was not altered [34]. This may explain the low infection rate among dental professionals, despite the aerosol generation and the close proximity to potentially infected patients. Dental professionals have a “culture” of infection control. When transmission rates of the pandemic are in the respective region high, dental professionals should act following a similar behaviour as they did in those days for HIV, considering every patient as COVID‑19 positive. However, when transmission is low or the pandemic is alleviated, these measures will cause waste of resources, contradict sustainability, and add burdens to countries where resources are limited. Using higher levels of protection should be dependent on community transmission levels of COVID-19. The facilities and personnel must undergo an even stricter infection control protocol, reduce AGPs, space appointment times, establish correct ventilation and train dental and other associated health workers [35,36]. Thus, the extra recommendations raised after the COVID-19 outbreak were rapidly adopted for most dental professionals that continued treating patients, either restricting it to dental urgencies/emergencies or those having elective care [34,35]. Public health organizations rapidly released enhanced infection prevention and control recommendations with specific PPEs, based on the knowledge of SARS-CoV-2 at the time. Thus, dental AGPs must be performed wearing surgical masks, basic clinical PPE and eye protection. For those care providers with no access to high-standard N95/FFP2 masks and when performing AGPs, the guidelines strongly suggest using a high-level surgical mask along with a face shield over it simultaneously [35,37,38]. Handling of equipment is also important, as bacterial contamination of masks during manipulation has been recently reported in the AGP dental settings [38,39]. Changing the mask after treating a patient followed by hand disinfection has been recommended [40]. It is recommended that the current international and national guidelines are maintained until evidence dictates otherwise or when the pandemic is alleviated.
Authors Contributions
G Campus, contributed to conception, design, data acquisition, analysis, and interpretation, drafted and critically revised the manuscript; M D Betancourt contributed to design, data analysis, and interpretation and critically revised manuscript; M G Cagetti, T G Wolf, contributed to conception, design, interpretation, drafted and critically revised the manuscript; R A Giacaman D J. Manton, G V.A. Douglas, T Saads Carvalho, J C Carvalho, contributed to design, acquisition, analysis, and interpretation, drafted and critically revised the manuscript; A Vukovic, J F. Cortés-Martinicorena, R Sava-Rosianu, J Krithikadatta, contributed to design, acquisition and interpretation, critically revised the manuscript; D Bourgeois contributed to interpretation and critically revised the manuscript; N Sergeevna Morozova, AM Acevedo, A A Agudelo-Suarez, G Aguirre, K Aguirre, I Alfonso, H A Ghaffar, R A El Fadl, S A A AlMaghlouth, T Almerich-Torres, F Amadori, K Antia, E Bajric, D M Barbosa-Liz, S Ben-Tanfous, H Bieber, S Bhusari, S Birch, G Bontà, P Bottenberg, J J Bruers, L Bustillos, P Bührens, J Cai, F CA Carrer, M B Correa, B Cortés-Acha, F Carrouel, R de Carvalho Oliveira, F Crombie, J I Csikar, D Declerck, M Denkovski, J Deschner, J Dopico-San Martin, O Viktorovna Dudnik, W Y Escobar, A Elwishahy, C E Fernandez, M Fontana, A Frattaroli Pericchi, M Ghorbe, Gigineishvili E, A Garcia Quintana, J Gray, N Gugnani, K Gambetta-Tessini, A Haider, M Hopcraft, J Hüttmann, N Hysenaj, A Jalal, M Jikia, J John, G Kaps-Richter, T Kerber Tedesco, S Leon, K A Levin, H Pau Lew, M Aperecida Moreira Machado, A Beneictovna MacLennan, J Onome Mafeni, M Minatel Braga, J M Montiel-Company, A Malerba, S Mandić-Rajčević, A Askerovich Mamedo, S Ann Man, O Marouane, D Markovic, E Paredes Martinez, N Maroufidis, F Medeiros Mendes, S Musa, A Necibi, N Azlida Mohd Nor, B Tochukwu Ojukwu, N Opdam, L Ottolenghi, J Owen, A Pássaro, I F Persoon, T Peric, V Philippides, S P Plaza-Ruiz, D Procida Raggio, F J Rivas Cartagena, F Ramos-Gomez, M Sabashvili, G Solis Sanchez, H Schrader, S Serban, B Shi, C PC Sim, S Slabsinskiene, G Spagnuolo, O Olufemi Taiwo, A Thodhorjani, P Tietler, E Pesaressi Torres, C M C Volgenant, M H van der Veen, Z Vlahovic, A Visaria, Y Romero Uzcategui, E Xhajanka, Q Yan, O Zen, O Zeyer, A Zukanovic, contributed to acquisition and critically revised the manuscript; J L Cairoli, A Senna, contributed to conception, design, acquisition, critically revised the manuscript; F Cocco contributed to analysis and interpretation, drafted and critically revised the manuscript. All authors gave final approval and agreed to be accountable for all aspects of the work.
Appendix 1
G Campusa , b , c , ⁎, M Diaz Betancourta, MG Cagettid, RA Giacamane, DJ Mantonf, GVA Douglasg, TS Carvalhoa, JC Carvalhoh, A Vukovici, FJ Cortés-Martinicorenaj, D Bourgeoisk, V Machiulskienel, R Sava-Rosianum, J Krithikadattan, N Sergeevna Morozovac, AM Acevedoo, AA Agudelo-Suarezp, G Aguirreq, K Aguirreq, I Alfonsoo, HA Ghaffarr, RA El Fadlr, SA Al Maghlouths, T Almerich-Torrest, F Amadoriu, K Antiav, E Bajricw, DM Barbosa-Lizx, S Ben-Tanfousy, H Bieberz, S Bhusariaa, S Birchg, G Bontàd, P Bottenbergab, JJ Bruersac, L Bustillosad, P Bührensae, J Caiaf, JL Cairoliag, FCA Carrerah, MB Correaah, B Cortés-Achaai, F Carrouelk, R de Carvalho Oliveiraah, F Coccob, F Crombieaj, JI Csikarg, D Declerckak, M Denkovskial, J Deschneram, J Dopico-San Martinan, O Viktorovna Dudnikc, WY Escobarq, A Elwishahyao, CE Fernàndeze, M Fontanaap, A Frattaroli Pericchiaq, M Ghorbey, E. Gigineishviliar, A Garcia Quintanao, J Grayas, N Gugnaniat, K Gambetta-Tessinie, A Haideraw, M Hopcraftau, J Hüttmannae, N Hysenajav, A Jalalaw, M Jikiaax, J Johnaz, G Kaps-Richterae, T Kerber Tedescoah, S Leòne, KA Leving, H Pau Leway, M Aperecida Moreira Machadoah, A Beneictovna MacLennanc, J Onome Mafeniba, M Minatel Bragaah, JM Montiel-Companybb, A Malerbad, S Mandić-Rajčevićd , i, A Askerovich Mamedoc, S A Maniaz, O Marouaney, D Markovici, E Paredes Martinezbc, N Maroufidisbd, F Medeiros Mendesah, C F Mendezbw, S Musaaz, A Necibiy, N Azlida Mohd Noraz, B Tochukwu Ojukwuba, N Opdambe, L Ottolenghibf, J Owenbg, A Pássaroah, IF Persoonbh, T Perici, E Pesaressi-Torresbi, V Philippidesbj, SP Plaza-Ruizbk, D Procida Raggioah, FJ Rivas Cartagenaq, F Ramos-Gomezbl, M Sabashvilibm, G Solis Sanchezbn, R Villena Sarmientobn, H Schraderae, S Serbang, R Bairstowg, A Sennad, B Shiaf, CPC Simbo, E Slabsinskienebp, G Spagnuoloc , bq, A F Squassibx, O Olufemi Taiwoba, A Thodhorjanibr, P Tietlerae, CMC Volgenantbh, MH van der Veenbh, Z Vlahovicbs, A Visariabt, Y Romero Uzcateguiad, E Xhajankabu, Q Yanaf, O Zengaf, O Zeyerbv, A Zukanovici, TG Wolfa,am
a Department of Restorative, Preventive and Pediatric Dentistry, University of Bern, Bern, Switzerland
b Department of Surgery, Microsurgery and Medicine Sciences, School of Dentistry, University of Sassari, Sassari, Italy
c School of Dentistry Sechenov University, Moscow, Russia
d Department of Biomedical, Surgical and Dental Science, University of Milan, Milan, Italy
e Cariology and Gerodontology Units, Department of Oral Rehabilitation, Faculty of Health Sciences, University of Talca, Talca, Chile
f Cariology and Paediatric Dentistry, Centrum voor Tandheelkunde en Mondzorgkunde, University Medical Centre Groningen, Groningen, the Netherlands
g Department of Dental Public Health, School of Dentistry, University of Leeds, Leeds, UK
h Faculty of Medicine and Dentistry, UCLouvain, Louvain, Belgium
i Department of Pediatric and Preventive Dentistry School of Dental Medicine University of Belgrade, Belgrade, Serbia
j Pamplona; Ex-Facultad de Odontología, Universidad de Barcelona, Spain
k University Claude Bernard Lyon 1, Laboratory “Systemic Health Care,” University of Lyon, Lyon, France
l Clinic of Dental and Oral Pathology, Faculty of Odontology, Lithuanian University of Health Sciences, Kaunas, Lithuania
m Department of Preventive, Community Dentistry and Oral Health, Faculty of Dentistry, University of Medicine and Pharmacy “Victor Babes”, Timisoara, Romania
n Department of Conservative Dentistry & Endodontics, Saveetha Dental College and Hospitals, Chennai, India
o Universidad Central de Venezuela, Facultad de Odontología, Caracas, Venezuela
p Faculty of Dentistry, University of Antioquia, Colombia, Medellín, Antioquia
q Facultad de Odontologia, Universidad de El Salvador, El Salvador
r Faculty of Dentistry, Ain Shams University, Cairo, Egypt
s King Fahad Medical City, Riyadh, Saudi Arabia
t Facultad de Odontología, Universidad de Valencia, Spain
u Dental Clinic, School of Pediatric Dentistry, University of Brescia, Brescia, Italy
v School of Health Sciences, University of Georgia, Tbilisi, Georgia
w Department of Preventive and Pediatric Dentistry, Faculty of Dentistry with Clinics of Sarajevo University, Sarajevo, Bosnia Herzegovina
x Faculty of Dentistry, University of Antioquia, Colombia, Medellín, Antioquia
y Faculty of Dental Medicine of Monastir, Monastir, Tunisia
z Bundeswehr Medical Service Headquarters, Koblenz, Germany
aa Heidelberg Institute of Global Health (HIGH), Heidelberg, Germany
ab Oral Health Research Cluster, VUB, Bruxelles, Belgium
ac University of Amsterdam and Vrije Universiteit Amsterdam, Amsterdam, the Netherlands
ad Universidad de Los Andes, Facultad de Odontología, Merida, Venezuela
ae Freier Verband Deutscher Zahnärzte, Bonn, Germany
af The State Key Laboratory Breeding Base of Basic Science of Stomatology & Key Laboratory of Oral Biomedicine Ministry of Education, School & Hospital of Stomatology, Wuhan University, Wuhan, People's Republic of China
ag Department of Biotechnology and Life Sciences, University of Insubria, Varese, Italy
ah Universidade de Sao Paulo- School of Dentistry - Department of Community Dentistry, Sao Paulo, Brazil
ai Private Practitioner, Pamplona, Spain
aj Melbourne Dental School, Faculty of Medicine, Dentistry & Health Sciences, The University of Melbourne, Melbourne, Australia
ak Department of Oral Health Sciences, Population Studies in Oral Health, KULeuven, Belgium
al Private practioner, Kumanovo, North Macedonia
am Department of Periodontology and Operative Dentistry, University Medical Center of the Johannes Gutenberg University Mainz, Mainz, Germany
an Private Practitioner, Pamplona, Spain
ao Heidelberg Institute of Global Health at Heidelberg University Hospital, Heidelberg, Germany
ap University of Michigan School of Dentistry, Ann Arbor, USA
aq Universidad Central de Venezuela, Facultad de Odontología, Caracas, Venezuela
ar School of Health Sciences, University of Georgia, Tbilisi, Georgia
as King Fahad Medical City, Ryad, Saudi Arabia
at Department of Pediatric and Preventive Dentistry, Dental college, Haryana, India
au Melbourne Dental School, Faculty of Medicine, Dentistry& Health Sciences, The University of Melbourne, Melbourne, Australia; eviDent Foundation, Melbourne, Australia
av Department of Prosthodontic, Faculty of Dental Medicine, University of Medicine, Tirana, Albania
aw Department of Oral and Maxillofacial Surgery, Fatima Memorial Hospital, Lahore, Pakistan
ax School of Health Sciences, University of Georgia, Tbilisi, Georgia
ay Department of Restorative Dentistry National Dental Centre Singapore, Singapore
az Faculty of Dentistry, University of Malaya, Kuala Lumpur, Malaysia
ba Intercountry Center for Oral Health for Africa, Jos, Nigeria
bb School of Dentistry University of Valencia, Valencia, Spain
bc Facultad de Odontología - Universidad San Martin de Porres, Lima, Peru
bd Private Practioner, Athens, Greece
be School of Dentistry, Radboud University Medical Centre, Nijmegen, the Netherlands
bf Department of Dental and Maxillo-Facial Sciences, Sapienza Rome University, Rome, Italy
bg Department of Dental Public Health, School of Dentistry, University of Leeds, Leeds, UK
bh Department of Preventive Dentistry, Academic Centre for Dentistry Amsterdam, Amsterdam, the Netherlands
bi Facultad de Odontología - Universidad San Martin de Porres, Lima, Peru
bj President Cyprus Dental Association, Nicosia, Cyprus
bk Orthodontic Department, Fundación Universitaria CIEO-UniCIEO Bogotá, Colombia
bl UCLA Center for Children's Oral Health (UCCOH) UCLA School of Dentistry, Los Angeles, USA
bm School of Health Sciences, University of Georgia, Tbilisi, Georgia
bn Facultad de Odontología - Universidad San Martin de Porres, Lima, Peru
bo Department of Restorative Dentistry National Dental Centre Singapore, Singapore
bp Faculty of Odontology, Department of Pediatric and Preventive Dentistry, Lithuanian University of Health Sciences, Kaunas, Lithuania
bq Department of Neurosciences, Reproductive and Odontostomatological Sciences, University of Naples “Federico II”, Naples, Italy
br Department of Prosthodontic, Faculty of Dental Medicine, University of Medicine, Tirana, Albania
bs Medical Faculty of Pristina - Kosovska Mitrovica, Serbia
bt Centre for Ageing Research and Education, Duke-NUS Medical School, Singapore
bu Department of Prosthodontic, Faculty of Dental Medicine, University of Medicine, Tirana, Albania
bv Schweizerische Zahnärzte-Gesellschaft SSO, Bern, Switzerland
bw Instituto de Investigaciones Biomédicas INBIOMED, Universidad de Buenos Aires-CONICET, Buenos Aires, Argentina
bx Instituto de Investigaciones en Salud Pública (IISAP), Facultad de Odontología, Universidad de Buenos Aires, Buenos Aires, Argentina
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jdent.2021.103749.
Contributor Information
COVIDental Collaboration Group:
G Campus, M Diaz Betancourt, MG Cagetti, RA Giacaman, DJ Manton, GVA Douglas, TS Carvalho, JC Carvalho, A Vukovic, FJ Cortés-Martinicorena, D Bourgeois, V Machiulskiene, R Sava-Rosianu, J Krithikadatta, N Sergeevna Morozova, AM Acevedo, AA Agudelo-Suarez, G Aguirre, K Aguirre, I Alfonso, HA Ghaffar, RA El Fadl, SA Al Maghlouth, T Almerich-Torres, F Amadori, K Antia, E Bajric, DM Barbosa-Liz, S Ben-Tanfous, H Bieber, S Bhusari, S Birch, G Bontà, P Bottenberg, JJ Bruers, L Bustillos, P Bührens, J Cai, JL Cairoli, FCA Carrer, MB Correa, B Cortés-Acha, F Carrouel, R de Carvalho Oliveira, F Cocco, F Crombie, JI Csikar, D Declerck, M Denkovski, J Deschner, J Dopico-San Martin, O Viktorovna Dudnik, WY Escobar, A Elwishahy, CE Fernàndez, M Fontana, A Frattaroli Pericchi, M Ghorbe, E. Gigineishvili, A Garcia Quintana, J Gray, N Gugnani, K Gambetta-Tessini, A Haider, M Hopcraft, J Hüttmann, N Hysenaj, A Jalal, M Jikia, J John, G Kaps-Richter, T Kerber Tedesco, S Leòn, KA Levin, H Pau Lew, M Aperecida Moreira Machado, A Beneictovna MacLennan, J Onome Mafeni, M Minatel Braga, JM Montiel-Company, A Malerba, S Mandić-Rajčević, A Askerovich Mamedo, S A Mani, O Marouane, D Markovic, E Paredes Martinez, N Maroufidis, F Medeiros Mendes, C F Mendez, S Musa, A Necibi, N Azlida Mohd Nor, B Tochukwu Ojukwu, N Opdam, L Ottolenghi, J Owen, A Pássaro, IF Persoon, T Peric, E Pesaressi-Torres, V Philippides, SP Plaza-Ruiz, D Procida Raggio, FJ Rivas Cartagena, F Ramos-Gomez, M Sabashvili, G Solis Sanchez, R Villena Sarmiento, H Schrader, S Serban, R Bairstow, A Senna, B Shi, CPC Sim, E Slabsinskiene, G Spagnuolo, A F Squassi, O Olufemi Taiwo, A Thodhorjani, P Tietler, CMC Volgenant, MH van der Veen, Z Vlahovic, A Visaria, Y Romero Uzcategui, E Xhajanka, Q Yan, O Zeng, O Zeyer, A Zukanovic, and TG Wolf
Appendix. Supplementary materials
References
- 1.Peng X., Xu X., Li Y., Cheng L., Zhou X., Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int. J. Oral Sci. 2020;3(1):9. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Banakar M., Bagheri Lankarani K., Jafarpour D., Moayedi S., Banakar M.H., Mohammad Sadeghi A. COVID-19 transmission risk and protective protocols in dentistry: a systematic review. BMC Oral Health. 2020;20:275. doi: 10.1186/s12903-020-01270-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gallagher J.E., Sukriti K.C., Johnson I.G., Al-Yaseen W., Jones R., McGregor S., Robertson M., Harris R., Innes N., Wade W.G. A systematic review of contamination (aerosol, splatter and droplet generation) associated with oral surgery and its relevance to COVID-19. BDJ Open. 2020;6:25. doi: 10.1038/s41405-020-00053-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Innes N., Johnson I.G., Al-Yaseen W., Harris R., Jones R., Sukriti K.C., McGregor S., Robertson M., Wade W.G., Gallagher J.E. A systematic review of droplet and aerosol generation in dentistry. J Dent. 2021;105 doi: 10.1016/j.jdent.2020.103556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Michaels D., Wagner G.R. Occupational Safety and Health Administration (OSHA) and worker safety during the COVID-19 pandemic. JAMA. 2020;324:1389–1390. doi: 10.1001/jama.2020.16343. [DOI] [PubMed] [Google Scholar]
- 6.The New York Times, The Workers Who Face the Greatest Coronavirus Risk. https://www.nytimes.com/interactive/2020/03/15/business/economy/coronavirus-worker-risk.html?smid=em-share, 2020 (accessed 8 December 2020).
- 7.Pan Y., Liu H., Chu C., Li X., Liu S., Lu S. Transmission routes of SARS-CoV-2 and protective measures in dental clinics during the COVID-19 pandemic. Am. J. Dent. 2020;33:129–134. [PubMed] [Google Scholar]
- 8.Bontà G., Campus G., Cagetti M.G. COVID-19 pandemic and dental hygienists in Italy: a questionnaire survey. BMC Health Serv Res. 2020;20:994. doi: 10.1186/s12913-020-05842-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cagetti M.G., Cairoli J.L., Senna A., Campus G. COVID-19 Outbreak in North Italy: an overview on dentistry. a questionnaire survey. Int. J. Environ. Res. Public Health. 2020;17:3835. doi: 10.3390/ijerph17113835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Campus G., Diaz-Betancourt M., Cagetti M.G., Carvalho J.C., Carvalho T.S., Cortés-Martinicorena J.F., Deschner J., Douglas G.V.A., Giacaman R.S., Machiulskiene V., et al. Study protocol for an online questionnaire survey on symptoms/signs, protective measures, level of awareness and perception regarding COVID-19 outbreak among dentists. a global survey. Int. J. Environ. Res. Public Health. 2020;17:5598. doi: 10.3390/ijerph17155598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hodge Jr J.G., Wetter S., Carey E., Pendergrass E., Reeves C.M., Reinke H. Legal "Tug-of-Wars" During the COVID-19 Pandemic: Public Health vs. Economic Prosperity. J Law Med Ethics. 2020;48:603–607. doi: 10.1177/1073110520958888. [DOI] [PubMed] [Google Scholar]
- 12.https://github.com/datasets/covid-19. 2021 (accessed 18 May 2021).
- 13.https://datacatalog.worldbank.org/dataset/gni-capita-ranking-atlas-method-and-ppp-based. 2021 (accessed 18 May 2021).
- 14.Baj J., Karakuła-Juchnowicz H., Teresiński G., Buszewicz G., Ciesielka M., Sitarz E., Forma A., Karakuła K., Flieger W., Portincasa P., et al. COVID-19: specific and non-specific clinical manifestations and symptoms: the current state of knowledge. J Clin Med. 2020;9:1753. doi: 10.3390/jcm9061753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Symptoms of COVID-19 https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html, 2021(accessed 18 May 2021).
- 16.Belser J.A., Rota P.A., Tumpey T.M. Ocular tropism of respiratory viruses. Microbiol. Mol. Biol. Rev. 2013;77:144–156. doi: 10.1128/MMBR.00058-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gandhi M., Yokoe D.S., Havlir D.V. Asymptomatic transmission, the Achilles' Heel of current strategies to control Covid-19. N. Engl. J. Med. 2020;382:2158–2160. doi: 10.1056/NEJMe2009758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lai C.C., Shih T.P., Ko W.C., Tang H.J., Hsueh P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int. J. Antimicrob. Agents. 2020;55 doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lake M.A. What we know so far: COVID-19 current clinical knowledge and research. Clin. Med. 2020;20:124–127. doi: 10.7861/clinmed.2019-coron. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holliday R., Allison J.R., Currie C.C., Edwards D.C., Bowes C., Pickering K., Reay S., Durham J., Lumb J., Rostami N., Coulter J., Nile C., Jakubovics N. Evaluating contaminated dental aerosol and splatter in an open plan clinic environment: Implications for the COVID-19 pandemic. J. Dent. 2021;105 doi: 10.1016/j.jdent.2020.103565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sterne J.A., White I.R., Carlin J.B., Spratt M., Royston P., Kenward M.G., Wood A.M., Carpenter J.R. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338:b2393. doi: 10.1136/bmj.b2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jakobsen J.C., Gluud C., Wetterslev J., Winkel P. When and how should multiple imputation be used for handling missing data in randomised clinical trials - a practical guide with flowcharts. BMC Med. Res. Methodol. 2017;17:162. doi: 10.1186/s12874-017-0442-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Woloshin S., Patel N., Kesselheim A.S. False Negative Tests for SARS-CoV-2 Infection — Challenges and Implications. N. Engl. J. Med. 2020;383:e38. doi: 10.1056/NEJMp2015897. [DOI] [PubMed] [Google Scholar]
- 24.Middelburg R.A., Rosendaal F.R. COVID-19: How to make between-country comparisons. Int. J. Infect. Dis. 2020;96:477–481. doi: 10.1016/j.ijid.2020.05.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johns Hopkins University – Coronavirus Resource Center. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). https://coronavirus.jhu.edu/map.html, 2021 (accessed 12 May 2021).
- 26.Estrich C.G., Mikkelsen M., Morrissey R., Geisinger M.L., Ioannidou E., Vujicic M., Araujo M.W.B. Estimating COVID-19 prevalence and infection control practices among US dentists. J. Am. Dent. Assoc. 2020;151:815–824. doi: 10.1016/j.adaj.2020.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yanes-Lane M., Winters N., Fregonese F., Bastos M., Perlman-Arrow S., Campbell J.R., Menzies D. Proportion of asymptomatic infection among COVID-19 positive persons and their transmission potential: a systematic review and meta-analysis. PLoS One. 2020;15 doi: 10.1371/journal.pone.0241536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carrouel F., Gonçalves L.S., Conte M.P., Campus G., Fisher J., Fraticelli L., Gadea-Deschamps E., Ottolenghi L., Bourgeois D. Antiviral activity of reagents in mouth rinses against SARS-CoV-2. J Dent Res. 2021;100:124–132. doi: 10.1177/0022034520967933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Calò F., Russo A., Camaioni C., De Pascalis S., Coppola N. Burden, risk assessment, surveillance and management of SARS-CoV-2 infection in health workers: a scoping review. Infect. Dis. Poverty. 2020;9:139. doi: 10.1186/s40249-020-00756-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Coto J., Restrepo A., Cejas I., Prentiss S. The impact of COVID-19 on allied health professions. PLoS One. 2020;15 doi: 10.1371/journal.pone.0241328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Greenhalgh T., Jimenez J.L., Prather K.A., Tufekci Z., Fisman D., Schooley R. Ten scientific reasons in support of airborne transmission of SARS-CoV-2. Lancet. 2021;397:1603–1605. doi: 10.1016/S0140-6736(21)00869-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.World Health Organization: Prevention, identification and management of health worker infection in the context of COVID-19, https://www.who.int/publications/i/item/10665-336265, 2020 (accessed 28 June 2021).
- 33.Wong S.C.Y., Kwong R.T., Wu T.C., Chan J.W.M., Chu M.Y., Lee S.Y., Wong H.Y., Lung D.C. Risk of nosocomial transmission of coronavirus disease 2019: an experience in a general ward setting in Hong Kong. J Hosp Infect. 2020;105:119–127. doi: 10.1016/j.jhin.2020.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention. Summary of infection prevention practices in dental settings: Basic expectations for safe care. https://www.cdc.gov/oralhealth/infectioncontrol/summary-infection-prevention-practices/index.html, 2020 (accessed 28th June 2021).
- 35.Centers for Disease Control and Prevention. Interim infection prevention and control recommendations for healthcare personnel during the Coronavirus Disease 2019 (COVID-19) Pandemic. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html, 2021 (accessed 28th June 2021).
- 36.World Health Organization: Roadmap to improve and ensure good indoor ventilation in the context of COVID-19, https://www.who.int/publications/i/item/9789240021280, 2021 (accessed 28th June 2021).
- 37.Al Kawas S., Al-Rawi N., Talaat W., Hamdoon Z., Salman B., Al Bayatti S., Jerjes W., Samsudin A.B.R. Post COVID-19 lockdown: measures and practices for dental institutes. BMC Oral Health. 2020;20:291. doi: 10.1186/s12903-020-01281-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.World Health Organization: Mask use in the context of COVID-19, https://www.who.int/publications/i/item/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak, 2020 (accessed 28th June 2021).
- 39.European Centre for Disease Prevention and Control. Infection prevention and control and preparedness for COVID-19 in healthcare settings – Fifth update. https://www.ecdc.europa.eu/en/publications-data/infection-prevention-and-control-and-preparedness-covid-19-healthcare-settings. 2020 (accessed 28th June 2021).
- 40.Gund M., Isack J., Hannig M., Thieme-Ruffing S., Gärtner B., Boros G., Rupf S. Contamination of surgical mask during aerosol-producing dental treatments. Clin Oral Investig. 2020;7:1–8. doi: 10.1007/s00784-020-03645-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.