Abstract
Background
The COVID-19 pandemic has spread widely among healthcare workers. Recently, new effective vaccines against COVID-19 have begun to be administered to healthcare workers in several countries, including Italy.
Purpose
Our aim was to evaluate the intentions to be vaccinated against COVID-19 in a population of nursing students, identifying factors associated with the intentions.
Method
We conducted an anonymous online survey among 728 nursing students. The questionnaire collected data on demographic and academic characteristics, health status, vaccine attitudes, and specific reasons regarding the intention to get or not get the COVID-19 vaccination.
Results
A total of 422 nursing students completed the survey. Almost 81% of participants wanted to take the vaccine against coronavirus. The intention to adhere to the vaccination program was associated with male gender, a previous flu vaccine uptake, and high school education. The main reason in favor of taking the vaccine was to protect family and friends. The main reason for opposition was the fear of adverse events.
Conclusion
It is fundamental to consider vaccine hesitancy in healthcare students and face it properly, since these are the healthcare workers of the future who will have to provide recommendations to patients and promote adherence to vaccination programs.
Keywords: COVID-19, Coronavirus, Healthcare student, Nursing student, Vaccine, Vaccine hesitancy
Introduction
The coronavirus disease-19 (COVID-19) pandemic has spread widely among healthcare workers (HCWs) (M. Belingheri, Paladino, & Riva, 2020; Michael Belingheri, Paladino, & Riva, 2020; Nguyen et al., 2020). In Italy, in 2020, 28,000 nurses became infected with SARS-CoV-2 and 60 died, including five nurses who committed suicide (Italian Workers Compensation Authority [INAIL], 2020). HCWs are victims of the disease, but they are also potential spreaders to patients and colleagues as well as relatives and cohabitants (M. Belingheri, Paladino, & Riva, 2020; Nguyen et al., 2020). Recently, new effective vaccines against COVID-19 have begun to be administered to HCWs in the final weeks of December 2020 in the United Kingdom, the United States, and Europe (Dooling et al., 2020). Previous studies have investigated intentions to be vaccinated against COVID-19 among HCWs, but these were conducted in a period when vaccines had not yet been developed and the mechanisms of action were not yet known (Gagneux-Brunon et al., 2020; Kwok et al., 2021; Wang et al., 2020).
These prior studies did not include healthcare students, which is also a category directly affected by the epidemic. Some healthcare students became infected during hospital internships, but the greatest damage they suffered was during their training. In many hospitals, internships have had to be suspended, thus preventing students from reaching their educational goals. Furthermore, as with other university students, they were unable to attend classrooms, limiting their access to lessons, practical exercises, and seminars (Carolan et al., 2020). In recent months, a debate has opened up on the opportunity for medical and nursing students to attend internships even during the COVID-19 emergency, which has led to conflicting opinions (Miller et al., 2020; Riva et al., 2020). For this reason, it is important to encourage student vaccination for their rapid return to hospitals and classrooms. Nevertheless, healthcare students are not considered priority categories for COVID-19 vaccination in all countries, probably due to their young age and the lower risk of complications if infected. The reality, however, is that infection by SARS-CoV-2 and its repercussions—quarantine, self-isolation, distancing from relatives and friends, social stigma—may lead to significant psychological problems in a population that is already at greater risk (Belingheri et al., 2019; Belingheri, Pellegrini, et al., 2020; Cavasin et al., 2020; Savitsky et al., 2020; Shaw, 2020).
In order for the global vaccination campaign to be effective, any reasons for hesitation about vaccination must be addressed as soon as possible, especially in a young population such as healthcare students. However, those reasons are unknown in the nursing student population; moreover, factors associated with hesitation are also unknown. Having this information could help educators identify students at risk of hesitation and to develop effective interventions to promote adherence to vaccination protocols. In light of these gaps in knowledge, our aim was to evaluate the intentions to be vaccinated against COVID-19 in a population of nursing students, identifying factors associated with those intentions. We focused on a population of nursing students living in Lombardy, an Italian region dramatically hit by the disease in the first wave of the epidemic in March and April 2020.
Methods
Design
This is a descriptive correlational study designed to evaluate the intentions to be vaccinated against COVID-19 in a population of nursing students. Data was originally collected to provide information to the public health authority about the demand of vaccines among healthcare students; therefore, the data used in this study were related to a public health surveillance activity, which does not require IRB.
Sample and setting
We conducted an online survey from 21 to 27 December 2020 among 728 nursing students enrolled at the University of Milano-Bicocca. There were no exclusion criteria since we included all nursing students enrolled at the University. The survey was introduced to the students in an e-mail that described how participation was voluntary and completely anonymous since no personal data were collected. In this way, we also avoided the appearance of coercion for students to participate and allayed the students' fear of retaliation if they did not participate.
Instruments and data collection procedure
The questionnaire was completed electronically and was composed of: (a) a first part on demographic and academic characteristics (age, gender, education, year of the course, working student status, habitual district); (b) a second part on health information (smoking, general health status, previous diagnosis of COVID-19, diagnosis of COVID-19 among family members or friends); (c) a third part on vaccine attitudes (previous flu vaccines uptake, intention to get the COVID-19 vaccine); (d) a fourth part on specific reasons regarding the intention to get or not get the COVID-19 vaccine. All questions were closed-ended questions requiring a single answer in the first, second, and third sections of the questionnaire. The fourth part regarding reasons included closed-ended questions and multiple answer. When participants selected “other reason,” they were able to provide an open-ended answer.
During the early stages of the pandemic, Lombardy was the most affected region in Italy, but some areas in the region were more affected than others. To assess if the different impact of the pandemic within the region might have influenced opinions about vaccination, we determined the number of COVID-19 cases per 1000 inhabitants for each district as an indicator of the burden of disease. Data about COVID-19 cases and inhabitants by district was collected from the Italian Civil Protection Department and the Italian National Institute of Statistics, respectively (Dipartimento della Protezione Civile, 2020; Istituto Nazionale di Statistica (ISTAT), 2020). Data were updated to 21 December 2020.
Data analysis
Data were analyzed using SAS (SAS Institute, Cary, NC, USA) statistical software. Categorical variables were reported as absolute and relative frequencies. The continuous variable (age) did not follow normal distribution, and it was reported as median and interquartile range (IQR). A chi-square test was used to examine differences among districts, and results with p-value > 0.05 were considered not to be statistically significant. Logistic regression was used in both univariable and multivariable models to test association between the potential adherence to the COVID-19 vaccination program and variables collected (demographic and academic characteristics, health information, and previous flu vaccine uptake). The variables included in the multivariable model were gender, education, and flu vaccination. Odds ratio (OR) and 95% confidence interval (CI) were reported.
Results
A total of 422 nursing students completed the questionnaire (422/728, response rate 58%). The main characteristics of the study population are shown in Table 1 . The median age was 21 years old (IQR 20–22) and 82.9% of participants were female. Most students attended a high school (61.4%), followed by vocational or technical school (33.4%). Twenty-two students (5.2%) had already graduated in other programs before starting the nursing education program. Participants were from all years of the nursing course: 41.5% were attending the first year, 28.9% the second year, and 29.6% the third and last year. The status of “working student” was reported by 19.4% of participants. The prevalence of smokers was 30.8%, and 67.8% of students declared themselves to be in a very good/excellent health. Moreover, 28.2% of participants declared to be in a good state of health, while 4.0% declared to be in a poor/fair state of health. Focusing on COVID-19, 23.0% of respondents were diagnosed with coronavirus disease, and 67.3% had at least one family member or a friend with COVID-19.
Table 1.
Characteristics of the study population (n = 422).
| Variables | N | % |
|---|---|---|
| Age | ||
| Median (IQR) | 21 (20−22) | |
| Gender | ||
| Male | 72 | 17.1 |
| Female | 350 | 82.9 |
| Education | ||
| Vocational/technical school | 141 | 33.4 |
| High school | 259 | 61.4 |
| University | 22 | 5.2 |
| Course year | ||
| First year | 175 | 41.5 |
| Second year | 122 | 28.9 |
| Third year | 125 | 29.6 |
| Working student | ||
| No | 340 | 80.6 |
| Yes | 82 | 19.4 |
| District | ||
| Bergamo | 114 | 27.0 |
| Como | 17 | 4.0 |
| Lecco | 63 | 14.9 |
| Milan | 62 | 14.7 |
| Monza Brianza | 107 | 25.4 |
| Sondrio | 42 | 10.0 |
| Other districts | 17 | 4.0 |
| Smoker | ||
| No | 292 | 69.2 |
| Yes | 130 | 30.8 |
| State of health | ||
| Poor/fair | 17 | 4.0 |
| Good | 119 | 28.2 |
| Very good/excellent | 286 | 67.8 |
| Flu vaccination | ||
| No | 240 | 56.9 |
| Yes | 182 | 43.1 |
| COVID-19 diagnosis (personal) | ||
| No | 325 | 77.0 |
| Yes | 97 | 23.0 |
| COVID-19 diagnosis (family/friends) | ||
| No | 138 | 32.7 |
| Yes | 284 | 67.3 |
| Potential COVID-19 vaccine | ||
| No | 18 | 4.2 |
| Probably no | 63 | 14.9 |
| Probably yes | 142 | 33.7 |
| Yes | 199 | 47.2 |
Table 1 also reports the intention to adhere to the COVID-19 vaccination program among nursing students. Out of the participants, 81% declared their intention to be vaccinated against coronavirus. Specifically, 47.2% answered “Yes” and 33.7% answered “Probably yes.” On the other end of the scale, 4.2% and 14.9% of students answered “No” and “Probably no,” respectively.
Considering that some parts of the region were more affected by the pandemic than others, we investigated the relationship between districts and opinions about vaccination. Table 2 reports the potential adherence to the vaccine and the number of COVID-19 cases per 1000 inhabitants by district. We did not find any associations; no significant difference was detected among districts.
Table 2.
Potential adherence to the COVID-19 vaccine and cases per 1000 inhabitants by district (n = 422).
| District | Potential COVID-19 vaccine⁎ |
COVID-19 cases per 1000 inhabitants | |||
|---|---|---|---|---|---|
| Yes |
No |
||||
| N | % | N | % | ||
| Bergamo | 89 | 78.1 | 25 | 21.9 | 24.7 |
| Como | 15 | 88.2 | 2 | 11.8 | 53.8 |
| Lecco | 56 | 88.9 | 7 | 11.1 | 37.7 |
| Milan | 51 | 82.3 | 11 | 17.7 | 51.3 |
| Monza Brianza | 83 | 77.6 | 24 | 22.4 | 53.7 |
| Sondrio | 31 | 73.8 | 11 | 26.2 | 44.5 |
| Other district | 16 | 94.1 | 1 | 5.9 | NA |
p-Value > 0.05.
Table 3 reports the association between demographic and academic characteristics, health information, and previous flu vaccine uptake and the potential adherence to the COVID-19 vaccination program. In univariate analysis, the intention to adhere to the COVID-19 vaccination program was associated with male gender (OR 2.49, CI 1.10–5.66) and a previous adhesion to at least one flu vaccination campaign (OR 2.56, CI 1.49–4.39). Furthermore, having already attended a high school was associated with the intention to uptake the vaccine (OR 1.64, CI 1.01–2.73). In other words, male students, students who have previously received a flu vaccine, and students who have attended a high school were more determined to comply with the COVID-19 vaccination program.
Table 3.
Univariate logistic regression results showing the odds ratios for the association between potential adherence to the COVID-19 vaccination program and variables collected (demographic and academic characteristics, health information, and previous flu vaccine uptake). The multivariate model includes gender, education, and flu vaccination.
| Variables | Univariate model |
Multivariate model* |
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |||
| Age | ||||||
| 1.0 | 0.94 | 1.06 | ||||
| Gender | ||||||
| Female | Ref | – | – | Ref | – | – |
| Male | 2.49 | 1.10 | 5.66 | 2.71 | 1.17 | 6.29 |
| Education | ||||||
| Vocational/technical school | Ref | – | – | Ref | – | – |
| High school | 1.64 | 1.01 | 2.73 | 1.84 | 1.09 | 3.12 |
| University | 1.08 | 0.37 | 3.15 | 1.18 | 0.40 | 3.52 |
| Course year | ||||||
| First year | Ref | – | – | |||
| Second year | 1.47 | 0.82 | 2.64 | |||
| Third year | 1.71 | 0.94 | 3.11 | |||
| Working student | ||||||
| No | Ref | – | – | |||
| Yes | 0.57 | 0.33 | 1.01 | |||
| District | ||||||
| Other district | Ref | – | – | |||
| Bergamo | 0.22 | 0.03 | 1.76 | |||
| Como | 0.47 | 0.04 | 5.72 | |||
| Lecco | 0.50 | 0.06 | 4.37 | |||
| Milan | 0.29 | 0.04 | 2.42 | |||
| Monza Brianza | 0.22 | 0.03 | 1.71 | |||
| Sondrio | 0.18 | 0.02 | 1.49 | |||
| Smoker | ||||||
| No | Ref | – | – | |||
| Yes | 1.0 | 0.59 | 1.68 | |||
| State of health | ||||||
| Poor/fair | Ref | – | – | |||
| Good | 2.70 | 0.90 | 8.15 | |||
| Very good/excellent | 2.29 | 0.81 | 6.46 | |||
| Flu vaccination | ||||||
| No | Ref | – | – | Ref | – | – |
| Yes | 2.56 | 1.49 | 4.39 | 2.51 | 1.45 | 4.33 |
| COVID-19 diagnosis (personal) | ||||||
| No | Ref | – | – | |||
| Yes | 0.89 | 0.51 | 1.57 | |||
| COVID-19 diagnosis (family/friends) | ||||||
| No | Ref | – | – | |||
| Yes | 1.19 | 0.71 | 1.97 | |||
All these associations were statistically significant and were confirmed in the multivariate model, as reported in Table 3. We did not find associations between opinions about the novel vaccine and age, year of the program, district, smoking habit, state of health, and previous COVID-19 diagnosis (including family members or friends).
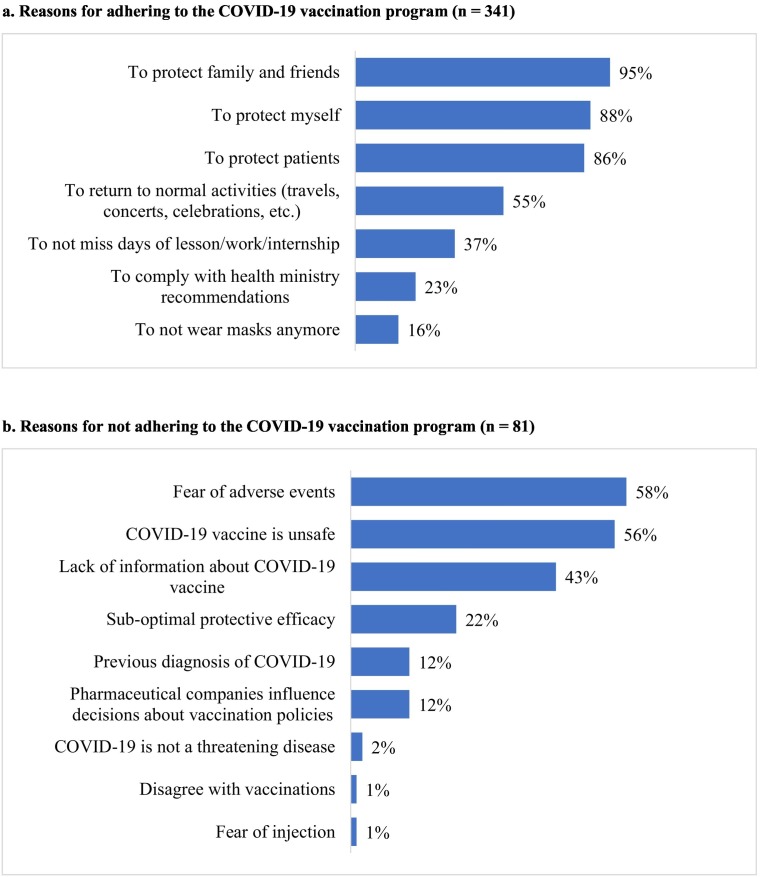
We also assessed the reasons related to the decision about the novel vaccine, and the data are shown in Fig. 1a and b. Among 341 students who were favorable to the vaccination, the main reasons were to protect family and friends (95%), protect oneself (88%), and protect patients during internship (86%). In the same group, 55% of students agreed to the vaccination as a condition of returning to normal activities (such as travels, concerts, and celebrations), 37% so as not to miss days of lessons, work, or internship, and 23% to comply with health ministry recommendations. Finally, 16% of students reported wanting to be vaccinated to avoid wearing masks (Fig. 1a).
Fig. 1.
a. Reasons for adhering to the COVID-19 vaccination program (n = 341).
b. Reasons for not adhering to the COVID-19 vaccination program (n = 81).
On the contrary, the main reasons related to opposition to the COVID-19 vaccine were the fear of adverse events (58%), the opinion that the vaccine is unsafe (56%), and the lack of information (43%). Among people who did not want to be vaccinated, about 22% believed that the vaccine has a sub-optimal protective efficacy, 12% had a previous diagnosis of COVID-19, and 12% stated that pharmaceutical companies influence decisions about vaccination policies. A small number of participants provided other reasons: the opinion that COVID-19 is not a threatening disease (2%), disagreement with vaccinations in general (1%), and fear of injection (1%) (Fig. 1b).
Discussion
Our study aimed at evaluating the intentions to be vaccinated against COVID-19 in a population of nursing students and identifying the associated factors. Previous studies on these topics were conducted when vaccines were not yet available and their mechanisms of action were still not known. Furthermore, a lack of information on nursing students as a specific population was found. Instead, at the time of our study, COVID-19 vaccines were already available, and in several countries, including Italy, the coronavirus vaccination campaign had already started. We reported a high percentage of nursing students favorable to the vaccination (81%). This rate of COVID-19 vaccine acceptance is similar to the percentage reported in an Italian survey among university students, including healthcare students (Barello et al., 2020). However, a recent survey of the general Italian population conducted in September reported that only 1 out of 2 Italian people wanted to be vaccinated (La Vecchia et al., 2020).
We found that the intention to be vaccinated was associated with a previous flu vaccine uptake. This is not a surprise, since attitudes towards COVID-19 vaccines are influenced by attitudes towards vaccines in general (Gagneux-Brunon et al., 2020). Furthermore, it is important to note that a previous diagnosis of COVID-19 or a diagnosis among family members and friends, as well as living in a district with a higher number of COVID-19 cases, were not associated with the inclination to be vaccinated. As a result, a direct exposure to COVID-19 did not influence student opinion and it is in accordance with the literature (Lucia et al., 2020). Healthcare students have mostly positive attitudes towards vaccines, due to their education in healthcare and regardless of their personal history with the disease.
Vaccine hesitancy was reported in 1 out of 5 students. The main reasons given were the lack of information about new vaccines, potential adverse events, and vaccination safety in general. These reasons are typical arguments associated with vaccine hesitancy (Giambi et al., 2018; Lane et al., 2018; Lucia et al., 2020). As the COVID-19 vaccination campaign was beginning, the debate emerged about whether to make vaccination mandatory for some professional categories, such as healthcare workers—or even for the general population. From 1 April 2021 in Italy, anti-SARS-CoV-vaccination became mandatory for HCWs. We recognize this is a complex and sensitive issue, and despite the mandatory vaccination, in our opinion, it is desirable to provide information through educational initiatives about vaccines, to deal with misinformation and “fake news,” and to raise awareness about the vital importance of widespread vaccination (Jarrett et al., 2015). The focal point for a successful vaccination campaign should be to reduce vaccine hesitancy and thereby achieve high vaccination coverage. Indeed, the only way for a rapid return to “normal activities,” which includes both hospital internships and lessons in classrooms, is to encourage the vaccination of students as well as the general population.
Limitations
The main limit of this study is that all participants were selected from the same university, within several locations, all located in the most affected Italian region. Our findings may not be representative of the other healthcare students in Italy. Furthermore, the respondent rate was suboptimal, and the risk of distortion should be taken into account. Despite these limitations, our study is the first to investigate attitudes and opinions about COVID-19 vaccines among Italian nursing students, as well as among Italian healthcare students in general, during a period when vaccines are actually available.
Conclusion
In conclusion, it is fundamental to consider vaccine hesitancy in healthcare students and to address it comprehensively, since these are the healthcare workers of the future who will have to provide recommendations to patients and promote adherence to vaccination programs. Furthermore, our study investigated the reasons related to non-adherence to the COVID-19 vaccination program; this knowledge is also important for nursing educators to be able to implement strategies that properly address vaccine hesitancy for COVID-19 during the nursing education program at the university.
Source of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
None.
References
- Barello S., Nania T., Dellafiore F., Graffigna G., Caruso R. “Vaccine hesitancy” among university students in Italy during the COVID-19 pandemic. European Journal of Epidemiology. 2020;35:781–783. doi: 10.1007/s10654-020-00670-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belingheri M., Facchetti R., Scordo F., Butturini F., Turato M., De Vito G.…Riva M.A. Risk behaviors among Italian healthcare students: A cross-sectional study for health promotion of future healthcare workers. La Medicina del Lavoro. 2019;110:155–162. doi: 10.23749/mdl.v110i2.7573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belingheri M., Paladino M.E., Riva M.A. Beyond the assistance: Additional exposure situations to COVID-19 for healthcare workers. The Journal of Hospital Infection. 2020;105:353. doi: 10.1016/j.jhin.2020.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belingheri M., Pellegrini A., Facchetti R., De Vito G., Cesana G., Riva M.A. Self-reported prevalence of sleep disorders among medical and nursing students. Occupational Medicine (London) 2020;70:127–130. doi: 10.1093/occmed/kqaa011. [DOI] [PubMed] [Google Scholar]
- Belingheri M., Paladino M.E., Riva M.A. Risk exposure to coronavirus disease 2019 in pregnant healthcare workers. Journal of Occupational and Environmental Medicine. 2020;62 doi: 10.1097/JOM.0000000000001881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carolan C., Davies C.L., Crookes P., McGhee S., Roxburgh M. COVID 19: Disruptive impacts and transformative opportunities in undergraduate nurse education. Nurse Education in Practice. 2020;46 doi: 10.1016/j.nepr.2020.102807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavasin D., Paladino M.E., Riva M.A., Persico G., Belingheri M. Prolonged PCR positivity stigma and return-to-work after SARS-CoV-2 infection. Journal of Occupational and Environmental Medicine. 2020 doi: 10.1097/JOM.0000000000002111. Publish Ah. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dipartimento della Protezione Civile Emergenza Coronavirus. 2020. http://www.protezionecivile.gov.it/attivita-rischi/rischio-sanitario/emergenze/coronavirus [WWW document]. URL. Last accessed on December 2020.
- Dooling K., McClung N., Chamberland M., Marin M., Wallace M., Bell B.P.…Oliver S.E. The advisory committee on immunization practices’ interim recommendation for allocating initial supplies of COVID-19 vaccine — United States, 2020. MMWR. Morbidity and Mortality Weekly Report. 2020;69:1782–1786. doi: 10.15585/mmwr.mm6949e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gagneux-Brunon A., Detoc M., Bruel S., Tardy B., Rozaire O., Frappe P., Botelho-Nevers E. Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: A cross sectional survey. The Journal of Hospital Infection. 2020 doi: 10.1016/j.jhin.2020.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giambi C., Fabiani M., D’Ancona F., Ferrara L., Fiacchini D., Gallo T.…Rota M.C. Parental vaccine hesitancy in Italy – Results from a national survey. Vaccine. 2018;36:779–787. doi: 10.1016/j.vaccine.2017.12.074. [DOI] [PubMed] [Google Scholar]
- Istituto Nazionale di Statistica (ISTAT) Popolazione residente. 2020. http://dati.istat.it/Index.aspx?QueryId=18460 [WWW Document]. URL. Last accessed on December 2020.
- Italian Workers Compensation Authority (INAIL) 2020. https://www.inail.it/ [WWW Document]. URL. Last accessed on December 2020.
- Jarrett C., Wilson R., O'Leary M., Eckersberger E., Larson H.J., Eskola J., Liang X., Chaudhuri M., Dube E., Gellin B., Goldstein S., Larson H., MacDonald N., Manzo M.L., Reingold A., Tshering K., Zhou Y., Duclos P., Guirguis S.…Schuster M. Strategies for addressing vaccine hesitancy - A systematic review. Vaccine. 2015;33:4180–4190. doi: 10.1016/j.vaccine.2015.04.040. [DOI] [PubMed] [Google Scholar]
- Kwok K.O., Li K.K., W.I W.E.I., Tang A., Wong S.Y.S., Lee S.S. Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. International Journal of Nursing Studies. 2021;114 doi: 10.1016/j.ijnurstu.2020.103854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Vecchia C., Negri E., Alicandro G., Scarpino V. Attitudes towards influenza vaccine and a potential COVID-19 vaccine in Italy and differences across occupational groups, September 2020. La Medicina del Lavoro. 2020;17;111:445–448. doi: 10.23749/mdl.v111i6.10813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane S., MacDonald N.E., Marti M., Dumolard L. Vaccine hesitancy around the globe: Analysis of three years of WHO/UNICEF Joint Reporting Form data-2015–2017. Vaccine. 2018;36:3861–3867. doi: 10.1016/j.vaccine.2018.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucia V.C., Kelekar A., Afonso N.M. COVID-19 vaccine hesitancy among medical students. Journal of Public Health (Bangkok) 2020 doi: 10.1093/pubmed/fdaa230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller D.G., Pierson L., Doernberg S. The role of medical students during the COVID-19 pandemic. Annals of Internal Medicine. 2020;173:145–146. doi: 10.7326/M20-1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen L., Drew D.A., Joshi A., Guo C.-G., Ma W., Mehta R.…Chan A. vol. 5. medRxiv Prepr. Serv. Heal. Sci.; 2020. Risk of COVID-19 among frontline healthcare workers and the general community: A prospective cohort study; pp. e475–e483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riva M.A., Paladino M.E., Belingheri M. The role of medical students during the COVID-19 pandemic. Annals of Internal Medicine. 2020;173:858–859. doi: 10.7326/L20-1194. [DOI] [PubMed] [Google Scholar]
- Savitsky B., Findling Y., Ereli A., Hendel T. Anxiety and coping strategies among nursing students during the covid-19 pandemic. Nurse Education in Practice. 2020;46 doi: 10.1016/j.nepr.2020.102809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw S.C.K. Hopelessness, helplessness and resilience: The importance of safeguarding our trainees’ mental wellbeing during the COVID-19 pandemic. Nurse Education in Practice. 2020;44 doi: 10.1016/j.nepr.2020.102780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang K., Wong E.L.Y., Ho K.F., Cheung A.W.L., Chan E.Y.Y., Yeoh E.K., Wong S.Y.S. Intention of nurses to accept coronavirus disease 2019 vaccination and change of intention to accept seasonal influenza vaccination during the coronavirus disease 2019 pandemic: A cross-sectional survey. Vaccine. 2020;38:7049–7056. doi: 10.1016/j.vaccine.2020.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]