Abstract
Providing health information is a non-pharmaceutical intervention designed to reduce disease transmission and infection risk by encouraging behavior change. But does knowledge change behavior? We test whether coronavirus health knowledge promotes protective risk mitigation behaviors early in the Covid-19 pandemic in samples from four African countries (Ghana, Malawi, Sierra Leone, and Tanzania). Despite reputations for weak health sectors and low average levels of education, health knowledge of the symptoms and transmission mechanisms was high in all countries in the two months after the virus entered the country. Higher knowledge was associated with increased protective measures that would likely lower disease risk with one exception–knowledge was inversely correlated with social distancing. Respondents largely adhered to mask mandates and lockdowns, but continued coming into contact with others at small, informal gatherings, gatherings not affected by mandates. Knowledge alone did not reduce all risky activities, especially gatherings within other people’s homes. Even early in the pandemic, income loss or stress were commonly reported. Our results suggest that early and consistent government provision of health information likely reduced the initial severity of the pandemic in Africa but was not a panacea.
Keywords: Pandemics, Non-pharmaceutical interventions, Coronavirus, Health behaviors, Risk mitigation, Lockdowns
1. Introduction
As the coronavirus pandemic emerged, policy makers were concerned that the health impacts of the pandemic may be disproportionately borne by lower income countries because of their weak health sectors and their populations’ inability to socially isolate (United Nations Economic Commission for Africa, 2020). This concern was particularly acute in Africa where despite younger populations, many residents had co-morbidities that could result in more severe symptoms, pushing weak health infrastructures past their limits (Lone and Ahmad, 2020). Absent a vaccine, countries relied on information campaigns to encourage individual non-pharmaceutical interventions (NPIs)–social distancing, hand washing, and mask wearing—and imposing community NPIs–closures of schools, businesses, and/or houses of worship. These NPIs did not rely on the sophistication or capacity of the health sector but instead depended on voluntary behavior change. Whether NPIs can be successful in lower income countries is an empirical question–do people understand and trust the information, adhere to mandates, and have the capacity and ability to change their risky behaviors?
We analyze the level of health knowledge and whether health knowledge increased the adoption of NPIs, such as mask-wearing and social distancing, using detailed survey data from four African countries collected early in the pandemic, early April through mid-June 2020, less than 2 months after the virus was first reported in each country. Our countries represent varied geography–West, East, and South–and income–lower-middle and low income. To collect data as quickly as possible we relied on samples for whom we already had phone numbers, resulting in samples that are not nationally representative. We sampled educators in Ghana, men in Malawi who frequented bars pre-pandemic, public transit riders in Sierra Leone, and Tanzanian shop owners about their knowledge of coronavirus symptoms and transmission mechanisms, their and their household’s experience with social distancing, and how their households were affected by the pandemic. With unified measures across four countries, we compare the knowledge, risk mitigation practices, and consequences of the pandemic (including associated lockdowns).
We have four main findings. 1) We find high levels of knowledge were associated with increased take-up of risk mitigation measures–the average respondent correctly reported 3 symptoms, 2 transmission mechanisms, and almost no incorrect symptoms or transmission mechanisms and undertook 2.3 “effective” protective measures.1 Despite the differences in sample characteristics across countries, we find substantial similarities in respondent knowledge across our samples. 2) Early government action, including messaging, mask mandates, and lockdowns, was associated with meaningful behavior change. People reported a substantial number of protective behaviors, particularly those that are relatively easy to adopt, such as masks, hand-washing, and not shaking hands. Mask use appeared heavily affected by policy: the rates of using masks were 50 percentage points higher in the mask mandate countries (Ghana and Sierra Leone) relative to the non-mask mandate countries (Malawi and Tanzania). The likelihood of coming into close contact with another person at a house of worship was similarly 50 percentage points lower in countries that mandated their closure (Ghana and Sierra Leone) relative to those that did not (Malawi and Tanzania). 3) Knowledge was not sufficient for adoption of social distancing, behavior that is likely the most effective at reducing disease transmission. The average respondent was in close physical contact with someone not in their household at 3.1 different locations in the week preceding the survey, with substantial variation across countries. Many of these interactions were in places satisfying basic needs, i.e. transportation, markets, and shared toilet facilities. However, non-essential contacts were also common—46 percent of respondents reported visiting another person’s home in the previous week. 4) Across all countries this pandemic and the policies enacted in response had severe impacts relatively early–54 percent of respondents reported income loss as a result of the pandemic and 49 percent reported increased stress.
Our paper contributes to four related literatures. First we contribute to the growing literature on how to manage and mitigate the effects of pandemics through NPIs. We show that information is an effective NPI as health knowledge increases protective health behaviors and encourages low-cost behavior that mitigates risk, e.g. hand washing, mask-wearing, and other risk mitigation measures. These findings are similar to the existing literature on information regarding sexual partners (Dupas, 2011a), unsafe water (Madajewicz et al., 2007), hygiene (Jalan, Somanathan, 2008, Cairncross, Shordt, Zacharia, Govindan, 2005), and the hypothesized ways NPIs could address Covid-19 (Haushofer and Metcalf, 2020). In lower income countries, individuals may not be able to reduce their risk to desired levels despite their level of knowledge. Consistent with that intuition, we show that health knowledge is positively correlated with the number of times in the past week an individual was in close contact with those outside of their household (i.e., knowledge is negatively correlated with social distancing) adding additional evidence on how the effectiveness of information can depend upon other factors, including the costs of following the information (Kremer et al., 2007), household bargaining power (Dupas, 2011b), a respondent’s beliefs regarding their eventual likelihood of contracting the disease (Kerwin, 2020), their life expectancy (Oster, 2012), or who issues the directives (Kao et al., 2020).
Second, our results contribute to a broader understanding of the combined effects of a pandemic and related lockdowns. Early in the pandemic the direct health effects of the disease were a focus, and we show that only 4 percent of households were directly infected by the virus, while about half reported income loss and half reported increased stress. Notably, the stress consequences were not concentrated among those who had lost income. Parents, in particular, reported additional stress, a worrisome outcome in a context with high rates of child abuse (Meinck, Cluver, Boyes, Mhlongo, 2015, Badoe, 2017).
Third, our results contribute to the literature on the differential experience of the pandemic across countries. We are the first to use harmonized individual level data across lower income countries on behavior change in response to the pandemic. The majority of the existing literature consists of descriptive statistics and does not discuss correlates of NPI use, nor the role of policy in contributing to differential NPI use across countries. While existing literature has focused on the role of demographics (Goldberg, Reed, 2020, Castex, Dechter, Lorca, 2020, Castex, Dechter, Lorca, 2020), government policies (Rannan-Eliya et al.), or political economy (Alsan, Braghieri, Eichmeyer, Kim, Stantcheva, Yang, et al., 2020, Chiplunkar, Das), less work has used individual level data on what role, if any, individual risk mitigation practices play at explaining Covid-19 prevalence worldwide (Rannan-Eliya et al.). In the US, Alsan et al. (2020b) showed the relationship between sociodemographic characteristics and reported knowledge and behavior in the US. We show that across four countries individual knowledge increased mitigation measures, but did not curtail all risky behaviors. We show that mandates helped individuals adopt risk mitigation strategies. Together, both of these findings suggest that both individual risk mitigation strategies and high rates of compliance with mandated, community NPIs may have contributed to the relatively low rates of Covid-19 cases in Africa, relative to richer countries, as of early 2021. Despite the lack of a direct health effect reported by households, we also add to the growing evidence that the social and economic consequences of the pandemic and related policies were severe and will likely linger (Erokhin, Gao, 2020, Amare, Abay, Tiberti, Chamberlin, 2020, Jain, Budlender, Zizzamia, Bassier, Mahmud, Riley, Josephson, Kilic, Michler).
Finally, we contribute to the literature on the elements of a successful public health campaign. Vaccinations have been successful at reducing the burden of disease and increasing life expectancy, in part because once an individual achieves immunity through vaccination no additional action is necessary by them (Karing, 2020a). In contrast, attempts to reduce malaria transmission through regular bed net use and reduce HIV/AIDS transmission through adherence to pharmaceutical regimes and risky behavior elimination have been more complicated (e.g. Lucas, 2010, Lucas, Wilson, 2018). Our contradiction between knowledge and some forms of action are similar to the behavior change-communication messaging campaigns during the HIV epidemics in the early 2000s (Lo et al., 2016). While abstinence-only education was ineffective at reducing transmission, encouraging a suite of other risk mitigation strategies such as using condoms was more effective, particularly for high risk groups (Okafor et al. 2017). However, continued use of condoms was difficult for individuals at lower risk to maintain (Foss et al. 2007). In the same way, individuals adopted risk mitigation measures in response to the coronavirus threat, but were unable to voluntarily adhere to extreme measures such as reducing all non-household contacts. Early in the pandemic, households in our sample were engaging in relatively lower-cost protective measures. However, we caution that such protective measures may wane as individuals find ongoing efforts burdensome as they wait for vaccine availability. We show that despite the important role of information as a non-pharmaceutical intervention, even knowledgeable households perform constrained optimization that might not allow them to fully realize the benefits of risk-mitigation.
2. Background
2.1. Country details
We selected four African countries that represent a wide dispersion of geography, population size, and income. Both Ghana and Sierra Leone are in West Africa, while Malawi is in the South and Tanzania is in East Africa. Tanzania has a population of 59 million, Ghana 30 million, Malawi 21 million, and Sierra Leone 7 million people. Based on gross domestic product per capita in 2019, purchasing power parity adjusted international dollars, Ghana was the richest ($5637) and Malawi the poorest ($1104) with Tanzania ($2771) and Sierra Leone ($1790) between the two, making Ghana and Tanzania lower-middle income and Sierra Leone and Malawi low-income (World Bank, 2020). Countries also varied substantially in their hospital bed capacity, reflective of their weak health infrastructures. In the most recent year data were available, for every 10,000 population, Ghana had 9, Malawi had 13, Tanzania had 7, and Sierra Leone had 4 hospital beds (World Health Organization, 2016). For comparison, the United States had 28.7 beds per 10,000 population. Finally, countries vary substantially in their educational attainment and literacy rate. Among those over 15, the literacy rate is relatively high in Ghana and Tanzania (79 and 78 percent, respectively) and lower in Malawi (62 percent) and Sierra Leone (43 percent).
2.2. Continent-wide responses
Health ministers across Africa acted early in response to the pandemic. Approximately one month after the January 22, 2020 consensus that Covid-19 transmitted between humans and in recognition of the potential impact of the pandemic, African health ministers established a coronavirus task force to create a continent-wide strategy (Osseni, 2020). This action was earlier than strategies and plans announced by richer countries.2 On March 11, the WHO declared the coronavirus a pandemic, and on June 5 the WHO updated its guidance on mask-wearing.
Governments, international bodies, and nonprofits enacted public health messaging campaigns, often in local languages, across the continent starting in early March. In addition to any programs by specific countries, UNICEF began large-scale public health messaging campaigns to improve awareness about the coronavirus. To combat misinformation, starting in April the WHO partnered with Twitter, Facebook, Tencent and TikTok to ensure the content on their platforms was accurate, set up websites to disseminate accurate information in local languages, and engaged Google to allow for targeted search of coronavirus information in local languages. In addition to private sector mobilization, the World Bank also issued $14 billion in grants to affected countries, with an intention to deploy up to an additional $16 billion over the next year and half to help countries cope with containing the public health threat. Other major NGOs, including Catholic Relief Services, Living Water International, Sightsavers, the Red Cross, and Save the Children, repurposed their campaigns from other diseases and ailments to focus on the coronavirus, including messaging targeted to increasing awareness and induce risk mitigation measures, such as hand washing. Individual philanthropists also contributed to the disaster preparedness. Chinese billionaire Jack Ma, for example, shipped a cargo flight containing 6 million medical items in late March to be distributed across the continent.
2.3. Country experiences with the pandemic
In addition to continent-wide policies, individual African countries sought to instigate behavior change through information campaigns, public service announcements, and community-level NPIs such as lockdowns and mask mandates. Rates of NPIs were notably higher in Africa than on other continents (Zheng et al., 2020). Table 1 , Panel A summarizes the experience of each country in our sample with the pandemic and associated closures.
Table 1.
Country & Dataset Descriptions.
| (1) | (2) | (3) | (4) | |
|---|---|---|---|---|
| Ghana | Malawi | Sierra Leone | Tanzania | |
| Panel A: COVID experiences | ||||
| First COVID case | March 12 | April 2 | March 30 | March 16 |
| Lockdown | March 16-May 20 | - | May 2-June 24, | March 17-June 1 |
| Scope of Closures | All public gatherings banned, churches and schools closed | Lockdown was announced but challenged in court and did not occur | 2 3-day lockdowns; businesses churches/schools closed | Schools closed, ban on mass public gatherings, otherwise limited in scope. |
| Nationwide Mask Mandate | April 24 | August 7 | April 24 | Not Enacted (See notes) |
| Est. Cumulative Cases (June 19, 2020) | 13,203 | 620 | 1298 | 509 (see notes) |
| Cases Per Million Pop | 440.1 | 29.5 | 185.4 | 9 (see notes) |
| Panel B: COVID Survey Statistics | ||||
| Geographic Scope | 7 regions | Zomba | Freetown | Dar Es Salaam and Dodoma regions |
| Respondent type | Educators | Men who frequent bars | Travelers | Microenterprise owners |
| Data Collection Period (2020) | May 7-May 22 | May 29-June 19 | April 22, - 30, May 6, - 16 | April 10-May 4 |
| Total Respondents | 362 | 1232 | 633 | 557 |
| Survey Response Rate | 0.88 | 0.46 | 0.79 | 0.93 |
Notes: In Tanzania, the nationwide mask mandate was only a recommendation and not a requirement. Local officials in Dar es Salaam ordered residents to wear face masks starting April 18. Tanzania stopped reporting virus cases and deaths May 8. Data on coronavirus caseloads are from the Kaiser Family Foundation database as of June 19, 2020, the last day of data collection in our sample. The Ghana lockdown was partially lifted April 20.
Ghana’s first diagnosed case was in March 12, and on March 16, the government closed churches, schools, and instituted an expansive lockdown that was partially lifted April 20. A nationwide mask mandate was instituted April 24. By July, Ghana released a miniseries called “Corona Life” to promote hygiene and sanitation, instituted enhanced public sanitation programs at markets, and began a testing and tracing program (for Strategic Studies, 2020). Schools reopened January 2021. As of June 19, 2020, the last day of our fieldwork across all four countries, Ghana had 13,203 cases (440 per million population) and 70 deaths.
Malawi’s first case was reported on April 2. The government began an extensive information campaign, including going door-to-door providing health information (Masina, 2020). The government proposed a complete lockdown to start on April 18, but the high court of Malawi blocked the lockdown in the absence of income protections, and no lockdown occurred. The government enacted a mask mandate on August 7. As of June 19, 2020, Malawi reported 620 cases (33 per million population) and 8 deaths.
Sierra Leone’s first case of the coronavirus was documented March 30. The lockdowns in Sierra Leone were brief, but almost total: two separate 3-day total lockdowns in which all non-essential businesses, schools, and churches were closed and travel was restricted. The government also instituted a mask mandate on April 24. By summer, the government (in coordination with the UNDP) had mobilized to provide lessons and trainings, including weekly videos on social media and community campaigns in local languages (UNDP Africa, GRID3). As of June 19, 2020, Sierra Leone reported 1298 cases (29.5 per million population) and 53 deaths.
Tanzania reported its first case on March 16, closing schools and banning mass gatherings the next day. While there was no nationwide mask mandate during our data collection, several areas within the country, including Dar es Salaam, one of our regions of study, mandated masks on April 18. In contrast to the other countries, the government prohibited media from reporting on the pandemic, prompting outrage from Reporters Without Borders and other civil liberties groups. After reporting 509 cases (9 per million population) and 21 deaths on May 8, on May 9, the government stopped reported coronavirus-related statistics, declaring the country free from the virus.
Our analysis uses individual survey data to show the commonalities and differences among our samples in their early experiences with the pandemic. Together, our results provide additional insight into the observation that the early health impacts of the coronavirus pandemic had not been as devastating as feared in Africa, and that most of the decreases in years of lost life early in the pandemic were concentrated in richer countries (Marois et al., 2020).
3. Data
Our data span four countries and three months. We collected our data through phone-based surveys that occurred from April 10 to June 19, with variation by country. Panel B of Table 1 provides the exact dates of each survey, along with additional details of data collection. To reach many respondents in a short period of time, we used existing samples from studies with previously collected phone numbers. As a result we had high response rates (averaging over 62 percent) and were able to collect data early in the pandemic, but our data are not nationally representative. Data from Ghana were collected from educators, i.e. teachers, head teachers (school principals), and circuit supervisors (school supervisors who oversee clusters of eight geographically proximate schools), as part of a follow-up for a school-based differentiated instruction intervention from Beg et al (2020). Respondents from Malawi were men who frequented bars pre-pandemic in the Zomba district and were part of an HIV study by Derksen et al. (2020). Respondents in Sierra Leone were residents of Freetown who rode public transportation pre-pandemic and participated in a pilot of an intervention designed to improve safety on public transportation (Karing, 2020b). Respondents in Tanzania were microenterprise owners participating in a study on the effects of kinship taxation (Squires, 2020). Data were collected starting just over 3 weeks after the first case in Sierra Leone and Tanzania and 8 weeks after the first case in both Ghana and Malawi.
Respondents in each country were asked the same questions about their coronavirus knowledge and related behaviors and the effects of the pandemic and related government mandates on their households. Respondents volunteered their responses and were not prompted about each individual symptom, mechanism, or location.3 Following public health guidance early in the pandemic, we consider hand-washing, social distancing, using hand sanitizer, wearing a mask, not sharing food, and not shaking hands as effective preventative measures. We highlight the role of masks in our discussion out of growing evidence of the high effectiveness of masks at reducing transmission and death (Eikenberry, Mancuso, Iboi, Phan, Eikenberry, Kuang, Kostelich, Gumel, 2020, Gandhi, Beyrer, Goosby, 2020, Lyu, Wehby, 2020, Murray, 2020). The correct transmission mechanisms were airborne, touching others, touching contaminated surfaces, and asymptomatic transmission. The correct symptoms were coughing, fever, fatigue, difficulty breathing, loss of taste or smell, headache, and sore throat (although results are not sensitive to the inclusion of less commonly reported symptoms, such as sneezing).
We additionally collected demographic details from these respondents. Because educational systems are not uniform across countries, we created three educational categories across transition points common to all countries–no schooling, some schooling but less than secondary school completion, and secondary school completion or more. Table 2 contains summary statistics of the sample demographics. While the sample characteristics vary by country, our overall sample is about 34 years old, 75% male, and almost all have at least one child in their household. Appendix Table B1 contains averages from nationally representative samples. Overall, our sample is older, more likely to be male, more likely to have children, and more highly educated. In all countries except Ghana, our sample is more urban than in the general population. Our sample characteristics may also differ in other ways. For example, the Ghanaian educators in our sample continued to receive their salaries during the sample period despite school closures. However, the Tanzanian shop owners in our sample may have disproportionately been affected by demand changes from the pandemic and associated lockdowns, although whether business improved or slowed likely varied by shop type. We report findings by country, noting the similarities and differences, and include country fixed effects and demographic controls when we pool our data. Even though our samples are not nationally representative, they are informative about experiences, knowledge, and behavior changes early in the pandemic.
Table 2.
Sample Statistics.
| (1) | (2) | (3) | (4) | (5) | (6) | |
|---|---|---|---|---|---|---|
| Ghana | Malawi | Sierra Leone | Tanzania | Average | PValue Joint Eq | |
| Age | 34.8 | 35.1 | 30.5 | 37.0 | 34.2 | 0.00 |
| Male | 0.82 | 1.00 | 0.66 | 0.56 | 0.75 | 0.00 |
| Has children | 0.86 | 0.93 | 0.94 | 0.87 | 0.91 | 0.00 |
| Rural | 0.76 | 0 | 0 | 0.40 | 0.23 | 0.00 |
| No schooling | 0.00 | 0.00 | 0.02 | 0.02 | 0.01 | 0.02 |
| Some Schooling | 0.00 | 0.20 | 0.17 | 0.83 | 0.35 | 0.00 |
| Secondary or Higher | 1.0 | 0.79 | 0.82 | 0.15 | 0.63 | 0.00 |
| Observations | 362 | 563 | 633 | 557 | 2115 | |
Notes: Above are averages of select variables aggregated for each country. Missing observations for a given variable are not included. Column 6 contains the p-value of the joint test of equality of the averages by country. * p 0:10, ** p 0:05, *** p 0:01
4. Empirical strategy
We first present evidence on the average levels of knowledge and preventative measures taken across countries. We then test the relationship between demographics and knowledge and behavior by estimating
| (1) |
where is knowledge or behavior for respondent in country , are individual level demographic covariates, and are country fixed effects.4 Our outcomes of interest are the number of correct symptoms, the number of correct transmission mechanisms, the number of effective protective measures taken, and the number of contacts. The coefficients on the individual demographics, , tell us the relationships between demographics and outcomes net of country-level differences while the country fixed effects elucidate the differences between countries net of demographic differences in the sample.
To test whether health knowledge is correlated with risk mitigation health behaviors we estimate the following equation:
| (2) |
where is a protective health behavior undertaken by respondent in country , and are the number of correct symptoms and transmission mechanisms the respondent reported, are the individual level demographic covariates considered above, and are country fixed effects. In this specification our focus is on and —the relationships between knowledge and behavior, net of demographic characteristics and country fixed effects.5 Our outcomes of interest are the number of effective protective measures taken and the number of non-socially distant contacts.
5. Results
5.1. Average levels of knowledge, actions, and pandemic effects
Table 3 contains the averages both within each country (columns 1–4) and across countries (column 5) for the knowledge and behavior questions, with column 6 providing the p-value associated with joint equality across all samples.
Table 3.
Knowledge and Action by Country.
| Ghana | Malawi | Sierra Leone | Tanzania | Total | PValue Joint Eq | |
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Panel A: Transmission Knowledge | ||||||
| No transmission knowledge | 0.00 | 0.01 | 0.02 | 0.02 | 0.01 | 0.09 |
| #Correct transmission mechanisms | 2.4 | 2.1 | 2.0 | 2.1 | 2.1 | 0.66 |
| Airborne cough | 0.84 | 0.96 | 0.82 | 0.79 | 0.85 | 0.00 |
| Touching others | 0.80 | 0.71 | 0.77 | 0.82 | 0.77 | 0.00 |
| Touching surfaces | 0.64 | 0.37 | 0.36 | 0.38 | 0.42 | 0.63 |
| Asymptomatic people | 0.10 | 0.03 | 0.08 | 0.08 | 0.07 | 0.00 |
| Panel B: Symptom Knowledge | ||||||
| Stated no knowledge of symptoms | 0.01 | 0.01 | 0.02 | 0.05 | 0.02 | 0.00 |
| # Correct symptoms listed | 3.2 | 2.8 | 3.1 | 2.9 | 3.0 | 0.51 |
| Coughing | 0.90 | 0.79 | 0.77 | 0.709 | 0.78 | 0.01 |
| Fever | 0.74 | 0.80 | 0.73 | 0.618 | 0.72 | 0.00 |
| Sneezing | 0.57 | 0.63 | 0.74 | 0.44 | 0.60 | 0.00 |
| Difficulty breathing | 0.38 | 0.60 | 0.39 | 0.46 | 0.46 | 0.00 |
| Headache | 0.42 | 0.00 | 0.28 | 0.43 | 0.27 | 0.00 |
| Sore throat | 0.32 | 0.01 | 0.26 | 0.13 | 0.17 | 0.00 |
| Fatigue | 0.17 | 0.02 | 0.15 | 0.24 | 0.14 | 0.00 |
| Loss of smell | 0.04 | 0.32 | 0.04 | 0.01 | 0.10 | 0.00 |
| Loss of taste | 0.03 | 0.146 | 0.04 | 0.00 | 0.06 | 0.00 |
| Panel C: Protective Measures | ||||||
| No protective measures | 0.00 | 0.13 | 0.00 | 0.00 | 0.04 | 0.00 |
| # Protective measures taken | 3.4 | 2.1 | 3.4 | 2.4 | 2.8 | 0.00 |
| # Effective protective measures taken | 3.0 | 1.7 | 3.0 | 1.7 | 2.3 | 0.00 |
| Wearing mask | 0.78 | 0.30 | 0.82 | 0.18 | 0.49 | 0.00 |
| Hand washing | 0.85 | 0.82 | 0.85 | 0.86 | 0.84 | 0.28 |
| Hand sanitizer | 0.66 | 0.00 | 0.61 | 0.18 | 0.33 | 0.00 |
| Not shaking hands | 0.25 | 0.48 | 0.35 | 0.60 | 0.44 | 0.00 |
| Not sharing foods | 0.04 | 0.01 | 0.00 | 0.01 | 0.01 | 0.11 |
| Not affected | 0.08 | 0.11 | – | 0.18 | 0.14 | 0.00 |
| Panel D: Social Distancing | ||||||
| Decreased social contacts | 0.74 | 0.75 | 0.66 | 0.52 | 0.66 | 0.00 |
| Contact non-household? | 0.72 | 1.00 | 1.00 | 1.00 | 0.95 | 0.00 |
| # Places In Last Week | 1.61 | 5.47 | 1.72 | 3.18 | 3.11 | 0.00 |
| Children Had Contact Outside HH | 0.48 | 0.79 | 0.50 | 0.60 | 0.60 | 0.00 |
| Observations | 362 | 563 | 633 | 557 | 2115 | |
Notes: Above are averages of select variables aggregated for each country. Missing observations for a given variable are not included. Whether children living in the household had contacts with others is among the sample that reported children living in their household. Due to an omission, how respondents were affected by the pandemic were not asked in Sierra Leone. Column 6 contains the p-value of the joint test of equality of the averages by country. Correct transmission is defined as reporting contracting the coronavirus through air, by touching others, from touching contaminated surfaces, and asymptomatic infections. Correct symptoms are defined as coughing, fever, fatigue, difficulty breathing, loss of smell/taste, headache, and sore throat. * p 0:10, ** p 0:05, *** p 0:01
Almost everyone (99%) had at least some correct transmission knowledge with the average person listing 2 (of 4). Interestingly, despite all the differences between the countries and the samples, we fail to reject that the number of correct transmission mechanisms listed is the same across countries. We also find very high symptom knowledge (Panel B)–only 2% of respondents could list no correct symptoms, with the average person naming 3 symptoms. In our data, with voluntary response, 55% of respondents report 3 or more correct symptoms, with a maximum of 8.6 7 By comparison, Alsan et al. (2020) found that in a US sample 87% of respondents could correctly identify the top three symptoms of coronavirus out of a list. Geldsetzer (2020) also found high rates of knowledge (80–85%) in the US and UK using voluntary response, although the number of symptoms given is not reported (Geldsetzer, 2020, Alsan, Stantcheva, Yang, Cutler, 2020). As with transmission knowledge, we fail to reject equality across countries.
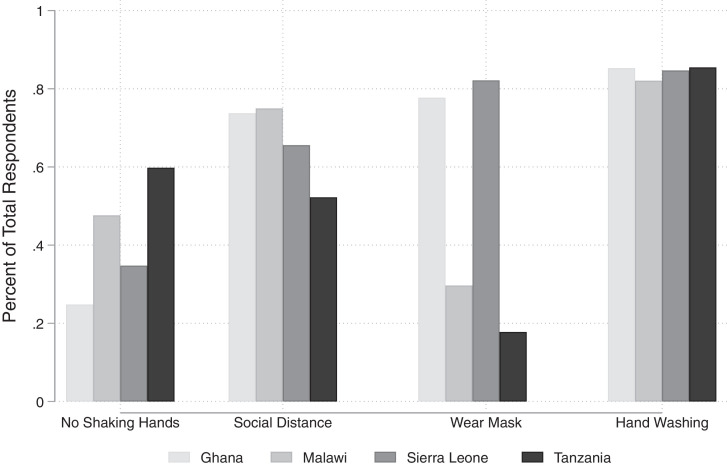
The protective measure means appear in Panel C. Despite people knowing statistically indistinguishable numbers of transmission mechanisms across countries, respondents’ actions vary by country. Malawi is an obvious outlier—in Malawi almost 13% of the sample was taking no protective measures. This relatively high average in the Malawian sample may reflect the sampling frame—men who frequented bars pre-pandemic may be disproportionately likely to take risks. In the other countries, almost all respondents were taking at least one protective measure. In the two countries without mask mandates (Malawi and Tanzania), fewer than 30 percent of respondents reported wearing a mask, while over three-quarters of respondents reported wearing a mask in the two countries with mask mandates (Ghana and Sierra Leone). Over 80 percent of respondents in each country, statistically equivalent across countries, offered hand washing as one protective measure they were taking. Appendix Fig. B1 graphically depicts the portion of people in each country who reported taking each measure.
Fig. B1.
Percent of Respondents Reporting Each Protective Measure Notes: This bar chart shows the percent of respondents reporting the most commonly mentioned protective measures by country.
Despite over 50% of respondents in each country knowing that reducing exposure to others is a way to protect against infection, over 70% of respondents reported having contact within two meters of someone outside of their household in the last week, averaging 3 such places where that contact occurred. Further, slightly more than half of respondents with children reported that their children had close contacts with others outside their household in the last week. Across all four countries, the most common place that people had contacts with others was the market (Appendix Fig. B2 presents a bar chart of the most commonly mentioned contact locations by country). For our Ghana, Sierra Leone, and Tanzania respondents, the next places of contact in descending order were other houses, public transportation, and work. In contrast, the Malawian respondents reported work almost as frequently as the market. This average may also reflect the sampling frame in Malawi—men who patronized bars pre-pandemic may be disproportionately likely to have work outside the home that requires in person attendance and be in an urban area.
Fig. B2.
Type of Social Contacts By Country Notes: This bar chart shows where respondents reported close contact with a person outside of their household in the previous week by country.
The full set of responses by country appear in Appendix Table B3, disaggregated by whether the contact occurred at “informal” (i.e., smaller gatherings or contacts that are incidental to the activity–markets, another person’s house, transportation, communal wash facilities, or takeout dining) or “formal” (i.e., organized events or larger gatherings where contact is assumed–work, worship, dine-in restaurant, weddings or other celebrations or festivals, or other large meetings) activities. Informal activities were less likely to be affected by government lockdowns and would therefore be primarily affected by voluntary behavior change. In our data, informal contacts were nearly twice as commonly reported as formal contacts (2 locations compared to 1 location, on average).
The relative magnitude of contacts at formal vs. informal activities could be partially driven by government policies in effect at the time of data collection that closed businesses and resulted in canceled formal gathering opportunities. Informal gatherings were still commonly reported in all countries, suggesting that mandates would not reduce this sort of risky behavior. However, our data suggest that lockdowns were effective at reducing large gatherings, such as at houses of worship or restaurants. For example, enforced mandates of closures of houses of worship resulted in virtually no contacts at those locations among Ghanaian and Sierra Leonean respondents.8 Rates of informal contacts may be high because many of the locations of informal contacts lack readily available substitutes in the developing country context. For example, in richer countries grocery delivery or refrigerator storage can limit market trips, uncommon features in lower income countries. Home visits were also frequent–on average 48% of respondents across all countries visited another person’s home. While such visits are small gatherings, the secondary transmission rate within an enclosed home can be as high as 35% (Liu et al., 2020). Our data suggest that mandates potentially reduced large gatherings (aside from markets), and substantially reduced the number of contacts, but that close encounters with others was still commonly reported.
Table 4 shows that respondents varied substantially in their experiences with the coronavirus and associated lockdowns. Although very few individuals were affected directly in terms of health of themselves or a household member (4%), mental health and economic impacts of the lockdown were commonly reported by about 50 percent of our sample.
Table 4.
Effects of the Pandemic.
| (1) | (2) | (3) | (4) | (5) | |
|---|---|---|---|---|---|
| Ghana | Malawi | Tanzania | Average | PValue Joint Eq | |
| Reduction in income/resources | 0.39 | 0.75 | 0.40 | 0.54 | 0.00 |
| Stress | 0.65 | 0.45 | 0.44 | 0.49 | 0.00 |
| Children home from school | 0.44 | 0.47 | 0.25 | 0.38 | 0.41 |
| Reduction in food | 0.17 | 0.11 | 0.05 | 0.10 | 0.0 |
| Household infected | 0.01 | 0.09 | 0.00 | 0.04 | 0.0 |
| Increase in household size | 0.09 | 0.02 | 0.04 | 0.04 | 0.0 |
| Fewer monetary transfers | 0.00 | 0.08 | 0.00 | 0.03 | 0.32 |
| Sent more transfers | 0.07 | 0.00 | 0.04 | 0.03 | 0.0 |
| Increase on phone/internet | 0.07 | 0.00 | 0.01 | 0.02 | 0.0 |
| Decrease in household size | 0.01 | 0.02 | 0.02 | 0.02 | 0.0 |
| More monetary transfers | 0.00 | 0.00 | 0.01 | 0.08 | 0.32 |
| Household death | 0.01 | 0.01 | 0.00 | 0.01 | 0.45 |
| Self-infected | 0.01 | 0.01 | 0.00 | 0.01 | 0.99 |
| Observations | 278 | 563 | 557 | 1398 | |
Notes: Averages of select variables aggregated for each country. Missing observations for a given variable are not included. Due to an omission these questions were not asked in Sierra Leone. Column 5 contains the p-value of the joint test of equality of the averages by country. * p 0:10, ** p 0:05, *** p 0:01
Stress was the most common effect of the pandemic for our Ghana sample, even though Ghanian educators, the respondents in our sample, continued to be paid by the government while schools were closed. Stress was in the top three of all reported effects in the other two countries.9 An online poll similarly found increases in reported stress during the lockdown period in Ghana (Asiamah et al., 2020). Reduction of income was the most common effect of the pandemic in our Malawi sample and was also mentioned by about 40% of respondents in Ghana and Tanzania. This substantial reporting of income loss in Malawi is particularly noteworthy because Malawi did not have a government-mandated lockdown. Having children home from school was another frequently mentioned effect of the pandemic. In Appendix Table B4, we show the effects of the pandemic, disaggregated by whether that respondent reported increased stress. Increased stress is not only felt among those that lost income—those who reported income loss were as likely to report stress as those who did not report income loss. To test for expenditure changes, we collected additional data regarding spending in Sierra Leone. In our Sierra Leone sample, 82 percent of respondents reported pandemic related expenditure changes. Respondents reported higher spending on food, electricity, and medicine and lower spending on clothing and communications. Respondents reported price increases and shortages driving the increased expenditures.
5.2. Correlates of knowledge and behavior
In this sub-section we combine the data from all four countries to consider the correlation between sociodemographic characteristics and knowledge and behavior as well as country-specific differences, estimates of Eq. (1) with a separate outcome each time. The results appear in Table 5 . Net of country fixed effects, knowledge of correct symptoms (column 1) is statistically positively correlated with age and increases with educational attainment (relative to no education). Knowledge of correct transmission mechanisms (column 2) is positively related to education. For both of these knowledge outcomes, the other three countries have lower levels of knowledge than among our Ghanaian respondents, the reference category in this Table.
Table 5.
Correlates of Knowledge and Behavior.
| (1) | (2) | (3) | (4) | |
| # Correct Symptoms | # Correct Transmission | # Effective Protective Measures | # Social Contacts | |
| Demographic Variables | ||||
| Male | -0.107 | 0.063 | 0.110* | 0.267*** |
| (0.066) | (0.043) | (0.061) | (0.088) | |
| Age | 0.023* | 0.007 | 0.014 | 0.018 |
| (0.013) | (0.010) | (0.013) | (0.021) | |
| Children in HH | -0.049 | -0.014 | 0.212** | 0.055 |
| (0.089) | (0.060) | (0.085) | (0.125) | |
| Some Schooling | 0.312* | 0.390** | 0.050 | 0.436 |
| (0.186) | (0.168) | (0.216) | (0.422) | |
| Secondary or Higher | 0.757*** | 0.634*** | 0.243 | 0.431 |
| (0.188) | (0.171) | (0.219) | (0.420) | |
| Rural | -0.111 | -0.078 | -0.072 | -0.146 |
| (0.089) | (0.058) | (0.071) | (0.142) | |
| Country Dummies | ||||
| Malawi | -0.185 | -0.299*** | -1.188*** | 3.777*** |
| (0.120) | (0.080) | (0.103) | (0.172) | |
| Sierra Leone | -0.214* | -0.272*** | 0.055 | 0.123 |
| (0.124) | (0.080) | (0.101) | (0.156) | |
| Tanzania | -0.062 | -0.105 | -0.839*** | 2.089*** |
| (0.125) | (0.082) | (0.108) | (0.186) | |
| Observations | 1991 | 1991 | 1991 | 1991 |
| 0.04 | 0.04 | 0.21 | 0.48 | |
| Mean Dep. | 2.69 | 2.11 | 2.71 | 3.17 |
| Country Jointly Zero | 0.28 | 0.00 | 0.00 | 0.00 |
| Education Jointly Zero | 0.00 | 0.00 | 0.03 | 0.58 |
Notes: The omitted category for education is those with no schooling. The omitted country is Ghana. Individuals with missing control variables have their value set equal to the mean for their country with a dummy variable to mark the imputation. Robust standard errors correcting for heteroskedasticity in parenthesis. ”Country Jointly Zero” presents the p-value on the null that all country dummies are jointly equal to zero. ”Education Jointly Zero” presents the p-value on the null that all education dummies are jointly equal to zero. * p 0:10, ** p 0:05, *** p 0:01
The number of increased protective measures undertaken was not statistically related to education (column 3). Being male or living in households with children were associated with taking more protective measures. As with the knowledge outcomes, both our Malawi and Tanzania samples report fewer protective measures relative to Ghana (the reference category) while those from Sierra Leone are statistically indistinguishable from those in the Ghana sample. None of the sociodemographic covariates besides gender–men have more contacts–have a statistically significant relationship with the number of social contacts (column 4). Respondents from both the Malawian and Tanzanian samples have more contacts relative to Ghanaian sample, net of demographic differences.
Although individual characteristics included in our specification explain little of the variation of symptom or transmission knowledge (R-squared of 0.04 in columns 1 and 2), our independent variables explain 48% of the variation in the number of locations of social contacts. Most of the variation in contacts is across countries, not within, potentially reflective of the messaging and political economy surrounding the coronavirus experience.
5.3. Relationship between knowledge and behavior
In Table 6 , we show that health knowledge is positively associated with behaviors that protect individuals against the coronavirus, whether or not we control for sociodemographic controls. Specifically, knowledge of coronavirus transmission mechanisms and symptoms is positively related to taking more risk mitigation measures—each correct symptom known is associated with an additional 0.23 protective measures and each additional transmission mechanism known is associated with another 0.40 effective protective measures (column 1). Despite the correlations found in Table 3 between knowledge and sociodemographic controls, these point values are nearly identical with the inclusion of those controls (column 2). Results for individual protective measures are in Appendix Table B5. Individuals with higher knowledge of either symptoms or transmission mechanisms reported increasing the likelihood that they sanitized their hands, engaged in social distancing, washed their hands, did not shake hands, and wore masks.10 These results are evidence that information encourages the adoption of NPIs that are likely easy to adopt in resource-poor settings.
Table 6.
Correlates of Protective Measures Taken.
| (1) | (2) | |
|---|---|---|
| # Effective Protective Measures | # Effective Protective Measures | |
| # Correct Symptoms Listed | 0.230*** | 0.230*** |
| (0.020) | (0.021) | |
| # Correct Transmission Mechanisms | 0.400*** | 0.398*** |
| (0.030) | (0.031) | |
| Male | 0.092* | |
| (0.055) | ||
| Age | 0.010 | |
| (0.012) | ||
| Rural | -0.013 | |
| (0.064) | ||
| Some Schooling | -0.168 | |
| (0.190) | ||
| Secondary or Higher | -0.179 | |
| (0.194) | ||
| Observations | 1,991 | 1,991 |
| R2 | 0.35 | 0.35 |
| Mean Dep. | 2.71 | 2.71 |
Notes: All regressions include a country fixed effect. Column 2: The reference educational category is those with no schooling. Individuals with missing control variables have their value set equal to the mean for their country with a dummy variable to mark the imputation. Robust standard errors to correct for heteroskedasticity in parenthesis. * p 0:10, ** p 0:05, *** p 0:01
In Table 7 , we estimate the correlation between knowledge and the number of locations at which an individual came within 2 m of another person outside of their household in the previous week, controlling for country fixed effects and sociodemographic controls. In contrast to the results in Table 6 that showed higher knowledge resulted in more protective measures, higher knowledge of coronavirus transmission mechanisms are positively correlated with the number of locations with close contacts, indicating those with more knowledge undertook additional risky behaviors (column 1).This coefficient remains positive and statistically significant even after controlling for the number of other protective measures (column 2). Notably, other protective measures are also positively correlated with the number of social contacts, suggesting that individuals may be compensating for their increased social contacts with increasing other risk mitigation measures. In particular, as Appendix Table B7 shows, transmission knowledge is positively associated with going to other people’s homes, taking public transport, and eating at a restaurant, suggesting more informed individuals were more likely to interact with others in casual settings that might have lower perceived risk.13
Table 7.
Correlates of Number of Contacts.
| (1) | (2) | (3) | |
|---|---|---|---|
| # Contacts | # Contacts | # Formal Contacts | |
| # Correct Symptoms Listed | 0.030 | -0.007 | -0.006 |
| (0.035) | (0.035) | (0.018) | |
| # Correct Transmission Mechanisms | 0.258*** | 0.191*** | 0.037 |
| (0.050) | (0.052) | (0.027) | |
| #Protective Measures (excluding social distancing) | 0.189*** | 0.058*** | |
| (0.040) | (0.021) | ||
| Male | 0.249*** | 0.245*** | 0.187*** |
| (0.086) | (0.086) | (0.043) | |
| Age | 0.017 | 0.015 | 0.027*** |
| (0.021) | (0.021) | (0.010) | |
| Rural | -0.122 | -0.100 | 0.363*** |
| (0.142) | (0.142) | (0.074) | |
| Some Schooling | 0.329 | 0.346 | 0.267 |
| (0.414) | (0.406) | (0.214) | |
| Secondary or Higher | 0.247 | 0.278 | 0.226 |
| (0.413) | (0.405) | (0.213) | |
| Observations | 1,991 | 1,991 | 1,991 |
| R2 | 0.49 | 0.50 | 0.53 |
| Mean Dep. | 3.17 | 3.17 | 1.11 |
Notes: All regressions include a country fixed effect. Individuals with missing control variables have their value set equal to the mean for their country with a dummy variable to mark the imputation. Column 3: Number of formal contacts includes contacts at houses of worship, events such as wedding or funerals, meetings, and meals at restaurants. Robust standard errors to correct for heteroskedasticity in parenthesis. * p 0:10, ** p 0:05, *** p 0:01
In column 3, we consider whether information is effective at reducing “formal” contacts: the number of times an individual went to a location that would potentially be affected by a lockdown (religious services, dining at restaurants, meetings, or other events). Knowledge did not change the overall number of formal contacts but did increase the likelihood of coming into contact with someone at a restaurant (Appendix Table B7).
In Appendix Fig. B3, we plot the number of protective behaviors taken relative to a person with 0 reported contacts to test if individuals relatively more exposed to the coronavirus through more contacts were more likely to engage in protective measures. For individuals with only 1 or 2 contacts there was a weakly negative relationship. However, once an individual reported three or more contacts, there was a weak, but positive relationship: as individuals frequent more places, the number of protective behaviors that the individual engaged in also increased. Although some estimates are not different than zero, these results suggest some degree of risk compensation. Maintaining social distancing appears hard, and individuals with knowledge compensated by engaging in other risk mitigation measures. However, for the specific outcome of mask-wearing, a highly effective way to reduce transmission in the presence of close contacts, additional contacts were not associated with a higher likelihood of mask wearing (see Appendix Fig. B4), and the correlation is not differential according to health knowledge (not shown).
Fig. B3.
Number of Preventive Behaviors By Number of Social Contacts Notes: This coefficient plot displays the difference in number of protective activities that a respondent engages in disaggregated by the number of places that they report visiting in the past week.
Fig. B4.
Likelihood of Mask Wearing By Number of Social Contacts Notes: This coefficient plot displays the difference in number of protective activities that a respondent engages in disaggregated by the number of places that they report visiting in the past week. Coefficient estimates are based upon a regression that includes country fixed effects and the standard controls.
Those with more contacts could have increased knowledge due to discussing the ongoing pandemic with those contacts. In Sierra Leone, we collected data on where individuals received their information on Covid-19. Learning from friends and family was mentioned by 50% of respondents, and was the third-most common source, behind radio (68%) and TV (75%). If individuals were learning Covid-19 knowledge from their contacts, then knowledge would potentially have increased during the course of our data collection. Fig. 1 shows the average knowledge of coronavirus symptoms and transmission by interview date in each country. In each country, the time trend of knowledge is relatively flat, suggesting that average knowledge of the disease was not growing over time. As our question regarding contacts asked people to reflect on the previous 7 days, these findings suggest that individuals were not acquiring knowledge as a result of more social contacts, but rather had knowledge and continued with relatively high rates of contacts. There is similarly no clear triend of social distancing in any country.11
Fig. 1.
Time Trend of Symptom Knowledge Notes: Lines are the time trends of the primary knowledge variables, disaggregated by country, weighted by the number of interviews in the country per day. In Ghana, Sierra Leone, and Tanzania there is no statistically significant time trend of symptom or transmission knowledge. In Malawi, there is a weak positive time trend for symptom knowledge (p=0.052) but not transmission knowledge.
6. Discussion and conclusion
In this paper we examine the role of information as a non-pharmaceutical intervention (NPI) to induce risk mitigation behaviors early in the coronavirus pandemic across four samples in Africa—educators in Ghana, men who frequented bars pre-pandemic in Malawi, public transit riders in Sierra Leone, and microenterprise owners in Tanzania. Only one to two months after the first reported cases in each country, knowledge of the coronavirus symptoms and transmission mechanisms was relatively high. Information was positively correlated with reports of other non-pharmaceutical interventions that mitigate the spread of the coronavirus, such as hand washing, mask wearing, increased social distancing, and using hand sanitizer. Relatively high rates of use of these measures early on in the pandemic may partly explain why Africa had relatively few deaths per capita in 2020 compared to richer regions. Across the four countries we study, the same high rates of knowledge were found across the data collection period.
The risk mitigation strategies we observe range from relatively easy for individuals to adopt (such as not shaking hands) to relatively hard to adopt (such as not coming into contact with someone when undertaking essential life-sustaining activities like shopping at a market). Many of the places where individuals had contact with others lack low-risk alternatives. For example, grocery deliveries may be expensive or unavailable, particularly in rural areas. Car ownership is also less common in developing countries, making public transportation more essential for travel. Therefore, avoiding others by avoiding markets or public transportation may be a relatively high-cost strategies for individuals to mitigate risk. Below, we discuss whether small, informal gatherings at other people’s houses are indeed easily avoidable by our sample.
Two of our findings could be counter-intuitive. First, we find that health knowledge was either not correlated with or positively related to a particular risky behavior—the number of locations an individual came into close contact with someone outside their household in the past seven days. Therefore, knowledgeable people undertook some but not all behavior changes to mitigate their risk. This puzzling relationship could have been due to those who knew that they could not limit their contacts seeking to learn more about the disease. If this were the dominant source of the relationship, knowledge would likely be increasing during our data collection period, which was early in the pandemic. Instead we find no trend in knowledge. Therefore, while we cannot empirically reject this knowledge seeking hypothesis, we find it unlikely. Instead our findings are consistent with risk compensation, i.e. safety measures can increase risky behaviors (Peltzman, 1975). More knowledgeable people were more likely to engage in safety measures such as mask-wearing and washing hands, while also having more points of contacts with those outside their immediate households. Therefore, our findings are suggestive that having a deeper understanding of how to mitigate risk could cause people to take some precautions that lower their risk, while also increasing the likelihood of engaging in activities outside the home that put them at a higher risk of infections.
Second, smaller informal gatherings persisted despite high overall levels of transmission knowledge. Visiting other people’s homes could have been viewed as a relatively safer activity than interactions with the general public. Individuals may have had more information regarding the activities of those whom they knew well and thus perceived the risk of infection to be relatively low from interacting inside their home. Unfortunately, we lack direct evidence on risk perceptions of Covid-19 of various locations and thus do not know people's relative perceived Covid-19 risk. These home visits could further have been calculated reactions to increased stress levels reported by our respondents: the cost to mental health of not having these contacts could have exceeded the perceived threat of infection from maintaining them. High levels of stress during the pandemic are not specific to our sample, but rather have been noted in a range of other countries and populations, including Groarke et al. (2020), Kowal et al. (2020), Varma et al. (2021) and Loades et al. (2020). Further, people could have visited with other households to maintain networks that might provide social insurance if the household experienced a negative economic or health shock. Meeting in person could have been the only way to maintain social ties whether to reduce stress or as social insurance. While people in higher income countries can visit with friends and family via video-chat, limited or expensive internet and smart device availability would have made this more difficult for our respondents. These results confirm the findings in Kao et al. (2020) that information as an NPI is most effective when the particular risk mitigation strategy has low costs or high benefits. The continuation of the visits could also be related to the NPIs changing information but not norms. Norms can influence an individual’s decision to reduce contacts and informing people about community support for social distancing could change their likelihood of compliance (Allen et al., 2021). Finally, individuals may have felt that if they were the only ones avoiding others, then the costs to them were high relative to the benefit.
Our findings have three implications for public policy. First, even those with high levels of knowledge continued to engage in informal gatherings, perhaps because of the stressful context of the early pandemic period. While Maire (2020) found that extreme poverty, and those with vulnerable employment, particularly in agriculture, were less able to comply with lockdown requests, Krekel et al. (2020) found that personal happiness and mental health were also a key factor in lockdown compliance. Therefore, additional campaigns that increase symptom and transmission knowledge will likely not reduce these interactions. Instead, voluntary behavior change appears a more complicated utility maximization problem that could involve changing people’s norms and cost-benefit assessments.
Second, the direct health effects of the pandemic were not the only costs. Many more respondents reported income loss and increased stress than those that reported direct health effects in their households. The potential negative consequences of long-term stress should be given appropriate consideration, particularly in the context of children at home from school at risk of abuse.
Third, individuals will undertake their own cost-benefit assessments that might not align with true underlying risks or those perceived by policymakers. Individuals largely adhered to formal closures in the countries in which they were instituted, yet continued small indoor gatherings that are both a substantial potential source of transmission and not likely easy to curtail. Clear, consistent communication about risks and benefits appear paramount along with providing messaging about which activities are relatively lower risk.
Early in the pandemic, consistent and timely health information across the four countries of study likely increased the likelihood that people took many, but not all, preventative health behaviors. As the pandemic continues into year 2, the messaging and support available to households will likely need to evolve, especially as pandemic fatigue increases.
Declaration of Competing Interest
None.
Footnotes
We gratefully acknowledge generous funding from the Sandra Rotman Centre for Health Sector Strategy, the Joseph P. Healey Research Grant, the Canada Excellence Research Chairs program awarded to Dr. Erik Snowberg in Data-Intensive Methods in Economics, Co-Impact through a Jameel Poverty Action Lab (J-PAL) sub-award. For excellent research management and assistance we thank Henry Atimone, Charlotte Burlingame, and Heather Wong. We thank the entire field team in each country for their efforts in completing these surveys. We thank Marcella Alsan, Emily Beam, Janet Currie, Alan de Brauw, David Molitor, Kosali Simon, and Laura Wherry for helpful comments. All errors are our own.
Effective protective measures were wearing a mask, washing hands, using hand sanitizer, and reducing social contacts (Cowling and Aiello, 2020).
For example, the United States suspended some travel from China on January 31, and from Europe March 11, suspended visa services March 18, and closed the Canadian and Mexican borders to non-essential travel on March 23. Although the European response varied by country, the EU began repatriating citizens from China on February 1, set up a response team on March 2, and announced a coordinated response March 13. The WHO special envoy advised countries to act quickly and decisively on March 30.
Appendix Appendix A contains the exact questions. Questions were open-ended and interviewers used pre-coded options to record responses but did not prompt respondents. Therefore, our results are likely an underestimate of true knowledge and risk mitigation practices, and primarily reflect the salience of an individual symptom, risk mitigation mechanism, or way that they had been affected. In the Tanzanian sample, for the first 149 responses, individuals were asked in sequence about whether they had been to a particular location in the past 6 days. However, due to concerns of placing too high a burden on respondent time, the question was no longer promoted and instead simply open-ended for the rest of that country and the other countries. We include a control for the mode of question administration, and findings are robust to excluding those early respondents (not shown). In Sierra Leone, the question about how respondents were affected by the coronavirus was inadvertently omitted. However, other questions about respondent well-being were asked, and so we harmonize responses for those topics. All estimates include country fixed effects, and results are robust to excluding the Sierra Leonean sample.
Whether respondents were given choices or responded freely changed during the course of the survey in Tanzania. We control for this change in all specifications.
Since enumerator knowledege may affect recorded responses, we re-estimate our primary analyses with enumerator fixed effects in lieu of country fixed effects (Kerwin and Reynoso, 2020). Results are robust to this change (not shown).
As our samples have more education than average in these countries, our respondents might be more knowledgeable than average. In subsequent tables we show that education is positively related to symptoms and transmission knowledge but not protective measures taken.
Based on studies of other health knowledge, this Covid-19 knowledge is likely higher than other health knowledge in similar contexts. For example, malaria is a common disease in Uganda, yet the average score on a standard set of questions about malaria transmission was only 74% (Fitzpatrick 2020). Similarly, Chan and Tsai (2018); Fitzpatrick (2020) estimate only 35–41% of adults in sub-Saharan Africa have comprehensive HIV knowledge. Our respondents in Malawi were generally knowledgeable about health. In our sample, the average Malawian respondent answered 90 percent of HIV knowledge questions correctly. Interestingly, we find no statistically significant relationship between the knowledge of Covid-19 symptoms or transmission mechanisms and either a count of correctly answering questions about HIV or an index of HIV knowledge (see Appendix Table B2). At least in Malawi, Covid-19 knowledge is not concentrated among individuals who are already more informed about health or disease risk more broadly.
In Tanzania, houses of worship remained open. In Malawi, gatherings of more than 100 people were outlawed, including at households of worship. By contrast, in Sierra Leone and Ghana houses of worship were ordered closed.
These questions were not asked in Sierra Leone.
Despite small sample sizes when analyzed by country, in each country symptom and transmission knowledge were positively related to the number of protective measures (see Appendix Table B6). Knowing an additional symptom was associated with an increase of 0.09 (Ghana) to 0.33 (Malawi) additional protective measures and knowing an additional transmission mechanisms with an increase of 0.20 (Malawi) to 0.35 (Tanzania) additional protective measures.
Appendix Table B8 disaggregates these results by country.
Our Sierra Leone and Tanzania samples both have a weak positive trend in mask wearing.
Appendix A. Survey Questions
Below are the list of questions asked of respondents in each country. Questions were translated into local languages as appropriate.
-
1.Consider your household to be individuals who normally live and eat their meals together. In the past 7 days, have you or any household member come within 2 m of other individuals who are not part of your household?
-
(a)Yes
-
(b)No (if no, skip to Question 3)
-
(a)
-
2.Where have you or any other household members come within 2 s of other individual(s) not in your household?Do not prompt, tick all that respondent mentions.
-
(a)Market or a trading center or mall or supermarket
-
(b)Home of a friend or non-household family member
-
(c)Food distribution location
-
(d)Ate/drank at a Restaurant/bar/shop/hotel
-
(e)Getting takeaway from a restaurant/bar/shop/hotel
-
(f)During employment activities, e.g. working near someone.
-
(g)Religious or other worship services (including bible study and choir)
-
(h)Wedding or funeral or anniversary
-
(i)Non-religious community, political or other group meeting
-
(j)Minibus (Trotro) or Taxi
-
(k)Okada (Motor cycle taxi)
-
(l)Communal toilet or bath
-
(m)Other (Specify)
-
(a)
-
3.In the past 7 days, have the children or youth in your household played or socialized in close physical proximity with children outside of your household?
-
(a)I do not have any children or youth in my household.
-
(b)Yes
-
(c)No
-
(a)
-
4.Can you tell me what you know about the symptoms of COVID? Do not prompt, tick all that respondent mentions.
-
(a)I don’ t know any symptoms (if select this cannot select anything else)
-
(b)Coughing
-
(c)Fever
-
(d)Sneezing
-
(e)Fatigue
-
(f)Difficulty breathing
-
(g)Loss of smell
-
(h)Loss of taste
-
(i)Headache
-
(j)Sore Throat
-
(k)Other (Specify)
-
(a)
-
5.Can you tell me what you know about how COVID is transmitted?Do not prompt, tick all that respondent mentions.
-
(a)I do not know how it’ s transmitted (if select this cannot select anything else)
-
(b)From other people coughing/breathing common air/inhaling germs
-
(c)Shaking hands/touching other people
-
(d)Touching contaminated surfaces
-
(e)Even people who do not show symptoms might be infected
-
(f)Even people who do not show symptoms might be contagious
-
(g)Eating bad/spoiled/unripe food
-
(h)Witchcraft
-
(i)It only/primarily affects older people
-
(j)It only/primarily affects younger people
-
(k)Other(specify)
-
(a)
-
6.What are you doing to prevent an infection of the Covid-19? Do not prompt, tick all that respondent mentions.
-
(a)Nothing (if select this cannot select anything else)
-
(b)Increased hand washing
-
(c)Wearing a nose/face mask
-
(d)Not shaking hands
-
(e)Stay distanced from others
-
(f)Not eating unwashed food
-
(g)Not eating from a shared plate or drinking from shared cup
-
(h)Drinking clean water
-
(i)Praying
-
(j)Preventative medicine (traditional or otherwise)
-
(k)Eating more healthfully
-
(l)Using hand sanitizer
-
(m)Other (specify)
-
(a)
-
7.How has Covid and any related restrictions affected you? Do not prompt, tick all that respondent mentions.
-
(a)No effect (if select this cannot select anything else)
-
(b)I am infected/believe to be infected
-
(c)Someone in my household is infected/believe to be infected
-
(d)Someone in my household died
-
(e)I am stressed, depressed, worried, and/or anxious
-
(f)Children home from school
-
(g)A reduction in household income or resources
-
(h)A reduction in food availability
-
(i)The size of my household has increased, e.g. migrants have returned or other kin now reside together
-
(j)The size of my household has decreased, e.g. kin have left to live elsewhere
-
(k)Spending more time on the phone/internet
-
(l)Receiving more monetary transfers
-
(m)Receiving fewer monetary transfers
-
(n)Sending more monetary transfers
-
(o)Sending fewer monetary transfers
-
(p)Other (specify)
-
(a)
Appendix B. Additional Figures and Tables
Table B1.
Comparison of Study Characteristics to Population Averages.
| (1) | (2) | (3) | (4) | |
|---|---|---|---|---|
| Ghana | Malawi | Sierra Leone | Tanzania | |
| Age (Median) | 20.4 | 17.4 | 18.3 | 17.3 |
| Male | 0.51 | 0.49 | 0.50 | 0.50 |
| Has children | 0.62 | 0.85 | 0.85 | 0.81 |
| Rural | 0.43 | 0.83 | 0.58 | 0.66 |
| No Schooling | 0.16 | 0.11 | 0.41 | 0.13 |
| Some Schooling | 0.16 | 0.61 | 0.13 | 0.62 |
| Secondary or Higher | 0.67 | 0.28 | 0.45 | 0.24 |
Notes: Averages of key variables for each country from other nationally representative surveys. Age: United Nations Population Division. Male: 2019 World Bank Development Indicators, refers to the working age population (15–64). Education/Has Children: from the most recent Demographic and Health Survey for each country, representative of women aged 15–49 in all countries, men aged 15–59 in Ghana, Sierra Leone, and Tanzania, and men aged 15–54 in Malawi. Rural: 2019 World Bank Development Indicators. Education is mutually exclusive but may not sum to 1 due to rounding.
Table B2.
HIV Knowledge is Uncorrelated with Covid-19 Knowledge.
| (1) | (2) | (3) | (4) | (5) | (6) | |
|---|---|---|---|---|---|---|
| -HIV Knowledge Count- | HIV Knowledge PCA Index- | |||||
| # Correct Symptoms Listed | 0.024 | 0.028 | 0.003 | 0.012 | ||
| (0.020) | (0.020) | (0.034) | (0.033) | |||
| # Correct Transmission Mechanisms | -0.010 | -0.021 | -0.042 | -0.046 | ||
| (0.030) | (0.031) | (0.060) | (0.060) | |||
| Age | 0.008 | 0.010 | 0.009 | 0.017 | 0.018 | 0.018 |
| (0.012) | (0.012) | (0.012) | (0.024) | (0.024) | (0.024) | |
| Some Schooling | 0.595 | 0.587 | 0.571 | 1.969 | 1.923 | 1.917 |
| (0.741) | (0.751) | (0.741) | (1.958) | (1.961) | (1.959) | |
| Secondary or Higher | 0.760 | 0.760 | 0.740 | 2.157 | 2.121 | 2.113 |
| (0.740) | (0.750) | (0.740) | (1.956) | (1.959) | (1.957) | |
| Observations | 460 | 460 | 460 | 460 | 460 | 460 |
| R2 | 0.04 | 0.04 | 0.04 | 0.03 | 0.03 | 0.03 |
| Mean Dep. | 2.77 | 2.77 | 2.77 | 0.01 | 0.01 | 0.01 |
Notes: The outcome variable in Columns 1–3 is the count of correct HIV questions answered by the respondent. The outcome variable in Columns 4–6 is a PCA index of the HIV knowledge questions. These HIV questions were asked approximately one year prior to the Covid-19 survey in 2019. Sample size differs from the main analysis because some respondents from the 2019 data collection round could not be definitively matched to respondents from the pandemic data collection rounddue to the difficulty of verifying identities through a phone survey. All regressions include additional controls of age, age-squared, male, urban-rural status, and a set of dummies for educational attainment. Robust standard errors to correct for heteroskedasticity in parenthesis.* p 0:10, ** p 0:05, *** p 0:01
Table B3.
Social Contact Locations By Country.
| Ghana | Malawi | Sierra Leone | Tanzania | Average | PValue of Equality | |
|---|---|---|---|---|---|---|
| (1) | (2) | (3) | (4) | (5) | (6) | |
| Panel A: Contact Variables At Informal Gatherings | ||||||
| Total Informal Contacts | 1.38 | 3.09 | 1.46 | 2.04 | 2.04 | 0.00 |
| Contact at a market | 0.56 | 0.72 | 0.44 | 0.61 | 0.58 | 0.00 |
| Contact in another home | 0.40 | 0.60 | 0.41 | 0.40 | 0.46 | 0.00 |
| Contact on minibus | 0.19 | 0.53 | 0.31 | 0.34 | 0.36 | 0.00 |
| Contact on motorcycle taxi | 0.13 | 0.45 | 0.28 | 0.37 | 0.32 | 0.00 |
| Contact in communal toilet or bath | 0.04 | 0.41 | 0.02 | 0.12 | 0.16 | 0.00 |
| Contact by takeout from bar, restaurant, etc. | 0.06 | 0.36 | 0.00 | 0.10 | 0.14 | 0.00 |
| Panel B: Contact Variables At Formal Gatherings | ||||||
| Total Formal Contacts | 0.21 | 2.31 | 0.24 | 1.35 | 1.09 | 0.00 |
| Contact at work | 0.08 | 0.72 | 0.20 | 0.30 | 0.35 | 0.00 |
| Contact at religious service/activity | 0.02 | 0.54 | 0.00 | 0.5 | 0.28 | 0.00 |
| Contact eating/drinking at bar, restaurant, etc. | 0.09 | 0.61 | 0.03 | 0.18 | 0.24 | 0.00 |
| Contact at wedding, funeral, anniversary, etc. | 0.01 | 0.29 | 0.00 | 0.22 | 0.14 | 0.00 |
| Contact at non-religious meeting | 0.01 | 0.15 | 0.01 | 0.07 | 0.06 | 0.00 |
| Observations | 362 | 563 | 597 | 523 | 2045 | |
Notes: Columns 1–4: Country-level aggregates. Column 5: Overall average. Column 6: the p-value of the joint test of equality of the averages by country. * p 0:10, ** p 0:05, *** p 0:01
Table B4.
Effects of the Pandemic Disaggregated by Reported Stress.
| Did Not Report Stress | Reported Stress | Average | PValue of Equality | |
|---|---|---|---|---|
| (1) | (2) | (3) | (4) | |
| Number of Ways Affected | 0.98 | 2.23 | 1.58 | 0.00*** |
| Reduction in income/resources | 0.53 | 0.54 | 0.54 | 0.18 |
| Children home from school | 0.27 | 0.49 | 0.38 | 0.00*** |
| Self-infected | 0.01 | 0.00 | 0.01 | 0.067* |
| Household infected | 0.07 | 0.01 | 0.04 | 0.00*** |
| Household death | 0.01 | 0.01 | 0.01 | 0.564 |
| Reduction in food | 0.12 | 0.08 | 0.10 | 0.00*** |
| Increase in household size | 0.04 | 0.04 | 0.04 | 0.937 |
| Decrease in household size | 0.01 | 0.02 | 0.02 | 0.966 |
| Increase on phone/internet | 0.01 | 0.02 | 0.07 | 0.621 |
| More monetary transfers | 0.01 | 0.01 | 0.01 | 0.906 |
| Less monetary transfers | 0.06 | 0.00 | 0.03 | 0.869 |
| Sent more transfers | 0.03 | 0.04 | 0.03 | 0.729 |
| Observations | 717 | 681 | 1398 | |
Notes: Columns 1–2: Ways reported affected by pandemic disaggregated by reported stress. Column 3: Average in full sample. Column 4: the p-value of the equality of the average of those affected by stress and those not affected. * p 0:10, ** p 0:05, *** p 0:01
Table B5.
Correlates of Specific Protective Measures Taken.
| (1) | (2) | (3) | (4) | (5) | |
|---|---|---|---|---|---|
| Sanitize Hands | Social Distancing | Wash Hands | Not Shaking Hands | Mask Wearing | |
| # Correct Symptoms Listed | 0.034*** | 0.056*** | 0.019** | 0.077*** | 0.031*** |
| (0.008) | (0.009) | (0.008) | (0.009) | (0.008) | |
| # Correct Transmission Mechanisms | 0.029** | 0.088*** | 0.067*** | 0.158*** | 0.030** |
| (0.012) | (0.014) | (0.012) | (0.014) | (0.013) | |
| Male | -0.028 | 0.061** | 0.016 | 0.011 | 0.034 |
| (0.025) | (0.027) | (0.020) | (0.026) | (0.021) | |
| Age | -0.003 | 0.005 | -0.001 | 0.001 | 0.009** |
| (0.004) | (0.006) | (0.004) | (0.006) | (0.004) | |
| Rural | -0.034 | 0.074** | 0.035 | -0.040 | -0.055** |
| (0.030) | (0.037) | (0.026) | (0.035) | (0.028) | |
| Some Schooling | 0.154* | 0.005 | -0.084 | -0.207* | -0.026 |
| (0.079) | (0.114) | (0.063) | (0.106) | (0.064) | |
| Secondary or Higher | 0.201** | 0.048 | -0.125** | -0.266** | 0.025 |
| (0.080) | (0.115) | (0.063) | (0.107) | (0.065) | |
| Observations | 1991 | 1991 | 1991 | 1991 | 1991 |
| R2 | 0.37 | 0.10 | 0.03 | 0.18 | 0.37 |
| Mean Dep. | 0.33 | 0.66 | 0.84 | 0.44 | 0.49 |
Notes: All regressions include a country fixed effect, age, age-squared, male, urban-rural status, and a set of dummies for educational attainment. Individuals with missing control variables have their value set equal to the mean for their country with a dummy variable to mark the imputation. Robust standard errors to correct for heteroskedasticity in parenthesis.* p 0:10, ** p 0:05, *** p 0:01
Table B6.
Correlates of Protective Measures Taken: Results by Country.
| (1) | (2) | (3) | (4) | |
|---|---|---|---|---|
| Ghana | Malawi | Sierra Leone | Tanzania | |
| # Correct Symptoms Listed | 0.092** | 0.327*** | 0.095*** | 0.150*** |
| (0.044) | (0.047) | (0.033) | (0.036) | |
| # Correct Transmission Mechanisms | 0.230*** | 0.195*** | 0.282*** | 0.349*** |
| (0.081) | (0.069) | (0.056) | (0.049) | |
| Age | -0.099* | 0.004 | 0.029 | -0.015 |
| (0.056) | (0.018) | (0.023) | (0.020) | |
| Male | -0.181 | 0.101 | 0.113 | |
| (0.124) | (0.080) | (0.074) | ||
| Rural | -0.129 | -0.074 | ||
| (0.137) | (0.087) | |||
| Some Schooling | -0.642 | -0.523* | 0.157 | |
| (0.392) | (0.274) | (0.210) | ||
| Secondary or Higher | -0.686* | -0.394 | 0.307 | |
| (0.389) | (0.268) | (0.226) | ||
| Observations | 277 | 491 | 633 | 557 |
| R2 | 0.43 | 0.37 | 0.39 | 0.21 |
| Mean Dep. | 3.29 | 2.10 | 3.29 | 2.33 |
Notes: All regressions include controls for age, age-squared, male, urban-rural status, a set of dummies for educational attainment, and enumerator fixed effects. Individuals with missing control variables have their value set equal to the mean for their country with a dummy variable to mark the imputation. The sample in Malawi is exclusively males in urban areas, and the sample in Sierra Leone is exclusively urban. Robust standard errors to correct for heteroskedasticity in parenthesis. * p 0:10, ** p 0:05, *** p 0:01
Table B7.
Correlates of Contacts at Specific Locations.
| (1) | (2) | (3) | (4) | (5) | |
|---|---|---|---|---|---|
| Market | Work | Other Homes | Public Transport | Ate Restaurant | |
| # Correct Symptoms Listed | 0.003 | -0.003 | 0.014 | 0.008 | -0.005 |
| (0.010) | (0.009) | (0.010) | (0.010) | (0.008) | |
| # Correct Transmission Mechanisms | 0.015 | 0.007 | 0.055*** | 0.046*** | 0.030*** |
| (0.015) | (0.013) | (0.015) | (0.014) | (0.011) | |
| Male | -0.082*** | 0.090*** | 0.048* | 0.025 | 0.080*** |
| (0.028) | (0.022) | (0.028) | (0.025) | (0.016) | |
| Age | -0.013** | 0.015*** | -0.010* | 0.003 | 0.016*** |
| (0.006) | (0.006) | (0.006) | (0.006) | (0.005) | |
| Rural | -0.107*** | 0.070** | 0.027 | -0.281*** | 0.007 |
| (0.037) | (0.033) | (0.037) | (0.033) | (0.027) | |
| Some Schooling | 0.011 | 0.113 | -0.146 | 0.068 | 0.003 |
| (0.103) | (0.095) | (0.108) | (0.085) | (0.053) | |
| Secondary or Higher | -0.024 | 0.102 | -0.130 | 0.091 | 0.029 |
| (0.103) | (0.096) | (0.109) | (0.085) | (0.053) | |
| Observations | 1991 | 1991 | 1991 | 1991 | 1991 |
| R2 | 0.07 | 0.26 | 0.05 | 0.10 | 0.32 |
| Mean Dep. | 0.58 | 0.36 | 0.46 | 0.36 | 0.25 |
Notes: All regressions include controls for age, age-squared, male, urban-rural status, a set of dummies for educational attainment, and enumerator fixed effects. Individuals with missing control variables have their value set equal to the mean for their country with a dummy variable to mark the imputation. Data on enumerator and schooling were not available for 72 respondents in Malawi. Robust standard errors to correct for heteroskedasticity in parenthesis. * p 0:10, ** p 0:05, *** p 0:01
Table B8.
Correlates of Contacts at Specific Locations: Results by Country.
| (1) | (2) | (3) | (4) | |
|---|---|---|---|---|
| Ghana | Malawi | Sierra Leone | Tanzania | |
| # Correct Symptoms Listed | 0.105 | -0.098 | 0.048 | -0.021 |
| (0.090) | (0.092) | (0.032) | (0.079) | |
| # Correct Transmission Mechanisms | -0.026 | 0.265** | 0.200*** | 0.257** |
| (0.114) | (0.125) | (0.054) | (0.115) | |
| #Protective Measures (excluding social distancing) | 0.038 | 0.241** | 0.148*** | 0.314*** |
| (0.092) | (0.105) | (0.037) | (0.100) | |
| Age | 0.005 | 0.017 | -0.027 | 0.023 |
| (0.089) | (0.039) | (0.024) | (0.053) | |
| Male | 0.087 | 0.118 | 0.411** | |
| (0.220) | (0.074) | (0.173) | ||
| Rural | -0.457** | 0.054 | ||
| (0.224) | (0.180) | |||
| Some Schooling | 0.328 | -0.137 | 0.757 | |
| (1.169) | (0.523) | (0.613) | ||
| Secondary or Higher | 0.638 | -0.291 | 0.377 | |
| (1.159) | (0.522) | (0.638) | ||
| Observations | 277 | 562 | 597 | 555 |
| R2 | 0.04 | 0.04 | 0.10 | 0.14 |
| Mean Dep. | 1.61 | 5.47 | 1.72 | 3.18 |
Notes: All regressions include controls for age, age-squared, male, urban-rural status, a set of dummies for educational attainment, and enumerator fixed effects. Individuals with missing control variables have their value set equal to the mean for their country with a dummy variable to mark the imputation. Enumerator data were not available for 72 respondents in Malawi. Robust standard errors to correct for heteroskedasticity in parenthesis. * p 0:10, ** p 0:05, *** p 0:01
References
- Africa Center for Strategic Studies, 2020. African Adaptations to the COVID-19 Response.
- Allen J., Mahumane A., Riddell J., Rosenblat T., Yang D., Yu H. University of Michigan Working Paper. 2021. Correcting Perceived Social Distancing Norms to Combat Covid-19. [Google Scholar]
- Alsan M., Braghieri L., Eichmeyer S., Kim M.J., Stantcheva S., Yang D.Y. NBER Working Paper. 2020. Civil Liberties in Times of Crisis. [Google Scholar]
- Alsan M., Stantcheva S., Yang D., Cutler D. Disparities in coronavirus 2019 reported incidence, knowledge, and behavior among US adults. JAMA Netw. Open. 2020;3(6) doi: 10.1001/jamanetworkopen.2020.12403. [DOI] [PMC free article] [PubMed] [Google Scholar]; e2012403–e2012403.
- Amare M., Abay K.A., Tiberti L., Chamberlin J. Impacts of Covid-19 on food security: panel data evidence from Nigeria. Int. Food Policy Res. Inst. 2020;1956 doi: 10.1016/j.foodpol.2021.102099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asiamah N., Opuni F.F., Mends-Brew E., Mensah S.W., Mensah H.K., Quansah F. Short-term changes in behaviors resulting from Covid-19-related social isolation and their influences on mental health. Community Ment. Health J. 2020 doi: 10.1007/s10597-020-00722-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badoe E. A critical review of child abuse and its management in africa. Afr. J. Emerg. Med. 2017;7:S32–S35. doi: 10.1016/j.afjem.2017.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beg, S., Fitzpatrick, A., Lucas, A., 2020. Successful interventions at scale: the importance of managers.
- Cairncross S., Shordt K., Zacharia S., Govindan B.K. What causes sustainable changes in hygiene behaviour? A cross-sectional study from Kerala, India. Soc. Sci. Med. 2005;61(10):2212–2220. doi: 10.1016/j.socscimed.2005.04.019. [DOI] [PubMed] [Google Scholar]
- Castex G., Dechter E., Lorca M. Covid-19: cross-country heterogeneity in effectiveness of non-pharmaceutical interventions. Covid Econ. 2020;14:175–199. [Google Scholar]
- Castex G., Dechter E., Lorca M. Covid-19: the impact of social distancing policies, cross-country analysis. Econ. Disasters Clim. Change. 2020:1–25. doi: 10.1007/s41885-020-00076-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan B., Tsai A. Hiv knowledge trends during an era of rapid antiretroviral therapy scale-up: an analysis of 33 sub-saharan african countries. J. Int. AIDS Soc. 2018;21(7):e25169. doi: 10.1002/jia2.25169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiplunkar, G., Das, S., 2020. Political institutions and policy responses during a crisis. Available at SSRN 3629397. [DOI] [PMC free article] [PubMed]
- Cowling B.J., Aiello A.E. Public health measures to slow community spread of coronavirus disease 2019. J. Infect. Dis. 2020;221(11):1749–1751. doi: 10.1093/infdis/jiaa123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derksen, L., Kerwin, J., Ordaz Reynoso, N., Sterck, O., 2020. Appointments versus commitments: overcoming self-control problems in preventive health.
- Dupas P. Do teenagers respond to HIV risk information? Evidence from a field experiment in kenya. Am. Econ. J. 2011;3(1):1–34. [Google Scholar]
- Dupas P. Health behavior in developing countries. Annu. Rev. Econ. 2011;3(1):425–449. [Google Scholar]
- Eikenberry S.E., Mancuso M., Iboi E., Phan T., Eikenberry K., Kuang Y., Kostelich E., Gumel A.B. To mask or not to mask: modeling the potential for face mask use by the general public to curtail the Covid-19 pandemic. Infect. Dis. Model. 2020 doi: 10.1016/j.idm.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erokhin V., Gao T. Impacts of Covid-19 on trade and economic aspects of food security: evidence from 45 developing countries. Int. J. Environ. Res. Public Health. 2020;17(16):5775. doi: 10.3390/ijerph17165775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick A. When patients diagnose: the effect of patient beliefs and information on provider behavior. Econ. Dev. Cult. Change. 2020;69(1):51–72. [Google Scholar]
- Gandhi M., Beyrer C., Goosby E. Masks do more than protect others during Covid-19: reducing the inoculum of SARS-COV-2 to protect the wearer. J. Gen. Intern. Med. 2020;35(10):3063–3066. doi: 10.1007/s11606-020-06067-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geldsetzer P. Knowledge and perceptions of Covid-19 among the general public in the united states and the United Kingdom: a cross-sectional online survey. Ann. Intern. Med. 2020 doi: 10.7326/M20-0912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg P.K., Reed T. The effects of the coronavirus pandemic in emerging market and developing economies an optimistic preliminary account. Brook. Pap. Econ. Act. 2020;6:1. [Google Scholar]
- GRID3, 2020. Sierra leone is fighting smart against Covid-19. Blog Post.
- Groarke J.M., Berry E., Graham-Wisener L., McKenna-Plumley P.E., McGlinchey E., Armour C. Loneliness in the UK during the Covid-19 pandemic: cross-sectional results from the covid-19 psychological wellbeing study. PLoS One. 2020;15(9):e0239698. doi: 10.1371/journal.pone.0239698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haushofer J., Metcalf C.J.E. Which interventions work best in a pandemic? Science. 2020;368(6495):1063–1065. doi: 10.1126/science.abb6144. [DOI] [PubMed] [Google Scholar]
- Jain, R., Budlender, J., Zizzamia, R., Bassier, I., 2020. The labor market and poverty impacts of Covid-19 in South Africa.
- Jalan J., Somanathan E. The importance of being informed: experimental evidence on demand for environmental quality. J. Dev. Econ. 2008;87(1):14–28. [Google Scholar]
- Josephson, A., Kilic, T., Michler, J. D., 2020. Socioeconomic impacts of Covid-19 in four African countries. [DOI] [PubMed]
- Kao K., Lust E., Dulani B., Ferree K.E., Harris A.S., Metheney E. The abcs of Covid-19 prevention in malawi: authority, benefits, and costs of compliance. World Dev. 2020;137:105167. doi: 10.1016/j.worlddev.2020.105167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karing, A., 2020a. Operation of and demand for public transport during Covid-19: Descriptive evidence from sierra leone.
- Karing, A., 2020b. Operation of and demand for public transport during Covid-19: Descriptive evidence from sierra leone.
- Kerwin, J. T., 2020. The effect of HIV infection risk beliefs on sexual behavior: scared straight or scared to death?.
- Kerwin J.T., Reynoso N.O. You know what i know: interviewer knowledge effects in subjective expectation elicitation. Demography. 2020 doi: 10.1215/00703370-8932274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowal M., Coll-Martín T., Ikizer G., Rasmussen J., Eichel K., Studzińska A., Koszałkowska K., Karwowski M., Najmussaqib A., Pankowski D. Who is the most stressed during the Covid-19 pandemic? Data from 26 countries and areas. Appl. Psychol. 2020;12(4):946–966. doi: 10.1111/aphw.12234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krekel C., Swanke S., De Neve J.-E., Fancourt D. IZA Discussion Paper. 2020. Are Happier People More Compliant? Global Evidence From Three Large-scale Surveys During Covid-19 Lockdowns. [Google Scholar]
- Kremer M., Leino J., Miguel E., Zwane A.P. Spring cleaning: a randomized evaluation of source water quality improvement. Q. J. Econ. 2007;4(2):09–30. [Google Scholar]
- Liu Y., Eggo R.M., Kucharski A.J. Secondary attack rate and superspreading events for SARS-COV-2. Lancet. 2020;395(10227):e47. doi: 10.1016/S0140-6736(20)30462-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo N.C., Lowe A., Bendavid E. Abstinence funding was not associated with reductions in HIV risk behavior in sub-saharan Africa. Health Aff. 2016;35(5):856–863. doi: 10.1377/hlthaff.2015.0828. [DOI] [PubMed] [Google Scholar]
- Loades M.E., Chatburn E., Higson-Sweeney N., Reynolds S., Shafran R., Brigden A., Linney C., McManus M.N., Borwick C., Crawley E. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of Covid-19. J. Am. Acad. Child Adolesc. Psychiatry. 2020 doi: 10.1016/j.jaac.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lone S.A., Ahmad A. Covid-19 pandemic–an african perspective. Emerg. Microbes Infect. 2020:1–28. doi: 10.1080/22221751.2020.1775132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas A.M. Malaria eradication and educational attainment: evidence from paraguay and sri lanka. Am. Econ. J. 2010;2(2):46–71. doi: 10.1257/app.2.2.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas A.M., Wilson N.L. Can at-scale drug provision improve the health of the targeted in sub-saharan Africa? Am. J. Health Econ. 2018;4(3):358–382. [Google Scholar]
- Lyu W., Wehby G.L. Community use of face masks and Covid-19: evidence from a natural experiment of state mandates in the us: study examines impact on Covid-19 growth rates associated with state government mandates requiring face mask use in public. Health Aff. 2020;39(8):1419–1425. doi: 10.1377/hlthaff.2020.00818. [DOI] [PubMed] [Google Scholar]
- Madajewicz M., Pfaff A., van Geen A., Graziano J., Hussein I., Momotaj H., Sylvi R., Ahsan H. Can information alone change behavior? Response to arsenic contamination of groundwater in Bangladesh. J. Dev. Econ. 2007;84(2):731–754. [Google Scholar]
- Mahmud, M., Riley, E., 2020. Household response to an extreme shock: evidence on the immediate impact of the Covid-19 lockdown on economic outcomes and well-being in rural Uganda. [DOI] [PMC free article] [PubMed]
- Maire J. Peterson Institute for International Economics blog post; 2020. Why has Covid-19 Lockdown Compliance Varied Between High- and Low-income Countries? [Google Scholar]
- Marois G., Muttarak R., Scherbov S. Assessing the potential impact of Covid-19 on life expectancy. PLoS One. 2020;15(9):e0238678. doi: 10.1371/journal.pone.0238678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masina L. VOANews; 2020. Malawi Orders Political Opposition to Halt Coronavirus Education Campaigns. [Google Scholar]
- Meinck F., Cluver L.D., Boyes M.E., Mhlongo E.L. Risk and protective factors for physical and sexual abuse of children and adolescents in Africa: a review and implications for practice. Trauma Violence Abuse. 2015;16(1):81–107. doi: 10.1177/1524838014523336. [DOI] [PubMed] [Google Scholar]
- Murray E.J. Epidemiology’s time of need: Covid-19 calls for epidemic-related economics. J. Econ. Perspect. 2020;34(4):105–120. [Google Scholar]
- Osseni I.A. Covid-19 pandemic in sub-saharan Africa: preparedness, response, and hidden potentials. Trop. Med. Health. 2020;48(1):1–3. doi: 10.1186/s41182-020-00240-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oster E. Hiv and sexual behavior change: why not Africa? J. Health Econ. 2012;31(1):35–49. doi: 10.1016/j.jhealeco.2011.12.006. [DOI] [PubMed] [Google Scholar]
- Peltzman S. The effects of automobile safety regulation. J. Polit. Econ. 1975;83(4):677–725. [Google Scholar]
- Rannan-Eliya R.P., Wijemunige N., Gunawardana J., Amarasinghe S.N., Sivagnanam I., Fonseka S., Kapuge Y., Sigera C.P. Increased intensity of PCR testing reduced Covid-19 transmission within countries during the first pandemic wave. Health Aff. 2020;0(0) doi: 10.1377/hlthaff.2020.01409. [DOI] [PubMed] [Google Scholar]; PMID: 33264048.
- Squires M. Working paper. 2020. Kinship Taxation as an Impediment to Growth: Experimental Evidence From Kenyan and Tanzanian Microenterprises. [Google Scholar]
- UNDP Africa, 2020. Beating covid-19 with solidarity. Medium.com.
- United Nations Economic Commission for Africa, 2020. Covid-19 in Africa: protecting lives and economies.
- Varma P., Junge M., Meaklim H., Jackson M.L. Younger people are more vulnerable to stress, anxiety and depression during Covid-19 pandemic: a global cross-sectional survey. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2021;109:110236. doi: 10.1016/j.pnpbp.2020.110236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Bank, 2020. World development indicators.
- World Health Organization . Global health observatory (GHO) data. 2020. Hospital Beds (per 10,000 population) WHO; Geneva: 2016. [Google Scholar]
- Zheng Q., Jones F.K., Leavitt S.V., Ung L., Labrique A.B., Peters D.H., Lee E.C., Azman A.S. Hit-Covid, a global database tracking public health interventions to Covid-19. Sci. Data. 2020;7(1):1–8. doi: 10.1038/s41597-020-00610-2. [DOI] [PMC free article] [PubMed] [Google Scholar]