Abstract
Background
Trauma-induced coagulopathy in patients with traumatic brain injury (TBI) is associated with high rates of complications, unfavourable outcomes and mortality. The mechanism of the development of TBI-associated coagulopathy is poorly understood.
Methods
This analysis, embedded in the prospective, multi-centred, observational Collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury (CENTER-TBI) study, aimed to characterise the coagulopathy of TBI. Emphasis was placed on the acute phase following TBI, primary on subgroups of patients with abnormal coagulation profile within 4 h of admission, and the impact of pre-injury anticoagulant and/or antiplatelet therapy. In order to minimise confounding factors, patients with isolated TBI (iTBI) (n = 598) were selected for this analysis.
Results
Haemostatic disorders were observed in approximately 20% of iTBI patients. In a subgroup analysis, patients with pre-injury anticoagulant and/or antiplatelet therapy had a twice exacerbated coagulation profile as likely as those without premedication. This was in turn associated with increased rates of mortality and unfavourable outcome post-injury. A multivariate analysis of iTBI patients without pre-injury anticoagulant therapy identified several independent risk factors for coagulopathy which were present at hospital admission. Glasgow Coma Scale (GCS) less than or equal to 8, base excess (BE) less than or equal to − 6, hypothermia and hypotension increased risk significantly.
Conclusion
Consideration of these factors enables early prediction and risk stratification of acute coagulopathy after TBI, thus guiding clinical management.
Keywords: CENTER-TBI, Traumatic brain injury, Coagulopathy, Risk factors
Introduction
Traumatic brain injury (TBI) remains a leading cause of death and disability worldwide [1]. The initial insult often results in disruptions of the cerebral vasculature and pathological alterations of the blood–brain barrier (BBB) which may evolve into haemorrhagic lesions. In addition, TBI-associated factors may disturb the body’s haemocoagulative capacity and alter the delicate balance between bleeding and thrombus formation leading to a substantial exacerbation of the initial injury sustained [2–5]. Recent evidence suggests that the acute phase after TBI is rather characterised by dysfunction of the coagulation cascade and hyperfibrinolysis, both of which likely contribute to haemorrhagic progression. This may then be followed by platelet dysfunction and decreased platelet count while the clinical implication of these alterations remains unclear. At later stages, a poorly defined prothrombotic state emerges, partly due to fibrinolysis shutdown and hyperactive platelets [6–8]. Haemostatic alterations, in particular those during the acute phase after TBI, have been associated with higher mortality and more unfavourable outcome than in non-coagulopathic TBI patients [2, 4, 9–11].
The present study aimed to further characterise the alterations to the haemostatic system occurring in the context of isolated TBI (iTBI) based upon data collected into the central database (INCF Neurobot tool version 2.0 (INCF, Stockholm, Sweden) of the prospective, multi-centred, observational Collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury (CENTER-TBI) cohort study. Particular interest was given to the impact of pre-injury anticoagulant and/or antiplatelet therapy. Risk stratification was performed to identify independent predictors indicating coagulopathy after iTBI.
Methods
Study Population
The present study was an embedded study to the longitudinal, observational CENTER-TBI study, which recruited patients from 60 selected centres across Europe and Israel between December 2014 and December 2017 [12]. A total of 4509 patients with a clinical diagnosis of TBI were included in the CENTER-TBI core database. Inclusion criteria were a clinical diagnosis of TBI, indication for CT scanning, presentation to study centre within 24 h of injury, and informed consent obtained according to local and national requirements [12]. Participants were excluded if they had any severe pre-existing neurological disorder that could have confounded outcome assessments. As part of the CENTER-TBI core study, the present analysis was performed in accordance with all relevant local and European laws. Informed consent, including the approval to use data for research purposes, was obtained from each subject according to local ethics and regulations.
Patients with extracranial injuries, defined as AISExtracranial > 0, and those missing critical data points were excluded a priori. We included patients for whom data reporting conventional coagulation parameters within 4 h following iTBI were available. This population included subgroups that developed laboratory abnormalities and those with pre-injury anticoagulant and/or antiplatelet therapy.
Data Collection
The cohort included patients with iTBI who were characterised with respect to the presence of haemostatic abnormalities based upon conventional coagulation parameters within 4 h of injury. The prospectively recorded parameters in scope of the CENTER-TBI core study that were considered for analysis comprised demographics, injury characteristics, medical history, medical presentation in the emergency department (ED), admission laboratory values and pre-injury anticoagulant and/or antiplatelet therapy. Follow-up data on functional outcome, including mortality and Glasgow Outcome Score-Extended (GOS-E), were obtained 6-month post-injury. A GOS-E between 1 and 4 (dead, vegetative state, low severe and upper severe disability) was considered unfavourable.
The primary outcome as the presence or absence of abnormal coagulation profile was defined by conventional coagulation parameters obtained within 4 h of the injury. The following parameters were considered for diagnosing an abnormal coagulation profile: International Normalised Ratio (INR) > 1.2 or activated partial thromboplastin time (aPTT) > 35 s or fibrinogen < 150 mg/dL or platelet count < 100 × 103/nL. All relevant data for further analysis were extracted from the INCF Neurobot tool version 2.0 (INCF, Stockholm, Sweden).
Statistical Analysis
For the descriptive analysis of iTBI patients with and without pre-injury anticoagulant and/or antiplatelet therapy, metric data are presented as median and interquartile range (IQR). Categorical data are presented in percentage. Differences were tested using the Mann–Whitney U test and Chi-squared (Chi2) test, respectively. Nonparametric Kruskal–Wallis test was performed to compare the standard coagulation test in relation to injury severity (AISBrain) in iTBI. A p value < 0.05 was considered statistically significant.
In a univariate analysis, potential predictors for an abnormal coagulation profile were identified via Chi2 test. A logistic regression analysis (multivariate analysis) with coagulopathy as dependent variable was performed to evaluate independent risk factors associated with acute coagulopathy in iTBI. Analysis of potential predictors and independent risk factors of iTBI patients with pre-injury anticoagulant and/or antiplatelet therapy was not feasible due to the low number of cases. Some predictors were discriminated as independent risk factors (e.g. age ≥ 75, sex, neuroworsening) as no differences were detected. The predictor “arrival haemoglobin” was excluded due to low prevalence. The results are presented as odds ratio (OR) with 95% confidence interval (Cl95) and regression coefficient. Statistical analyses were performed using SPSS statistics version 25 for Windows (IBM Corp., Armonk, NY, USA) and GraphPadPrism version 7.00 (GraphPad Software, La Jolla California, USA).
Results
Cohort Characteristics
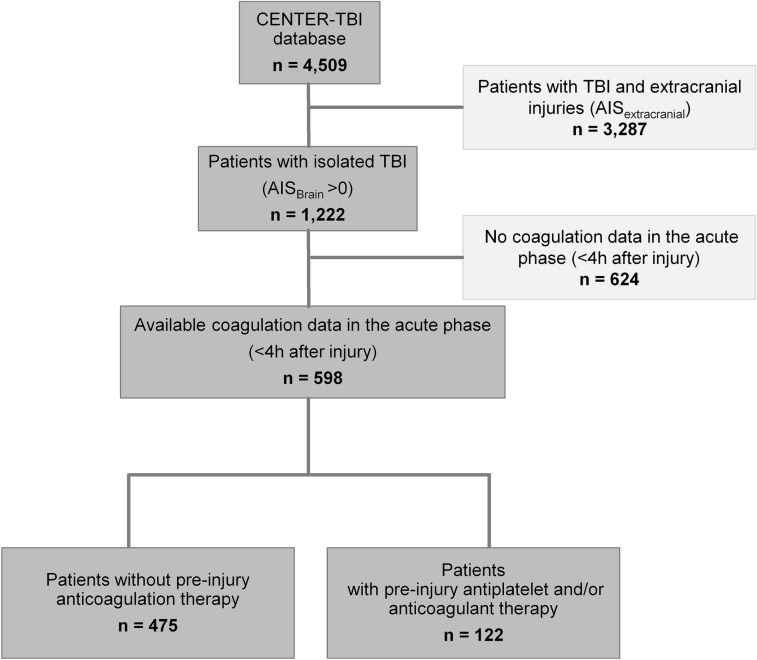
From the 4509 patients included into the CENTER-TBI core study database, 3287 had to be excluded for co-existing extracranial injuries and 624 for missing data (Fig. 1). Thus, 598 patients with iTBI were included in the present analysis. Approximately one-fifth of the cohort was assigned to the group of elderly patients (≥ 75 years, Table 1). Almost all patients (98.7%, data not shown) had sustained a blunt trauma mechanism resulting from various injury patterns, with ground-level falls being the most common cause of injury (28.3%, data not shown). The majority of the injuries sustained were severe (AISBrain ≥ 3, 85%, Table 1) and closed head injuries (93.5%, Table 1). Computed tomography (CT) scans performed immediately after emergency department (ED) admission revealed the following most frequent intracranial pathologies: (1) subarachnoid haemorrhage (52%), (2) subdural haematoma (46.4%), (3) midline shift (24.9%), (4) extradural haematoma (16.5%), (5) basal cistern compression (13.5%), (6) depressed skull fracture (13.2%) and (7) diffuse axonal injury (9.2%) (data not shown).
Fig. 1.
Schematic overview of CENTER-TBI cohort with inclusion and exclusion process for the present subgroup
Table 1.
Characteristics of patients with isolated traumatic brain injury < 4 h following injury (n = 598)
| iTBI patients n = 598 | |
|---|---|
| Demographics | |
| Age, years; median [IQR] | 52 [30–69] |
| Age ≥ 75; n [%] | 106 [17.7] |
| Male gender; n [%] | 415 [69.4] |
| Injury characteristics | |
| Closed TBI; n [%] | 559 [93.5] |
| AISBrain 2; n [%] | 71 [11.9] |
| AISBrain 3; n [%] | 205 [34.3] |
| AISBrain 4; n [%] | 158 [26.4] |
| AISBrain 5; n [%] | 147 [24.6] |
| AISBrain 6; n [%] | 17 [2.8] |
| Medical presentation at admission (ED) | |
| GCS; median [IQR] | 14 [10–15] |
| SBP; mmHg; median [IQR] | 138 [121–156] |
| Heart rate; bpm; median [IQR] | 80.0 [70.5–95.0] |
| Temperature; °C; median [IQR] | 36.2 [35.8–36.7] |
| Received emergency surgical intervention; n [%] | 119 [19.9] |
| Coagulation status, tests and medications | |
| Coagulopathy; n [%] | 117 [19.6] |
| Haemoglobin; g/dl; median [IQR] | 13.7 [12.6–14.7] |
| INR; median [IQR] | 1.04 [1.00–1.15] |
| aPTT; seconds; median [IQR] | 28.2 [25.1–32.4] |
| Platelets;/nl; median [IQR] | 224 [183–267.5] |
| Fibrinogen; mg/dl; median [IQR] | 274.5 [230–320] |
| Pre-injury antiplatelet/anticoagulant medication; n [%] | 122 [20.4] |
| Outcomes | |
| Death [overall]; n [%] | 98 [16.4] |
| GOS-E [6 months—derived]; median [IQR] | 7 [3–8] |
AIS Abbreviated Injury Scale, aPTT activated partial thromboplastin time, ED Emergency department, GCS Glasgow Coma Scale, GOS-E Glasgow Outcome Score-Extended, INR International Normalized Ratio, SBP Systolic blood pressure
Haemostatic alterations based upon conventional coagulation parameters within 4 h after injury were present in 19.6% of included iTBI patients (n = 117/598, Table 1). In addition, for one in five patients pre-injury anticoagulant and/or antiplatelet therapy was documented (Table 1). Ninety-eight iTBI patients (16.4%, Table 1) died while the median outcome in surviving patients at 6 months after iTBI was favourable (Table 1).
Subgroup Analysis of Patients with Pre-injury Antiplatelet and/or Anticoagulant Therapy
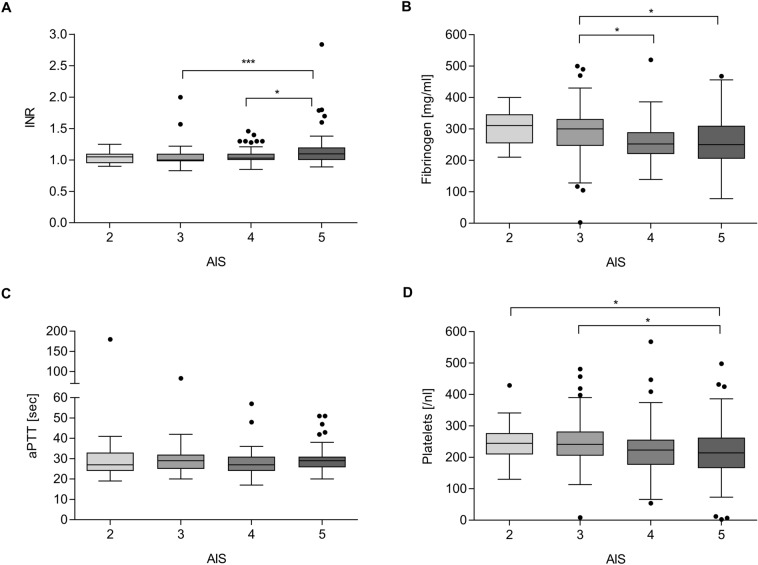
Patients with pre-injury anticoagulant and/or antiplatelet therapy were significantly older than those without. The proportion of patients ≥ 75 years of age comprised more than half in the group of patients on pre-injury anticoagulant and/or antiplatelet therapy (Table 2). A greater proportion of patients with pre-injury anticoagulant and/or antiplatelet medication had an untreatable TBI defined as AISBrain = 6. Coagulopathy by conventional coagulation parameters was diagnosed twice as frequently in patients on pre-injury anticoagulant and/or antiplatelet therapy (Table 2). Conventional coagulation parameters such as INR and aPTT were significantly deteriorated and platelet counts trended to decrease among patients with pre-injury anticoagulation and/or antiplatelet therapy (Table 2). In those patients without pre-injury anticoagulant therapy, conventional coagulation parameters significantly deteriorated with increasing severity of brain injury; a higher AISBrain correlated with higher INR, lower fibrinogen levels and lower platelet counts (Fig. 2). Patients with iTBI and on pre-injury anticoagulant and/or antiplatelet therapy had threefold higher mortality and higher frequency of unfavourable 6-month outcomes (GOS-E 1–4) compared to those without pre-injury anticoagulant and/or antiplatelet therapy (51.9% vs. 23.5%) (Table 2, Fig. 3). Notably, a higher percentage of patients with pre-injury intake of vitamin K antagonists had an abnormal coagulation profile after iTBI than patients on other pre-injury anticoagulant or antiplatelet therapy (Table 3).
Table 2.
Characteristics of iTBI patients with and without pre-injury anticoagulation therapy (n = 598)
| iTBI patients without pre-injury antiplatelet and/or anticoagulant therapy n = 475 | iTBI patients with pre-injury antiplatelet and/or anticoagulant therapy n = 122 | p value | |
|---|---|---|---|
| Demographics | |||
| Age; years; median [IQR], | 44 [25–61] | 75 [68–81] | < 0.001 |
| Age ≥ 75; n [%] | 42 [8.8] | 64 [52.5] | < 0.001 |
| Male gender; n [%] | 333 [70.1] | 82 [67.2] | 0.536 |
| Injury characteristics | |||
| Closed TBI; n [%] | 443 [93.2] | 115 [94.2] | 0.690 |
| AISBrain 2; n [%] | 55 [11.5] | 16 [13.1] | 0.640 |
| AISBrain 3; n [%] | 164 [34.5] | 41 [33.6] | 0.849 |
| AISBrain 4; n [%] | 130 [27.4] | 28 [23.0] | 0.324 |
| AISBrain 5; n [%] | 118 [24.8] | 28 [23.0] | 0.665 |
| AISBrain 6; n [%] | 8 [1.7] | 9 [7.4] | 0.001 |
| Medical presentation at admission (ED) | |||
| GCS; median [IQR] | 14 [11–15] | 14 [9–15] | 0.747 |
| SBP; mmHg; median [IQR] | 135 [120–150] | 150 [132.5–169.2] | < 0.001 |
| Heart rate; bpm; median [IQR] | 80 [72–95] | 80 [67.8–92.3] | 0.368 |
| Temperature; °C; median [IQR] | 36.2 [35.8–36.7] | 36.3 [35.8–36.7] | 0.581 |
| Received emergency surgical intervention; n [%] | 97 [20.4] | 21 [17.2] | 0.427 |
| Coagulopathy, standard laboratory | |||
| Coagulopathy; n [%] | 75 [15.8] | 42 [34.4] | < 0.001 |
| Haemoglobin; g/dl; median [IQR] | 13.9 [12.7–14.8] | 13.7 [12.7–14.9] | 0.993 |
| INR; median [IQR] | 1.03 [1.0–1.1] | 1.1 [1.0–2.48] | < 0.001 |
| aPTT; seconds; median [IQR] | 28.0 [25.0–32.0] | 29.2 [26.0–35.0] | 0.007 |
| Platelets;/nl; median [IQR] | 226 [183–272] | 214 [185–254] | 0.052 |
| Fibrinogen; mg/dl; median [IQR] | 270 [230–316.5] | 304 [251.7–380] | 0.018 |
| Outcomes | |||
| Death [overall]; n [%] | 55 [11.6] | 43 [35.2] | < 0.001 |
| GOS-E [6 months—derived]; median [IQR] | 7 [5–8] | 4 [1–8] | < 0.001 |
Data on the presence of pre-injury anticoagulation therapy were missing in one case
AIS Abbreviated Injury Scale, aPTT activated partial thromboplastin time, ED Emergency department, GCS Glasgow Coma Scale, GOS-E Glasgow Outcome Score-Extended, INR International Normalized Ratio, SBP Systolic blood pressure
Fig. 2.
Conventional coagulation parameters INR (a), fibrinogen level (b) aPTT (c) and platelet count (d) in relation to injury severity (AISBrain) of iTBI patients (n = 475). One patient with AISBrain = 6 was excluded from the analysis. Statistically significant differences are marked with asterisks (*p < 0.05, **p < 0.001, ***p < 0.0001)
Fig. 3.
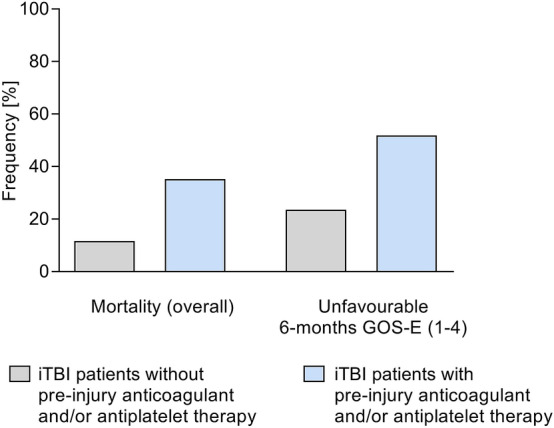
Incidence of mortality and unfavourable Glasgow Outcome Score-Extended (GOS-E) (1–4) 6-month post-injury in iTBI patients with no pre-injury anticoagulation therapy (n = 475) versus patients with pre-injury anticoagulation therapy (n = 122)
Table 3.
Overview of pre-injury anticoagulant and/or antiplatelet therapy in iTBI patients (n = 122)
| iTBI patients with pre-injury antiplatelet and/or anticoagulant therapy n = 122 | Coagulopathy n; [%] | |
|---|---|---|
| Anticoagulants | ||
| Vitamin K antagonists | 37 | 31 [84] |
| Heparin | 2 | 1 [50] |
| Direct oral anticoagulants (DOACs) | 12 | 2 [17] |
| Other anticoagulants | 4 | 1 [25] |
| Platelet inhibitors | ||
| ASS | 43 | 4 [9] |
| Other platelet inhibitors* | 23 | 3 [13] |
Anticoagulants were defined as Vitamin K antagonist (Coumarin derivates Coumadin or Warfarin), direct oral anticoagulants (Factor Xa inhibitor (e.g. Xarelto, Rivaroxaban), direct thrombin inhibitors (e.g. Dabigatran) and antithrombin protein inhibitor (e.g. ATryn). Platelet inhibitors mainly included acetylsalicylic acid (ASS). Patient specified with “Other” received platelet aggregation inhibitor such as Clopidogrel or Parasugrel. Data about specific pre-injury antiplatelet and/or anticoagulant therapy were missing for one case
*Patients with dual platelet inhibitor therapy
Risk Factors for Coagulopathy of Patients Without Pre-injury Antiplatelet and/or Anticoagulant Therapy
Univariate analysis identified higher magnitude of brain injury (AISBrain) (p = 0.001) and lower GCS on admission as potential independent risk factors (p < 0.001) for an acute coagulopathy (Table 4). Patients with coagulopathy were three times as likely to have unreactive pupils than non-coagulopathic patients with (Table 4). Coagulopathic patients were three times more likely to be hypoxic (patients with a PaO2 < 8 kPa (60 mmHg) and/or a SaO2 < 90%), eight times more likely to be hypotensive and more than five times more likely to be hypothermic (Table 4). Altered base excess (BE) (≤ − 6) occurred 5.7 times more frequently in coagulopathic patients (Table 4). Severe intracranial lesions causing basal cistern compression and severe contusions were associated with coagulopathy, with 2.5- and 2.4-fold increased incidence, respectively, among coagulopathic patients (Table 4). Mortality among coagulopathic patients with iTBI was almost three times higher than those with normal coagulation profile (25.3% vs. 9.0%; p < 0.0001) (data not shown). Multivariate regression analysis identified significant independent risk factors associated with coagulopathy in iTBI patients including odds ratios (OR): the GCS ≤ 8 at hospital admission had an OR of 2.4 and unbalanced BE (≤ − 6) had an OR of 3.1 (Table 5). Systemic secondary insults such as hypotension (< 90 mmHg SBP), which had an OR of 3.5 and hypothermia (temperature < 35 °C), with an OR of 2.9, were also identified (Table 5).
Table 4.
Univariate analysis of potential risk factors associated with acute coagulopathy following iTBI of patients without pre-injury antiplatelet and/or anticoagulant therapy (n = 475)
| No coagulopathy n = 400 | Coagulopathy n = 75 | p value | |
|---|---|---|---|
| Demographics | |||
| Age ≥ 75; n [%] | 38 [9.5] | 4 [5.3] | 0.243 |
| Male gender; n [%] | 283 [70.8] | 50 [66.7] | 0.478 |
| Injury characteristics | |||
| AISBrain severity | 0.001 | ||
| AIS 2; n [%] | 50 [12.5] | 5 [6.7] | |
| AIS 3; n [%] | 143 [35.8] | 21 [28.0] | |
| AIS 4; n [%] | 115 [28.7] | 15 [20.0] | |
| AIS ≥ 5; n [%] | 92 [23.0] | 34 [45.3] | |
| Medical presentation at admission (ED) | |||
| GCS on admission | < 0.001 | ||
| GCS ≥ 8; n [%] | 249 [62.3] | 25 [33.3] | |
| GCS ≤ 8; n [%] | 49 [12.3] | 22 [29.3] | |
| GCS unknown; n [%] | 102 [25.5] | 28 [37.3] | |
| Pupils [uni- or bilateral unreactive]; n [%] | 29 [7.2] | 17 [22.7] | < 0.001 |
| Hypoxia; n [%] | 13 [3.3] | 7 [9.3] | 0.016 |
| Hypotension; n [%] | 6 [1.5] | 9 [12.0] | < 0.001 |
| Hypothermia; n [%] | 10 [2.5] | 10 [13.3] | < 0.001 |
| Neuroworsening; n [%] | 48 [12.0] | 8 [10.7] | 0.742 |
| Laboratory tests | |||
| Arrival haemoglobin < 11; n [%] | 16 [4.0] | 3 [4.0] | 0.742 |
| Arrival Base Excess ≤ − 6; n [%] | 16 [4.0] | 17 [22.7] | < 0.001 |
| Injuries identified on initial CT scan | |||
| Diffuse axonal injury; n [%] | 39 [10.2] | 10 [14.1] | 0.338 |
| Extradural haematoma; n [%] | 77 [19.5] | 11 [14.7] | 0.321 |
| Subdural haematoma; n [%] | 160 [40.4] | 37 [49.3] | 0.151 |
| Subarachnoid haemorrhage; n [%] | 208 [52.4] | 43 [57.3] | 0.432 |
| Midline shift; n [%] | 77 [19.6] | 22 [29.3] | 0.058 |
| Basal cistern compression; n [%] | 40 [10.2] | 19 [25.3] | < 0.001 |
| Depressed skull fracture; n [%] | 52 [13.1] | 15 [20.0] | 0.116 |
| Severe contusion; n [%] | 22 [5.6] | 10 [13.3] | 0.016 |
Systemic secondary insult parameters pre-hospital/at hospital admission were defined as following: hypotension with systolic blood pressure (SBP) < 90 mmHg, hypothermia with temperature < 35 °C and hypoxia with a PaO2 < 8 kPa (60 mmHg) and/or a SaO2 < 90%. Neuroworsening was defined as follows: (1) a decrease in GCS motor score of 2 or more points; (2) a new loss of pupillary reactivity or development of pupillary asymmetry ≥ 2 mm; (3) deterioration in neurological or CT status sufficient to warrant immediate medical or surgical intervention
AIS Abbreviated Injury Scale, CT computed tomography, ED Emergency department, GCS Glasgow Coma Scale
Table 5.
Independent risk factors associated with acute coagulopathy in iTBI of patients without pre-injury antiplatelet and/or anticoagulant therapy (n = 475)
| Regression coefficient | Odds ratio (CI95) | p value | |
|---|---|---|---|
| Injury characteristics | |||
| AISBrain severity | |||
| AIS 3; n [%] | 0.21 | 1.02 [0.45-2.31] | 0.961 |
| AIS 4; n [%] | − 0.52 | 0.59 [0.23–1.49] | 0.267 |
| AIS ≥ 5; n [%] | − 0.18 | 0.83 [0.30–2.29] | 0.721 |
| Medical presentation at admission (ED) | |||
| GCS on admission | |||
| GCS ≤ 8; n [%] | 0.86 | 2.37 [1.20–4.69] | 0.013 |
| GCS unknown; n [%] | 0.45 | 1.57 [0.87–2.85] | 0.133 |
| Pupils [uni- or bilateral unreactive]; n [%] | 0.47 | 1.59 [0.78–3.24] | 0.197 |
| Hypoxia; n [%] | 0.74 | 2.09 [0.79–5.57] | 0.138 |
| Hypotension; n [%] | 1.25 | 3.51 [1.25–9.83] | 0.017 |
| Hypothermia; n [%] | 1.06 | 2.89 [1.11–7.58] | 0.030 |
| Laboratory test | |||
| Arrival base excess ≤ − 6; n [%] | 1.13 | 3.11 [1.33–7.26] | 0.009 |
| No arrival base excess ≤ − 6; n [%] | − 0.92 | 0.91 [0.54–1.53] | 0.729 |
| Injuries identified on initial CT scan | |||
| Midline shift; n [%] | 0.50 | 1.65 [0.94–2.90] | 0.830 |
| Basal cistern compression; n [%] | − 0.009 | 0.99 [0.49–2.01] | 0.980 |
| Depressed skull fracture; n [%] | − 0.004 | 0.99 [0.51–1.93] | 0.991 |
| Severe contusion; n [%] | 0.24 | 1.27 [0.56–2.89] | 0.558 |
Systemic secondary insult parameters pre-hospital/at hospital admission were defined as following: hypotension with systolic blood pressure (SBP) < 90 mmHg, hypothermia with temperature < 35 °C and hypoxia with a PaO2 < 8 kPa (60 mmHg) and/or a SaO2 < 90%. In nine cases, data were missing for multivariate analysis
AIS Abbreviated Injury Scale, CT computed tomography, ED Emergency department, GCS Glasgow Coma Scale
In contrast to the univariate analysis (p = 0.016), hypoxia could not be identified as a risk factor in the multivariate analysis (p = 0.138) (Table 4, Table 5). However, hypoxia was only documented in 20 iTBI patients.
Discussion
The characterisation of haemostatic abnormalities which occur in the context of isolated TBI informs our knowledge and may promote a more effective clinical risk assessment and management during the early course after trauma. The cohort analysed in the present study had a median age of 52 years, with almost one out of five patients being 75 years of age or older. For over 20% of the cohort pre-injury anticoagulant and/or antiplatelet agents, intake was documented. The mortality of the entire iTBI cohort was 16.4% and almost every fifth patient required an emergency surgical intervention. Overall, the presence of coagulopathy in the acute phase of iTBI based upon conventional coagulation parameters was observed in about 20% of all patients with iTBI. In previous reports, the prevalence of coagulopathy in TBI patients with and without extracranial injuries patients upon hospital admission was variable ranging from 7 to 63% [5]. The reported prevalence in all cases was highly dependent on how both TBI and coagulopathy were defined, the sensitivity of the coagulation assays used, the time point after injury at which the coagulation system was assessed and the range of injury severity [9, 13–16]. We used conventional coagulation plasma based assays to assess the degree of coagulopathy in our cohort. However, prothrombin time and aPTT assays only provide a rather incomplete assessment of a patient’s current haemostatic capacity [17]. Although viscoelastic testing, such as TEG and ROTEM, allows a more detailed analysis of the coagulation system in time, data based on this technology were only available in a small proportion of iTBI patients from the CENTER-TBI study core documentation, thus precluding meaningful analysis. For this reason, the conventional parameters INR, aPTT and platelet count were used as primary outcome marker indicating coagulopathy using the thresholds based upon previous studies [5, 18, 19].
The frequency of haemostatic alterations which occur in the context of iTBI may increase with injury severity [5, 9]. In the present study, AISBrain was not an independent predictor of coagulopathy; however, a larger proportion of patients with severe head injury (AISBrain ≥ 5) displayed alterations as compared to those with lower magnitudes sustained. Coagulopathy has previously been reported more frequently in penetrating than in blunt brain injuries [9, 19, 20]. In the present study, less than 2% of iTBI patients had sustained a penetrating injury mechanism. Therefore, the prevalence of coagulopathy reported corresponds rather to its prevalence in the context of a blunt injury mechanism.
Previous reports indicated that coagulopathic TBI patients had a nine times higher mortality and 30 times higher risk of unfavourable outcome compared to non-coagulopathic TBI patients [2, 9]. In the present cohort, a significant increase in mortality among coagulopathic iTBI patients (25.3%) compared to non-coagulopathic patients (9.0%) was observed. A retrospective study based upon a large dataset from trauma patients including those with TBI revealed that patients with blunt TBI showing at least one abnormality in their coagulation profile had a higher mortality rate than non-coagulopathic TBI patients [20]. In line with these findings, the coagulation parameters of iTBI patients in the present study without pre-injury anticoagulant and/or antiplatelet therapy were significantly deteriorated with increasing severity of brain injury, e.g. the higher the AISBrain, the higher the INR and the lower the fibrinogen levels and platelet counts.
Anticoagulant and antiplatelet agents appear to worsen outcome in iTBI. For every fifth iTBI patient in the present study (n = 122), pre-injury intake of anticoagulant and/or antiplatelet agents was documented. Anticoagulant and/or antiplatelet drugs are increasingly prescribed for several indications in the elderly [21]. Vice versa, epidemiological studies have confirmed that the highest incidence of TBI occurs in older adults with falls as the most common mechanism leading to severe head injuries [22–24]. In particular, patients with pre-injury anticoagulant and/or antiplatelet drugs are at increased risk of developing a progressive haemorrhagic injury following a traumatic intracranial haemorrhage [5, 25–29]. In the present study, elderly iTBI patients with pre-injury anticoagulant and/or antiplatelet drugs had an almost twofold increased risk to establish haemostatic abnormalities than those without this risk factor (34% vs. 16%). It is conceivable that the increased haemostatic alteration risk in geriatric TBI patients is associated with pre-injury anticoagulant and/or antiplatelet therapy. In the present study, iTBI patients with pre-injury medication of vitamin K antagonists displayed a higher risk to develop an abnormal coagulation profile compared to those with other pre-injury anticoagulant and/or antiplatelet therapy. Most likely, these patients have an exacerbated progress of TBI, severe complications and outcome due to their pre-existing with vitamin K antagonists. In line with these findings, retrospective studies described higher prevalence of spontaneous bleeding rates and worse outcome in elderly, vitamin K-antagonist treated iTBI patients compared to other anticoagulant agents and platelet inhibitors [30–32]. Despite both groups having a median AISBrain = 4, haemostatic alteration was much more common among anticoagulated patients. If the risk factors for coagulopathy in iTBI patients with pre-injury anticoagulant and/or antiplatelet drugs were similar to those not on these drugs remain speculative due to the limited numbers of patients in these subgroups precluding a meaningful analysis. The overall outcomes among elderly iTBI patients on pre-injury anticoagulant and/or antiplatelet drugs in the present study were significantly worse compared to iTBI patients without anticoagulation therapy (mortality 35.2% in anticoagulated patients vs. 11.6% in non-anticoagulated patients).
Clinical data from prospective observational studies and meta-analyses on TBI patients have been used to describe factors that characterise the development of TBI-associated coagulopathy [2, 20, 33, 34]. The results of both uni- and multivariate analyses obtained from the present study identified hypotension, deranged BE, hypothermia, low GCS and hypoxia being associated with coagulopathy in iTBI patients. With an odds ratio of 3.51, hypotension was the most strongly associated risk factor identified. The results from an earlier prospective study showed that iTBI patients only developed a coagulopathy in the presence of a hypotension, regardless of head injury severity [35]. A base excess ≤ − 6 suggests tissue hypoperfusion most likely to result from systemic hypotension which had an odds ratio of 3.11 indicating coagulopathy. Hypothermia was further identified as an associated risk factor for acute coagulopathy following iTBI with OR of 2.89. In previous studies of trauma patients, hypothermia has been a risk factor for mortality but not directly for coagulopathy [36, 37]. Hypothermia induces coagulopathy by causing deterioration of platelet function, reducing activity of coagulation factors and reducing fibrinogen synthesis all together with increased morbidity and mortality [38–40]. Hypoxia plays an important role in worsening outcome in TBI as it may cause cerebral inflammation and the release of cytokines, augmenting further secondary brain injury [41, 42]. In the present study, hypoxia was identified as another risk factor indicating coagulopathy and poor outcome following iTBI (OR 2.09). In contrast to the univariate analysis (p = 0.016), hypoxia could not be statistically identified as risk factor in the multivariate analysis (p = 0.138). The difference in p values was marginal but exceeded p = 0.05. On the one hand, the variance of p values in the multivariate model was probably attenuated by correlation with other variables, hereby changing the effects (odds ratios) and p values of the other predictors. Thus, it may be that hypoxic patients showed other physical findings that may be captured in the model, so that the effect may differ from the univariate effect. On the other hand, hypoxia was observed in only 20 patients providing a further limitation leading to increased p values. Nevertheless, we consider that hypoxia is indeed a risk factor for coagulopathy, with an odds ratio of 2.09, but our data are not sufficient to prove this with 95% certainty.
Last but not least, GCS ≤ 8 at hospital admission was identified as an independent risk factor for acute coagulopathy in iTBI patients in this study. Other studies which have linked altered GCS with coagulopathy have proposed that injury to the brain itself may induce coagulation disturbances [5, 20, 43]. In a multivariate analysis of iTBI patients from the German Trauma Registry (TR-DGU®), a low GCS (≤ 8) was identified as an independent risk factor for coagulopathy after TBI [20]. It was also concluded that a lower GCS may correlate with a higher risk of neurological decline in iTBI patients with coagulopathy [20]. Related to the identified risk factors, we cannot exclude volume substitution as well as receipt of blood products or haemostatic agents during early prehospital care as a potential cofounder that may have altered haemostatic capacity in the severely injured patients, as a prehospital data collection was not part of the CENTER-TBI core study. Likewise, early in-hospital blood product administration prior to any laboratory coagulation testing was marginally evaluated and precluded a more detailed analysis at this stage. The predictors identified in this study could be used in clinical settings to identify high-risk patients earlier. The results could also support in defining the course and the severity of coagulopathy following iTBI.
Limitations
The present study is the first report on haemostatic alterations occurring in the context of iTBI based upon data from the longitudinal, observational CENTER-TBI core study cohort. The results confirm previous findings on demographics, clinical presentation and coagulation status during the acute phase, e.g. within 4 h, after iTBI. Future analyses will now more thoroughly investigate the coagulation abnormalities encountered in this unique and highly detailed patient dataset. The limitations to the given study apart from those inherent to retrospective analysis of a large prospectively collected dataset include that the recruitment to the CENTER-TBI core study was not consecutive and was determined by site logistics and research interests. This means that patient selection bias may be possible. Likewise, coagulation parameters beyond those used for conventional testing, in particular those potentially reflecting functional deficits, were only marginally captured and precluded more in-depth analysis at this stage. This also refers to the completeness of the datasets analysed as data collection was performed over 4 years. However, among variables considered for this analysis, there was little missing data. The reported associations remain purely descriptive. It can certainly not be concluded from the present analysis whether the observed coagulopathy was the result of the iTBI itself or the precipitating factor that led to a worsening of the clinical situation along with iTBI.
Conclusion
The prevalence of coagulopathy in iTBI patients on pre-injury anticoagulant and/or antiplatelet therapy was significantly higher than in patients without anticoagulant therapy. Independent risk factors associated with acute coagulopathy in iTBI included systolic hypotension, base excess, hypothermia, reduced GCS on ED admission and hypoxia. The acknowledgement and assessment of these risk factors could be helpful in clinical practice for the early identification of TBI-associated coagulopathy, resulting in the expeditious provision of appropriate, targeted clinical management. It remains to be determined whether to coagulopathy seen was the result of the iTBI itself or a precipitating factor for neuroworsening.
Acknowledgements
We would like to thank all CENTER-TBI centres, participants and investigators for all their efforts realising this project.
The CENTER-TBI Participants and Investigators: Cecilia Åkerlund1, Krisztina Amrein2, Nada Andelic3, Lasse Andreassen4, Audny Anke5, Anna Antoni6, Gérard Audibert7, Philippe Azouvi8, Maria Luisa Azzolini9, Ronald Bartels10, Pál Barzó11, Romuald Beauvais12, Ronny Beer13, Bo-Michael Bellander14, Antonio Belli15, Habib Benali16, Maurizio Berardino17, Luigi Beretta9, Morten Blaabjerg18, Peter Bragge19, Alexandra Brazinova20, Vibeke Brinck21, Joanne Brooker22, Camilla Brorsson23, Andras Buki24, Monika Bullinger25, Manuel Cabeleira26, Alessio Caccioppola27, Emiliana Calappi27, Maria Rosa Calvi9, Peter Cameron28, Guillermo Carbayo Lozano29, Marco Carbonara27, Simona Cavallo17, Giorgio Chevallard30, Arturo Chieregato30, Giuseppe Citerio31,32, Iris Ceyisakar33, Hans Clusmann34, Mark Coburn35, Jonathan Coles36, Jamie D. Cooper37, Marta Correia38, Amra Čović39, Nicola Curry40, Endre Czeiter24, Marek Czosnyka26, Claire Dahyot-Fizelier41, Paul Dark42, Helen Dawes43, Véronique De Keyser44, Vincent Degos16, Francesco Della Corte45, Hugo den Boogert10, Bart Depreitere46, Đula Đilvesi47, Abhishek Dixit48, Emma Donoghue22, Jens Dreier49, Guy-Loup Dulière50, Ari Ercole48, Patrick Esser43, Erzsébet Ezer51, Martin Fabricius52, Valery L. Feigin53, Kelly Foks54, Shirin Frisvold55, Alex Furmanov56, Pablo Gagliardo57, Damien Galanaud16, Dashiell Gantner28, Guoyi Gao58, Pradeep George59, Alexandre Ghuysen60, Lelde Giga61, Ben Glocker62, Jagoš Golubovic47, Pedro A. Gomez63, Johannes Gratz64, Benjamin Gravesteijn33, Francesca Grossi45, Russell L. Gruen65, Deepak Gupta66, Juanita A. Haagsma33, Iain Haitsma67, Raimund Helbok13, Eirik Helseth68, Lindsay Horton69, Jilske Huijben33, Peter J. Hutchinson70, Bram Jacobs71, Stefan Jankowski72, Mike Jarrett21, Ji-yao Jiang58, Faye Johnson73, Kelly Jones53, Mladen Karan47, Angelos G. Kolias70, Erwin Kompanje74, Daniel Kondziella52, Evgenios Koraropoulos48, Lars-Owe Koskinen75, Noémi Kovács76, Ana Kowark35, Alfonso Lagares63, Linda Lanyon59, Steven Laureys77, Fiona Lecky78,79, Didier Ledoux77, Rolf Lefering80, Valerie Legrand81, Aurelie Lejeune82, Leon Levi83, Roger Lightfoot84, Hester Lingsma33, Andrew I. R. Maas44, Ana M. Castaño-León63, Marc Maegele85, Marek Majdan20, Alex Manara86, Geoffrey Manley87, Costanza Martino88, Hugues Maréchal50, Julia Mattern89, Catherine McMahon90, Béla Melegh91, David Menon48, Tomas Menovsky44, Ana Mikolic33, Benoit Misset77, Visakh Muraleedharan59, Lynnette Murray28, Ancuta Negru92, David Nelson1, Virginia Newcombe48, Daan Nieboer33, József Nyirádi2, Otesile Olubukola78, Matej Oresic93, Fabrizio Ortolano27, Aarno Palotie94,95,96, Paul M. Parizel97, Jean-François Payen98, Natascha Perera12, Vincent Perlbarg16, Paolo Persona99, Wilco Peul100, Anna Piippo-Karjalainen101, Matti Pirinen94, Horia Ples92, Suzanne Polinder33, Inigo Pomposo29, Jussi P. Posti102, Louis Puybasset103, Andreea Radoi104, Arminas Ragauskas105, Rahul Raj101, Malinka Rambadagalla106, Jonathan Rhodes107, Sylvia Richardson108, Sophie Richter48, Samuli Ripatti94, Saulius Rocka105, Cecilie Roe109, Olav Roise110,111, Jonathan Rosand112, Jeffrey V. Rosenfeld113, Christina Rosenlund114, Guy Rosenthal56, Rolf Rossaint35, Sandra Rossi99, Daniel Rueckert62, Martin Rusnák115, Juan Sahuquillo104, Oliver Sakowitz89,116, Renan Sanchez-Porras116, Janos Sandor117, Nadine Schäfer80, Silke Schmidt118, Herbert Schoechl119, Guus Schoonman120, Rico Frederik Schou121, Elisabeth Schwendenwein6, Charlie Sewalt33, Toril Skandsen122,123, Peter Smielewski26, Abayomi Sorinola124, Emmanuel Stamatakis48, Simon Stanworth40, Robert Stevens125, William Stewart126, Ewout W. Steyerberg33,127, Nino Stocchetti128, Nina Sundström129, Anneliese Synnot22,130, Riikka Takala131, Viktória Tamás124, Tomas Tamosuitis132, Mark Steven Taylor20, Braden Te Ao53, Olli Tenovuo102, Alice Theadom53, Matt Thomas86, Dick Tibboel133, Marjolein Timmers74, Christos Tolias134, Tony Trapani28, Cristina Maria Tudora92, Andreas Unterberg89, Peter Vajkoczy135, Shirley Vallance28, Egils Valeinis61, Zoltán Vámos51, Mathieu van der Jagt136, Gregory Van der Steen44, Joukje van der Naalt71, Jeroen T.J.M. van Dijck100, Thomas A. van Essen100, Wim Van Hecke137, Caroline van Heugten138, Dominique Van Praag139, Thijs Vande Vyvere137, Roel P. J. van Wijk100, Alessia Vargiolu32, Emmanuel Vega82, Kimberley Velt33, Jan Verheyden137, Paul M. Vespa140, Anne Vik122,141, Rimantas Vilcinis132, Victor Volovici67, Nicole von Steinbüchel39, Daphne Voormolen33, Petar Vulekovic47, Kevin K. W. Wang142, Eveline Wiegers33, Guy Williams48, Lindsay Wilson69, Stefan Winzeck48, Stefan Wolf143, Zhihui Yang142, Peter Ylén144, Alexander Younsi89, Frederick A. Zeiler48,145, Veronika Zelinkova20, Agate Ziverte61, Tommaso Zoerle27.
1Department of Physiology and Pharmacology, Section of Perioperative Medicine and Intensive Care, Karolinska Institutet, Stockholm, Sweden, 2János Szentágothai Research Centre, University of Pécs, Pécs, Hungary, 3Division of Surgery and Clinical Neuroscience, Department of Physical Medicine and Rehabilitation, Oslo University Hospital and University of Oslo, Oslo, Norway, 4Department of Neurosurgery, University Hospital Northern Norway, Tromso, Norway, 5Department of Physical Medicine and Rehabilitation, University Hospital Northern Norway, Tromso, Norway, 6Trauma Surgery, Medical University Vienna, Vienna, Austria, 7Department of Anesthesiology & Intensive Care, University Hospital Nancy, Nancy, France, 8Raymond Poincare hospital, Assistance Publique – Hopitaux de Paris, Paris, France, 9Department of Anesthesiology & Intensive Care, S Raffaele University Hospital, Milan, Italy, 10Department of Neurosurgery, Radboud University Medical Center, Nijmegen, The Netherlands, 11Department of Neurosurgery, University of Szeged, Szeged, Hungary, 12International Projects Management, ARTTIC, Munchen, Germany, 13Department of Neurology, Neurological Intensive Care Unit, Medical University of Innsbruck, Innsbruck, Austria, 14Department of Neurosurgery & Anesthesia & intensive care medicine, Karolinska University Hospital, Stockholm, Sweden, 15NIHR Surgical Reconstruction and Microbiology Research Centre, Birmingham, UK, 16Anesthesie-Réanimation, Assistance Publique – Hopitaux de Paris, Paris, France, 17Department of Anesthesia & ICU, AOU Città della Salute e della Scienza di Torino - Orthopedic and Trauma Center, Torino, Italy, 18Department of Neurology, Odense University Hospital, Odense, Denmark, 19BehaviourWorks Australia, Monash Sustainability Institute, Monash University, Victoria, Australia, 20Department of Public Health, Faculty of Health Sciences and Social Work, Trnava University, Trnava, Slovakia, 21Quesgen Systems Inc., Burlingame, California, USA, 22Australian & New Zealand Intensive Care Research Centre, Department of Epidemiology and Preventive Medicine, School of Public Health and Preventive Medicine, Monash University, Melbourne, Australia, 23Department of Surgery and Perioperative Science, Umeå University, Umeå, Sweden, 24Department of Neurosurgery, Medical School, University of Pécs, Hungary and Neurotrauma Research Group, János Szentágothai Research Centre, University of Pécs, Hungary, 25Department of Medical Psychology, Universitätsklinikum Hamburg-Eppendorf, Hamburg, Germany, 26Brain Physics Lab, Division of Neurosurgery, Dept of Clinical Neurosciences, University of Cambridge, Addenbrooke’s Hospital, Cambridge, UK, 27Neuro ICU, Fondazione IRCCS Cà Granda Ospedale Maggiore Policlinico, Milan, Italy, 28ANZIC Research Centre, Monash University, Department of Epidemiology and Preventive Medicine, Melbourne, Victoria, Australia, 29Department of Neurosurgery, Hospital of Cruces, Bilbao, Spain, 30NeuroIntensive Care, Niguarda Hospital, Milan, Italy, 31School of Medicine and Surgery, Università Milano Bicocca, Milano, Italy, 32NeuroIntensive Care, ASST di Monza, Monza, Italy, 33Department of Public Health, Erasmus Medical Center-University Medical Center, Rotterdam, The Netherlands, 34Department of Neurosurgery, Medical Faculty RWTH Aachen University, Aachen, Germany, 35Department of Anaesthesiology, University Hospital of Aachen, Aachen, Germany, 36Department of Anesthesia & Neurointensive Care, Cambridge University Hospital NHS Foundation Trust, Cambridge, UK, 37School of Public Health & PM, Monash University and The Alfred Hospital, Melbourne, Victoria, Australia, 38Radiology/MRI department, MRC Cognition and Brain Sciences Unit, Cambridge, UK, 39Institute of Medical Psychology and Medical Sociology, Universitätsmedizin Göttingen, Göttingen, Germany, 40Oxford University Hospitals NHS Trust, Oxford, UK, 41Intensive Care Unit, CHU Poitiers, Potiers, France, 42University of Manchester NIHR Biomedical Research Centre, Critical Care Directorate, Salford Royal Hospital NHS Foundation Trust, Salford, UK, 43Movement Science Group, Faculty of Health and Life Sciences, Oxford Brookes University, Oxford, UK, 44Department of Neurosurgery, Antwerp University Hospital and University of Antwerp, Edegem, Belgium, 45Department of Anesthesia & Intensive Care, Maggiore Della Carità Hospital, Novara, Italy, 46Department of Neurosurgery, University Hospitals Leuven, Leuven, Belgium, 47Department of Neurosurgery, Clinical centre of Vojvodina, Faculty of Medicine, University of Novi Sad, Novi Sad, Serbia, 48Division of Anaesthesia, University of Cambridge, Addenbrooke’s Hospital, Cambridge, UK, 49Center for Stroke Research Berlin, Charité – Universitätsmedizin Berlin, corporate member of Freie Universität Berlin, Humboldt-Universität zu Berlin, and Berlin Institute of Health, Berlin, Germany, 50Intensive Care Unit, CHR Citadelle, Liège, Belgium, 51Department of Anaesthesiology and Intensive Therapy, University of Pécs, Pécs, Hungary, 52Departments of Neurology, Clinical Neurophysiology and Neuroanesthesiology, Region Hovedstaden Rigshospitalet, Copenhagen, Denmark, 53National Institute for Stroke and Applied Neurosciences, Faculty of Health and Environmental Studies, Auckland University of Technology, Auckland, New Zealand, 54Department of Neurology, Erasmus MC, Rotterdam, the Netherlands, 55Department of Anesthesiology and Intensive care, University Hospital Northern Norway, Tromso, Norway, 56Department of Neurosurgery, Hadassah-hebrew University Medical center, Jerusalem, Israel, 57Fundación Instituto Valenciano de Neurorrehabilitación (FIVAN), Valencia, Spain, 58Department of Neurosurgery, Shanghai Renji hospital, Shanghai Jiaotong University/school of medicine, Shanghai, China, 59Karolinska Institutet, INCF International Neuroinformatics Coordinating Facility, Stockholm, Sweden, 60Emergency Department, CHU, Liège, Belgium, 61Neurosurgery clinic, Pauls Stradins Clinical University Hospital, Riga, Latvia, 62Department of Computing, Imperial College London, London, UK, 63Department of Neurosurgery, Hospital Universitario 12 de Octubre, Madrid, Spain, 64Department of Anesthesia, Critical Care and Pain Medicine, Medical University of Vienna, Austria, 65College of Health and Medicine, Australian National University, Canberra, Australia, 66Department of Neurosurgery, Neurosciences Centre & JPN Apex trauma centre, All India Institute of Medical Sciences, New Delhi-110029, India, 67Department of Neurosurgery, Erasmus MC, Rotterdam, the Netherlands, 68Department of Neurosurgery, Oslo University Hospital, Oslo, Norway, 69Division of Psychology, University of Stirling, Stirling, UK, 70Division of Neurosurgery, Department of Clinical Neurosciences, Addenbrooke’s Hospital & University of Cambridge, Cambridge, UK, 71Department of Neurology, University of Groningen, University Medical Center Groningen, Groningen, Netherlands, 72Neurointensive Care, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, UK, 73Salford Royal Hospital NHS Foundation Trust Acute Research Delivery Team, Salford, UK, 74Department of Intensive Care and Department of Ethics and Philosophy of Medicine, Erasmus Medical Center, Rotterdam, The Netherlands, 75Department of Clinical Neuroscience, Neurosurgery, Umeå University, Umeå, Sweden, 76Hungarian Brain Research Program - Grant No. KTIA_13_NAP-A-II/8, University of Pécs, Pécs, Hungary, 77Cyclotron Research Center, University of Liège, Liège, Belgium, 78Centre for Urgent and Emergency Care Research (CURE), Health Services Research Section, School of Health and Related Research (ScHARR), University of Sheffield, Sheffield, UK, 79Emergency Department, Salford Royal Hospital, Salford UK, 80Institute of Research in Operative Medicine (IFOM), Witten/Herdecke University, Cologne, Germany, 81VP Global Project Management CNS, ICON, Paris, France, 82Department of Anesthesiology-Intensive Care, Lille University Hospital, Lille, France, 83Department of Neurosurgery, Rambam Medical Center, Haifa, Israel, 84Department of Anesthesiology & Intensive Care, University Hospitals Southhampton NHS Trust, Southhampton, UK, 85Cologne-Merheim Medical Center (CMMC), Department of Traumatology, Orthopedic Surgery and Sportmedicine, Witten/Herdecke University, Cologne, Germany, 86Intensive Care Unit, Southmead Hospital, Bristol, Bristol, UK, 87Department of Neurological Surgery, University of California, San Francisco, California, USA, 88Department of Anesthesia & Intensive Care,M. Bufalini Hospital, Cesena, Italy, 89Department of Neurosurgery, University Hospital Heidelberg, Heidelberg, Germany, 90Department of Neurosurgery, The Walton centre NHS Foundation Trust, Liverpool, UK, 91Department of Medical Genetics, University of Pécs, Pécs, Hungary, 92Department of Neurosurgery, Emergency County Hospital Timisoara, Timisoara, Romania, 93School of Medical Sciences, Örebro University, Örebro, Sweden, 94Institute for Molecular Medicine Finland, University of Helsinki, Helsinki, Finland, 95Analytic and Translational Genetics Unit, Department of Medicine; Psychiatric & Neurodevelopmental Genetics Unit, Department of Psychiatry; Department of Neurology, Massachusetts General Hospital, Boston, MA, USA, 96Program in Medical and Population Genetics; The Stanley Center for Psychiatric Research, The Broad Institute of MIT and Harvard, Cambridge, MA, USA, 97Department of Radiology, University of Antwerp, Edegem, Belgium, 98Department of Anesthesiology & Intensive Care, University Hospital of Grenoble, Grenoble, France, 99Department of Anesthesia & Intensive Care, Azienda Ospedaliera Università di Padova, Padova, Italy, 100Dept. of Neurosurgery, Leiden University Medical Center, Leiden, The Netherlands and Dept. of Neurosurgery, Medical Center Haaglanden, The Hague, The Netherlands, 101Department of Neurosurgery, Helsinki University Central Hospital, 102Division of Clinical Neurosciences, Department of Neurosurgery and Turku Brain Injury Centre, Turku University Hospital and University of Turku, Turku, Finland, 103Department of Anesthesiology and Critical Care, Pitié -Salpêtrière Teaching Hospital, Assistance Publique, Hôpitaux de Paris and University Pierre et Marie Curie, Paris, France, 104Neurotraumatology and Neurosurgery Research Unit (UNINN), Vall d’Hebron Research Institute, Barcelona, Spain, 105Department of Neurosurgery, Kaunas University of technology and Vilnius University, Vilnius, Lithuania, 106Department of Neurosurgery, Rezekne Hospital, Latvia, 107Department of Anaesthesia, Critical Care & Pain Medicine NHS Lothian & University of Edinburg, Edinburgh, UK, 108Director, MRC Biostatistics Unit, Cambridge Institute of Public Health, Cambridge, UK, 109Department of Physical Medicine and Rehabilitation, Oslo University Hospital/University of Oslo, Oslo, Norway, 110Division of Orthopedics, Oslo University Hospital, Oslo, Norway, 111Institue of Clinical Medicine, Faculty of Medicine, University of Oslo, Oslo, Norway, 112Broad Institute, Cambridge MA Harvard Medical School, Boston MA, Massachusetts General Hospital, Boston MA, USA, 113National Trauma Research Institute, The Alfred Hospital, Monash University, Melbourne, Victoria, Australia, 114Department of Neurosurgery, Odense University Hospital, Odense, Denmark, 115International Neurotrauma Research Organisation, Vienna, Austria, 116Klinik für Neurochirurgie, Klinikum Ludwigsburg, Ludwigsburg, Germany, 117Division of Biostatistics and Epidemiology, Department of Preventive Medicine, University of Debrecen, Debrecen, Hungary, 118Department Health and Prevention, University Greifswald, Greifswald, Germany, 119Department of Anaesthesiology and Intensive Care, AUVA Trauma Hospital, Salzburg, Austria, 120Department of Neurology, Elisabeth-TweeSteden Ziekenhuis, Tilburg, the Netherlands, 121Department of Neuroanesthesia and Neurointensive Care, Odense University Hospital, Odense, Denmark, 122Department of Neuromedicine and Movement Science, Norwegian University of Science and Technology, NTNU, Trondheim, Norway, 123Department of Physical Medicine and Rehabilitation, St.Olavs Hospital, Trondheim University Hospital, Trondheim, Norway, 124Department of Neurosurgery, University of Pécs, Pécs, Hungary, 125Division of Neuroscience Critical Care, John Hopkins University School of Medicine, Baltimore, USA, 126Department of Neuropathology, Queen Elizabeth University Hospital and University of Glasgow, Glasgow, UK, 127Dept. of Department of Biomedical Data Sciences, Leiden University Medical Center, Leiden, The Netherlands, 128Department of Pathophysiology and Transplantation, Milan University, and Neuroscience ICU, Fondazione IRCCS Cà Granda Ospedale Maggiore Policlinico, Milano, Italy, 129Department of Radiation Sciences, Biomedical Engineering, Umeå University, Umeå, Sweden, 130Cochrane Consumers and Communication Review Group, Centre for Health Communication and Participation, School of Psychology and Public Health, La Trobe University, Melbourne, Australia, 131Perioperative Services, Intensive Care Medicine and Pain Management, Turku University Hospital and University of Turku, Turku, Finland, 132Department of Neurosurgery, Kaunas University of Health Sciences, Kaunas, Lithuania, 133Intensive Care and Department of Pediatric Surgery, Erasmus Medical Center, Sophia Children’s Hospital, Rotterdam, The Netherlands, 134Department of Neurosurgery, Kings college London, London, UK, 135Neurologie, Neurochirurgie und Psychiatrie, Charité – Universitätsmedizin Berlin, Berlin, Germany, 136Department of Intensive Care Adults, Erasmus MC– University Medical Center Rotterdam, Rotterdam, the Netherlands, 137icoMetrix NV, Leuven, Belgium, 138Movement Science Group, Faculty of Health and Life Sciences, Oxford Brookes University, Oxford, UK, 139Psychology Department, Antwerp University Hospital, Edegem, Belgium, 140Director of Neurocritical Care, University of California, Los Angeles, USA, 141Department of Neurosurgery, St.Olavs Hospital, Trondheim University Hospital, Trondheim, Norway, 142Department of Emergency Medicine, University of Florida, Gainesville, Florida, USA, 143Department of Neurosurgery, Charité – Universitätsmedizin Berlin, corporate member of Freie Universität Berlin, Humboldt-Universität zu Berlin, and Berlin Institute of Health, Berlin, Germany, 144VTT Technical Research Centre, Tampere, Finland, 145Section of Neurosurgery, Department of Surgery, Rady Faculty of Health Sciences, University of Manitoba, Winnipeg, MB, Canada.
Author’s Contribution
Data were acquired, analysed and interpreted by JB, VR, ST, HG, NS and MM. Statistical expertise was provided by RL. HS, OG, RR, SS and NC contributed to the conception of the study, providing scientific support and critically revised the data. The manuscript was written by JB and has been critically reviewed by all authors. Supervision was provided by MM. All authors read and approved the final manuscript.
Source of Support
Open Access funding enabled and organized by Projekt DEAL. The research described above was supported by the European Union´s Seventh Framework Programme (FP7/2007-2013) under Grant Agreement No. 602150 (CENTER-TBI).
Conflicts of interest
The authors declare that they have no conflict of interest.
Consent to participate
The manuscript has not been published elsewhere and is not under consideration by another journal.
Ethics Approval
As part of the CENTER-TBI core study, the present analysis was performed in accordance with relevant local ethics and European law.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Marc Maegele, Email: Marc.Maegele@t-online.de.
CENTER-TBI Participants and Investigators:
Cecilia Åkerlund, Krisztina Amrein, Nada Andelic, Lasse Andreassen, Audny Anke, Anna Antoni, Gérard Audibert, Philippe Azouvi, Maria Luisa Azzolini, Ronald Bartels, Pál Barzó, Romuald Beauvais, Ronny Beer, Bo-Michael Bellander, Antonio Belli, Habib Benali, Maurizio Berardino, Luigi Beretta, Morten Blaabjerg, Peter Bragge, Alexandra Brazinova, Vibeke Brinck, Joanne Brooker, Camilla Brorsson, Andras Buki, Monika Bullinger, Manuel Cabeleira, Alessio Caccioppola, Emiliana Calappi, Maria Rosa Calvi, Peter Cameron, Guillermo Carbayo Lozano, Marco Carbonara, Simona Cavallo, Giorgio Chevallard, Arturo Chieregato, Giuseppe Citerio, Iris Ceyisakar, Hans Clusmann, Mark Coburn, Jonathan Coles, Jamie D. Cooper, Marta Correia, Amra Čović, Nicola Curry, Endre Czeiter, Marek Czosnyka, Claire Dahyot-Fizelier, Paul Dark, Helen Dawes, Véronique De Keyser, Vincent Degos, Francesco Della Corte, Hugo den Boogert, Bart Depreitere, Đula Đilvesi, Abhishek Dixit, Emma Donoghue, Jens Dreier, Guy-Loup Dulière, Ari Ercole, Patrick Esser, Erzsébet Ezer, Martin Fabricius, Valery L. Feigin, Kelly Foks, Shirin Frisvold, Alex Furmanov, Pablo Gagliardo, Damien Galanaud, Dashiell Gantner, Guoyi Gao, Pradeep George, Alexandre Ghuysen, Lelde Giga, Ben Glocker, Jagoš Golubovic, Pedro A. Gomez, Johannes Gratz, Benjamin Gravesteijn, Francesca Grossi, Russell L. Gruen, Deepak Gupta, Juanita A. Haagsma, Iain Haitsma, Raimund Helbok, Eirik Helseth, Lindsay Horton, Jilske Huijben, Peter J. Hutchinson, Bram Jacobs, Stefan Jankowski, Mike Jarrett, Ji-yao Jiang, Faye Johnson, Kelly Jones, Mladen Karan, Angelos G. Kolias, Erwin Kompanje, Daniel Kondziella, Evgenios Koraropoulos, Lars-Owe Koskinen, Noémi Kovács, Ana Kowark, Alfonso Lagares, Linda Lanyon, Steven Laureys, Fiona Lecky, Didier Ledoux, Rolf Lefering, Valerie Legrand, Aurelie Lejeune, Leon Levi, Roger Lightfoot, Hester Lingsma, Andrew I. R. Maas, Ana M. Castaño-León, Marc Maegele, Marek Majdan, Alex Manara, Geoffrey Manley, Costanza Martino, Hugues Maréchal, Julia Mattern, Catherine McMahon, Béla Melegh, David Menon, Tomas Menovsky, Ana Mikolic, Benoit Misset, Visakh Muraleedharan, Lynnette Murray, Ancuta Negru, David Nelson, Virginia Newcombe, Daan Nieboer, József Nyirádi, Otesile Olubukola, Matej Oresic, Fabrizio Ortolano, Aarno Palotie, Paul M. Parizel, Jean-François Payen, Natascha Perera, Vincent Perlbarg, Paolo Persona, Wilco Peul, Anna Piippo-Karjalainen, Matti Pirinen, Horia Ples, Suzanne Polinder, Inigo Pomposo, Jussi P. Posti, Louis Puybasset, Andreea Radoi, Arminas Ragauskas, Rahul Raj, Malinka Rambadagalla, Jonathan Rhodes, Sylvia Richardson, Sophie Richter, Samuli Ripatti, Saulius Rocka, Cecilie Roe, Olav Roise, Jonathan Rosand, Jeffrey V. Rosenfeld, Christina Rosenlund, Guy Rosenthal, Rolf Rossaint, Sandra Rossi, Daniel Rueckert, Martin Rusnák, Juan Sahuquillo, Oliver Sakowitz, Renan Sanchez-Porras, Janos Sandor, Nadine Schäfer, Silke Schmidt, Herbert Schoechl, Guus Schoonman, Rico Frederik Schou, Elisabeth Schwendenwein, Charlie Sewalt, Toril Skandsen, Peter Smielewski, Abayomi Sorinola, Emmanuel Stamatakis, Simon Stanworth, Robert Stevens, William Stewart, Ewout W. Steyerberg, Nino Stocchetti, Nina Sundström, Anneliese Synnot, Riikka Takala, Viktória Tamás, Tomas Tamosuitis, Mark Steven Taylor, Braden Te Ao, Olli Tenovuo, Alice Theadom, Matt Thomas, Dick Tibboel, Marjolein Timmers, Christos Tolias, Tony Trapani, Cristina Maria Tudora, Andreas Unterberg, Peter Vajkoczy, Shirley Vallance, Egils Valeinis, Zoltán Vámos, Mathieu van der Jagt, Gregory Van der Steen, Joukje van der Naalt, Jeroen T. J. M. van Dijck, Thomas A. van Essen, Wim Van Hecke, Caroline van Heugten, Dominique Van Praag, Thijs Vande Vyvere, Roel P. J. van Wijk, Alessia Vargiolu, Emmanuel Vega, Kimberley Velt, Jan Verheyden, Paul M. Vespa, Anne Vik, Rimantas Vilcinis, Victor Volovici, Nicole von Steinbüchel, Daphne Voormolen, Petar Vulekovic, Kevin K. W. Wang, Eveline Wiegers, Guy Williams, Lindsay Wilson, Stefan Winzeck, Stefan Wolf, Zhihui Yang, Peter Ylén, Alexander Younsi, Frederick A. Zeiler, Veronika Zelinkova, Agate Ziverte, and Tommaso Zoerle
References
- 1.Hyder AA, Wunderlich CA, Puvanachandra P, Gururaj G, Kobusingye OC. The impact of traumatic brain injuries: a global perspective. NeuroRehabilitation. 2007;22(5):341–353. doi: 10.3233/NRE-2007-22502. [DOI] [PubMed] [Google Scholar]
- 2.Harhangi BS, Kompanje EJO, Leebeek FWG, Maas AIR. Coagulation disorders after traumatic brain injury. Acta Neurochir (Wien) 2008;150(2):165–175. doi: 10.1007/s00701-007-1475-8. [DOI] [PubMed] [Google Scholar]
- 3.Hoyt DB. A clinical review of bleeding dilemmas in trauma. In: Seminars in hematology;2004, p. 40–3. [DOI] [PubMed]
- 4.Zhang J, Jiang R, Liu L, Watkins T, Zhang F, Dong JF. Traumatic brain injury-associated coagulopathy. J Neurotrauma. 2012;29(17):2597–2605. doi: 10.1089/neu.2012.2348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maegele M, Schöchl H, Menovsky T, et al. Coagulopathy and haemorrhagic progression in traumatic brain injury: advances in mechanisms, diagnosis, and management. Lancet Neurol. 2017;16(8):630–647. doi: 10.1016/S1474-4422(17)30197-7. [DOI] [PubMed] [Google Scholar]
- 6.Laroche M, Kutcher ME, Huang MC, Cohen MJ, Manley GT. Coagulopathy after traumatic brain injury. Neurosurgery. 2012;70(6):1334–1345. doi: 10.1227/NEU.0b013e31824d179b. [DOI] [PubMed] [Google Scholar]
- 7.Chen H, Xue LX, Guo Y, et al. The influence of hemocoagulation disorders on the development of posttraumatic cerebral infarction and outcome in patients with moderate or severe head trauma. Biomed Res Int. 2013 doi: 10.1155/2013/685174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sun Y, Wang J, Wu X, et al. Validating the incidence of coagulopathy and disseminated intravascular coagulation in patients with traumatic brain injury—analysis of 242 cases. Br J Neurosurg. 2011;25(3):363–368. doi: 10.3109/02688697.2011.552650. [DOI] [PubMed] [Google Scholar]
- 9.Talving P, Benfield R, Hadjizacharia P, Inaba K, Chan LS, Demetriades D. Coagulopathy in severe traumatic brain injury: a prospective study. J Trauma Inj Infect Crit Care. 2009;66(1):55–61. doi: 10.1097/TA.0b013e318190c3c0. [DOI] [PubMed] [Google Scholar]
- 10.Yuan Q, Sun YR, Wu X, et al. Coagulopathy in traumatic brain injury and its correlation with progressive hemorrhagic injury: a systematic review and meta-analysis. J Neurotrauma. 2016;33(14):1279–1291. doi: 10.1089/neu.2015.4205. [DOI] [PubMed] [Google Scholar]
- 11.Zhang D, Gong S, Jin H, et al. Coagulation parameters and risk of progressive hemorrhagic injury after traumatic brain injury: a systematic review and meta-analysis. Biomed Res Int. 2015 doi: 10.1155/2015/261825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Steyerberg EW, Wiegers E, Sewalt C, et al. Case-mix, care pathways, and outcomes in patients with traumatic brain injury in CENTER-TBI: a European prospective, multicentre, longitudinal, cohort study. Lancet Neurol. 2019;18(10):923–934. doi: 10.1016/S1474-4422(19)30232-7. [DOI] [PubMed] [Google Scholar]
- 13.Chhabra G, Rangarajan K, Subramanian A, Agrawal D, Sharma S, Mukhopadhayay AK. Hypofibrinogenemia in isolated traumatic brain injury in Indian patients. Neurol India. 2010;58(5):756–757. doi: 10.4103/0028-3886.72175. [DOI] [PubMed] [Google Scholar]
- 14.Shehata M, Afify I, El-Shafie M, Khaled M. Prevalence and clinical implications of coagulopathy in patients with isolated head trauma. Med J Cairo Univ. 2011;79(2):131–137. [Google Scholar]
- 15.Stein SC, Smith DH. Coagulopathy in traumatic brain injury. Neurocrit Care. 2004;1(4):479–488. doi: 10.1385/NCC:1:4:479. [DOI] [PubMed] [Google Scholar]
- 16.Zehtabchi S, Soghoian S, Liu Y, et al. The association of coagulopathy and traumatic brain injury in patients with isolated head injury. Resuscitation. 2008;76(1):52–56. doi: 10.1016/j.resuscitation.2007.06.024. [DOI] [PubMed] [Google Scholar]
- 17.Chandler WL, Dunbar NM. Thrombin generation in trauma patients. Transfusion. 2009;49(12):2652–2660. doi: 10.1111/j.1537-2995.2009.02335.x. [DOI] [PubMed] [Google Scholar]
- 18.Schöchl H, Solomon C, Traintinger S, et al. Thromboelastometric (ROTEM) findings in patients suffering from isolated severe traumatic brain injury. J Neurotrauma. 2011;28(10):2033–2041. doi: 10.1089/neu.2010.1744. [DOI] [PubMed] [Google Scholar]
- 19.Lustenberger T, Talving P, Kobayashi L, et al. Early coagulopathy after isolated severe traumatic brain injury: relationship with hypoperfusion challenged. J Trauma Inj Infect Crit Care. 2010;69(6):1410–1414. doi: 10.1097/TA.0b013e3181cdae81. [DOI] [PubMed] [Google Scholar]
- 20.Wafaisade A, Lefering R, Tjardes T, et al. Acute coagulopathy in isolated blunt traumatic brain injury. Neurocrit Care. 2010;12(2):211–219. doi: 10.1007/s12028-009-9281-1. [DOI] [PubMed] [Google Scholar]
- 21.Shoeb M, Fang MC. Assessing bleeding risk in patients taking anticoagulants. J Thromb Thrombolysis. 2013;35:312–319. doi: 10.1007/s11239-013-0899-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gardner RC, Dams-O’Connor K, Morrissey MR, Manley GT. Geriatric traumatic brain injury: epidemiology, outcomes, knowledge gaps, and future directions. J Neurotrauma. 2018;35(7):889–906. doi: 10.1089/neu.2017.5371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harvey LA, Close JCT. Traumatic brain injury in older adults: characteristics, causes and consequences. Injury. 2012;43:1821–1826. doi: 10.1016/j.injury.2012.07.188. [DOI] [PubMed] [Google Scholar]
- 24.Haring RS, Narang K, Canner JK, et al. Traumatic brain injury in the elderly: morbidity and mortality trends and risk factors. J Surg Res. 2015;195(1):1–9. doi: 10.1016/j.jss.2015.01.017. [DOI] [PubMed] [Google Scholar]
- 25.Tauber M, Koller H, Moroder P, Hitzl W, Resch H. Secondary intracranial hemorrhage after mild head injury in patients with low-dose acetylsalicylate acid prophylaxis. J Trauma Inj Infect Crit Care. 2009;67(3):521–525. doi: 10.1097/TA.0b013e3181a7c184. [DOI] [PubMed] [Google Scholar]
- 26.Nishijima DK, Offerman SR, Ballard DW, et al. Risk of traumatic intracranial hemorrhage in patients with head injury and preinjury warfarin or clopidogrel use. Acad Emerg Med. 2013;20(2):140–145. doi: 10.1111/acem.12074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nishijima DK, Zehtabchi S, Berrong J, Legome E. Utility of platelet transfusion in adult patients with traumatic intracranial hemorrhage and preinjury antiplatelet use: a systematic review. J Trauma Acute Care Surg. 2012;72(6):1658–1663. doi: 10.1097/TA.0b013e318256dfc5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nishijima DK, Shahlaie K, Sarkar K, Rudisill N, Holmes JF. Risk of unfavorable long-term outcome in older adults with traumatic intracranial hemorrhage and anticoagulant or antiplatelet use. Am J Emerg Med. 2013;31(8):1244–1247. doi: 10.1016/j.ajem.2013.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Joseph B, Pandit V, Aziz H, et al. Clinical outcomes in traumatic brain injury patients on preinjury clopidogrel: a prospective analysis. J Trauma Acute Care Surg. 2014;76(3):817–820. doi: 10.1097/TA.0b013e3182aafcf0. [DOI] [PubMed] [Google Scholar]
- 30.Prexl O, Bruckbauer M, Voelckel W, et al. The impact of direct oral anticoagulants in traumatic brain injury patients greater than 60-years-old. Scand J Trauma Resusc Emerg Med. 2018;26(1):20. doi: 10.1186/s13049-018-0487-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Grandhi R, Harrison G, Voronovich Z, et al. Preinjury warfarin, but not antiplatelet medications, increases mortality in elderly traumatic brain injury patients. J Trauma Acute Care Surg. 2015;78:614–621. doi: 10.1097/TA.0000000000000542. [DOI] [PubMed] [Google Scholar]
- 32.Dossett LA, Riesel JN, Griffin MR, Cotton BA. Prevalence and implications of preinjury warfarin use: an analysis of the National Trauma Databank. Arch Surg. 2011;146(5):565–570. doi: 10.1001/archsurg.2010.313. [DOI] [PubMed] [Google Scholar]
- 33.Epstein DS, Mitra B, O’Reilly G, Rosenfeld JV, Cameron PA. Acute traumatic coagulopathy in the setting of isolated traumatic brain injury: a systematic review and meta-analysis. Injury. 2014;45(5):819–824. doi: 10.1016/j.injury.2014.01.011. [DOI] [PubMed] [Google Scholar]
- 34.Epstein DS, Mitra B, Cameron PA, Fitzgerald M, Rosenfeld JV. Acute traumatic coagulopathy in the setting of isolated traumatic brain injury: definition, incidence and outcomes. Br J Neurosurg. 2015;29(1):118–122. doi: 10.3109/02688697.2014.950632. [DOI] [PubMed] [Google Scholar]
- 35.Cohen MJ, Brohi K, Ganter MT, Manley GT, Mackersie RC, Pittet JF. Early coagulopathy after traumatic brain injury: the role of hypoperfusion and the protein c pathway. J Trauma. 2007;63(6):1254–1262. doi: 10.1097/TA.0b013e318156ee4c. [DOI] [PubMed] [Google Scholar]
- 36.Waibel BH, Schlitzkus LL, Newell MA, Durham CA, Sagraves SG, Rotondo MF. Impact of hypothermia (below 36°C) in the rural trauma patient. J Am Coll Surg. 2009;209(5):580–588. doi: 10.1016/j.jamcollsurg.2009.07.021. [DOI] [PubMed] [Google Scholar]
- 37.Lapostolle F, Couvreur J, Koch FX, et al. Hypothermia in trauma victims at first arrival of ambulance personnel: an observational study with assessment of risk factors. Scand J Trauma Resusc Emerg Med. 2017;25(1):43. doi: 10.1186/s13049-017-0349-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Perlman R, Callum J, Laflamme C, et al. A recommended early goal-directed management guideline for the prevention of hypothermia-related transfusion, morbidity, and mortality in severely injured trauma patients. Crit Care. 2016;20(1):107. doi: 10.1186/s13054-016-1271-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hess JR, Brohi K, Dutton RP, et al. The coagulopathy of trauma: a review of mechanisms. J Trauma Inj Infect Crit Care. 2008;65(4):748–754. doi: 10.1097/TA.0b013e3181877a9c. [DOI] [PubMed] [Google Scholar]
- 40.Kaafarani HMA, Velmahos GC. Damage control resuscitation in trauma. Scand J Surg. 2014;103(2):81–88. doi: 10.1177/1457496914524388. [DOI] [PubMed] [Google Scholar]
- 41.Yan EB, Satgunaseelan L, Paul E, et al. Post-traumatic hypoxia is associated with prolonged cerebral cytokine production, higher serum biomarker levels, and poor outcome in patients with severe traumatic brain injury. J Neurotrauma. 2014;31(7):618–629. doi: 10.1089/neu.2013.3087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Davis DP, Meade W, Sise MJ, et al. Both hypoxemia and extreme hyperoxemia may be detrimental in patients with severe traumatic brain injury. J Neurotrauma. 2009;26(12):2217–2223. doi: 10.1089/neu.2009.0940. [DOI] [PubMed] [Google Scholar]
- 43.Scherer RU, Spangenberg P. Procoagulant activity in patients with isolated severe head trauma. Crit Care Med. 1998;26(1):149–156. doi: 10.1097/00003246-199801000-00031. [DOI] [PubMed] [Google Scholar]