Abstract
Obesity, binge-eating symptoms, and PTSD symptoms, commonly co-occur. Avoidance, a key feature of PTSD and proposed mechanism of binge-eating, is one potential mechanism for explaining this clinical overlap. The purpose of the current study was to: 1) examine the associations between PTSD symptoms (PTSD Checklist-Civilian; PCL-C) and measures of binge-eating symptoms (Binge Eating Scale; BES) and obesity-related quality of life (Obesity Related Well-Being Questionnaire-97; ORWELL-97) in a sample of veterans with overweight or obesity (N = 89), and 2) determine whether experiential avoidance (The Acceptance and Action Questionnaire–II; AAQ-II) explains the relationship between PTSD symptoms and binge-eating symptoms, and PTSD symptoms and obesity-related quality of life, respectively. Scores on the PCL-C, BES, ORWELL-97, and AAQ-II were all significantly correlated. Linear regression analyses indicated that higher PCL-C scores were related to higher scores on the BES and ORWELL-97 after controlling for potentially confounding factors (BMI and race). Effect sizes were in the medium-large range. Further, AAQ-II mediated the relationship between PCL-C and ORWELL-97, but did not mediate the relationship between PCL-C and BES. These findings suggest that experiential avoidance should be considered in interventions addressing co-occurring PTSD, binge-eating, and poor obesity-related well-being. Longitudinal research is needed to better understand directionality of these relationships and changes over time.
Keywords: PTSD, binge-eating, obesity-related quality of life, experiential avoidance, veterans, obesity
Obesity is a global epidemic related to higher health care costs (Biener, Cawley, & Meyerhoefer, 2017; Jia & Lubetkin, 2005) and poor health outcomes (Dixon, 2010). Additionally, individuals with obesity experience physical discomfort, impaired social functioning, and psychological distress, which in turn is associated with poor quality of life (Albano, Rowlands, Baciadonna, Lo Coco, & Cardi, 2019; De Zwaan et al., 2002; Mannucci et al., 1999). Among adults with overweight and obesity, binge-eating symptoms are common and can impede weight-loss efforts and increase the probability of weight (re)gain (Bertoli et al., 2016; Masheb et al., 2015). This relationship is particularly relevant for military veterans who access healthcare through the Veterans Healthcare Administration, who experience a higher rate of obesity than the general U.S. population (Breland et al., 2017). Prior studies have reported that 22% of Veterans endorsed experiencing two or more episodes of binge-eating per week and 26% of Veterans have endorsed feeling a loss of control around eating (Dorflinger, Ruser, & Masheb, 2017; Higgins et al., 2013; Slane et al., 2016).
Posttraumatic stress disorder (PTSD) is also prevalent among military veterans (Fulton et al., 2015; Kang, Natelson, Mahan, Lee, & Murphy, 2003; Marmar et al., 2015). In both veteran (Bartoli et al., 2015; Higgins et al., 2013; Litwack, Mitchell, Sloan, Reardon, & Miller, 2014; Smith, Tyzik, Neylan, & Cohen, 2015; Vieweg et al., 2007) and civilian samples (Brewerton, 2007; Mitchell, Mazzeo, Schlesinger, Brewerton, & Smith, 2012), PTSD frequently co-occurs with obesity and binge-eating (Mason et al., 2017). It has been hypothesized that experiencing trauma, in combination with pre-existing shared biological and emotional dysregulation, makes some individuals more susceptible to both disordered eating and PTSD (Mitchell et al., 2012). Additionally, individuals with PTSD may use food to cope with negative affect and stress, leading to the development of unhealthy eating habits and obesity (Mason et al., 2017; Scott, McGee, Wells, & Oakley Browne, 2008; Talbot, Maguen, Epel, Metzler, & Neylan, 2013). However, mechanisms explaining the relationship between binge-eating symptoms, obesity-related quality of life, and PTSD symptoms among veterans with overweight and obesity have not been explicitly examined. It is essential to understand the psychological processes underlying these commonly co-occurring broader symptomologies, as they are related to poorer physical and mental health outcomes (Hall, Hoerster, & Yancy, 2015; Higgins et al., 2013), and could potentially be treated simultaneously. Further, eating and weight concerns are common among male veterans (Rosenberger & Dorflinger, 2013), but men are typically underrepresented in eating disorder research (Rosenberger & Dorflinger, 2013; Valente et al., 2017), indicating a need for understanding mechanisms in men in particular.
Experiential avoidance, or the unwillingness to experience unpleasant thoughts, emotions, and memories, may partly explain the relationship between PTSD symptoms and binge-eating symptoms and between PTSD symptoms and obesity-related quality of life. Experiential avoidance is a compelling candidate mechanism since avoidance behaviors are a key feature of PTSD (American Psychiatric Association, 2013) and play an important role in binge-eating. In terms of PTSD, avoidance behaviors are related to the development of PTSD, as well as functional impairment (Solomon & Mikulincer, 2007) and poor quality of life in persons with PTSD (Kashdan, Morina, & Priebe, 2009). In a study utilizing ecological momentary assessment among individuals with PTSD, avoidance was the most commonly used emotion regulation strategy among participants, and predicted subsequent increases in PTSD symptom severity (Short, Boffa, Clancy, & Schmidt, 2018).
Binge-eating is well-documented as a means to avoid experiencing unpleasant and unwanted emotions, such as anxiety, depression, or boredom and thoughts (Allison, Grilo, Masheb, & Stunkard, 2005; Barnes & Tantleff-Dunn, 2010; Lillis, Hayes, & Levin, 2011). For example, experiential avoidance mediated the relationship between negative emotions and emotional eating among college students (Weineland, Lillis, & Dahl, 2013). In adults with obesity seeking weight-loss treatment, experiential avoidance was associated with poorer health-related quality of life and mediated the relationship between body mass index (BMI) and health-related quality of life (Lillis, Levin, & Hayes, 2011). Further, treatments for binge-eating and weight-loss addressing experiential avoidance have demonstrated improvements in BMI, weight-related self-stigma, binge-eating, and physical activity levels (Lillis, Hayes, Bunting, & Masuda, 2009; Lillis, Hayes, et al., 2011; Tapper et al., 2009). Thus, it is plausible that binge-eating behaviors function as a means to avoid unwanted symptoms of PTSD, such as hyperarousal, fear, and flashbacks. We are not aware of any studies that consider experiential avoidance in the context of obesity, binge-eating symptoms, and PTSD symptoms. However, in a sample of 71 persons with history of sexual trauma and 25 controls with no history of sexual trauma, Holzer and colleages (2008) found preliminary support that avoidance symptoms mediate the association between sexual trauma history and eating disorder symptoms.
Given that experiential avoidance relates to PTSD symptoms and binge-eating symptoms, we posit that avoidance may explain the relationship between PTSD symptoms and binge-eating symptoms, as well as the relationships between PTSD symptoms and obesity-related quality of life, among veterans with overweight/obesity. Understanding common underlying psychological processes among these co-occurring concerns may inform the development of treatments that address these concerns simultaneously (Brewerton, 2007). Thus, the purpose of the current study was to: 1) examine the associations among PTSD symptoms and measures of binge-eating symptoms and, obesity-related quality of life in a primarily male sample of veterans with overweight or obesity; and 2) determine whether experiential avoidance explains the relationship among PTSD symptoms and binge-eating symptoms, and obesity-related quality of life. We hypothesized that 1) greater PTSD symptoms would be related to greater binge-eating symptoms and lower obesity-related quality of life, and 2) experiential avoidance would mediate the relationship between PTSD symptoms and (a) binge-eating symptoms and (b) obesity-related quality of life.
Method
Participants
Participants (N = 89, nmale = 67) were U.S. military veterans recruited for a clinical trial comparing Acceptance and Commitment Therapy (ACT) to behavioral weight loss to treat problematic eating (Afari et al., 2019). Problematic eating included a range of disinhibited eating behaviors, including objective binge-eating, subjective binge-eating, overeating, loss of control eating, and emotional eating. Eligible participants had previously participated in MOVE!©, the Veteran Health Administration’s evidence-based, multidisciplinary weight management and health promotion program. Inclusion criteria for the original study and this secondary analysis were: aged 18-75 years, BMI ≥ 25 kg/m2, participation in at least 5 of 8 MOVE!© sessions, and self-endorsement of problems with stress-related eating. Those with serious or unstable medical or psychiatric illness (i.e., history of active psychosis, current substance use disorder, anorexia nervosa, and bulimia nervosa), psychosocial instability (e.g., homelessness), conditions in which exercise or weight loss could be detrimental to health, current suicidality, previous experience with ACT, or currently participating in other interventions for obesity or binge-eating were excluded. Potential participants were screened by telephone using the Mini International Neuropsychiatric Interview (Lecrubier et al., 1997). Measures collected at baseline from the clinical trial were used in the current study. The local Institutional Review Board and the Research and Development Committee approved the study. Informed consent was obtained from participants.
Measures
Demographic variables.
Participants reported demographic characteristics, including age, sex, race, ethnicity, education, and income at baseline.
Body Mass Index (BMI).
BMI (kg/m2) was calculated using weight and height assessed by research staff.
Binge-Eating Symptoms.
Binge-eating symptoms were assessed using the Binge Eating Scale (BES; Gormally, Black, Daston, & Rardin, 1982). The BES is a 16-item self-report measure that assesses the behavioral, cognitive, and emotional features of binge-eating in adults with overweight and obesity. Participants are instructed to select one statement out of four, which best describes their binge-eating-related attitudes and behaviors, from 16 groups of questions. Each statement is weighted either 0, 1, 2, or 3, and weights are summed for a total score. An example item weighted 0 is, “I rarely eat so much food that I feel uncomfortably stuffed afterward.” An example item weighted 3 from the same group of statements is, “I eat so much food that I regularly feel quite uncomfortable after eating and sometimes a bit nauseous.” Higher scores indicate greater binge-eating. The BES has good internal consistency and test-retest reliability in overweight and obese individuals (Gormally et al., 1982). A score of 18 or higher indicates clinically significant binge-eating (Greeno, Marcus, & Wing, 1995). Internal consistency in the current sample was excellent (Cronbach’s alpha = .90)
Obesity-Related Quality of Life.
The Obesity Related Well-Being Questionnaire-97 (ORWELL-97; Mannucci et al., 1999) is an 18-item self-report instrument designed to assess quality of life among persons with obesity in the domains of physical symptoms, physical discomfort, and familial, social, and occupational functioning. Respondents rate the frequency and severity of symptoms, and the extent to which certain domains are important or are limited due to obesity, on a 4-point scale from 0 (not at all) to 3 (much). Example items include, “Does shortness of breath represent an obstacle for your daily activities?” and “How important is it for you to exercise regularly?” The ORWELL-97 is scored by multiplying participants’ subjective importance rating of each domain with the frequency of distress rating for each domain. Higher scores indicate lower quality of life. Internal consistency in the current sample was good (Cronbach’s alpha = .88)
PTSD Symptoms.
The PCL-C (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996) is a 17-item self-report measure used to assess PTSD symptoms caused by any traumatic event. This version simplifies assessment in the context of multiple traumatic events because symptom endorsements are attributed to “stressful experiences” rather than a specific event. Respondents indicate on a 5-point scale how bothered they have been by symptoms of PTSD over the past month from 1 (not at all) to 5 (extremely). Example items include, “Repeated, disturbing dreams of a stressful experience from the past,” and “Feeling jumpy or easily startled” Items are summed to form a total score, with higher scores indicating greater PTSD symptom severity. Internal consistency in the current sample was excellent (Cronbach’s alpha = .96)
Experiential Avoidance.
The Acceptance and Action Questionnaire–II (AAQ-II; Bond et al., 2011) is a 7-item self-report scale that assesses response to difficult thoughts, feelings, and physiological sensations. Participants rate the accuracy of statements on a 7-point scale from 1 (never true) to 7 (always true). Example items include, “Emotions cause problems in my life” and “I worry about not being able to control my worries and feelings.” Higher scores indicate greater experiential avoidance. Internal consistency in the current sample was excellent (Cronbach’s alpha = .95)
Data analyses
All analyses were conducted using IBM SPSS Statistics, version 26 (IBM Corp., Armonk, N.Y., USA). Bivariate correlations were used to examine relationships among PTSD symptoms (PTSD Checklist-Civilian; PCL-C), binge-eating symptoms (BES), obesity-related quality of life (ORWELL-97), and experiential avoidance (AAQ-II). Bivariate correlations and independent samples t-tests were used to identify potential demographic covariates. To address aim 1, separate hierarchical linear regression models were used to examine relationships between PTSD symptoms (independent variable) with binge-eating symptoms (outcome) and obesity-related quality of life (outcome), respectively. For each model, demographic covariates that were significantly related to outcome variables (i.e., BMI and race) were entered on the first step, and PCL-C score was entered on the second step. Analyses included cases that were randomized to treatment with complete data at baseline; therefore, there were no missing data in the present analyses. To address aim 2, separate cross-sectional mediation models were employed using the program for simple mediation from the PROCESS macro for SPSS (Preacher & Hayes, 2004) to examine whether experiential avoidance explains the relationship between PTSD symptoms and each outcome (binge-eating symptoms, obesity-related quality of life). PROCESS uses bootstrapping, a non-parametric resampling procedure, to estimate the indirect effects and generate confidence intervals (CI). The mediation effect is considered significant if the 95% CI does not include zero. Bootstrapping can be appropriate for small samples, does not make assumptions about the distribution of the sample, and decreases the chance of both type I and type II errors (Preacher & Hayes, 2004). Each analysis used 10,000 bootstrapped samples. Mediation models controlled for BMI and race. We also conducted sensitivity analyses using data from male participants only (n = 67) for each regression and mediation analysis.
Results
The average age of the sample was 55.97 years (SD = 10.86). The majority of participants were male (77.5%) and identified as White (68.5%). On average, participants’ BMI (M = 37.5 m/kg2, SD = 7.3) fell within the category of class 2 obesity (Centers for Disease Control and Prevention [CDC], 2017), which corresponds to BMIs between 35 and < 40 m/kg2, and is associated with a moderate-risk of obesity-related health risks (Jensen, 2016). Of the whole sample, 42% were married or cohabitating; 41% completed a bachelor’s degree or higher education; 45% met the threshold for clinically significant binge-eating symptoms on the BES as proposed by Greeno et al. (1995), and 34% met criteria for PTSD at the time of the study per structured diagnostic interview. White participants had significantly higher BES scores [t(87) = 2.14, p = .04] than non-white participants. Higher BMI was related to higher ORWELL-97 scores (r = .34, p = .001). No other potential covariates were significantly related to study outcome variables.
Correlations, means, and standard deviations for study variables are presented in Table 1. Scores on the PCL-C, BES, ORWELL- 97, and AAQ-II were all significantly positively correlated. Hierarchical linear regression analyses indicated that higher PCL-C scores were related to higher scores on the BES and ORWEL-97, after controlling for BMI and race (see Table 2). Effect sizes were in the medium-large range for the BES (R2 = .25) and ORWELL-97 (R2 = .30).
Table 1.
Bivariate correlations, means, and standard deviations of study variables
| Measure | 1. | 2. | 3. | 4. | M (SD) | Range |
|---|---|---|---|---|---|---|
| 1. PCL-C | - | 34.10 (15.09) |
17-79 | |||
| 2. AAQ-II | .67* | - | 19.94 (10.58) |
7-49 | ||
| 3. BES | .43* | .46* | - | 16.34 (8.87) |
0-38 | |
| 4. ORWELL-97 | .39* | .48* | .48* | - | 49.58 (29.20) |
2-138 |
Note. PCL-C = The PTSD Check list-Civilian, AAQ-II = Acceptance and Action Questionnaire–II, BES = Binge Eating Scale, ORWELL-97 = The Obesity Related Well-Being Questionnaire-97, M = Mean, SD = Standard deviation.
p < .001
Table 2.
Hierarchical linear regression analyses with PTSD symptoms predicting binge-eating symptoms and weight-related quality of life
| BES | ORWELL-97 | |||||||
|---|---|---|---|---|---|---|---|---|
| Variable | B | SE B | β | 95% CI | B | SE B | β | 95% CI |
| 1. | ||||||||
| BMI | .12 | .13 | .10 | −.13, .38 | 1.35** | .41 | .34 | .53,2.16 |
| Ethnicity | −4.42* | 2.03 | −.23 | −8.46, −.38 | −8.06 | 6.43 | −.13 | −20.85, 4.73 |
| 2. | ||||||||
| BMI | .13 | .12 | .11 | −.10, .36 | 1.36** | .37 | .34 | .63, 2.10 |
| Ethnicity | −4.66* | 1.82 | −.24 | −8.29, −1.04 | −8.81 | 5.81 | −.14 | −20.36, 2.74 |
| PCL-C | .26** | .06 | .44 | .15, .37 | .80** | .18 | .41 | .44, 1.15 |
| R 2 | .51 | .55 | ||||||
| F | 9.47** | 11.81** | ||||||
Note. B = Unstandardized beta, SE B = Standard Error of Beta, β = Standardized coefficient Beta, CI = Confident Interval, BES = Binge Eating Scale, ORWELL 97= Obesity-related well-being 97, BMI = Body mass index, PCL-C = PTSD Checklist-Civilian.
p < .05
p < .001
Mediation analyses
Results of the mediation analyses are presented in Figure 1.
Figure 1.
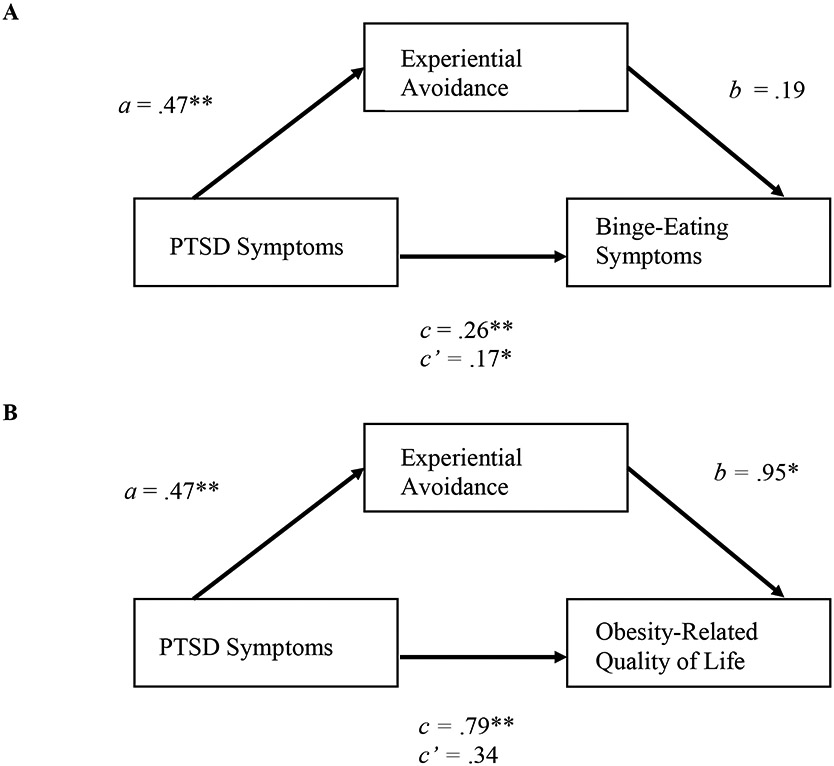
Coefficients for mediation models for binge-eating symptoms and obesity-related quality of life
Note. Model A shows the relationship between PTSD symptoms and binge-eating symptoms mediated by experiential avoidance. Model B shows the relationship between PTSD symptoms and obesity-related quality of life mediated by experiential avoidance. The paths a, b, c (total effect), and c’ (direct effect) are unstandardized regression coefficients. N = 87, Ethnicity and BMI were included as covariates for all models. * p < .05, ** p < .0001
Binge-eating symptoms.
The total effect, which is the association between PCL-C and BES scores without taking AAQ-II into account (path c), was significant (b = .26, SE = .06, t = 4.69, p < .001, [95% CI: .15, .37]). There was also a significant direct association between PCL-C and BES scores when taking AAQ-II scores into account (path c’) (b = .17, SE = .07, t = 2.24, p = .03, [95% CI: .02, .32]). The path between PCL-C and AAQ-II scores (path a) was significant and positive (b = .47, SE = .05, t = 8.65, p < .001, [95% CI: .15, .37]). The path between AAQ-II and BES scores was not significant (path b), (b = .19, SE = .11, t =1.79, p = .08 [95% CI: −.02, .41]). The indirect association between PCL-C and BES scores through AAQ-II was not significant (B = .09, SE = .06, [95% CI: −.03, .20]), indicating that AAQ-II scores did not mediate the relationship between PCL-C and BES scores.
Obesity-Related Quality of Life.
The total effect between PCL-C and ORWELL-97 scores was significant (path c) (b = .79, SE = .18, t = 4.47, p < .001, [95% CI:,.44, 1.13]). The direct association between PCL-C and ORWELL-97 was not significant, (path c’) (b = .34., SE = .23, t = 1.45, p = .15, [95% CI: −.12, .80]). The path between PCL-C and AAQ-II scores was significant and positive (path a) (b = .47., SE = .05, t = 8.65, p < .001, [95% CI: .36, .58]). The path between AAQ-II and ORWELL-97 scores was significant and positive, (path b) (b = .95, SE = .33, t = 2.84, p = .006, [95% CI: .29, 1.62]). The indirect association between PCL-C and ORWELL-97 scores was significant (B = .45, SE = .19, [95% CI: .01, .79]), indicating that AAQ-II scores mediated the relationship between PCL-C and ORWELL-97 scores.
Results in the subsample of men only (n = 69) were similar, such that patterns of significance did not differ.
Discussion
In this sample of veterans with overweight/obesity, greater PTSD symptoms were associated with greater binge-eating symptoms and poorer obesity-related quality of life. Experiential avoidance mediated the relationship between PTSD symptoms and obesity-related quality of life, but did not mediate the relationship between PTSD symptoms and binge-eating symptoms.
Our hypothesis that greater PTSD symptoms would be related to greater binge-eating symptoms and lower obesity-related quality of life was supported. These results are consistent with previous findings in male veterans indicating an association between PTSD symptoms and greater endorsement of eating disorder symptoms (Litwack et al., 2014). For example, in a sample of veterans with overweight and obesity, veterans with more clinically meaningful binge-eating behavior were more likely to have a PTSD diagnosis (Higgins et al., 2013). Additionally, in a national sample of civilians, meeting criteria for either PTSD or subthreshold PTSD was more common among both men and women with binge-eating disorder than individuals without binge-eating disorder (Mitchell et al., 2012).
The relationship between PTSD symptoms and worse obesity-related quality of life is also consistent with previous research. Studies have found a relationship between PTSD symptoms and worse health-related quality of life in civilian populations with coronary heart disease (Cohen et al., 2009) and PTSD (Pagotto et al., 2015), as well as veteran populations who are tobacco-dependent (Aversa et al., 2012), and who experienced combat during operation Enduring Freedom/Operation Iraqi Freedom (Pittman, Goldsmith, Lemmer, Kilmer, & Baker, 2012). The current study extends these findings to veterans with overweight/obesity and suggests that PTSD symptoms may specifically increase the physical symptoms, discomfort, and impact of obesity.
Our hypothesis that experiential avoidance would mediate the relationship between PTSD symptoms and obesity-related quality of life was supported. Avoidance behaviors among individuals with PTSD are associated with decreased functioning across several domains (Solomon & Mikulincer, 2007), and in one prior study experiential avoidance partially accounted for the relationship between PTSD and quality of life among civilian survivors of the Kosovo war (Kashdan et al., 2009). Kashdan et al. (2009) suggest that PTSD symptoms may contribute to moving away from valued activities, leading to worse quality of life. Our results extend this prior research by showing that experiential avoidance associated with PTSD symptoms among veterans with overweight/obesity may exacerbate the negative impacts of obesity on quality of life. Taken together, treatments targeting experiential avoidance among those with PTSD symptoms may also decrease obesity-related detriments to well-being. Third-wave psychotherapies such as ACT are promising options for those with comorbid PTSD symptoms and obesity-related problems. The ACT model theorizes that experiential avoidance, or the unwillingness to experience unwanted internal events (thoughts, emotions, and physical sensations), is at the root of many psychological and behavioral problems (Hayes, Luoma, Bond, Masuda, & Lillis, 2006). In relation to the present study, mindfulness and acceptance skills around unwanted internal events related to PTSD and weight management could be addressed to encourage adaptive behaviors associated with personal meaning (e.g., accepting feelings of hypervigilance while in public with loved ones in accordance with affiliative values; accepting urges to consume excessive food rather than attempting to avoid them by eating, in according with health values). However, additional research is needed to investigate this hypothesis.
Contrary to predictions, experiential avoidance did not mediate the relationship between PTSD symptoms and binge-eating symptoms. This is surprising given the existing literature suggesting that negative emotions associated with PTSD, such as guilt and anger, tend to precede binge-eating (Dingemans, Danner, & Parks, 2017). Previous studies with civilian and primarily female samples that suggest binge-eating functions as means to manage emotions (e.g., Dingemans et al., 2017; Keating, Mills, & Rawana, 2019) may not generalize to our primarily male veteran sample. For military personnel, binge-eating behaviors may be a means to adapt to the circumstances of military service. For example, veterans may have initially engaged in binge-eating during active duty following the use of compensatory strategies to ‘make weight’ or because of forming habits around eating quickly in response to situational demands (Masheb et al., 2019). Further, the relationship between PTSD symptoms and engaging in binge-eating may be better explained by alternative processes, such as impulsivity, which has also been associated with both PTSD (James, Strom, & Leskela, 2014; Roley, Contractor, Weiss, Armour, & Elhai, 2017) and binge-eating (Schag, Schönleber, Teufel, Zipfel, & Giel, 2013). Lastly, only approximately half of our sample met the threshold for clinically meaningful binge-eating symptoms. Therefore, our participants may have less severe deficits in the emotional regulation strategies (e.g., rumination, suppression) that have been identified in samples of participants with binge-eating disorder (Dingemans et al., 2017); however, we did not collect data to assess this. If less severe deficits in these emotional regulation strategies are identified in future work, it would imply emotion regulation is not the ideal target for these individuals, and alternative treatment targets should be identified.
Strengths of the current study include a primarily male veteran sample, which is typically underrepresented in eating disorder research. This study also contributes to the literature by demonstrating one potential mechanism – experiential avoidance – that may explain the relationship between PTSD symptoms and poor obesity-related quality of life among veterans with overweight/obesity. However, these preliminary results must be considered with caution as the study was cross-sectional and cannot be used to draw conclusions related to causality or directionality of relationships. Future research should examine these relationships longitudinally and with a larger sample size to determine directionality of relationships among PTSD symptoms, obesity-related factors, and experiential avoidance. Further, in our sample of veterans with overweight/obesity, participants were not required to meet full criteria for PTSD and/or binge-eating disorder. Consequently, the current study examines broader symptoms of trauma-related and eating disorders. Continued work examining the role of experiential avoidance in samples that meet full diagnostic criteria for BED and/or PTSD is needed to understand and inform treatments for these clinical populations. Data collection commenced before the publication of the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5). Therefore, we used the PCL-C to assess PTSD, which was developed based on DSM-IV criteria. Examining relationships between our study variables and DSM-5 diagnostic criteria using updated measures (e.g., the PCL-5) would help identify the role of the added mood and cognitive symptom cluster in explaining the relationships among binge-eating symptoms, experiential avoidance, and PTSD (Weathers et al., 2013). Further, experiential avoidance may play a role in other poor health behaviors associated with both PTSD and obesity, such as physical inactivity (Butryn et al., 2015; Hall et al., 2015). Ultimately, further tailoring and testing of interventions for treating comorbid eating and trauma-related concerns is needed.
The current study is the first to examine experiential avoidance as a potential mechanism explaining the relationship between the broader symptomologies of PTSD and binge-eating and obesity-related quality of life in a sample of veterans with overweight/obesity. The study provides preliminary evidence that experiential avoidance may be an underlying psychological process that explains the relationship between PTSD symptoms and obesity-related quality of life, but not binge-eating symptoms. These cross-sectional results can inform future longitudinal work seeking to identify psychological mechanisms contributing to these commonly co-occurring concerns and the development of targeted treatments to address trauma-related symptoms and binge-eating behaviors simultaneously.
References
- Afari N, Herbert MS, Godfrey KM, Cuneo JG, Salamat JS, Mostoufi S, … Wetherell JL (2019). Acceptance and commitment therapy as an adjunct to the MOVE! programme: a randomized controlled trial. Obesity Science & Practice. 10.1002/osp4.356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albano G, Rowlands K, Baciadonna L, Lo Coco G, & Cardi V (2019). Interpersonal difficulties in obesity: A systematic review and meta-analysis to inform a rejection sensitivity-based model. Neuroscience & Biobehavioral Reviews. 10.1016/j.neubiorev.2019.09.039 [DOI] [PubMed] [Google Scholar]
- Allison KC, Grilo CM, Masheb RM, & Stunkard AJ (2005). Binge eating disorder and night eating syndrome: A comparative study of disordered eating. Journal of Consulting and Clinical Psychology, 73(6), 1107–1115. 10.1037/0022-006X.73.6.1107 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). DSM-5® Handbook of Differential Diagnosis. DSM-5® Handbook of Differential Diagnosis. Arlington, VA. 10.1176/appi.books.9781585629992 [DOI] [Google Scholar]
- Aversa LH, Stoddard JA, Doran NM, Au S, Chow B, McFall M, … Baker DG (2012). PTSD and depression as predictors of physical health-related quality of life in tobacco-dependent veterans. Journal of Psychosomatic Research, 73(3), 185–190. 10.1016/j.jpsychores.2012.06.010 [DOI] [PubMed] [Google Scholar]
- Barnes RD, & Tantleff-Dunn S (2010). Food for thought: Examining the relationship between food thought suppression and weight-related outcomes. Eating Behaviors, 11(3), 175–179. 10.1016/j.eatbeh.2010.03.001 [DOI] [PubMed] [Google Scholar]
- Bartoli F, Crocamo C, Alamia A, Amidani F, Paggi E, Pini E, … Carrà G (2015). Posttraumatic Stress Disorder and Risk of Obesity. The Journal of Clinical Psychiatry, 76(10), e1253–e1261. 10.4088/JCP.14r09199 [DOI] [PubMed] [Google Scholar]
- Bertoli S, Leone A, Ponissi V, Bedogni G, Beggio V, Strepparava MG, & Battezzati A (2016). Prevalence of and risk factors for binge eating behaviour in 6930 adults starting a weight loss or maintenance programme. Public Health Nutrition, 19(1), 71–77. 10.1017/S1368980015001068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biener A, Cawley J, & Meyerhoefer C (2017). The High and Rising Costs of Obesity to the US Health Care System. Journal of General Internal Medicine, 32(S1), 6–8. 10.1007/s11606-016-3968-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, & Forneris CA (1996). Psychometric properties of the PTSD Checklist (PCL). Behaviour Research and Therapy, 34(8), 669–673. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/8870294 [DOI] [PubMed] [Google Scholar]
- Bond FW, Hayes SC, Baer RA, Carpenter KM, Guenole N, Orcutt HK, … Zettle RD (2011). Preliminary Psychometric Properties of the Acceptance and Action Questionnaire–II: A Revised Measure of Psychological Inflexibility and Experiential Avoidance. Behavior Therapy, 42(4), 676–688. 10.1016/j.beth.2011.03.007 [DOI] [PubMed] [Google Scholar]
- Breland JY, Phibbs CS, Hoggatt KJ, Washington DL, Lee J, Haskell S, … Frayne SM (2017). The Obesity Epidemic in the Veterans Health Administration: Prevalence Among Key Populations of Women and Men Veterans. Journal of General Internal Medicine, 32, 11–17. 10.1007/s11606-016-3962-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewerton TD (2007). Eating Disorders, Trauma, and Comorbidity: Focus on PTSD. Eating Disorders, 15(4), 285–304. 10.1080/10640260701454311 [DOI] [PubMed] [Google Scholar]
- Butryn ML, Arigo D, Raggio GA, Kaufman AI, Kerrigan SG, & Forman EM (2015). Measuring the Ability to Tolerate Activity-Related Discomfort: Initial Validation of the Physical Activity Acceptance Questionnaire (PAAQ). Journal of Physical Activity and Health, 12(5), 717–726. 10.1123/jpah.2013-0338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2017). About Adult BMI. Retrieved July10, 2019, from https://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html [Google Scholar]
- Cohen BE, Marmar CR, Neylan TC, Schiller NB, Ali S, & Whooley MA (2009). Posttraumatic stress disorder and health-related quality of life in patients with coronary heart disease: Findings from the heart and soul study. Archives of General Psychiatry, 66(11), 1214–1220. 10.1001/archgenpsychiatry.2009.149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Zwaan M, Lancaster KL, Mitchell JE, Howell LM, Monson N, Roerig JL, & Crosby RD (2002). Health-related quality of life in morbidly obese patients: Effect of gastric bypass surgery. Obesity Surgery, 12(6), 773–780. 10.1381/096089202320995547 [DOI] [PubMed] [Google Scholar]
- Dingemans A, Danner U, & Parks M (2017, November 22). Emotion regulation in binge eating disorder: A review. Nutrients. MDPI AG. 10.3390/nu9111274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon JB (2010). The effect of obesity on health outcomes. Molecular and Cellular Endocrinology, 316(2), 104–108. 10.1016/J.MCE.2009.07.008 [DOI] [PubMed] [Google Scholar]
- Dorflinger LM, Ruser CB, & Masheb RM (2017). A brief screening measure for binge eating in primary care. Eating Behaviors, 26, 163–166. 10.1016/j.eatbeh.2017.03.009 [DOI] [PubMed] [Google Scholar]
- Fulton JJ, Calhoun PS, Wagner HR, Schry AR, Hair LP, Feeling N, … Beckham JC (2015, April 1). The prevalence of posttraumatic stress disorder in Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) Veterans: A meta-analysis. Journal of Anxiety Disorders. Elsevier Ltd. 10.1016/j.janxdis.2015.02.003 [DOI] [PubMed] [Google Scholar]
- Gormally J, Black S, Daston S, & Rardin D (1982). The assessment of binge eating severity among obese persons. Addictive Behaviors, 7(1), 47–55. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/7080884 [DOI] [PubMed] [Google Scholar]
- Greeno CG, Marcus MD, & Wing RR (1995). Diagnosis of binge eating disorder: Discrepancies between a questionnaire and clinical interview. International Journal of Eating Disorders, 17(2), 153–160. [DOI] [PubMed] [Google Scholar]
- Hall KS, Hoerster KD, & Yancy WS (2015). Post-Traumatic Stress Disorder, Physical Activity, and Eating Behaviors. Epidemiologic Reviews, 37(1), 103–115. 10.1093/epirev/mxu011 [DOI] [PubMed] [Google Scholar]
- Hayes SC, Luoma JB, Bond FW, Masuda A, & Lillis J (2006). Acceptance and Commitment Therapy: Model, processes and outcomes. Behaviour Research and Therapy, 44(1), 1–25. 10.1016/j.brat.2005.06.006 [DOI] [PubMed] [Google Scholar]
- Higgins DM, Dorflinger L, MacGregor KL, Heapy AA, Goulet JL, & Ruser C (2013). Binge eating behavior among a national sample of overweight and obese veterans. Obesity, 21(5), 900–903. 10.1002/oby.20160 [DOI] [PubMed] [Google Scholar]
- Holzer SR, Uppala S, Wonderlich SA, Crosby RD, & Simonich H (2008). Mediational significance of PTSD in the relationship of sexual trauma and eating disorders. Child Abuse & Neglect, 32(5), 561–566. 10.1016/j.chiabu.2007.07.011 [DOI] [PubMed] [Google Scholar]
- James LM, Strom TQ, & Leskela J (2014). Risk-taking behaviors and impulsivity among veterans with and without PTSD and mild TBI. Military Medicine, 179(4), 357–363. 10.7205/MILMED-D-13-00241 [DOI] [PubMed] [Google Scholar]
- Jensen M (2016). Obesity. In Goldman L & Schafer A (Eds.), Goldman-Cecil Medicine (25th ed.). Philadelphia,: Elsevier Saunders. [Google Scholar]
- Jia H, & Lubetkin EI (2005). The impact of obesity on health-related quality-of-life in the general adult US population. Journal of Public Health, 27(2), 156–164. 10.1093/pubmed/fdi025 [DOI] [PubMed] [Google Scholar]
- Kang HK, Natelson BH, Mahan CM, Lee KY, & Murphy FM (2003). Post-traumatic stress disorder and chronic fatigue syndrome-like illness among gulf war veterans: A population-based survey of 30,000 veterans. American Journal of Epidemiology, 157(2), 141–148. 10.1093/aje/kwf187 [DOI] [PubMed] [Google Scholar]
- Kashdan TB, Morina N, & Priebe S (2009). Post-traumatic stress disorder, social anxiety disorder, and depression in survivors of the Kosovo War: experiential avoidance as a contributor to distress and quality of life. Journal of Anxiety Disorders, 23(2), 185–196. 10.1016/j.janxdis.2008.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keating L, Mills JS, & Rawana JS (2019). Momentary predictors of binge eating: An attachment perspective. Eating Behaviors, 32, 44–52. 10.1016/j.eatbeh.2018.12.003 [DOI] [PubMed] [Google Scholar]
- Lecrubier Y, Sheehan DV, Weiller E, Amorim P, Bonora I, Sheehan KH, … Dunbar GC (1997). The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: Reliability and validity according to the CIDI. European Psychiatry, 12(5), 224–231. 10.1016/S0924-9338(97)83296-8 [DOI] [Google Scholar]
- Lillis J, Hayes SC, Bunting K, & Masuda A (2009). Teaching Acceptance and Mindfulness to Improve the Lives of the Obese: A Preliminary Test of a Theoretical Model. Annals of Behavioral Medicine, 37(1), 58–69. 10.1007/s12160-009-9083-x [DOI] [PubMed] [Google Scholar]
- Lillis J, Hayes SC, & Levin ME (2011). Binge eating and weight control: The role of experiential avoidance. Behavior Modification, 35(3), 252–264. 10.1177/0145445510397178 [DOI] [PubMed] [Google Scholar]
- Lillis J, Levin ME, & Hayes SC (2011). Exploring the relationship between body mass index and health-related quality of life: A pilot study of the impact of weight self-stigma and experiential avoidance. Journal of Health Psychology, 16(5), 722–727. 10.1177/1359105310388321 [DOI] [PubMed] [Google Scholar]
- Lillis J, Luoma JB, Levin ME, & Hayes SC (2010). Measuring Weight Self-stigma: The Weight Self-stigma Questionnaire. Obesity, 18(5), 971–976. 10.1038/oby.2009.353 [DOI] [PubMed] [Google Scholar]
- Litwack SD, Mitchell KS, Sloan DM, Reardon AF, & Miller MW (2014). Eating disorder symptoms and comorbid psychopathology among male and female veterans. General Hospital Psychiatry, 36(4), 406–410. 10.1016/j.genhosppsych.2014.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannucci E, Ricca V, Barciulli E, Di Bernardo M, Travaglini R, Cabras PL, & Rotella CM (1999). Quality of life and overweight: the obesity related well-being (Orwell 97) questionnaire. Addictive Behaviors, 24(3), 345–357. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10400274 [DOI] [PubMed] [Google Scholar]
- Marmar CR, Schlenger W, Henn-Haase C, Qian M, Purchia E, Li M, … Kulka RA (2015). Course of posttraumatic stress disorder 40 years after the Vietnamwar findings from the national Vietnam veterans longitudinal study. JAMA Psychiatry, 72(9), 875–881. 10.1001/jamapsychiatry.2015.0803 [DOI] [PubMed] [Google Scholar]
- Masheb RM, Kutz AM, Marsh AG, Min KM, Ruser CB, & Dorflinger LM (2019). “Making weight” during military service is related to binge eating and eating pathology for veterans later in life. Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity. 10.1007/s40519-019-00766-w [DOI] [PubMed] [Google Scholar]
- Masheb RM, Lutes LD, Myra Kim H, Holleman RG, Goodrich DE, Janney CA, … Damschroder LJ (2015). High-frequency binge eating predicts weight gain among veterans receiving behavioral weight loss treatments. Obesity, 23(1), 54–61. 10.1002/oby.20931 [DOI] [PubMed] [Google Scholar]
- Mason SM, Frazier PA, Austin SB, Harlow BL, Jackson B, Raymond NC, & Rich-Edwards JW (2017). Posttraumatic Stress Disorder Symptoms and Problematic Overeating Behaviors in Young Men and Women. Annals of Behavioral Medicine, 51(6), 822–832. 10.1007/s12160-017-9905-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell KS, Mazzeo SE, Schlesinger MR, Brewerton TD, & Smith BN (2012, April). Comorbidity of partial and subthreshold PTSD among men and women with eating disorders in the national comorbidity survey-replication study. International Journal of Eating Disorders. 10.1002/eat.20965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagotto LF, Mendlowicz MV, Coutinho ESF, Figueira I, Luz MP, Araujo AX, & Berger W (2015). The impact of posttraumatic symptoms and comorbid mental disorders on the health-related quality of life in treatment-seeking PTSD patients. Comprehensive Psychiatry, 58, 68–73. 10.1016/j.comppsych.2015.01.002 [DOI] [PubMed] [Google Scholar]
- Pittman JOE, Goldsmith AA, Lemmer JA, Kilmer MT, & Baker DG (2012). Post-traumatic stress disorder, depression, and health-related quality of life in OEF/OIF veterans. Quality of Life Research, 21(1), 99–103. 10.1007/s11136-011-9918-3 [DOI] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers, 36(4), 717–731. 10.3758/BF03206553 [DOI] [PubMed] [Google Scholar]
- Roley ME, Contractor AA, Weiss NH, Armour C, & Elhai JD (2017). Impulsivity facets’ predictive relations with DSM-5 PTSD symptom clusters. Psychological Trauma: Theory, Research, Practice, and Policy, 9(1), 76–79. 10.1037/tra0000146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberger PH, & Dorflinger L (2013). Psychosocial factors associated with binge eating among overweight and obese male veterans. Eating Behaviors, 14(3), 401–404. 10.1016/j.eatbeh.2013.06.006 [DOI] [PubMed] [Google Scholar]
- Schag K, Schönleber J, Teufel M, Zipfel S, & Giel KE (2013). Food-related impulsivity in obesity and Binge Eating Disorder - a systematic review. Obesity Reviews, 14(6), 477–495. 10.1111/obr.12017 [DOI] [PubMed] [Google Scholar]
- Scott KM, McGee MA, Wells JE, & Oakley Browne MA (2008). Obesity and mental disorders in the adult general population. Journal of Psychosomatic Research, 64(1), 97–105. 10.1016/j.jpsychores.2007.09.006 [DOI] [PubMed] [Google Scholar]
- Short NA, Boffa JW, Clancy K, & Schmidt NB (2018). Effects of emotion regulation strategy use in response to stressors on PTSD symptoms: An ecological momentary assessment study. Journal of Affective Disorders, 230, 77–83. 10.1016/j.jad.2017.12.063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slane JD, Levine MD, Borrero S, Mattocks KM, Ozier AD, Silliker N, … Haskell SG (2016). Eating behaviors: Prevalence, psychiatric comorbidity, and associations with body mass index among male and female Iraq and Afghanistan Veterans. Military Medicine, 181(11), e1650–e1656. 10.7205/MILMED-D-15-00482 [DOI] [PubMed] [Google Scholar]
- Smith BN, Tyzik AL, Neylan TC, & Cohen BE (2015). PTSD and obesity in younger and older veterans: Results from the mind your heart study. Psychiatry Research, 229(3), 895–900. 10.1016/J.PSYCHRES.2015.07.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon Z, & Mikulincer M (2007). Posttraumatic intrusion, avoidance, and social functioning: A 20-year longitudinal study. Journal of Consulting and Clinical Psychology, 75(2), 316–324. 10.1037/0022-006X.75.2.316 [DOI] [PubMed] [Google Scholar]
- Talbot LS, Maguen S, Epel ES, Metzler TJ, & Neylan TC (2013). Posttraumatic stress disorder is associated with emotional eating. Journal of Traumatic Stress, 26(4), 521–525. 10.1002/jts.21824 [DOI] [PubMed] [Google Scholar]
- Tapper K, Shaw C, Ilsley J, Hill AJ, Bond FW, & Moore L (2009). Exploratory randomised controlled trial of a mindfulness-based weight loss intervention for women. Appetite, 52(2), 396–404. 10.1016/j.appet.2008.11.012 [DOI] [PubMed] [Google Scholar]
- Valente S, Di Girolamo G, Forlani M, Biondini A, Scudellari P, De Ronchi D, & Atti AR (2017). Sex-specific issues in eating disorders: a clinical and psychopathological investigation. Eating and Weight Disorders, 22(4), 707–715. 10.1007/s40519-017-0432-7 [DOI] [PubMed] [Google Scholar]
- Vieweg WVR, Julius DA, Bates J, Quinn JF, Fernandez A, Hasnain M, & Pandurangi AK (2007). Posttraumatic stress disorder as a risk factor for obesity among male military veterans. Acta Psychiatrica Scandinavica, 116(6), 483–487. 10.1111/j.1600-0447.2007.01071.x [DOI] [PubMed] [Google Scholar]
- Weathers F, Litz B, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013). The PTSD Checklist for DSM-5 (PCL-5). National Center for PTSD, 5(August), 2002. 10.1037/t02622-000 [DOI] [Google Scholar]
- Weineland S, Lillis J, & Dahl J (2013). Measuring experiential avoidance in a bariatric surgery population—Psychometric properties of AAQ-W. Obesity Research & Clinical Practice, 7(6), e464–e475. 10.1016/j.orcp.2012.06.002 [DOI] [PubMed] [Google Scholar]


