Abstract
Background: The Willingness to pay (WTP) for and acceptance of cervical cancer prevention (CCP) methods have an important role in the control of this type of cancer. Therefore, the aim of this study was to estimate the WTP and acceptance of CCP methods with the contingent valuation method (CVM).
Methods: In this systematic review and meta-analysis study, the required information was collected by searching relevant keywords in PubMed, Scopus, Embase, Web of Knowledge, and their Persian equivalent in the Scientific Information Database (SID) and Elmnet databases during January 1, 2000 to June 30, 2020. All studies that reported the WTP and CCP methods with the CVM in English or Persian were included. The reporting quality of studies was assessed by strengthening the Reporting of Observational Studies in Epidemiology (STROBE). Comprehensive meta-analysis (CMA: 2) software was used to conduct the meta-analysis. The content analysis method was used for qualitative data analysis.
Results: Finally, 28 articles (with 49610 people) were included in the study. Most of the participants were women (35.7%). The HPV vaccine was the most common method of prevention (75%). The overall acceptance rate was 64% and the overall positive WTP rate was 66%. The average WTP was US$30.44, which accounts for about 0.84% of GDP per capita. The most significant effective factors included income, age, education, high-risk sexual behaviors, and awareness of cervical cancer, belief in the risk of cervical cancer, and belief about the effectiveness of prevention methods. The cost was the most important reason for the unwillingness to pay and accept.
Conclusion: Results show that the WTP and acceptance rate of CCP methods are relatively high. It is recommended to reduce the cost of prevention methods, especially the HPV vaccine, and to increase awareness and improve the attitude of people. Also, it is recommended to consider other methods of estimation of WTP and other cancers in future studies.
Keywords: Acceptance, Preventive Measures, Cervical Cancer, Human Papillomavirus Vaccine
↑ What is “already known” in this topic:
In recent years, many studies have been conducted on the willingness to pay (WTP) and acceptance rate of cervical cancer prevention (CCP) methods. However, based on the results of reviewing the literature, the results of these studies were not systematically collected and analyzed.
→ What this article adds:
According to the results of this study, it is recommended that attentions should be paid to reducing the cost of preventive measures, focusing on target age groups; and reducing risky sexual behaviors to increase the WTP and acceptance of CCP methods.
Introduction
Over the past 2 decades, with the expansion of primary health care, success in controlling infectious diseases, covering more than 90% of the population, and changing population structure has increased the prevalence of noncommunicable diseases such as cancer (1). Cancers are now one of the major problems of health systems around the world (2). More than 70% of all cancer-related deaths occur in low- and middle-income countries (LMICs). Mathers and Loncar (2006) results showed that global cancer deaths will be increase, with 11.5 million deaths in 2030 (3). Today, cancers are plaguing these countries with increasing attenuation in LMICs as well as in high-income countries (HICs).
One of the most important types of cancers is cervical cancer, which is the second leading cause of mortality for women after breast cancer at the age of 15 to 44 years. Even in many LMICs, cervical cancer is the most common cause of cancer deaths, with half a million new cases diagnosed worldwide each year, with nearly 250 000 deaths (4). Relatively effective methods are available today in the management of this cancer (5).
Many different tests and methods have been developed for the early detection and prevention of cervical cancer (6). Most of these methods are highly effective and are among the simple, low-cost, painless, and high- effectiveness prevention methods (7).
Despite these benefits of cervical cancer prevention (CCP) methods, the results of the previous studies show that these methods are not well-liked and accepted. Also, for a variety of reasons, including financial problems, people have a little willingness to pay (WTP) for these methods (8-10).
In economics, the WTP is the highest price a person is willing to pay for a unit more than a service or good (11). Various methods have been used to measure WTP; one of the most common and widely used methods is the contingent valuation method (CVM). In this method, people are asked to state the maximum amount of money that they are willing to pay for a particular product that may not be purchased (nonconsumable). In other words, this method specifies the maximum price that a person is WTP to buy a product or receive health services (12).
In recent years, especially with the production and use of human papillomavirus (HPV) vaccines, many studies have been conducted on the WTP and acceptance rate of CCP methods (13-15). However, the results of these studies were not systematically collected and analyzed. The availability of such information is critical for effective decision-making and planning to help implement or develop cancer prevention programs. Therefore, the purpose of this study was to estimate the WTP and the acceptance of different methods of CCP using the CVM method.
Methods
This systematic review and meta-analysis study was conducted in 2020. In this study, authors used the systematic review guide book entitled “Systematic Review to Support Evidence-Based Medicine" (16) and the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement (17).
Search Strategy
The search strategy in this study was developed and implemented by an experienced and knowledgeable librarian with the guidance of an expert in the subject area (Appendix 1).
The required information was collected by searching relevant keywords and medical subject heading (Mesh) terms in 4 subjects in PubMed, Scopus, Embase, Web of Knowledge, and their Persian equivalent have been searched in the scientific information database (SID) and Elmnet database.
The timeframe selected for searching the articles was January 1, 2000 to June 30, 2020. To identify and cover most articles published after searching the databases, some prestigious journals (the European Journal of Cancer Prevention, Cancer Prevention Research, the Asian Pacific Journal of Cancer Prevention, Cancer Communications, BMC Cancer, Cancer Epidemiology, the International Journal of Cancer Management, etc.) in the field of study and the Google Scholar search engine were also searched manually. After excluding studies that had little relevance to the study objectives, to increase the certainty of identifying and reviewing existing studies, reference checks of selected articles, Gray literature review (European Association for Grey Literature Exploitation (EAGLE), and Health Care Management Information Consortium (HMIC)) was done. Finally, all relevant articles were collected by contacting an expert.
Inclusion and Exclusion Criteria
All studies that reported the WTP and CCP methods with the CVM in English or Persian were included in the study.
Evaluation of the Reports on the Quality of Articles
The quality of reporting of included studies was evaluated by 2 independent reviewers using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist (18). In this study, minor modifications were made to the questions, and finally, 33 items were measured. The checklist options included "Yes", "No", "Not Applicable" and "Unclear". Cases of disagreement between the reviewers were referred to a third person who had more knowledge and experience in the methodological issues of the research.
Data Extraction
To extract data, 2 data extraction forms were designed in Word: 2013 software (one for extracting general specifications of studies and the other for extracting studies results). The general profile form of studies included author, year, country, the purpose of study, study design, participants: N (response rate), data collection tool, type of test, administration, type of questions and type of information. Information on the results of the study form included the demographic characteristics of participants, % of acceptance of the test, % of positive WTP, WTP (US$) mean ± SD OR median (CR), WTP as a % of gross domestic product (GDP) per capita, other results of variable effects in WTP (significant positive, significant negative, and nonsignificant) were the main reasons for no WTP (%). Initially, the data of 5 papers were extracted experimentally and the shortcomings and problems in the original form were eliminated.
Data Analysis Methods
A meta-analysis was used to estimate the quantitative data (acceptance of CCP methods, WTP for CCP methods, and percentage of WTP per capita GDP). CMA: 2 (Comprehensive Meta-Analysis) software was used to perform the meta-analysis with a random effect model. Forest plot diagrams were used to report the results. Q and I2 tests were used to measure the heterogeneity of the results. In this study, with I2 more than 50%, the heterogeneity of articles was determined.
To calculate the WTP, the countries' currency value reported in studies was converted to US dollars (in study published year) using a free online website (19). In cases where the year of the study was not reported, the baseline year was considered 1 year before the study was published. In some studies, the values were not reported as central indexes (mean or median) indices (were reported as intervals), in which case the intermediate interval was used as the WTP. In some studies, the values were reported as a percentage of the participants (eg, 65% of participants have X amount of WTP); in such cases, the reported amount was chosen as the baseline. Also, to calculate the percentage of WTP from GDP per capita, the amount of WTP was divided by GDP per capita in the year of the study or 1 year before the study was published. The World Bank data were used as a basis for calculating GDP per capita and country segmentation based on economic status (20).
Given how the results were reported on the monetary amounts (in US dollars) that individuals were willing to pay, the researchers decided to convert the reported values in mean± SD to mean (95% confidence interval) format using the Z statistics method by online tools. Studies that reported the median or only 1 number (without SD or CI) were not included in the meta-analysis.
Content-analysis methods were used for qualitative data analysis, which is a method for identifying, analyzing, and reporting patterns within themes and is widely used in qualitative data analysis (21). Data were analyzed by 2 researchers. The steps for analyzing and coding the data were as follows: familiarity with the content of the articles (reading multiple times extracted data); identifying and extracting primary codes (identifying and extracting data more relevant to the primary codes); identifying themes (Inserting extracted primary codes into related themes); reviewing and completing identified themes; naming and defining themes; and ensuring the reliability of the extracted codes and themes (agreeing between the 2 coders through discussion and fixing Disputes).
Results
Out of the 3118 articles found from the databases and other sources, 1879 were excluded due to duplication between databases. In the title and abstract screening phase, 1168 cases were also excluded. A total of 43 studies were excluded from the full-text review, and finally, 28 articles were included in the study, of which 26 were included in the meta-analysis (Fig. 1).
Fig. 1.

Search and screening process for articles
The characteristics and results of the reviewed articles are presented in (Tables 1 and 2).
Table 1. Characteristics of Included Studies .
| Author, year country | Aim of study |
Study design |
Participants: N (response rate) | Data collection tool | Type of prevention methods | Administration | Type of questions | Informed by …. information | Type of information |
| 1. Wordsworth S, et al: 2001: Scotland(22) | Assess the value of the cervical smear test to women, | A Postal Survey | Women aged 20-59: 595 (30) | Questionnaire | Pap-smear | Mailed |
Payment card technique |
General |
Time of cervical smear, method of carrying out screening, time between smears time for results, chance of being recalled, chance of having an abnormality, chance of dying having an abnormality will result in a need for further smears |
| 2. Choi HCW et al, 2013: Hong Kong(23) | Provide a more representative and updated assessment on the acceptability of female adoles- cent HPVvaccination | Survey |
Mothers with daughters aged ≤18 years’ in 2008 year: 1022 (39.3) In 2012 year: 1005 (50.2) Adolescent schoolgirl: 2252 (93.4) |
Random digit-dialing telephone interviewing | HPV vaccination | Telephone interviewing | Open ended | General |
HPVvaccineand its market price range |
| 3. Rajiah K et al, 2015: Malaysia(18) |
Evaluate the knowledge, attitude, practice and to find out the willingness to pay for HPV vaccination |
Cross-Sectional Study |
University students studying health sciences: 273 (85.3) |
Self-administered validated questionnaire |
HPV vaccination | Telephone interviewing | - | - | - |
| 4. Tarekegn AA, et al, 2019: Ethiopia(24) | Willingness to pay and associated factors for cervical cancer screening program | Cross-Sectional Study | Female health professionals in the College of Medicine and Health Sciences: 392 (92.7) | Questionnaire | Screening service | Face-to-face |
Double- Bounded Dichotomous Choice |
- | - |
| 5. Tarekegn AA and Yismaw AE, 2019: Ethiopia (25) | Willingness to accept and pay, and associated factors for human papilloma virus vaccination | Cross-Sectional Study | Female health professionals in the College of Medicine and Health Sciences: 392 (92.7) | Questionnaire | HPV vaccination | Face-to-face |
Double- Bounded Dichotomous Choice |
- | - |
| 6. Philips Z,et al, 2003: UK (17) |
Delineate their knowledge of cervical cancer and screening and valuation of the introduction of HPV testing |
Cross-Sectional Study |
female students at the University of Nottingham: 222 (44.4) |
Questionnaire | HPV vaccination | Mailed |
payment card technique |
- | - |
| 7. Hoque ME et al, 2013: South Africa(26) |
Assess the awareness of CC and its risk factors and to determine the level of acceptability of HPV vaccination |
Cross-Sectional Study | undergraduate female students: 440 (97.7) | Questionnaire | HPV vaccination | Face-to-face | - | - | - |
| 8. Maharajan MK et al, 2015: Malaysia (27) |
To assess the knowledge and determine variation between different cultural groups, WTP for cervical cancer vaccination and the relationships between knowledge and attitudes towards HPV vaccination |
Cross-Sectional Study | Ethnically Diverse Medical Students: 302 (99) | Questionnaires | HPV vaccination | Face-to-face | - | - | - |
| 9. Kruiroongroj S et al, 2014: Thailand(28) |
Examine the level of knowledge, attitude, acceptance, and WTP for HPV vaccination |
Cross-Sectional Study | Female parents of girls aged 12-15 years: 861 (71.7) | Questionnaires | HPV vaccination | Face-to-face |
Payment card technique-open-ended |
- | - |
| 10. Songthap A et al, 2012: Thailand(29) |
Assess the knowledge and attitudes about HPV and cervical cancer, and the acceptability of HPV vaccine |
Cross-Sectional Study |
Students: 644(80.5) Parents: 664 (83) Teachers: 304 (76) |
Questionnaires | HPV vaccination | Face-to-face | Closed-ended | - | - |
| 11. Alder S et al, 2015: Argentina (30) |
explore maternal HPV vaccination acceptance, WTP for HPV vaccination and correlates of this willingness, awareness of HPV and HPV-associated disease and behaviors and attitudes Associated with HPV vaccination acceptance. |
cross-sectional study | mothers of girls aged 9-15 year: 180 (85.3) | questionnaires | HPV vaccination | face-to-face | - | General | natural history of HPV and cervical cancer |
| 12. Dinh Thu H et al, 2018: Vietnam (31) | Identifying mothers’ WTP for HPV vaccine for daughters, and the associated factors | Cross-Sectional Study | married women 15--49 years old: 606(96) | Questionnaires | HPV vaccination | Face-to-face | open ended | - | - |
| 13. Umeh IB et al, 2016: Nigeria (16) | Assessed Nigerian mothers’ WTP for HPV vaccine. | Cross-Sectional Study | Mothers has girls aged 9–12: 438 (88) | Questionnaires | HPV vaccination | Face-to-face | open ended-payment card technique | - | - |
| 14. Philips Z et al, 2006: UK (32) |
Experiment to test the construct validity of contingent valuation, by eliciting women’s valuations for the NHS cervical cancer screening programme |
Randomised Experiment |
women eligible for cervical screening during routine (non-screening) consultations: 1524 (25.4) |
Questionnaires | Screening service | Face-to-face |
payment scale-(open-ended) |
General and detailed |
Risk factors, incidence, screening efficacy, HPV testing as triage for low-grade abnormal smears and explained the potential benefits and uncertainties associated with its Implementation. |
| 15. Yan Yuen WW et al, 2018: Hong Kong (33) |
Assessing the feasibility of delivering the HPV vaccine to girls through a school-based program in Hong Kong, as well as to examine the facilitators and barriers associated with their participation |
Cross-Sectional Study |
girls aged 9 to 14: 1147 (89.9) parents: 1160 (90.9) |
Questionnaires | HPV vaccination | Face-to-face | - | - | - |
| 16. Liao CH et al, 2009: Taiwan (34) |
Apply the CVM to elicit the WTP, and measure the value of a statistic life (VSL), for HPV vaccine |
Cross-Sectional Study |
women aged 20–55 years with at least one daughter: 512 |
Questionnaires | HPV vaccination | Face-to-face |
double-bounded binary-choice |
General | - |
| 17. Raab SS et al, 2002:USA (35) |
WTP for New Papanicolaou Test Technologies and influence factors |
cross-sectional study |
female patients who attended obstetrics-gynecology practices: 175 |
questionnaires | (liquid-based) Papanicolaou (Pap) test | face-to-face |
payment card technique |
detailed |
conventional Pap smear screening, the, impact of Pap smear screening, the current average risk of dying of CC, new Pap tests and their potential benefits, charges for conventional and liquid-based Pap tests, and the risks for an average American of dying of a variety of other causes (e.g., particular diseases, Accidents, natural disasters). |
| 18. Dahlström LA et al, 2010: Sweden (36) |
Investigated correlates of attitudes to HPV vaccination |
Population-Based Survey |
Parents of children aged 12–15 years: Parents of girls: 11187 (70%) Parents of boys: 2759 (69%) |
Questionnaires | HPV vaccination |
Online face-to-face Telephone interview |
- | - | - |
| 19. Oh JK et al, 2010: Korea (37) |
Awareness and acceptance of HPV infection and vaccination for CC prevention, as well as factors associated with willingness to be administered the HPV vaccine |
Population-Based Survey | Male (496) and female (504) adults: 1000 (27.3) | Questionnaires | HPV vaccination | Face-to-face |
Closed-ended questionnaire including some multiple choice question |
- | - |
| 20. Rajiah K et al, 2017: Malaysia (38) |
Determine the influence of dental students’ knowledge and attitude regarding HPV infection of CC on WTP for vaccination |
Cross-Sectional Study |
Final year dental students from the School of Dentistry: 142 (94.7) |
Questionnaires | HPV vaccination | Face-to-face | Opened-ended questions | - | - |
| 21. Tran BX et al, 2018: Vietnam (39) | investigate barriers related to knowledge–attitude–practice (KAP) about the HPV vaccine and WTP for the vaccine | cross-sectional study | vaccination service users: 492 | questionnaires | HPV vaccination | face-to-face | Double-bounded dichotomous-choice questions with open-ended questions | - | - |
| 22. Touch S and Oh JK, 2018: Cambodia (40) |
examine the cervical cancer knowledge, attitudes, and practices as well as cervical cancer prevention methods |
cross-sectional study | women aged 20–69 years: 440(98.8) | questionnaires | HPV vaccination | face-to-face interview survey |
close-ended, multiple-choice responses and open-ended |
- | - |
| 23. Opoku CA et al, 2016: Ghana (41) | assessed the perception of risk of CC and existence of risk factors for CC | cross-sectional study |
women had to be between the ages of 18-45 years: 300 (98.4) |
semistructured questionnaire |
screening service | face-to-face interview survey | - | - | - |
| 24. Lin Y et al, 2020:China (42) | investigate acceptance and willingness to pay for HPV vaccination among adult women in China | cross-sectional study | mothers aged 27–45 years of primary school pupils: 2339 (62) | questionnaires | HPV vaccines | online | open ended single bounded dichotomous-choice-open ended | - | - |
| 25. You D et al, 2020: China (43) | determine HPV vaccine uptake and willingness to receive HPV vaccination | cross-sectional survey | female college students: 4220 | questionnaires | HPV vaccines | online | - | - | - |
| 26.Lin W et al, 2020: China(44) | Valuate the differences on awareness and attitude towards HPV and its vaccine between local and migrant residents who participated in CC screening | Cross-Sectional Survey | women aged from 21 to 60 years: 9855 (93.8) | Questionnaires | HPV vaccines | Face-to-face | Open ended | - | - |
| 27.Kristina S et al, 2020: Indonesia(45) | Examine the perception of seriousness and knowledge of CC risk and to evaluate the WTP for CC screening | Community based cross-sectional survey | women who visited clinics or pharmacies: 675 | Questionnaires | Screening service | Face-to-face | Bid contingent valuation method | - | - |
| 28.Weng Q et al, 2020: Tanzania (21) | Describe women’s awareness of CC and to explore the attitudes toward, acceptability of and barriers to CC | Cross-sectional | women aged 14–65 years old: 1483 (98.8) | Questionnaires | Screening service | Face-to-face | Closed-response questions | - | - |
Table 2. Results of Included Studies .
| Author, year country | Demographic characteristics of participants | % of acceptance of test | % of Positive WTP | WTP (US$) M±SD OR median (CR) |
WTP as a % of GDP per capita |
Other results |
InfluencedVariables effects in WTP |
Main reason for no WTP (%) | |
| Significant positive | non-significant | ||||||||
|
1. Wordsworth S et al, 2001: Scotland (22) |
Mean age: 38 Income range of £10 000 ± £25 000. |
- | 89.3 | 80.8±51.5 | 0.49 | Zero value=10.7% of participants |
➢ Income |
➢ Age ➢ Smear status |
|
|
2. Choi HCW et al, 2013: Hong Kong(23) |
83% of mother has more than 35 years |
Schoolgirls: 27.1 Mothers 2008: 27.5 Mothers 2012: 37.6 |
Schoolgirls:54.8 Mothers 2008:44.6 Mothers 2012:66.7 |
Schoolgirls:38 (13–128) Mothers 2008: 128 (77-192 ) Mothers 2012: 128 (64-192) |
Schoolgirls:0.12 Mothers 2008:0.40 Mothers 2012: 0.40 |
Perceived minimum age appropriate for vaccination (years): Schoolgirls:12 Mothers 2008:15 Mothers 2012:14 |
Mothers: ➢ Had heard of HPV vaccines before ➢ Monthly household income ≥2564 ➢ Age of daughters: <9 years ➢ Perception on the health of daughters: Good/Very good/Excellent Schoolgirls: ➢ Had heard of HPV before ➢ Risky sexual behaviors ➢ Education attainment ➢ Age: >13 |
Mothers: ➢ Had heard of HPV before ➢ Identified HPV infection as risk factor ➢ Monthly household income 1282–2564 ➢ Education: Secondary ➢ Education: Tertiary or above ➢ History of cervical screening without symptoms Schoolgirls: ➢ Had heard of HPV vaccines before ➢ Identified HPV infection as risk factor Monthly household income ➢ Self-rated health: Good/Very good/Excellent |
|
|
3. Rajiah K et al, 2015: Malaysia (18) |
mean age: 22.2 |
83.8 | 86 | 108.66 | 0.97 |
- Almost all the students wanted the vaccine to be cost free - Almost half of the respondents were willing to spend around USD 200 for their children |
- | - | Cost |
|
4. Tarekegn AA, et al, 2019: Ethiopia (24) |
mean age: 28 years Average monthly income: US$ 226 |
- | 83.4 | 7.12±4.83 | 0.91 | 34.6% of participants were WTP more than US$11 |
➢ Age>30years ➢ perceived seriousness of cervical cancer ➢ perceived quality of cervical screening service ➢ educational status ➢ monthly income |
➢ Marital status ➢ Religion ➢ Ethnicity ➢ Background profession ➢ Knowledge ➢ Health Status ➢ Source of more Information |
|
|
5. Tarekegn AA and Yismaw AE, 2019: Ethiopia (25) |
mean age: 28 years Average monthly income: US $ 226 |
- | 85.9 | 8.46±4.83 | 1.09 | 36.6% of participants were WTP more than US$11 |
➢ Age ➢ educational status ➢ Knowledge about cervical cancer and its risk factors ➢ monthly income |
➢ Marital status ➢ Background profession ➢ Knowledge ➢ Health status ➢ Perceived seriousness cervical cancer |
|
|
6. Philips Z,et al, 2003: UK (17) |
mean age: 18.9 years about 80% received annual incomes of less than £5000 per annum, |
- | - | 35.92± 32.01 | 0.12 |
WTP for 10% increase in screening accuracy: US$22.16 |
➢ WTP for routine smear test (£) ➢ Proportion of smears testing normal ➢ Perceived above average risk of cervical cancer |
➢ Accuracy of smear test ➢ Age where most abnormal results occur ➢ Current smoker |
|
|
7. Hoque ME et al, 2013: South Africa (26) |
mean age: 20.3 years 63% of the students were sexually Experienced. |
77.3 | - | - | - | - |
➢ Age more than 21 ➢ knew about the Pap smear test ➢ were aware that having multiple sex partners ➢ sexual intercourse before the age of 18 years ➢ smoking ➢ having contracted any STDs |
- |
|
|
8. Maharajan MK et al, 2015: Malaysia (27) |
mean age: 23.5 years 56.2% reported as being in a relationship |
89.7 | 87.75 | 152.48 | 1.34 |
30% affirmed that they could not afford the total cost of the three doses of HPV vaccine |
- |
- |
cost |
|
9. Kruiroongroj S et al, 2014: Thailand (28) |
mean age: 43.47years Monthly household income: about 33% in 3.300 to 10000 US$ |
Bivalent: 76.9 Quadrivalent: 74.4 |
Bivalent: 68.9 Quadrivalent: 67.3 |
Bivalent: 24.5 (16.3-32.7 ) Quadrivalent: 32.7 (16.3-49) |
Bivalent 0.40 Quadrivalent: 0.53 |
Participants would pay more for quadrivalent vaccine as compared to bivalent vaccine. |
➢ - |
➢ - |
financial limitations (39-43) |
|
10. Songthap A et al, 2012: Thailand (29) |
Students mean age: 13.1 Parents: mean age: 43.2 mean monthly income of USD 1,116.40 Teachers mean age: 46.1 mean monthly income was USD 1,787.50 |
Students:26.1 Parents:44.8 Teachers:43 |
- |
Students: <14.2: 12.9% 14.3-57.1: 56.1% 57.2-114.3: 31% Parents: <14.2: 16.9% 14.3-57.1: 71.1% 57.2-114.3: 12% Teachers: <14.2: 27.3% 14.3-57.1: 59.1% 57.2-114.3: 13.6% |
- | - |
➢ - |
➢ - |
- |
|
11. Alder S et al, 2015: Argentina (30) |
median age:37 | 90.1 | 59.8 | 30.28 (0.91-165.8) | 0.23 |
About 12% were willing to vaccinate their daughter regardless of the cost |
➢ having a high school education or more ➢ gainful employment ➢ a disposable household income of 438-1,050 euro/month ➢ being aware of cervical cancer prior to the study |
➢ Age ➢ Marital status ➢ No. of children ➢ Heard of HPV prior to study ➢ Heard of condyloma (genital warts) prior to study ➢ Believes vaccination in general to be an effective ➢ way to prevent disease ➢ Believes vaccination in general to be a safe method to prevent disease ➢ Believes daughter to have had boyfriend ➢ Believes daughter is sexually active ➢ Concerned daughter will have more sexual partners |
- |
|
12. Dinh Thu H et al, 2018: Vietnam (31) |
About 70% has 36--49 years | - | 53.1 | 34.5 (23-46) | 1.47 | 65.6% viewed the cost as Expensive or Very Expensive |
➢ perceived the cost as acceptable ➢ better knowledge on HPV ➢ Not being a farmer ➢ Previously screened for cervical cancer |
➢ Age ➢ Not Kinh people ➢ Urban commune ➢ Higher education ➢ Having 1--2 children ➢ Poor household ➢ Positive attitude ➢ always use condom |
➢ No information on HPV/ HPV vaccine (60-67%) ➢ living far from health facilities ➢ (12.6-13.8%), ➢ High cost (9.2-19.7%) ➢ Not Considering vaccination as important (4%) ➢ Afraid that the vaccine was unsafe (4%). |
|
13. Umeh IB et al, 2016: Nigeria (16) |
About 75% has 31--50 years. 57.6 %: household monthly income less than <US$ 251 |
92.5 | 91.6 | 11.6 | 0.43 | most frequently stated amount was US$ 5.02 |
➢ mothers living in an rural ➢ previously diagnosed of HPV infection |
➢ - |
➢ - |
|
14. Philips Z et al, 2006: UK (32) |
About 53% has more than 40 years. | - | 79.8 | 282.32 | 0.63 | About 25% WTP more than US$344 |
➢ - |
➢ - |
➢ - |
|
15. Yan Yuen WW et al, 2018: Hong Kong (33) |
- |
girls: 84.9 Parents: 87.1 |
- | 64.5% of participants: 125 | 0.29 | About 8% WTP more than US$125 |
Parents: ➢ heard of the HPV vaccine ➢ Having correct knowledge of CC ➢ knowledge that the HPV vaccine does not affect growth ➢ perception that the vaccine could protect their daughter ➢ doctor recommended the vaccine ➢ not had a regular family doctor ➢ preference for their daughter to receive the vaccine at school |
➢ fear of side effects (52) ➢ not think the vaccine was effective (46) ➢ perception of promiscuity (2) |
|
|
16. Liao CH et al, 2009: Taiwan (34) |
- | - | - | US$1098 to US$1233 (US$913–1004) | 6.06 to 6.81 (5.04-5.54) |
VSL was estimated at approximately US$0.65 to US$4.09 (US$0.56– 3.16) million |
- |
➢ - |
➢ - |
|
17. Raab SS et al, 2002:USA (35) |
Mean age:39 About 33% has more than 50.000 $ annual household income |
- | - |
reduced the risk of dying of CC from 1 in 37,000 to 1 in 50,000: 237 |
0.65 |
No statistically significant differences were seen in the mean WTP at different new Pap test performance Levels. |
➢ more than 2 children ➢ Highest education level ➢ Marital status ➢ Age ➢ Perception of high risk for cervical cancer |
➢ |
➢ |
|
18. Touch S and Oh JK, 2018: Cambodia (40) |
60% has more than 40 years. About 44% has Low (US$ 0–124) family income (monthly) |
62 | 35.6 | 20.5 ± 8.1 | 1.61 |
62 % Willingness to vaccinate their daughter against HPV |
➢ younger age ➢ married ➢ heard about CC ➢ believe CC is preventable |
➢ high Education ➢ family income ➢ Number of Children |
➢ High cost (32.7) ➢ Lack of knowledge (25) ➢ Don’t know where to get HPV vaccine (4.5) ➢ Don’t trust vaccine safety (5.2) ➢ No risk as not exposed to sexual contact (3.5) |
|
19. Opoku CA et al, 2016: Ghana (41) |
mean age: 28 27% were in a polygamous relationship |
97 | 76 | - | - | - |
➢ - |
➢ - |
➢ - |
|
20. Lin Y et al, 2020:China(42) |
majority of the respondents were age 31–35 years annual household income of about 7-17 |
58.5 |
2vHPV (81.2)4vHPV (75.9) 9vHPV (67.7) Mean:74.9 |
- | - | - |
➢ Household income ➢ mass media exposure to HPV vaccination ➢ perceived self-efficacy in HPV vaccination ➢ spouse/partner approval ➢ Single mothers and mothers who were divorced, separated or widowed |
➢ Age ➢ Ethnicity ➢ Place of birth ➢ Highest education level ➢ Occupation type ➢ Experience with cervical cancer ➢ HPV knowledge ➢ Health belief model ➢ Perceived severity ➢ Perceived benefit ➢ Perceived barriers |
- |
|
21. You D et al,2020: China(43) |
majority of the respondents were age 19-22 | 53.5 | - | - | - | - |
➢ Age group ➢ Birthplace ➢ Location of school ➢ Central China ➢ Year of study ➢ Maternal educational level ➢ Paternal educational level ➢ Monthly disposable fund ➢ Perceived family economic status ➢ Sexual risk profile ➢ HPV knowledge ➢ Attitudes ➢ Perceived benefit ➢ Perceived barriers |
➢ Ethnicity ➢ Study program ➢ Perceived severity |
➢ |
|
22. Lin W et al, 2020: China(44) |
mean age was 37.09 years The majority of them were married (90.6%) |
63.3 | 30 | - | - | Local residents had a relatively higher awareness of HPV and its vaccine, as well as a higher willingness to receive HPV vaccination than non-permanent residents and floating population. |
➢ younger ages ➢ being local residents ➢ higher levels of education ➢ being married ➢ high monthly income ➢ having daughter(s) ➢ heard of HPV ➢ heard of HPV vaccine |
➢ Race ➢ Medical insurance ➢ Age at menarche ➢ Age at sex debut ➢ No. of the sexual partners in the past 6 month |
➢ - |
|
23. Kristina S et al, 2020: Indonesia(45) |
majority of the respondent (31.5%) had 46 and more age year | - | 67.1 | 3.94±1.64 | 0.1 | - |
➢ Age ➢ Monthly income ➢ Family history of cancer ➢ Private insurance status ➢ Knowledge ➢ Perception on cancer risk |
➢ Education ➢ Marital status ➢ Perceived health status ➢ Perceived quality of service ➢ Source of information ➢ Experience in Pap smear test |
|
|
24. Weng Q et al, 2020: Tanzania (21) |
the mean age was 32.86 years |
87.9 | 57.4 | - | - | Only 4.38% of the respondents had previously received CC screening |
➢ Age ➢ Marital States ➢ Parity ➢ Education level ➢ Family Income ➢ Disease History ➢ Family Cancer History |
➢ Ethnicity ➢ First Sex Age ➢ Genetic Disease |
➢ |
|
25. Dahlström LA et al,2010: Sweden (36) |
mean age:44 about 70% of the participants lived in rural |
76 | 63 | - | - | - |
➢ Female gender of child ➢ believes vaccines are safe ➢ Believes vaccines are efficient ➢ Age ➢ Education ➢ Employment ➢ family income ➢ martial situation ➢ has 2 Number of children ➢ living in rural ➢ Have heard about HPV ➢ Worried child will have more partners ➢ Believes child has had girlfriend/boy friend |
➢ Gender of parent ➢ Believes child has had coition |
- |
|
26. Oh JK et al, 2010: Korea (37) |
About 56% has more than 40 years. About 56% has middle (2000–4000 USD) income per month |
men and women:55 participants’ daughters:77 |
- | - | - |
35.5% of men and 39.1% of women suggested under US$ 50 |
➢ Aged under than 50 years ➢ education ➢ income |
➢ Sex ➢ Living in a small town |
- |
|
27. Rajiah K et al, 2017: Malaysia (38) |
66.2% of students were female 78.9% of The respondents were in a relationship. |
- | - | 397.6 | 3.56 |
Students were WTP US$ 450.6vaccinate their children in the future |
➢ More knowledge towards CC |
➢ attitudes towards vaccines |
➢ - |
|
28. Tran BX et al, 2018: Vietnam(39) |
mean age was 26.8 average monthly household income was US$ 667 |
- | 86.6 | 49.3 (44.4—54.3) | 2.27 |
Male WTP is more than Female |
➢ Age 20–29 years ➢ High household income ➢ education ➢ Has children >6 years old ➢ Adult male ➢ Believes that HPV vaccine is effective ➢ Has ever examined reproductive health ➢ informed about HPV by except doctors, nurses, or other health professionals |
➢ Has family member who ever had sexually transmitted infection |
➢ being male (33.3), high cost (38.2), the vaccine being seen as unnecessary (34.5) |
Characteristics of the Included Studies
Studies were conducted in 19 different countries (Scotland, Hong Kong, Malaysia, UK, South Africa, Thailand, Argentina, Vietnam, Nigeria, Taiwan, USA, Sweden, Korea, Cambodia, Ghana, Ethiopia, China, Indonesia, and Tanzania). Most studies were conducted in upper-middle-income economies (UMIEs) (based on New World Bank country classifications by income level: 2019-20 (46)).
Acceptance of Cervical Cancer Prevention Methods
Out of the 28 articles included in the study, 17 studies (23 data) were meta-analysis on the rate of acceptance of CCP methods. The results showed that the overall acceptance rate was 64% (95% CI, 56-72) (Fig. 2).
Fig. 2.

Meta-analysis of Overall Rate of Acceptance of Cervical Cancer Prevention Methods Based on a Random Effect Model with 95% Confidence Level
The results also showed that among the different groups, the highest acceptance was among women (78%); based on the economic status of countries, the highest acceptance was in LIEs (88%); and based on the type of testing, the highest acceptance was related to overall prevention services (89.5) (Table 3).
Table 3. Results of the meta-analysis of the overall acceptance rate, willingness to pay, and percentage of positive willingness to pay based on GDP per capita for cervical cancer prevention methods based on participant variables, countries' economic segregation and types of prevention methods.
| Variable | Variable Level | Dimension Statues (95% CI) | Heterogeneity Test (95% CI) | ||||||
| Percent | Lower limit | Upper limit | df | Q | p | I 2 | |||
| Acceptance rate of CCS | Participants | Girls | 48 | 15 | 142 | 1 | 51.58 | 0.000 | 98.061 |
| Others | 43 | 25 | 73 | 0 | 0.00 | 1.000 | 0.000 | ||
| Parents/Mothers | 63 | 53 | 76 | 9 | 69.7 | 0.000 | 87.1 | ||
| Students | 62 | 44 | 86 | 4 | 24.5 | 0.000 | 83.7 | ||
| Women | 78 | 63 | 96 | 4 | 20.9 | 0.165 | 80.7 | ||
| Country by economies | High-Income Economies (HIEs) | 56 | 40 | 77 | 6 | 119.9 | 0.000 | 94.999 | |
| Lower-Middle Income Economies (LMIEs) | 83 | 64 | 108 | 2 | 3.810 | 0.149 | 47.511 | ||
| Low-Income Economies (LIEs) | 88 | 75 | 103 | 0 | 0 | 1 | 1 | ||
| Upper-Middle-Income Economies (UMIEs) | 63 | 55 | 71 | 11 | 40.4 | 0.000 | 72.8 | ||
| Type of prevention methods | HPV | 60.3 | 53 | 69 | 19 | 175.4 | 0.000 | 89.5 | |
| Pap-smear | 89.3 | 69 | 115 | 0 | 0.00 | 1.000 | 0.000 | ||
| screening service | 89.5 | 77 | 104 | 0 | 0.25 | 0.61 | 0.000 | ||
| Rate of Positive WTP | Participants | Girls | 55 | 46 | 65 | 0 | 0.00 | 1.000 | 0.000 |
| Health Professionals | 85 | 67 | 106 | 1 | 0.016 | 0.900 | 0.000 | ||
| Others | 87 | 65 | 115 | 0 | 0.00 | 1.000 | 0.000 | ||
| Parents/Mothers | 67 | 59 | 74 | 7 | 17 | 0.017 | 58.9 | ||
| Students | 87 | 66 | 113 | 1 | 0.00 | 0.942 | 0.000 | ||
| Women | 58 | 40 | 82 | 7 | 137 | 0.000 | 94.9 | ||
| Country by economies | High-Income Economies (HIEs) | 65 | 56 | 75 | 5 | 22.4 | 0.000 | 77.7 | |
| Lower-Middle Income Economies (LMIEs) | 67 | 53 | 86 | 5 | 15.7 | 0.008 | 68.2 | ||
| Low-Income Economies (LIEs) | 73 | 54 | 96 | 2 | 6 | 0.04 | 66.9 | ||
| Upper-Middle-Income Economies (UMIEs) | 64 | 43 | 96 | 6 | 13.7 | 0.00 | 95.6 | ||
| Type of prevention methods | HPV | 63 | 52 | 76 | 15 | 197.2 | 0.000 | 92.3 | |
| Pap-smear | 89 | 69 | 115 | 0 | 0.0 | 1.000 | 0.000 | ||
| screening service | 71 | 61 | 83 | 4 | 7.1 | 0.1 | 43.7 | ||
|
WTP as a percentage of GDP per capita |
Participants | Girls | 0.19 | 0 | 0.24 | 1 | 0.1 | 0.733 | 0.000 |
| Health Professionals | 1 | 011 | 9.1 | 1 | 0.0 | 0.937 | 0.000 | ||
| Others | 2.27 | 0.35 | 14.3 | 0 | 0.0 | 1.000 | 0.000 | ||
| Parents/Mothers | 0.40 | 0.10 | 1.51 | 6 | 0.0 | 1.000 | 0.000 | ||
| Students | 1.78 | 0.29 | 10.5 | 3 | 0.5 | 0.904 | 0.000 | ||
| Women | 0.94 | 0.31 | 2.09 | 5 | 1.01 | 0.96 | 0.000 | ||
| Country by economies | High-Income Economies (HIEs) | 0.39 | 0.13 | 1.19 | 8 | 0.7 | 0.999 | 0.000 | |
| Lower-Middle Income Economies (LMIEs) | 1.54 | 0.49 | 4.79 | 4 | 0.91 | 0.91 | 0.000 | ||
| Low-Income Economies (LIEs) | 1 | 0.1 | 9.12 | 1 | 0.0 | 0.937 | 0.000 | ||
| Upper-Middle-Income Economies (UMIEs) | 1 | 0.26 | 4.13 | 5 | 1.4 | 0.923 | 0.000 | ||
| Type of prevention methods | HPV | 0.91 | 0.43 | 1.90 | 16 | 505 | 0999 | 0.000 | |
| Pap-smear | 0.53 | 0.02 | 1.14 | 1 | 0.00 | 0936 | 0.000 | ||
| screening service | 0.63 | 0.12 | 3.3 | 2 | 0.27 | 0.87 | 0.000 | ||
The results of the heterogeneous assessment also showed that the results of the studies had a relatively acceptable heterogeneity (Q=193.8; df=22; I2=88.6; p<.001).
Willingness to Pay for Cervical Cancer Prevention Methods
Out of the 28 articles included in the study, 19 studies (22 data) were meta-analysis on WTP for CCP methods. The results showed that the overall positive WTP rate was 66% (95% CI; 57-76) (Fig. 3).
Fig. 3.

Fig. 3. Meta-analysis of the Positive WTP Rate of Cervical Cancer Prevention Methods Based on a Random Effect Model With 95% Confidence Level
The results also showed that among the different groups, the highest rate of positive WTP was found among students and other groups, and according to the economic status of countries, the highest rate of Positive WTP was in the low-income economies (LIEs). According to the type of prevention method, the highest WTP is for the Pap smear test (Table 3). The results of the heterogeneous assessment showed that the results of the studies have a relatively high heterogeneity (Q=226; DF=21; I2=90.7; p<0.001).
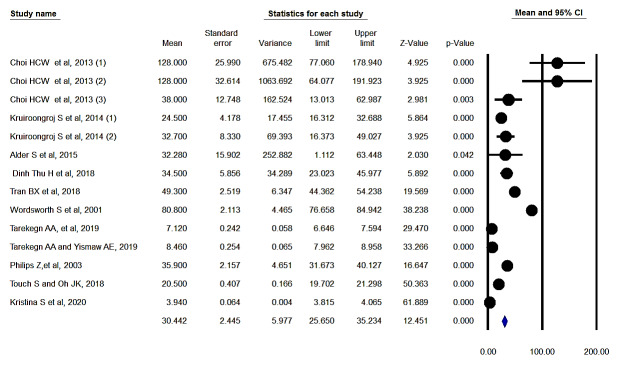
Amounts of Money (in US dollars) for Willingness to Pay
Out of the 28 articles included in the study, 11 studies (14 data) were meta-analysis of monetary amounts (in US$) that individuals were willing to pay for CCP methods. The results showed that the average money that people are willing to pay is US$ 30.44 (95% CI; 25.6-35.2) (Fig. 4).
Fig. 4.
Meta-analysis Results (in US$) of Individuals’ Willingness to Pay for Cervical Cancer Prevention Methods Based on a Random Effect Model with 95% Confidence Level
The results of the heterogeneous assessment also showed that the results of the studies are highly heterogeneous (Q=3888.3; df=13; I2=99.6; p<0.001).
Percentage of Willingness to Pay Based on the Gross Domestic Product (GDP) per Capita
Out of the 28 articles included in the study, 18 studies (22 data) were meta-analysis on the percentage of WTP for CCP methods. The results showed that this percentage was 0.84% (95% CI 0.44-1.62) (Fig. 5).
Fig. 5.

Meta-analysis of Percentage of Willingness to Pay for Cervical Cancer Prevention Based on GDP per Capita According to Fixed Effect Model with 95% Confidence Level
Based on GDP per Capita According to Fixed Effect Model with 95% Confidence Level
The results also showed that among the different groups, the highest percentage of WTP was among the other groups and students; and based on the economic situation of countries, the highest proportion was in LMIEs; and based on the type of prevention methods, the highest percentage was related to the HPV vaccine (Table 3).
The results of the heterogeneous assessment also showed that the results of heterogeneous studies were not consistent and had very good homogeneity (Q=6.8; df=21; I2=0.00; p<0.98).
Table 3. Results of the meta-analysis of the overall acceptance rate, willingness to pay, and percentage of positive willingness to pay based on GDP per capita for cervical cancer prevention methods based on participant variables, countries' economic segregation and types of prevention methods.
Effective Factors in Acceptance of and Willingness to Pay for Cervical Cancer Prevention Methods
In this study, by analyzing the content of the mentioned factors in the included studies, finally, 31 factors were divided into 2 groups of significant effective factors and nonsignificant effective factors. Most of the factors that have been mentioned in various studies as significant effective factors include income, age, education, risky sexual behaviors, awareness of cervical cancer and its risk factors, belief in cervical cancer risk, and belief about the effectiveness of prevention methods (Table 4).
Table 4. The Most Significant and Nonsignificant Effective Factors in Acceptance and Willingness to Pay for Cervical Cancer Prevention Methods .
| Variable | Significant positive | Nonsignificant |
|
1. Household Income |
************ | *** |
|
2. Age |
*********** | *** |
|
3. Age of daughters |
** | |
|
4. Test status (had screening test or not) |
** | ** |
|
5. Had heard of screening test |
**** | ** |
|
6. Had heard of cervical cancer and risk factors |
***** | ** |
|
7. Had heard of HPV vaccine |
* | |
|
8. Perception on the health of daughters |
* | |
|
9. Risky sexual behaviors |
***** | ****** |
|
10. Education |
********** | **** |
|
11. Self-rated health |
*** | |
|
12. perceived seriousness of cervical cancer |
**** | ** |
|
13. perceived quality /accuracy of screening test |
** | * |
|
14. Marital status |
***** | *** |
|
15. Religion |
* | |
|
16. Ethnicity |
** | |
|
17. Background profession |
** | |
|
18. Knowledge about screening test |
*** | |
|
19. Source of more Information about screening test |
** | * |
|
20. Proportion of screening testing normal |
* | |
|
21. Smoking |
* | * |
|
22. Has risk factor (STDs, family history...) |
*** | |
|
23. employment |
** | |
|
24. No. of children |
*** | *** |
|
25. Believes screening test is an effective |
**** | *** |
|
26. Living setting (urban or rural) |
** | ** |
|
27. Being local residents |
* | |
|
28. Having daughter(s) |
* | |
|
29. Family history of cancer |
** | |
|
3. Private insurance status |
* | |
|
31. Knowledge |
* |
* Number/ frequency
The Most Important Reasons for Unwillingness to Pay for Cervical Cancer Prevention Methods
Only 7 studies cited reasons for unwillingness to pay for CCP methods. In 6 of the 7 studies, the cost was one of the main reasons cited by individuals. Other reasons included lack of information and awareness of preventive methods, difficulties in accessing preventive methods, lack of attention to preventive methods, fear of unsafe methods of prevention, and social stigma.
Reporting Quality Assessment Results
As most of the reviewed articles were published in high-ranking journals, most articles complied with reporting assessment items. Out of the 924 assessment items (28 [the number of studies]) multiplied by 33 [number of tool items]), 628 (67.9) items met the standards (the option Yes). About 277 cases (29.9%) did not comply with the standards (no option) and about 19 cases (2.2%) included both "unclear" and "not-applicable" (Table 5).
Table 5. Example of Quality Assessment of Included Studies .
| Question | Wordsworth S, et al: 2001 |
Choi HCW et al, 2013 |
|
| 1 | (a) Indicate the study’s design with a commonly used term in the title or the abstract | Yes | Yes |
| 2 | (b) Provide in the abstract an informative and balanced summary of what was done and what was found | Yes | Yes |
| 3 | Explain the scientific background and rationale for the investigation being reported | Yes | Yes |
| 4 | State specific objectives, including any prespecified hypotheses | Yes | Yes |
| 5 | Present key elements of study design early in the paper | Yes | Yes |
| 6 | Describe the setting, locations, and relevant dates, including periods of recruitment, exposure, follow-up, and data collection | Yes | Yes |
| 7 | (a) Give the eligibility criteria, and the sources and methods of selection of participants | Yes | Yes |
| 8 | Clearly define all outcomes, exposures, predictors, potential confounders, and effect modifiers. Give diagnostic criteria, if applicable | Yes | Yes |
| 9 | For each variable of interest, give sources of data and details of methods of assessment (measurement). Describe comparability of assessment methods if there is more than one group | Yes | Yes |
| 10 | Describe any efforts to address potential sources of bias | No | No |
| 11 | Explain how the study size was arrived at | Yes | Yes |
| 12 | Explain how quantitative variables were handled in the analyses. If applicable, describe which groupings were chosen and why | Yes | Yes |
| 13 | (a) Describe all statistical methods, including those used to control for confounding | Yes | Yes |
| 14 | (b) Describe any methods used to examine subgroups and interactions | No | No |
| 15 | (c) Explain how missing data were addressed | No | Yes |
| 16 | (d) If applicable, describe analytical methods taking account of sampling strategy | Yes | Yes |
| 17 | (e) Describe any sensitivity analyses | No | No |
| 18 | (b) Give reasons for non-participation at each stage | No | No |
| 19 | (a) Give characteristics of study participants (eg demographic, clinical, social) and information on exposures and potential confounders | Yes | Yes |
| 20 | (b) Indicate number of participants with missing data for each variable of interest | No | No |
| 21 | Report numbers of outcome events or summary measures | Yes | Yes |
| 22 | (a) Give unadjusted estimates and, if applicable, confounder-adjusted estimates and their precision (eg, 95% confidence interval). Make clear which confounders were adjusted for and why they were included | Yes | Yes |
| 23 | (b) Report category boundaries when continuous variables were categorized | Yes | Yes |
| 24 | Summarise key results with reference to study objectives | Yes | Yes |
| 25 | Discuss limitations of the study, taking into account sources of potential bias or imprecision. Discuss both direction and magnitude of any potential bias | Yes | Yes |
| 26 | Give a cautious overall interpretation of results considering objectives, limitations, multiplicity of analyses, results from similar studies, and other relevant evidence | Yes | Yes |
| 27 | Discuss the generalisability (external validity) of the study results | Yes | Yes |
| 28 | Give the source of funding and the role of the funders for the present study and, if applicable, for the original study on which the present article is based | No | Yes |
| 29 | Does a detailed description of goods or services in question offered to the respondents? | No | Yes |
| 30 | Does the information and attributes expressed in goods or services scenarios is obtained from user or key informant assessments (e.g. focus groups, Delphi panels, interviews etc)? | No | Yes |
| 31 | Was there a pilot study conducted to assess the survey tool/design? | No | No |
| 32 | Does the survey involve face to face interviews? | No | No |
| 33 | Were those involved in data collection adequately trained? | No | NA |
Table 4. The Most Significant and Nonsignificant Effective Factors in Acceptance and Willingness to Pay for Cervical Cancer Prevention Methods
Discussion
Most of the reviewed studies were conducted in Southeast Asian countries. Epidemiological studies of cancers, and especially cervical cancer, have also shown that this type of cancer is one of the most common cancer in this region (47). One of the main reasons for this may be the high prevalence of high-risk sexual behaviors and the sex tourism industry in this region, which has been widespread in recent years (48). The results also show a high WTP for and acceptance of CCP in these areas, which is also due to the high prevalence of this type of cancer and its association with high-risk sexual behaviors. Also, one of the factors contributing to the high WTP and acceptance of CCP in these areas could be the issue of high economic growth in the countries in the region in recent years (49).
The HPV vaccine was the most common type of prevention methods in most studies. HPV accounts for 90% of cervical cancer cases (50, 51). The WHO recommends the HPV vaccine be included in countries' vaccination programs (52). However, in the present study, the HPV vaccine had a lower WTP and acceptance rate compared to other methods and had a high percentage of GDP per capita. However, Numerous other studies' results have confirmed the superiority and advantages of the HPV vaccine in comparison with other methods (53, 54). One of the main reasons for this issue may be the novelty of this method, as the HPV vaccine has been introduced and used since 2006, while other methods have been used for many years. The results of this study showed that the cost of prevention is one of the main reasons for the unwillingness or acceptance of CCP methods. Therefore, it is recommended that different countries and organizations adopt cost-cutting methods by adopting supportive policies, such as insurance coverage.
In this study, although CCP methods accounted for a high percentage of GDP per capita in LMICs, the rates of acceptance and WTP in these countries were higher than HICs. One of the main reasons for this may be the high prevalence of cervical cancer in LMICs. Studies have estimated that about 85% of the prevalence and mortality of this type of cancer occur in LMICs (55). However, these countries have many problems with these types of diseases and usually have very limited potential and resources for the prevention and treatment of these diseases (56, 57). An important reason for the high payment amount of GDP per capita in these countries is the low per capita GDP. Therefore, more attention should be paid to the policies and strategies offered by various organizations, especially by the WHO, to better control of this type of cancer and to increase the effectiveness of prevention methods (58, 59).
In terms of the significant factors in acceptance and WTP, in addition to the issues related to the costs and risky sexual behaviors mentioned, most of the other factors were related to individuals' knowledge and attitude (such as education, cervical cancer awareness, and its risk factors, etc.). Many studies have been published in recent years about the knowledge and attitude of screening and prevention methods of cervical cancer (60, 61). The results of most studies indicate that people's awareness, especially women about cervical cancer are not enough and prevention methods and interventions are needed to increase their awareness. Therefore, due to the low knowledge of individuals and the impact of attention given to these issues in acceptance and WTP for screening and prevention of cervical cancer, there is a need to increase public awareness in this regard.
Based on the results of the present study, it is suggested that policymakers and senior managers of the health system of countries, while considering the local conditions of their country, in general, pay attention to reducing the cost of preventive measures, to increase awareness, and improve people's attitudes about prevention methods, and to focus on target age groups and appropriate prevention and reducing risky sexual behaviors to increase the WTP and acceptance of prevention methods.
However, based on the results of the literature review and the experiences of the researchers, the present study for the first time systematically and comprehensively examined the different dimensions of WTP for and acceptance of different CCP methods and provided comprehensive and applicable information to policymakers and researchers. However, during this study, the researchers faced several limitations, one of which was the restriction of the articles to the CVM. In this study, only published studies in English and Persian were reviewed. Also, due to the type of results reporting, the authors could not conduct meta-analyses based on some of the variables, especially the type of information provided to participants that is a key first step in using the CVM method.
Conclusion
The results showed that the WTP for and acceptance of CCP methods was relatively high among individuals. According to the results of this study it is recommended that attention be paid to reduce the cost of preventive measures, especially the HPV vaccine, to increase awareness and to improve people's attitudes about prevention methods, to focus on target age groups and appropriate prevention, and to reduce risky sexual behaviors to increase the WTP and acceptance of CCP methods. Also, it is recommended to consider other methods of calculating WTP and other cancers in future studies.
Acknowledgement
This study was part of a PhD thesis in Health Economics at Iran University of Medical Sciences (IUMS), supported by Iran University of Medical Sciences (Grant No: IUMS/SHMIS_98-2-37-15495 and with Ethical code: IR.IUMS.REC.1398.423).
Ethical Approval
The thesis was approved by an Ethics approval code: IR.IUMS.REC.1398.423.
Conflict of Interests
The authors declare that they have no competing interests.
Appendix 1. Search Strategy .
| Database | Query | Items found |
| Pubmed | Search ((((((("Early Detection of Cancer"[Majr]) OR "Papanicolaou Test"[Majr]) OR "Human Papillomavirus DNA Tests"[Majr]) OR "Vaginal Smears"[Majr]) OR ((((((((((("cancer screening"[Title/Abstract]) OR "follow up testing"[Title/Abstract]) OR "pap smear"[Title/Abstract]) OR "hpv test"[Title/Abstract]) OR "human papillomavirus"[Title/Abstract]) OR "risk reduction"[Title/Abstract]) OR "cancer prevention/cancer risk"[Title/Abstract]) OR "human papilloma virus"[Title/Abstract]) OR "cervical excision"[Title/Abstract]) OR "pap test"[Title/Abstract])))) AND (((("Vaginal Neoplasms"[Majr]) OR "Vulvar Neoplasms"[Majr]) OR "Uterine Cervical Neoplasms"[Majr]) OR (((("cervical cancer"[Title/Abstract]) OR "vaginal cancer"[Title/Abstract]) OR "vulvar cancer"[Title/Abstract]) OR "uterine cervix cancer"[Title/Abstract]))) AND (((((((((((((((((((("willingness to pay"[Title/Abstract]) OR "willing to pay"[Title/Abstract]) OR "willing to accept"[Title/Abstract]) OR WTP[Title/Abstract]) OR "patient preference"[Title/Abstract]) OR "patient acceptance"[Title/Abstract]) OR "stated preference"[Title/Abstract]) OR "revealed preference"[Title/Abstract]) OR "consumers' hypothetical"[Title/Abstract]) OR "willingness to accept"[Title/Abstract]) OR WTA[Title/Abstract]) OR CVM[Title/Abstract]) OR "contingent valuation method"[Title/Abstract]) OR "contingent valuation survey"[Title/Abstract]) OR "cost benefit analysis"[Title/Abstract]) OR "economic evaluation"[Title/Abstract]) | 184 |
| Web of Science |
# 1 TS=("Early Detection of Cancer" OR "Papanicolaou Test" OR "Human Papillomavirus DNA Tests" OR "Vaginal Smears" OR "cancer screening" OR "follow up testing" OR "pap smear" OR "hpv test" OR "human papillomavirus" OR "risk reduction" OR "cancer prevention/cancer risk" OR "human papilloma virus" OR "cervical excision" OR "pap tests") Indexes=SCI-EXPANDED, SSCI, A&HCI, ESCI Timespan=All years # 2 TS=("Vaginal Neoplasms" OR "Vulvar Neoplasms" OR "Uterine Cervical Neoplasms" OR "cervical cancer" OR "vaginal cancer" OR "vulvar cancer" OR "uterine cervix cancer") Indexes=SCI-EXPANDED, SSCI, A&HCI, ESCI Timespan=All years # 3 TS=("willingness to pay" OR "willing to pay" OR "willing to accept" OR WTP OR "patient preference" OR "patient acceptance" OR "stated preference" OR "revealed preference" OR "consumers' hypothetical" OR "willingness to accept" OR WTA OR CVM OR "contingent valuation method" OR "contingent valuation survey" OR "cost benefit analysis" OR "economic evaluation") Indexes=SCI-EXPANDED, SSCI, A&HCI, ESCI Timespan=All years # 4 #3 AND #2 AND #1 Indexes=SCI-EXPANDED, SSCI, A&HCI, ESCI Timespan=All years |
245 |
| Scopus | (TITLE-ABS-KEY( "Early Detection of Cancer" OR "Papanicolaou Test" OR "Human Papillomavirus DNA Tests" OR "Vaginal Smears" OR "cancer screening" OR "follow up testing" OR "pap sme ar" OR "hpv test" OR "human papillomavirus" OR "risk reduction" OR "cancer prevention/cancer risk" OR "human papilloma virus" OR "cervical excision" OR "pap tests" ))AND(TITLE-ABS-KEY( "Vaginal Neoplasms" OR "Vulvar Neoplasms" OR " Uterine Cervical Neoplasms" OR "cervical cancer" OR "vaginal cancer" OR "vulvar cancer" OR "uterine cervix cancer" ))AND(TITLE-ABS-KEY( "willingness to pay" OR "willing to pay" OR "willing to accept" OR wtp OR "patient preference" OR "patient acceptance" OR "stated preference" OR "revealed preference" OR "consumers' hypothetical" OR "willingness to accept" OR wta OR cvm OR "contingent valuation method" OR "contingent valuation survey" OR "cost benefit analysis" OR "economic evaluation" )) | 2477 |
|
Embase |
'willingness to pay':ti,ab OR 'willing to pay':ti,ab OR 'willing to accept':ti,ab OR wtp:ti,ab OR 'patient preference':ti,ab OR 'patient acceptance':ti,ab OR 'stated preference':ti,ab OR 'revealed preference':t i,ab OR 'consumers hypothetical':ti,ab OR 'willingness to accept':ti,ab OR wta:ti,ab OR cvm:ti,ab OR 'contingent valuation method':ti,ab OR 'contingent valuation survey':ti,ab OR 'cost benefit analysis':ti,ab OR 'economic evaluation':ti,ab | 188 |
Appendix 1
Cite this article as: Shokri Jamnani A, Rezapour A, Moradi N, Langarizadeh M. Willingness to pay for and acceptance of cervical cancer prevention methods: A systematic review and meta-analysis. Med J Islam Repub Iran. 2021 (23 Jun);35:81. https://doi.org/10.47176/mjiri.35.81
Footnotes
Conflicts of Interest: None declared
Funding: Iran University of Medical Sciences (Grant No: IUMS/SHMIS_98-2-37-15495)
References
- 1.Pedersen K, Burger EA, Nygard M, Kristiansen IS, Kim JJ. Adapting cervical cancer screening for women vaccinated against human papillomavirus infections: The value of stratifying guidelines. Eur J Cancer. 2018;91:68–75. doi: 10.1016/j.ejca.2017.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baudendistel I, Winkler EC, Kamradt M, Brophy S, Langst G, Eckrich F. et al. Cross-sectoral cancer care: views from patients and health care professionals regarding a personal electronic health record. Eur J Cancer Care. 2016;3(10):12429. doi: 10.1111/ecc.12429. [DOI] [PubMed] [Google Scholar]
- 3.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murphy KM, Nguyen V, Shin K, Sebastian-Deutsch A, Frieden L. Health Care Professionals and the Employment-Related Needs of Cancer Survivors. J Occup Rehabil. 2016;8:8. doi: 10.1007/s10926-016-9629-2. [DOI] [PubMed] [Google Scholar]
- 5.Bahr S, Bzieh R, El Hayek GY, Adib S. Cost-benefit analysis of a projected national human papilloma virus vaccination programme in Lebanon. East Mediterr Health J. 2019;25(10):715–21. doi: 10.26719/2019.25.10.715. [DOI] [PubMed] [Google Scholar]
- 6.Anorlu RI. Cervical cancer: the sub-Saharan African per-spective. Reprod Health Matters. 2008;16(32):41–9. doi: 10.1016/S0968-8080(08)32415-X. [DOI] [PubMed] [Google Scholar]
- 7.Sawaya GF, Smith-Mccune K, Kuppermann M. Cervical Cancer Screening: More Choices in 2019. JAMA. 2019;321(20):2018–9. doi: 10.1001/jama.2019.4595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith A, Baines N, Memon S, Fitzgerald N, Chadder J, Politis C. et al. Moving toward the elimination of cervical cancer: Modelling the health and economic benefits of increasing uptake of human papillomavirus vaccines. Curr Oncol. 2019;26(2):80–4. doi: 10.3747/co.26.4795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li S, Liu S, Ratcliffe J, Gray A, Chen G. Preferences for cervical cancer screening service attributes in rural China: a discrete choice experiment. Patient Prefer Adherence. 2019;13:881–9. doi: 10.2147/PPA.S201913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Azami-Aghdash S, Gharaee H, Aghaei MH, Derakhshani N. Cardiovascular Disease Patient's Quality of Life in Tabriz City in Iran in 2018. J Community Health Res. 2019 [Google Scholar]
- 11.Lin YL, Lin Z, He F, Hu ZJ, Zimet GD, Alias H. et al. Factors influencing intention to obtain the HPV vaccine and acceptability of 2- 4-and 9-valent HPV vaccines: A study of undergraduate female health sciences students in Fujian, China. Vaccine. 2019;37(44):6714–23. doi: 10.1016/j.vaccine.2019.09.026. [DOI] [PubMed] [Google Scholar]
- 12. O'Brien B. Cost–Benefit Analysis, Willingness to Pay. Wiley StatsRef: Statistics Reference Online. 2014.
- 13.Mariani AW, Pêgo-Fernandes PM. Willingness to pay. What??? Sao Paulo Med J. 2014;132(3):131–2. doi: 10.1590/1516-3180.2014.1323844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Azami-Aghdash S, Sadeghi-Bazargani H, Saadati M, Mohseni M, Gharaee H. Experts’ perspectives on the application of public-private partnership policy in prevention of road traffic injuries. Chin J Traumatol. 2020;23(3):152–158. doi: 10.1016/j.cjtee.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Boyle KJ. Contingent valuation in practice. A primer on nonmarket valuation: Springer; 2017. p. 83-131.
- 16.Umeh IB, Nduka SO, Ekwunife OI. Mothers' willingness to pay for HPV vaccines in Anambra state, Nigeria: a cross sectional contingent valuation study. Cost Eff Resour Alloc. 2016;14:8. doi: 10.1186/s12962-016-0057-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Philips Z, Johnson S, Avis M, Whynes DK. Human papillomavirus and the value of screening: young women's knowledge of cervical cancer. Health Educ Res. 2003;18(3):318–28. doi: 10.1093/her/cyf022. [DOI] [PubMed] [Google Scholar]
- 18.Rajiah K, Maharajan MK, Chin NS, Num KS. Awareness and acceptance of human papillomavirus vaccination among health sciences students in Malaysia. Virusdisease. 2015;26(4):297–303. doi: 10.1007/s13337-015-0287-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Khan K, Kunz R, Kleijnen J, Antes G. Systematic reviews to support evidence-based medicine: Crc Press; 2011.
- 20.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M. et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weng Q, Jiang J, Haji FM, Nondo LH, Zhou H. Women’s knowledge of and attitudes toward cervical cancer and cervical cancer screening in Zanzibar, Tanzania: a cross-sectional study. BMC Cancer. 2020;20(1):63. doi: 10.1186/s12885-020-6528-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wordsworth S, Ryan M, Waugh N. Costs and benefits of cervical screening IV: valuation by women of the cervical screening programme. Cytopathology. 2001;12(6):367–76. doi: 10.1046/j.1365-2303.2001.00358.x. [DOI] [PubMed] [Google Scholar]
- 23.Choi HCW, Leung GM, Woo PPS, Jit M, Wu JT. Acceptability and uptake of female adolescent HPV vaccination in Hong Kong: A survey of mothers and adolescents. Vaccine. 2013;32(1):78–84. doi: 10.1016/j.vaccine.2013.10.068. [DOI] [PubMed] [Google Scholar]
- 24.Tarekegn AA, Mengistu MY, Mirach TH. Health professionals' willingness to pay and associated factors for cervical cancer screening program at College of Medicine and Health Sciences, University of Gondar, Northwest Ethiopia. PLoS One. 2019;14(4):12. doi: 10.1371/journal.pone.0215904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tarekegn AA, Yismaw AE. Health professionals' willingness to pay and associated factors for human papilloma virus vaccination to prevent cervical cancer at College of Medicine and Health Sciences University of Gondar, Northwest Ethiopia. BMC Res Notes. 2019;12(1):58. doi: 10.1186/s13104-019-4085-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hoque ME, Ghuman S, Van Hal G. Human Papillomavirus Vaccination Acceptability among Female University Students in South Africa. Asian Pac J Cancer Prev. 2013;14(8):4865–9. doi: 10.7314/apjcp.2013.14.8.4865. [DOI] [PubMed] [Google Scholar]
- 27.Maharajan MK, Rajiah K, Num KS, Yong NJ. Knowledge of Human Papillomavirus Infection, Cervical Cancer and Willingness to pay for Cervical Cancer Vaccination among Ethnically Diverse Medical Students in Malaysia. Asian Pac J Cancer Prev. 2015;16(14):5733–9. doi: 10.7314/apjcp.2015.16.14.5733. [DOI] [PubMed] [Google Scholar]
- 28.Kruiroongroj S, Chaikledkaew U, Thavorncharoensap M. Knowledge, Acceptance, and Willingness to Pay for Human Papilloma Virus (HPV) Vaccination among Female Parents in Thailand. Asian Pac J Cancer Prev. 2014;15(13):5469–74. doi: 10.7314/apjcp.2014.15.13.5469. [DOI] [PubMed] [Google Scholar]
- 29.Songthap A, Pitisuttithum P, Kaewkungwal J, Fungladda W, Bussaratid V. Knowledge, attitudes, and acceptability of a human papilloma virus vaccine among students, parents and teachers in Thailand. Southeast Asian J Trop Med Public Health. 2012;43(2):340–53. [PubMed] [Google Scholar]
- 30.Alder S, Gustafsson S, Perinetti C, Mints M, Sundstrom K, Andersson S. Mothers' acceptance of human papillomavirus (HPV) vaccination for daughters in a country with a high prevalence of HPV. Oncol Rep. 2015;33(5):2521–8. doi: 10.3892/or.2015.3817. [DOI] [PubMed] [Google Scholar]
- 31.Dinh Thu H, Nguyen Thanh H, Hua Thanh T, Nguyen Hai L, Tran Thi V, Nguyen Manh T. et al. Mothers' willingness to pay for daughters' HPV vaccine in northern Vietnam. Health Care Women Int. 2018;39(4):450–62. doi: 10.1080/07399332.2017.1411914. [DOI] [PubMed] [Google Scholar]
- 32.Philips Z, Whynes DK, Avis M. Testing the construct validity of willingness to pay valuations using objective information about risk and health benefit. Health Econ. 2006;15(2):195–204. doi: 10.1002/hec.1054. [DOI] [PubMed] [Google Scholar]
- 33.Yan Yuen WW, Lee A, Chan PKS, Tran L, Sayko E. Uptake of human papillomavirus (HPV) vaccination in Hong Kong: Facilitators and barriers among adolescent girls and their parents. PLoS One. 2018;13(3) doi: 10.1371/journal.pone.0194159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liao CH, Liu JT, Pwu RF, You SL, Chow I, Tang CH. Valuation of the economic benefits of human papillomavirus vaccine in Taiwan. Value Health. 2009;12 Suppl 3:S74–7. doi: 10.1111/j.1524-4733.2009.00632.x. [DOI] [PubMed] [Google Scholar]
- 35.Raab SS, Grzybicki DM, Hart AR, Kiely S, Andrew-JaJa C, Scioscia E, Jr Jr. Willingness to pay for new Papanicolaou test technologies. Am J Clin Pathol. 2002;117(4):524–33. doi: 10.1309/XNUG-XH8V-C1KM-T6GD. [DOI] [PubMed] [Google Scholar]
- 36.Dahlström LA, Tran TN, Lundholm C, Young C, Sundström K, Sparén P. Attitudes to HPV vaccination among parents of children aged 12‐15 years—A population‐based survey in Sweden. Int J Cancer. 2010;126(2):500–7. doi: 10.1002/ijc.24712. [DOI] [PubMed] [Google Scholar]
- 37.Oh JK, Lim MK, Yun EH, Lee EH, Shin HR. Awareness of and attitude towards human papillomavirus infection and vaccination for cervical cancer prevention among adult males and females in Korea: A nationwide interview survey. Vaccine. 2010;28(7):1854–60. doi: 10.1016/j.vaccine.2009.11.079. [DOI] [PubMed] [Google Scholar]
- 38.Rajiah K, Maharajan MK, Num KSF, Koh RCH. Knowledge about human papillomavirus and cervical cancer: predictors of HPV vaccination among dental students. Asian Pac J Cancer Prev. 2017;18(6):1573. doi: 10.22034/APJCP.2017.18.6.1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tran BX, Than PTQ, Doan TTN, Nguyen HLT, Mai HT, Nguyen THT. et al. Knowledge, attitude, and practice on and willingness to pay for human papillomavirus vaccine: a cross-sectional study in Hanoi, Vietnam. Patient Prefer Adherence. 2018;12:945. doi: 10.2147/PPA.S165357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Touch S, Oh JK. Knowledge, attitudes, and practices toward cervical cancer prevention among women in Kampong Speu Province, Cambodia. BMC Cancer. 2018;18(1) doi: 10.1186/s12885-018-4198-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Opoku CA, Browne ENL, Spangenberg K, Moyer C, Kolbilla D, Gold KJ. Perception and risk factors for cervical cancer among women in northern Ghana. Ghana Med J. 2016;50(2):84–9. doi: 10.4314/gmj.v50i2.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lin Y, Lin Z, He F, Chen H, Lin X, Zimet GD, et al. HPV vaccination intent and willingness to pay for 2-, 4-, and 9-valent HPV vaccines: A study of adult women aged 27–45 years in China. Vaccine. 2020. [DOI] [PubMed]
- 43.You D, Han L, Li L, Hu J, Zimet GD, Alias H. et al. Human Papillomavirus (HPV) Vaccine Uptake and the Willingness to Receive the HPV Vaccination among Female College Students in China: A Multicenter Study. Vaccines (Basel) 2020;8(1):31. doi: 10.3390/vaccines8010031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lin W, Wang Y, Liu Z, Chen B, Yuan S, Wu B. et al. Inequalities in Awareness and Attitude towards HPV and Its Vaccine between Local and Migrant Residents Who Participated in Cervical Cancer Screening in Shenzhen, China. Cancer Res Treat. 2020;52(1):207–17. doi: 10.4143/crt.2019.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kristina S, Darmawan K, Sandy N, Worojati T. Perception of seriousness, knowledge, and willingness to pay for cervical cancer screening among women in Indonesia. Int Medical J. (1994)2020;25(4):2019–26. [Google Scholar]
- 46. Bank TW. World Bank Country and Lending Groups 2019 [Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519.
- 47. Lancaster KE, Lungu T, Bula A, Shea JM, Shoben A, Hosseinipour MC, et al. Preferences for Pre-exposure Prophylaxis Service Delivery Among Female Sex Workers in Malawi: A Discrete Choice Experiment. AIDS Behav. 2019. [DOI] [PMC free article] [PubMed]
- 48.Arbyn M, Weiderpass E, Bruni L, de Sanjosé S, Saraiya M, Ferlay J. et al. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Glob Health. 2020;8(2):e191–e203. doi: 10.1016/S2214-109X(19)30482-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hooi DJ, Quint WG, Lissenberg-Witte BI, Kenter G, Pinedo HM, de Koning MN. et al. Human papillomavirus (HPV) types prevalence in cervical samples of female sex-workers on Curaçao. Prev Med Rep. 2018;11:120–4. doi: 10.1016/j.pmedr.2018.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Santhanes D, Wong CP, Yap YY, San SP, Chaiyakunapruk N, Khan TM. Factors involved in human papillomavirus (HPV) vaccine hesitancy among women in the South-East Asian Region (SEAR) and Western Pacific Region (WPR): a scoping review. Hum Vaccin Immunother. 2018;14(1):124–33. doi: 10.1080/21645515.2017.1381811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bong A, Premaratne G. Regional integration and economic growth in Southeast Asia. Glob Bus Rev. 2018;19(6):1403–15. [Google Scholar]
- 52. Hill H. Southeast Asia in the global economy: a selective analytical survey. Philipp Rev Econ. 2018.
- 53. Organization WH. The selection and use of essential medicines: report of the WHO expert committee, 2015 (including the 19th WHO model list of essential medicines and the 5th WHO model list of essential medicines for children): World Health Organization; 2015.
- 54. FAAEM F. Tarascon Pocket Pharmacopoeia 2017 Deluxe Lab-Coat Edition: Jones & Bartlett Learning; 2016.
- 55.Altobelli E, Scarselli G, LattanzI A, Fortunato C, Profeta VF. A comparison between Pap and HPV screening tests and screening methods. Mol Clin Oncol. 2016;5(2):348–54. doi: 10.3892/mco.2016.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Randall TC, Ghebre R. Challenges in prevention and care delivery for women with cervical cancer in sub-Saharan Africa. Front Oncol. 2016;6:160. doi: 10.3389/fonc.2016.00160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chuang L, Temin S, Camacho R, Dueñas-Gonzalez A, Feldman S, Gultekin M. Management and Care of Women With Invasive Cervical Cancer: American Society of Clinical Oncology Resource-Stratified Clinical Practice Guideline. J Glob Oncol. 2016;2:311–40. doi: 10.1200/JGO.2016.003954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Small Jr W, Bacon MA, Bajaj A, Chuang LT, Fisher BJ, Harkenrider MM. et al. Cervical cancer: a global health crisis. Cancer. 2017;123(13):2404–12. doi: 10.1002/cncr.30667. [DOI] [PubMed] [Google Scholar]
- 59.LaVigne AW, Triedman SA, Randall TC, Trimble EL, Viswanathan AN. Cervical cancer in low and middle income countries: Addressing barriers to radiotherapy delivery. Gynecol Oncol Rep. 2017;22:16–20. doi: 10.1016/j.gore.2017.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Canfell K, Kim JJ, Brisson M, Keane A, Simms KT, Caruana M. et al. Mortality impact of achieving WHO cervical cancer elimination targets: a comparative modelling analysis in 78 low-income and lower-middle-income countries. Lancet. 2020;395(10224):591–603. doi: 10.1016/S0140-6736(20)30157-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Thapa N, Maharjan M, Petrini MA, Shah R, Shah S, Maharjan N. et al. Knowledge, attitude, practice and barriers of cervical cancer screening among women living in mid-western rural, Nepal. J Gynecol Oncol. 2018;29(4) doi: 10.3802/jgo.2018.29.e57. [DOI] [PMC free article] [PubMed] [Google Scholar]