Abstract
Background
Non-vitamin K antagonist oral anticoagulants (NOACs) are as effective and safe as warfarin for thromboembolic prevention and treatment. The efficacy of NOACs lacks evidence from large and randomized studies in patients with inherited severe thrombophilia, including protein S deficiency. Further, some concerns still exist regarding the relative efficacy of edoxaban in preventing arterial thromboembolism in patients with normal to high creatinine clearance (CrCl). We present a case of a rare complication of lead thrombus under standard-dose edoxaban in a patient with protein S deficiency and supernormal renal function.
Case presentation
A 65-year-old man experienced persistent chest tightness and a high level of D-dimer. Chest computed tomography (CT) showed a lead thrombus at the superior vena cava. He had a medical history including, paroxysmal atrial fibrillation (PAf), sick sinus syndrome after permanent pacemaker implantation, and transient ischemic attack. He received standard-dose edoxaban (60 mg daily) after PAf was diagnosed. His estimated CrCl was 98.6–102.1 mL/min. However, protein S deficiency (22.8%; normal range: 55–130%) was diagnosed. After switching to dabigatran (150 mg twice daily) for 3 months, the chest CT showed lead thrombus resolution and no symptoms were seen during the follow-up period.
Conclusions
This case was a rare complication of lead thrombus in a protein S deficient patient with normal renal function receiving standard-dose edoxaban. Edoxaban efficacy is uncertain in patients with protein S deficiency, and intracardiac devices also increase the risk of thromboembolic events.
Keywords: Lead thrombus, Edoxaban, Paroxysmal atrial fibrillation, Protein S deficiency
Background
Non-vitamin K antagonist oral anticoagulants (NOACs) are as effective and safe as warfarin for thromboembolic prevention. In patients with inherited severe thrombophilia, including protein S deficiency, the efficacy of NOACs is still controversial. Some concerns still exist regarding the relative efficacy of edoxaban in preventing arterial thromboembolism in patients with normal to high creatinine clearance (CrCl). We present the case of a thromboembolic event (lead thrombus) that occurred from using standard-dose edoxaban in a patient with paroxysmal atrial fibrillation (PAf) and protein S deficiency but with normal renal function.
Case presentation
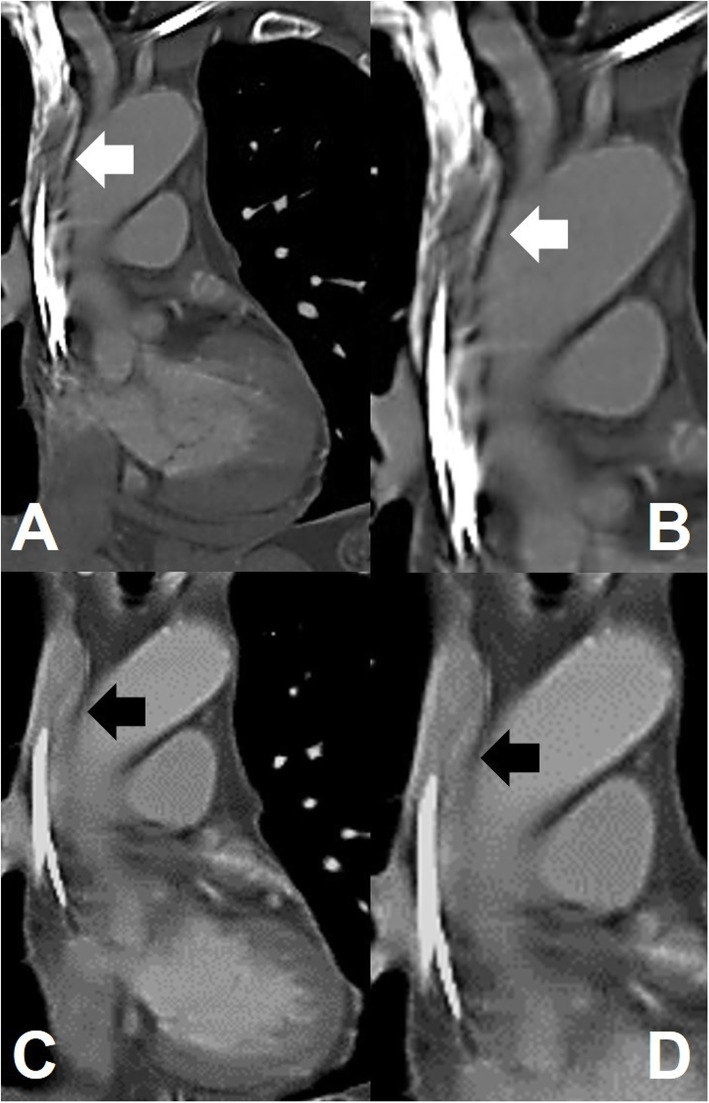
A 56-year-old man experienced chest tightness for hours, which gradually worsened for a day. Chest discomfort was more severe at the peak of inhalation. The tenderness was located at the central and upper chest wall, which radiated to the back. No cold sweating or compression was observed. He visited our emergency department for advanced evaluation and treatment. Electrocardiography showed normal pacemaker rhythm and no ST-T segment changes. Cardiac biomarker levels were normal, but a high D-dimer level (6.57 mg/L; normal range: < 0.5 mg/L) was noted. Emergency chest computed tomography (CT) revealed no pulmonary embolism but presented a filling defect in the right internal jugular vein and superior vena cava, which was highly suspected lead thrombosis (Fig. 1A, B; white arrows). Due to persistent symptoms, we did not suspect flow artefact or laminal effects.
Fig. 1.
Chest computed tomography. A, B. A filling defect in the right internal jugular vein and superior vena cava was noted with highly suspected lead thrombosis coated on the pacemaker leads (white arrows). Follow-up chest computed tomography. C, D. No filling defect and no residual lead thrombus were noted (black arrows)
The patient had a medical history of transient ischemic attack 7 years earlier. He also experienced dizziness and was diagnosed with PAf and sick sinus syndrome with long pauses (> 3 s) 2 years ago. After being diagnosed with PAf, he received standard-dose edoxaban (60 mg) daily for stroke prevention and received a transvenous permanent pacemaker for symptomatic bradycardia. CrCl estimated by the Cockcroft-Gault formula was supernormal to normal (98.6–102.1 mL/min). The burden of PAf was approximately 0.2–1% in pacemaker records after pacemaker implantation and the use of antiarrhythmic agents (amiodarone 100 mg daily). Intracardiac electrogram did not detect any atrial high rate in the last 3 months but noted protein S deficiency (22.8%; normal range: 55–130%). He did not receive p-glycoprotein or CYP3A4 inducers but did receive low-dose atorvastatin (10 mg daily). Then, 150 mg dabigatran twice daily was administered to resolve the thrombus and secondary prevention of thromboembolic events. Three months later, chest CT also showed no filling defect and no residual lead thrombus (Fig. 1C, D; black arrows). The patient denied recurrent chest discomfort during the half-year follow-up period. His medical history is listed in Fig. 2 and his biological characteristics are listed in Table 1.
Fig. 2.
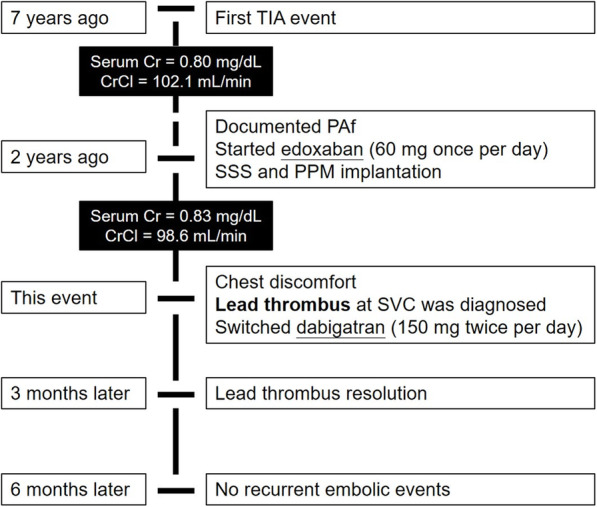
Perspective section about medical history. Abbreviations: TIA: transient ischemic attack; Cr: creatinine; CrCl: creatinine clearance; PAf: paroxysmal atrial fibrillation; SSS: sick sinus syndrome; PPM: permanent pacemaker; SVC: superior vena cava
Table 1.
Summary of biological characteristics
| Variable | Value | Normal range |
|---|---|---|
| D-dimer (mg/L) | 6.57 | < 0.5 |
| Creatinine (mg/dL) | 0.80–0.83 | 0.64–1.27 |
| Estimated CrCl (mL/min) | 102.12–98.57 | |
| Anti-thrombin III (%) | 99.2 | 75–125 |
| Protein-S (%) | 22.8 | 55–130 |
| Protein-C (%) | 77.3 | 70–140 |
| C3 (mg/dL) | 116.00 | 90–180 |
| C4 (mg/dL) | 21.30 | 10–40 |
| ANA | negative | negative |
| A-DSDNA (WHOunit/mL) | < 40.5 | < 92.6 |
Abbreviation: CrCl Creatinine clearance, ANA Antinuclear antibody, A-DSDNA Anti-double stranded DNA
Discussion
This was a case of lead thrombus under standard-dose edoxaban and a diagnosis of protein S deficiency. The patient still had a medical history of PAf, but a low burden (0.2–1%) was noted in the intracardiac electrogram. No strong drug-drug interaction was noted, and the patient also presented good medical adherence. Low-dose atorvastatin did not affect the efficacy of edoxaban. Because he had supernormal to normal renal function, inadequate protection against thromboembolic events caused by edoxaban needed to be considered. Protein S deficiency and intracardiac devices also increased the risk of thromboembolism. Edoxaban was switched to dabigatran (150 mg twice daily), and chest CT 3 months later revealed resolution of the lead thrombus. The associated chest discomfort was also resolved. Therefore, there are three potential underlying reasons for the therapeutic failure in the present case: first, a high-risk patient with protein S deficiency; second, uncertain edoxaban efficacy in the presence of an intracardiac device; and third, uncertain edoxaban efficacy in a patient with normal renal function.
In large randomized controlled trials, NOACs have been shown to be as effective and safe as warfarin [1–4]. NOACs also reduced the composite end point of stroke (odds ratio = 0.65) and systemic embolic events (odds ratio = 0.85) when compared with warfarin [5]. Edoxaban acts as a direct factor Xa inhibitor and renal clearance accounts for approximately 50% of the total clearance of edoxaban [6]. There are some concerns regarding the relative efficacy of edoxaban in preventing arterial thromboembolism in patients with CrCl > 95 mL/min [7]. Such concerns are of particular interest considering the United States Food and Drug Administration label, which restricts its use in patients with CrCl > 95 mL/min because of concerns of decreased efficacy in preventing arterial thromboembolism compared with warfarin [8]. However, both doses of edoxaban have been associated with reduced risks of stroke and systemic embolism without decreased efficacy when standard-dose edoxaban has been used in the presence of higher CrCl (> 95 mL/min) in real-world practice [9].
Pacemaker implantation is complicated by major thromboembolic events in 0.6–3.5% of cases [10]. One case report stated pacemaker-associated thrombosis in ongoing therapy with reduced-dose edoxaban [11]. Few previous reports have discussed thromboembolic events in patients with supernormal or normal renal function. Two other case reports have presented lead thrombi under other anti-factor Xa inhibitors [12, 13]. NOACs have comparable efficacy to warfarin for treating and preventing venous thromboembolisms (VTEs) [14]. Natural anticoagulant deficiencies (protein C, protein S, or anti-thrombin), homozygous factor V Leiden (FVL), and prothrombin G20210A, or combined defects, result in a severe thrombophilic phenotype, occurring in approximately 5% of patients with idiopathic VTE [15]. However, few studies have focused on the efficacy of NOACs for the treatment of inherited severe thrombophilia. A case series reported lower efficacy of NOACs in patients with protein S deficiency [16], but it did not present any data regarding edoxaban. In two meta-analyses, the rates of VTE recurrence were both low and were comparable in patients with various thrombophilias receiving either treatment; therefore, NOACs are an appropriate treatment option in this population [14, 17].
In clinical practice, NOAC therapy does not require routine monitoring of NOAC levels for dose adjustment [18, 19]. However, NOAC level measurement needs to be considered if the patients present special situations including, (A) acute or chronic renal insufficiency; (B) thrombolytic therapy consideration; (C) clinically significant bleeding; (D) therapeutic failure with recurrent VTE; or (E) urgent or emergent invasive procedures [20, 21]. Additionally, there are other scenarios where NOAC levels could be useful such as in patients with extreme body weights, the presence of interacting medications, and confirmation of chronic anticoagulation following the initial loading period [22]. Unfortunately, NOAC level measurements were not available in our hospital, so we did not know the efficacy of edoxaban in this patient with protein S deficiency, an intracardiac device, and normal renal function. Therefore, we switched to the direct thrombin inhibitor dabigatran to solve the therapeutic failure of edoxaban. Fortunately, the lead thrombus resolved, and no recurrent thromboembolic events happened in the follow-up period.
Conclusions
This case was a rare complication of lead thrombus in a patient with normal renal function receiving standard-dose edoxaban. Eoxaban inefficacy can be suspected in patients with protein S deficiency, and intracardiac devices also increase the risk of thromboembolic events.
Acknowledgements
None.
Disclosures
None.
Authors’ contributions
WC Lee wrote the manuscript. MP Huang prepared the figures and table. WC Lee did the final revision. All authors reviewed and approved the final manuscript.
Funding
None.
Availability of data and materials
Data available on request from the authors.
Declarations
Ethics approval and consent to participate
This case report followed the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1964 and later revisions.
Consent for publication
All authors read and approved this manuscript for publication.
Competing interests
None.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, Pogue J, Reilly PA, Themeles E, Varrone J, Wang S, Alings M, Xavier D, Zhu J, Diaz R, Lewis BS, Darius H, Diener HC, Joyner CD, Wallentin L. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361(12):1139–1151. doi: 10.1056/NEJMoa0905561. [DOI] [PubMed] [Google Scholar]
- 2.Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, Breithardt G, Halperin JL, Hankey GJ, Piccini JP, Becker RC, Nessel CC, Paolini JF, Berkowitz SD, Fox KAA, Califf RM, the ROCKET AF Steering Committee Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365(10):883–891. doi: 10.1056/NEJMoa1009638. [DOI] [PubMed] [Google Scholar]
- 3.Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365(11):981–992. doi: 10.1056/NEJMoa1107039. [DOI] [PubMed] [Google Scholar]
- 4.Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL, Waldo AL, Ezekowitz MD, Weitz JI, Špinar J, Ruzyllo W, Ruda M, Koretsune Y, Betcher J, Shi M, Grip LT, Patel SP, Patel I, Hanyok JJ, Mercuri M, Antman EM. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369(22):2093–2104. doi: 10.1056/NEJMoa1310907. [DOI] [PubMed] [Google Scholar]
- 5.Wang KL, Lip GY, Lin SJ, Chiang CE. Non-vitamin K antagonist Oral anticoagulants for stroke prevention in Asian patients with Nonvalvular atrial fibrillation: meta-analysis. Stroke. 2015;46(9):2555–2561. doi: 10.1161/STROKEAHA.115.009947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ogata K, Mendell-Harary J, Tachibana M, Masumoto H, Oguma T, Kojima M, Kunitada S. Clinical safety, tolerability, pharmacokinetics, and pharmacodynamics of the novel factor Xa inhibitor edoxaban in healthy volunteers. J Clin Pharmacol. 2010;50(7):743–753. doi: 10.1177/0091270009351883. [DOI] [PubMed] [Google Scholar]
- 7.Bohula EA, Giugliano RP, Ruff CT, Kuder JF, Murphy SA, Antman EM, Braunwald E. Impact of renal function on outcomes with edoxaban in the ENGAGE AF-TIMI 48 trial. Circulation. 2016;134(1):24–36. doi: 10.1161/CIRCULATIONAHA.116.022361. [DOI] [PubMed] [Google Scholar]
- 8.US Food and Drug Administration . Prescribing information for Savaysa (edoxaban) 2015. [Google Scholar]
- 9.Yu HT, Yang PS, Kim TH, Jang E, Kim D, Uhm JS, Kim JY, Pak HN, Lee MH, Lip GYH, Joung B. Impact of renal function on outcomes with edoxaban in real-world patients with atrial fibrillation. Stroke. 2018;49(10):2421–2429. doi: 10.1161/STROKEAHA.118.021387. [DOI] [PubMed] [Google Scholar]
- 10.Barakat K, Robinson NM, Spurrell RA. Transvenous pacing lead-induced thrombosis: a series of cases with a review of the literature. Cardiology. 2000;93(3):142–148. doi: 10.1159/000007018. [DOI] [PubMed] [Google Scholar]
- 11.Di Vincenzo A, Rizzo A, Russo L, Mioni R. Pacemaker-associated thrombosis in ongoing therapy with edoxaban tosylate. J Thromb Thrombolysis. 2018;46(4):549–550. doi: 10.1007/s11239-018-1733-z. [DOI] [PubMed] [Google Scholar]
- 12.Michałek P, Kubaszek-Kornatowska A, Pręgowska-Chwała B. Późna zakrzepica żyły podobojczykowej lewej po wszczepieniu układu stymulującego skutecznie leczona riwaroksabanem [Late pacemaker lead thrombosis treated with rivaroxaban] Kardiol Pol. 2014;72(9):840. doi: 10.5603/KP.2014.0173. [DOI] [PubMed] [Google Scholar]
- 13.Adar A, Önalan O, Cakan F. Development of pacemaker Lead thrombosis in a patient with atrial fibrillation during Apixaban treatment. J Tehran Heart Cent. 2019;14(4):183–186. [PMC free article] [PubMed] [Google Scholar]
- 14.van der Hulle T, Kooiman J, den Exter PL, Dekkers OM, Klok FA, Huisman MV. Effectiveness and safety of novel oral anticoagulants as compared with vitamin K antagonists in the treatment of acute symptomatic venous thromboembolism: a systematic review and meta-analysis. J Thromb Haemost. 2014;12(3):320–328. doi: 10.1111/jth.12485. [DOI] [PubMed] [Google Scholar]
- 15.Franchini M, Veneri D, Salvagno GL, Manzato F, Lippi G. Inherited thrombophilia. Crit Rev Clin Lab Sci. 2006;43(3):249–290. doi: 10.1080/10408360600552678. [DOI] [PubMed] [Google Scholar]
- 16.Undas A, Goralczyk T. Non-vitamin K antagonist oral anticoagulants in patients with severe inherited thrombophilia: a series of 33 patients. Blood Coagul Fibrinolysis. 2017;28(6):438–442. doi: 10.1097/MBC.0000000000000613. [DOI] [PubMed] [Google Scholar]
- 17.Elsebaie MAT, van Es N, Langston A, Büller HR, Gaddh M. Direct oral anticoagulants in patients with venous thromboembolism and thrombophilia: a systematic review and meta-analysis. J Thromb Haemost. 2019;17(4):645–656. doi: 10.1111/jth.14398. [DOI] [PubMed] [Google Scholar]
- 18.Eikelboom JW, Quinlan DJ, Hirsh J, Connolly SJ, Weitz JI. Laboratory monitoring of non-vitamin K antagonist Oral anticoagulant use in patients with atrial fibrillation: a review. JAMA Cardiol. 2017;2(5):566–574. doi: 10.1001/jamacardio.2017.0364. [DOI] [PubMed] [Google Scholar]
- 19.Rottenstreich A, Zacks N, Kleinstern G, Raccah BH, Roth B, Da'as N, et al. Direct-acting oral anticoagulant drug level monitoring in clinical patient management. J Thromb Thrombolysis. 2018;45(4):543–549. doi: 10.1007/s11239-018-1643-0. [DOI] [PubMed] [Google Scholar]
- 20.Weitz JI, Eikelboom JW. Urgent need to measure effects of direct Oral anticoagulants. Circulation. 2016;134(3):186–188. doi: 10.1161/CIRCULATIONAHA.116.022307. [DOI] [PubMed] [Google Scholar]
- 21.Tripodi A, Ageno W, Ciaccio M, Legnani C, Lippi G, Manotti C, Marcucci R, Moia M, Morelli B, Poli D, Steffan A, Testa S. Position paper on laboratory testing for patients on direct oral anticoagulants. A consensus document from the SISET, FCSA, SIBioC and SIPMeL. Blood Transfus. 2018;16(5):462–470. doi: 10.2450/2017.0124-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tripodi A. The laboratory and the new oral anticoagulants. Clin Chem. 2013;59(2):353–362. doi: 10.1373/clinchem.2012.189704. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data available on request from the authors.