Abstract
Prostate-specific membrane antigen (PSMA) is a glycosylated type-II transmembrane protein highly expressed in individual tumor cells. Lesions with PSMA expression in the liver are commonly reported as prostate cancer metastasis or hepatocellular cancer previously. This is the first case reported as hepatic focal nodular hyperplasia, mimicking hepatocellular carcinoma with imaging features. This patient, having a lesion that has been enlarged from 2.0 cm to 2.5 cm in 3 months, was referred to our department for restaging by gallium-68 PSMA (68Ga-PSMA) positron emission tomography/computed tomography (PET/CT). The CT scan showed a focal segment VI hypodensity, which was significantly PSMA-avid. Consequently, its biopsy resulted as focal nodular hyperplasia in liver. His follow-up 68Ga-PSMA PET/CT ultimately revealed a mass lesion of 8 cm of axial diameter.
Keywords: Focal nodular hyperplasia, gallium-68-prostate-specific membrane antigen positron emission tomography/computed tomography, hepatocellular cancer, liver, metastasis, pitfall, prostate cancer
INTRODUCTION
Focal nodular hyperplasia (FNH) is the second most common benign tumor of the liver, with an incidence of approximately 3%–5% in general population. We present a male case which has been followed conservatively with FNH in which the growth of liver lesion is thought to be associated with the use of androgen deprivation therapy (ADT) for primary prostate cancer.
CASE REPORT
A 66-year-old man who had been diagnosed as prostate cancer pT2cN0M1b, with Gleason score 8 (4 + 4) and had received chemotherapy in 2015 underwent restaging by gallium-68-prostate-specific membrane antigen (68Ga-PSMA) positron emission tomography/computed tomography (PET/CT) in June 2017 after a prostate-specific antigen (PSA) spike of 8.0 ng/ml. among his previous fluctuating PSA levels without a steady increase, after having his written consent. This PET/CT revealed increased levels of radiopharmaceutical in prostate gland with metastatic bone and lymph node lesions, with a subtle liver lesion in segment VI [Figure 1a-d] without any prominent lesion on noncontrast CT.
Figure 1.
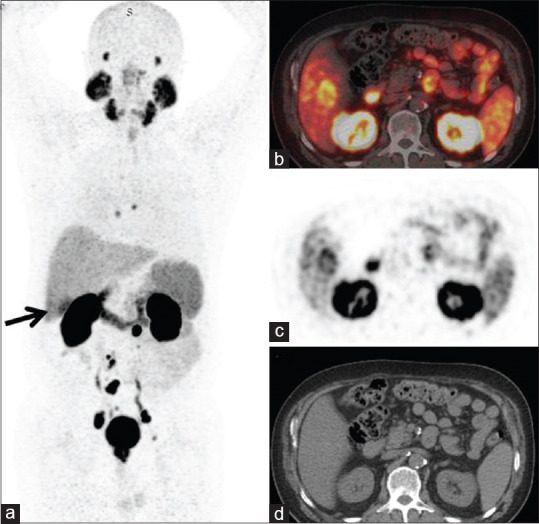
A 66-year-old man with prostate cancer restaged with gallium- 68-prostate-specific membrane antigen positron emission tomography/ computed tomography. Sixty minutes after administration of 278 MBq gallium-68-prostate-specific membrane antigen-HBED-CC, an intense uptake, with a diameter of 2 cm appeared in liver segment VI (a: arrow). Tru-cut biopsy of the liver performed, and histopathology revealed focal nodular hyperplasia. Gallium-68-prostate-specific membrane antigen-HBED-CC positron emission tomography/computed tomography showed peripherally increased prostate-specific membrane antigen expression around the hypodense liver lesion (b-d), apart from prostate tumoral, bone, supra-, infradiaphragmatic metastatic lymph nodes and physiological uptakes
The heterogeneous uptake of 68Ga-PSMA in liver segment VI was interpreted as hepatocellular cancer (HCC) or an organ metastasis from his primary prostate cancer. Although follow-up magnetic resonance imaging (MRI) was in favor of metastasis [Figure 2], the double checked histopathological findings ended-up as ductular proliferation and fibrosis of liver containing some vascular structures, that is, typical for FNH.[1]
Figure 2.
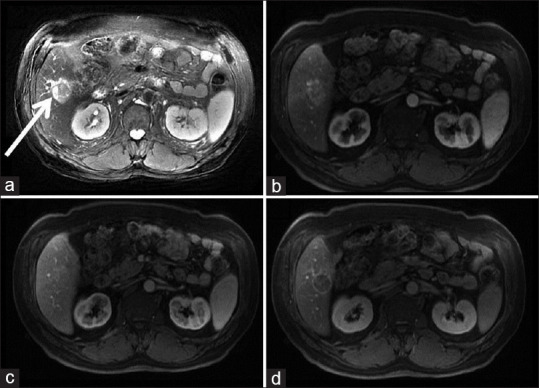
Upper abdominal magnetic resonance images. T2 weighted imaging (T2WI) shows a hyperintense mass in the right lobe of the liver (a–white arrow). Early arterial enhancement has seen in contrast-enhanced dynamic T1 weighted images (T1WIC+) (b) Contrast washes out in the equilibrium phase. (c) Enhancing the capsule on the delayed images (d)
During his follow-up, another 68Ga-PSMA PET/CT ordered in January 2020 showed multiple lesions with intense uptakes of the tracer in prostate, multiple infra-diaphragmatic lymph nodes, left of acetabulum posteriorly, and a markedly progressive liver lesion in segment VI [Figure 3b].
Figure 3.
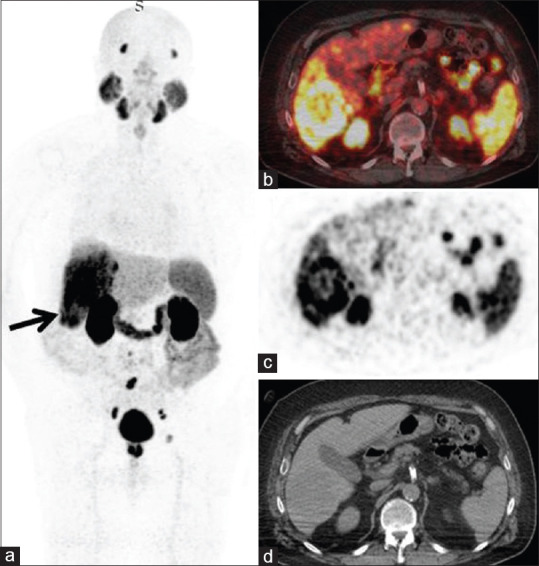
The patient treated with gonadotropin releasing hormone analogs and restaged in January 2020 with a decrease in prostate specific antigen levels to 3.54 ng/ml from previous records. Current scans (a-d) showed increase in liver lesion, from 2.0 cm to 8.0 cm, diagnosed as focal nodular hyperplasia with stable metastatic lymph node and bone lesions from prostate cancer
DISCUSSION
Metastatic prostate cancer has potential to disseminate in body organs especially after it changes to castration resistant form. Main sites of metastasis were known as lymph nodes, bone and lungs but liver metastasis are not so infrequent in these patients.[2] 68Ga-PSMA hybrid imaging is becoming modality of choice in the current follow-up of this kind of patients selectively wherever it is available and found more useful then biochemical markers. But it has some drawbacks due to its false-positive results: HCC,[3] renal cell cancer,[4] colorectal cancer,[5] follicular thyroid carcinoma,[6] anthracosis,[7] mediastinal sarcoidosis,[8] hepatic hemangioma,[9] vertebral hemangioma,[10] and glioblastoma.[11]
In this case report, we presented an intriguing liver uptake of 68Ga-PSMA, which could be interpreted as HCC or a metastatic lesion from prostate cancer. Further work-up even with MRI was not confirmative unless a histopathological examination was done.
The continued clinical survey of this patient suggested the primary prostate cancer had favorable course in pace with the PET/CT images showing stable disease in metastatic lymph node and bone lesions [Figure 3]. However, the relatively increased size of segment VI lesion in liver was noticed in his serial follow-up MRIs. This phenomena was hypothetically defined as a lesion progression probably due to the increased levels of estrogen as a result of ADT for primary prostate cancer and should be considered as a pitfall in the interpretation of liver lesions in those prostate cancer patients scanned with 68Ga-PSMA PET/CT.[12]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Zimmermann A. General and Surgical Pathology. Cham: Springer International Publishing; 2017. Focal Nodular Hyperplasia (FNH) of the Liver. Tumors and Tumor-Like Lesions of the Hepatobiliary Tract; pp. 2057–90. [Google Scholar]
- 2.Bubendorf L, Schöpfer A, Wagner U, Sauter G, Moch H, Willi N, et al. Metastatic patterns of prostate cancer: An autopsy study of 1,589 patients. Hum Pathol. 2000;31:578–83. doi: 10.1053/hp.2000.6698. [DOI] [PubMed] [Google Scholar]
- 3.Kuyumcu S, Has-Simsek D, Iliaz R, Sanli Y, Buyukkaya F, Akyuz F, et al. Evidence of prostate-specific membrane antigen expression in hepatocellular carcinoma using 68Ga-PSMA PET/CT. Clin Nucl Med. 2019;44:702–6. doi: 10.1097/RLU.0000000000002701. [DOI] [PubMed] [Google Scholar]
- 4.Demirci E, Ocak M, Kabasakal L, Decristoforo C, Talat Z, Halaç M, et al. (68) Ga-PSMA PET/CT imaging of metastatic clear cell renal cell carcinoma. Eur J Nucl Med Mol Imaging. 2014;41:1461–2. doi: 10.1007/s00259-014-2766-y. [DOI] [PubMed] [Google Scholar]
- 5.Hangaard L, Jochumsen MR, Vendelbo MH, Bouchelouche K. Metastases from colorectal cancer avid on 68Ga-PSMA PET/CT. Clin Nucl Med. 2017;42:532–3. doi: 10.1097/RLU.0000000000001700. [DOI] [PubMed] [Google Scholar]
- 6.Sager S, Vatankulu B, Uslu L, Sönmezoglu K. Incidental detection of follicular thyroid carcinoma in 68Ga-PSMA PET/CT imaging. J Nucl Med Technol. 2016;44:199–200. doi: 10.2967/jnmt.115.171660. [DOI] [PubMed] [Google Scholar]
- 7.Elri T, Aras M, Salihoglu YS, Erdemir RU, Cabuk M. A potential pitfall in the use of 68Ga-PSMA PET/CT: Anthracosis. Rev Esp Med Nucl Imagen Mol. 2017;36:65–6. doi: 10.1016/j.remn.2016.06.011. [DOI] [PubMed] [Google Scholar]
- 8.Ardies PJ, Gykiere P, Goethals L, De Mey J, De Geeter F, Everaert H. PSMA uptake in mediastinal sarcoidosis. Clin Nucl Med. 2017;42:303–5. doi: 10.1097/RLU.0000000000001543. [DOI] [PubMed] [Google Scholar]
- 9.Bhardwaj H, Stephens M, Bhatt M, Thomas PA. Prostate-specific membrane antigen PET/CT findings for hepatic hemangioma. Clin Nucl Med. 2016;41:968–9. doi: 10.1097/RLU.0000000000001384. [DOI] [PubMed] [Google Scholar]
- 10.Probst S, Bladou F, Abikhzer G. Extraosseous extension of aggressive vertebral hemangioma as a potential pitfall on 68Ga-PSMA PET/CT. Clin Nucl Med. 2017;42:624–5. doi: 10.1097/RLU.0000000000001731. [DOI] [PubMed] [Google Scholar]
- 11.Sasikumar A, Kashyap R, Joy A, Charan Patro K, Bhattacharya P, Reddy Pilaka VK, et al. Utility of 68Ga-PSMA-11 PET/CT in imaging of glioma-a pilot study. Clin Nucl Med. 2018;43:e304–9. doi: 10.1097/RLU.0000000000002175. [DOI] [PubMed] [Google Scholar]
- 12.Chandrasegaram MD, Shah A, Chen JW, Ruszkiewicz A, Astill DS, England G, et al. Oestrogen hormone receptors in focal nodular hyperplasia. HPB (Oxford) 2015;17:502–7. doi: 10.1111/hpb.12387. [DOI] [PMC free article] [PubMed] [Google Scholar]


