Abstract
Although genetic factors may contribute to initial liability for ADHD onset, there is growing evidence of the potential importance of the rearing environment on the developmental course of ADHD symptomatology. However, associations between family-level variables (maternal hostility, maternal depressive symptoms) and child behaviors (developmental course of ADHD and aggression) may be explained by genes that are shared by biologically related parents and children. Furthermore, ADHD symptoms and aggression commonly co-occur: it is important to consider both simultaneously to have a better understanding of processes underlying the developmental course of ADHD and aggression. To addresses these issues, we employed a longitudinal genetically sensitive parent-offspring adoption design. Analyses were conducted using Cohort I (n = 340) of the Early Growth and Development Study with cross-validation analyses conducted with Cohort II (n = 178). Adoptive mother hostility, but not depression, was associated with later child ADHD symptoms and aggression. Mothers and their adopted children were genetically unrelated, removing passive rGE as a possible explanation. Early child impulsivity/activation was associated with later ADHD symptoms and aggression. Child impulsivity/activation was also associated with maternal hostility, with some evidence for evocative gene-environment correlation processes on adoptive mother depressive symptoms. This study provides novel insights into family-based environmental influences on child ADHD and aggression symptoms, independent of shared parental genetic factors, implications of which are further explicated in the discussion.
Keywords: aggression, ADHD symptoms, maternal depression, maternal hostility, gene-environment correlation
Attention Deficit Hyperactivity Disorder (ADHD) is a neurodevelopmental disorder characterized by symptoms of hyperactivity, impulsivity, and inattention (American Psychological Association, 2013; Polanczyk et al., 2014) that, like autism spectrum disorder, typically onsets early in development. There is substantial evidence that ADHD, like other psychiatric disorders, is familial, with children of adults with ADHD at increased risk of developing ADHD themselves (Biederman et al., 1995; Faraone et al., 2000; Stergiakouli & Thapar, 2010). Twin studies show high heritability estimates of around 70 – 90% (Thapar et al., 2013; Thapar et al., 2012; Stergiakouli & Thapar, 2010), with adoption studies also evidencing genetic contributions to ADHD (see Thapar et al., 2013). The influence of non-inherited factors is also important, and although genetic factors may contribute to liability for initial ADHD onset, there is growing evidence of the potential importance of the rearing environment on the developmental course of ADHD symptomatology. However, a number of issues remain unaddressed: First associations between family level variables (e.g., maternal hostility; maternal depressive symptoms) and child outcomes may be explained by genes that are shared by biologically related parents and children. Thus it is necessary to examine associations between these family level variables and child outcomes using designs where parents and children are not genetically related. Second, family level variables have been associated with both child ADHD symptom course and child aggression. Given that ADHD symptoms and aggression commonly co-occur, it is important to consider both simultaneously to have a better understanding of the role family level variables (hostile maternal parenting and depressive symptoms) for the developmental course of both aggression and ADHD. Third, the specificity of early child characteristics (e.g., impulsivity) on child outcomes is unclear. Fourth, there is relatively limited examination of potential child effects of early child liability for ADHD on parent mental health, particularly parental depressive symptoms. The present study addresses these knowledge gaps, thus further developing understanding of genetic and environmental processes for the co-development of ADHD and aggression (see Figure 1 for a conceptual model).
Figure 1:
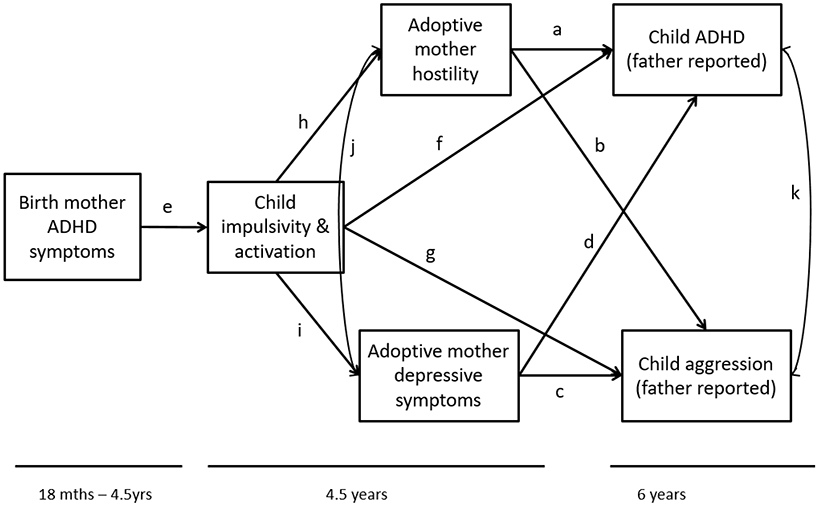
Conceptual model examining the relationship between birth mother ADHD symptoms, child impulsivity/activation, adoptive mother depressive symptoms and hostility, child ADHD symptoms, and child aggression. Letters refer to paths tested.
The contribution of the rearing environment to ADHD developmental course: maternal hostility and depression
Although observational studies find that parenting behaviors, including parental hostility, are associated with child ADHD symptoms (Choenni et al., 2018; Johnston & Mash, 2001; Harold et al., 2013; Ullsperger, Nigg, & Nikolas, 2016; Barkley et al., 1991; Lange et al., 2005; Lifford et al., 2008), these designs do not include the contribution of genetic factors shared by parent and child. Whilst hostile parenting may be associated with ADHD symptom course, the association between maternal hostility and child ADHD symptoms may be accounted for by genetic factors (Lifford et al., 2009; Harold et al, 2013; see also section on gene-environment correlation). The co-occurrence of genetic and environment contributions transmitted intergenerationally from parent to child are important to disentangle, if we are to better understand what family factors impact on the developmental course of ADHD.
Parental depression is a second well-established environmental risk factor for the development of psychopathology in children (Natsuaki et al., 2014), and has been associated with child ADHD symptoms (Shaw et al., 2005; Cheung et al., 2018; Nigg & Hinshaw, 1998). A number of mechanisms are thought to be involved in the association between parental depression and psychopathology, including disruptions in the parent child relationship (Lovejoy et al., 2000). Interestingly, recent studies show a strong genetic overlap between ADHD and depression (Demontis et al., 2019). Therefore, it is important to examine the associations using a genetically informative design.
Early temperament: an early manifestation of ADHD
Despite interest in the conceptual and empirical overlap between early temperamental dimensions and risk for subsequent ADHD (Nigg et al., 2004; Nigg, 2006), few studies have utilized longitudinal data to establish prospective associations (Foley et al., 2008; Martel, Nigg, & Von Eye, 2009). However, evidence is now emerging to suggest that specific early temperamental dimensions, including impulsivity, are associated with increased risk for later ADHD symptoms (Willoughby et al., 2017 et al., 2017; Miller et al., 2019; Harold et al, 2013; Frick et al 2019). Current frameworks consider impulsivity to be a multi-dimensional construct with several distinct dimensions, including activation difficulties such as behavioral inhibition, drive (sense of urgency, lack of planning, lack of persistence or perseverance), and sensation seeking (see Bezdjian, Baker, & Tuvblad, 2011; García-Forero et al., 2009; Congdon & Cani, 2005; Nigg et al., 2004). Therefore, we considered a measure of impulsivity/activation that encompassed these dimensions of impulsivity (behavioral inhibition, drive, fun seeking) and that are consistent with risk for later ADHD symptomatology (Harold et al., 2013; Congdon & Cani, 2005), and conceptualized this temperament dimension as an early liability factor for ADHD (Frick et al., 2019; Willoughby et al., 2017). Past evidence suggests early impulsivity in children evokes parental hostility (Harold et al., 2013). Building on this evidence, we include this measure in the present study, in addition to ADHD symptoms, aggression and family-level variables (see section ‘child effects on parents’).
Aggressive Behavior often Co-occurs with ADHD
Aggressive behaviors are relatively common among children (Hendriks et al., 2018; Bartels et al., 2018). Twin studies suggest aggressive behaviors are moderately heritable, with hertiability estimates of around 40-60% (Eley et al., 1999; Eley et al., 2003; Gelhorn et al., 2005; Mason & Frick, 1994; Vierikko et al., 2003). In addition, rearing environments are recognized as important for the development of aggression. Both maternal depression and maternal hostility have been associated with child disruptive behaviors such as aggression, conduct problems, and oppositional defiant behaviors (Pilowsky et al., 2006; Sellers et al., 2014; Stover et al., 2012). However, any association between parent hostility or depression with child aggression could also be due in part to shared genes (e.g., Klahr et al., 2014; Silberg et al., 2010; see section on ‘gene-environment correlation’).
Comorbid psychopathology in children is common and thought to be the rule rather than the exception (Caron & Rutter, 1991; Angold et al., 1999). ADHD and aggression commonly co-occur (Bartels et al., 2018; Biederman et al., 1996; Thapar et al., 2001). Comorbidity between ADHD and aggression may result, at least in part, from heritable mechanisms (Seroczynski et al., 1999; Nadder et al., 1998; Nadder et al., 2002; Thapar, et al., 2001), with most externalizing problems also demonstrating substantial shared environmental influences (Burt, 2009; Nikolas & Burt, 2010; Burt et al., 2001). Early impulsivity may thus predispose children to a broad range of psychopathology (Beauchaine et al., 2010; García-Forero et al., 2009; Bezdjian et al., 2011; Perry et al., 2018), but the specificity of risk to specific outcomes such as ADHD and aggression is unclear.
Furthermore, both maternal depression and maternal hostility have been associated with child disruptive behaviors such as aggression and with symptoms of ADHD. Therefore, any association between parent hostility or depressive symptoms and child aggression could be due to co-occurring ADHD symptoms (and vice versa) in the offspring. A recent study of biologically related parents and children suggested that negative parenting was no longer associated with child symptoms of ADHD after adjusting for co-occurring externalizing symptoms and earlier symptoms of ADHD (Choenni et al., 2018). Also, while parenting programs are an effective intervention for conduct problems (Scott & Gardner, 2015), and are helpful for improving parenting, there is no clear evidence of benefits to core ADHD symptoms (Daley et al, 2018). Early measures of child impulsivity have been evidenced to also play a role in the development of aggression, with lack of impulse control being associated with later aggression (see Bezdjian et al., 2011). Thus, it is important to examine whether specific family factors (e.g., maternal depressive symptoms, hostile parenting) and child characteristics (early impulsivity/activation) have effects on child ADHD symptom course and aggression, partialing out the effects of co-occurring symptomatology. This would provide a deeper understanding of factors that moderate and mediate liability to ADHD and comorbid psychopathology that is sorely needed (Martel et al., 2009).
Child Effects on Parents: Considering Early Temperament on Maternal Parenting & Depressive Symptoms
Children are also known to have effects on parents: recent twin and adoption studies suggest that early temperamental dimensions associated with risk for later ADHD symptoms (e.g., child impulsivity/activation) may evoke hostile parenting (Harold et al., 2013). However, the effects of child impulsivity on maternal depression have rarely been examined (Cheung et al., 2018), despite evidence suggesting that child ADHD and impulsivity are associated with parental distress and increases in parent psychopathology, including depression (Johnston & Mash, 2001; Deault 2010; Nigg & Hinshaw, 1998). Whilst it is increasingly recognized that children's psychopathology might impact maternal depression symptoms (Allen et al., 2010; Kouros & Garber, 2010; Nicholson et al., 2011; Sellers et al., 2016), there has been relatively limited examination that begins earlier; that is, the role of child impulsivity on maternal depression symptoms. One study of children in middle childhood provides evidence of bidirectional processes, but shows that the effects of maternal depressive symptoms on child hyperactivity tend to be stronger than the effects of child hyperactivity on maternal depression (Elgar et al., 2003). However, that study did not take into account parent-child genetic sharing (see next section). Therefore, more research is needed to examine the impact of early child indicators of risk for ADHD (e.g., impulsivity) on maternal depressive symptoms, in addition to effects on parenting processes such as maternal hostility (Harold et al., 2013; Miller et al., 2019).
Gene-Environment Correlation (rGE)
The majority of research examining the influences of family processes and child outcomes has typically been conducted with biologically related mothers and children. This makes it difficult to disentangle whether associations between family factors (e.g., parenting, parent depression) and child outcomes (e.g., ADHD symptoms, aggression) are due to environmental or shared genetic effects (Plomin et al., 1977). Three rGE processes have been described in the literature, with passive rGE and evocative rGE being the two most frequently examined. Passive rGE is indicated when parents’ genes (which are shared with their offspring) are correlated with the environment they provide, and therefore confound the association between family and child level variables (Plomin et al., 1977; Scarr & McCartney, 1983). Evocative rGE occurs when genetically influenced characteristics in a child evoke particular responses from others (Plomin et al., 1977). Evocative rGE effects have primarily been examined in the context of child disruptive behaviors, highlighting the importance of child disruptive behaviors evoking parent hostility (Elam et al., 2014; Neiderhiser et al., 2013; Riggins-Caspers et al., 2003; O’Connor et al., 1998), with some evidence of early child impulsivity evoking parent hostility, consistent with evocative rGE (Harold et al., 2013). There is less examination of evocative rGE processes of early child behavior on parent mental health. One recent study examined effects of infant negative affect on maternal anxiety, suggesting that increases in infant negative affect predicted more anxiety symptoms in adoptive parents (Brooker et al., 2015). More research is needed to examine evocative rGE processes of early child characteristics (specifically, impulsivity/activation) on maternal depressive symptoms.
To our knowledge, one study has used a longitudinal parent-offspring adoption design to disentangle genetic and environmental factors that may explain the association between parent ADHD, parenting practices, and child ADHD symptom course (Harold et al., 2013). This study, using Cohort I data from the Early Growth and Development Study (EGDS; Leve et al., 2019), found an association between adoptive mother hostility and child ADHD symptoms at age 6 years. The study also found evidence of evocative rGE, whereby biological mother ADHD symptoms, an index of inherited risk, had an indirect effect on adoptive mother hostility via child impulsivity/activation. However, this study did not include a measure of child aggression, which has been associated with both adverse parenting and ADHD symptoms. Furthermore, this study also did not examine the associations with maternal depressive symptoms, which have been associated with both hostile parenting and increased risk for child psychopathology (Harold et al., 2013; Lovejoy et al., 2000; Natsuaki, et al., 2014; Pemberton, et al., 2010). We therefore aimed to build on the findings from Harold and colleagues (2013), examining processes for both child ADHD symptom course and aggression, and including the role of maternal depressive symptoms and adding a second cohort of adoptive families as a replication test.
A number of questions remain to be addressed: First, is there an association between family level variables (maternal hostility; maternal depressive symptoms) and child outcomes (developmental course of ADHD and aggression) in children who are not genetically related (i.e., associations cannot be explained by shared genes) after taking into account the co-occurrence of ADHD symptoms and aggression? Given that family level variables have been associated with both child ADHD symptom course and child aggression, and that ADHD symptoms and aggression commonly co-occur, it is important to consider both simultaneously to have a better understanding of the role of hostile maternal parenting and depressive symptoms for the developmental course of both aggression and ADHD. Second, is early child impulsivity/activation associated with later child ADHD symptoms and aggression? Currently the specificity of early child temperament (e.g., impulsivity) on child outcomes is unclear. Third, does child early impulsivity/activation evoke maternal hostility and maternal depressive symptoms? Early child impulsivity/activation may affect both maternal hostility and maternal depressive symptoms (i.e., child effects on parents) but there is relatively limited examination of early child impulsivity/activation on these family processes, particularly examining potential evocative effects on maternal depression. The present study addresses these three research questions, thus further developing understanding of genetic and environmental processes for the co-development of ADHD and aggression.
The Present Study
The present study examined the interplay between genetic susceptibility and environmental processes (specifically, hostile maternal parenting and maternal depressive symptoms) in the developmental course of ADHD symptoms and aggression in middle childhood. We employed a longitudinal genetically sensitive parent-offspring adoption design (Leve et al., 2019). As part of the study design, children were not biologically related to their adoptive parents, thus removing the potential confound of passive rGE. The study included assessments of birth parent characteristics, allowing the examination of heritable risk, and considered whether genetic risk for ADHD (measured in the birth mother) was associated with early child impulsivity/activation. Furthermore, we were able to estimate evocative rGE (genetically influenced child characteristics) on specific family-level variables (specifically maternal hostility and depressive symptoms). Given concerns in the field regarding replicability of scientific findings (Conger et al., 1995; Lykken, 1968; Weisz, 1978), we also employed a cross-validation approach by examining these associations separately in two cohorts from EGDS (Cohorts I and II).
Specifically, we examined associations between genetically influenced (via birth mother symptoms of ADHD) early child impulsivity/activation on both maternal hostility and depressive symptoms (i.e., evocative rGE) as pathways associated with child ADHD symptom course and aggression (see Figure 1). We hypothesized that: (1) maternal hostility and maternal depressive symptoms would be associated with both child ADHD symptoms and child aggression after taking into consideration the co-occurrence of ADHD symptoms and aggression; (2) early child impulsivity/activation would be associated with later child ADHD symptoms and aggression; (3) early child impulsivity/activation would evoke maternal hostility and maternal depressive symptoms. We utilized a cross-rater approach to reduce the potential risk for shared method variance: adoptive mothers reported on their parenting and depressive symptoms, and fathers reported on child ADHD and aggression symptoms. We then sought to replicate the Cohort I model with Cohort II data.
Methods
Participants and Study Design
Participants were a subsample (n = 340) of 361 linked sets of adopted children, adoptive mothers and fathers, and biological mothers from Cohort I of the Early Growth and Development Study (EGDS), a longitudinal, multisite study of children adopted at birth (Leve et al., 2019). This subsample included all mother–father families who had data on at least one of the measures used in the present analyses. Cross-cohort validation analyses were conducted using a subsample (n = 178) of 200 linked sets of adopted children, adoptive mothers and fathers, and biological mothers from Cohort II of the EGDS study.
Participants were representative of the adoptive parent and birth parent populations that completed adoption plans at the participating agencies during the same time period. The EGDS sample was recruited between January 2003 and January 2010 in the United States across four recruitment sites (Mid-Atlantic, West/Southwest, Mid-West, and Pacific Northwest). Adoption agencies (N = 45 across 15 states) reflected the range of adoption agencies (e.g., private, public, religious, secular, and those with more open or more closed adoption philosophies). The median child age at adoption placement was 2 days (M = 6.2, SD = 12.45; range = 0 – 91 days). The majority of the children were male (Cohort I: 57.3%; Cohort II: 57.0%). The mean age of birth mothers at the time of childbirth was 24.4 years (Cohort I M = 24.1, SD = 5.9; Cohort II M = 24.8, SD = 6.3), and for birth fathers was 26.1 years (Cohort I M = 25.4, SD = 7.2; Cohort II M =27.0, SD = 8.5). The majority of birth parents were Caucasian (Cohort I birth mother = 71.1%, birth father = 74.6%; Cohort II birth mother = 68.4%, birth father = 62.7%), followed by African-American (Cohort I birth mother = 11.4%; birth father 8.7%; Cohort II birth mother = 16.8% birth father = 9.6%) and Hispanic/Latino (Cohort I birth mother = 6.7%; birth father = 8.7%; Cohort II birth mother = 6.6% birth father = 9.6%) and multi-ethnic (Cohort I birth mother = 5.0%; birth father = 4.8%; Cohort II birth mother = 4.6% birth father = 4.8%), with the remaining sample reported as ‘other’ (see Leve et al., 2019 for further details). Birth parents typically had high school education (Cohort I birth mother = 41.7%, birth father = 41.5%; Cohort II birth mother = 40.2%, birth father = 49.3%), and a median household income of less than $25,000 (Cohort I = <$15,000; Cohort II = $15,000-$25,000). Adoptive parents within both cohorts were typically college educated, middle to upper class families. At the birth of the child, adoptive parents age in Cohort I was 38.1 years (parent 1 M = 37.8, SD = 5.5; parent 2 M = 38.4, SD = 5.6), and in Cohort II was 37.5 years (parent 1 M = 36.8, SD = 5.7; parent 2 M = 38.1, SD = 5.9). The majority of adoptive parents reported their ethnicity as Caucasian (Cohort I = 90.8%; Cohort II = 91.6%). Cohort differences were examined across demographics (see Leve et al., 2019), with negligible differences identified. Data in the current study were collected by home visit assessments, telephone interviews, and online questionnaires. Further details about the study design and sample description have been previously described (Leve et al., 2019).
Measures
An index of birth mother ADHD symptoms.
In Cohorts I and II, birth mother ADHD symptoms were assessed using both the Adult Temperament Questionnaire (ATQ) at 18 months postpartum (Rothbart, Ahadi, & Evans, 2000) and the Barkley’s Adult ADHD scale at age 4.5 years postpartum (Murphy & Adler, 2004). The 5-item attention control subscale of the ATQ was used. Birth mothers reported on a 7-point scale ranging from ‘extremely untrue’ to ‘extremely true’ with higher scores indicating more symptoms of attentional control issues. The internal consistency estimate for the ATQ was good (Cohort I α = .75; Cohort II α = .74). Barkley’s Adult ADHD scale assessed impulsive, hyperactive, and inattentive behavior during the past 12 months. Mothers reported on a 4-point scale ranging from ‘never’ to ‘very often’, with higher scores indicating greater hyperactive or inattentive behavior. Internal consistency estimates were good (Cohort I α = .90; Cohort II α = .88). The attention control subscale of the ATQ and the Barkley’s Adult ADHD scale were found to be moderately correlated (Cohort I r = .48; Cohort II r = .43). The scales were standardized and summed into a single measure of mother ADHD symptoms (see Harold et al., 2013 for further details of the measure). Internal consistency for the combined measure was good (Cohort I α = .88; Cohort II α = .80).
Adoptive mother depressive symptoms.
In Cohort I, adoptive mother depressive symptoms were assessed using Beck Depression Inventory (Beck et al., 1979) at child age 4.5 years (α = .71). Depressive symptoms were calculated as the sum of 20 of the 21 items (suicidal ideation item not administered to minimize situations where clinical follow-up would be needed). In Cohort II, adoptive mother depressive symptoms were assessed using the Center for Epidemiologic Studies Depression Scale (CES-D) at age 4.5 years (Radloff, 1977). Depressive symptoms were calculated as the sum of 20 items (α = .86). Adoptive mother depressive symptoms were standardized within cohort prior to analyses to allow comparisons across Cohorts I and II.
Adoptive mother-to-child hostility.
In Cohorts I and II, hostility towards the child was assessed using adoptive mothers’ self-reports of the Iowa Family Interaction Rating Scales (Melby et al., 1993) at child age 4.5 years. Adoptive mothers reported on their own hostile behaviors towards their child on a 5-item, 7-point scale ranging from ‘never’ to ‘always’, with higher scores indicative of higher hostility (Cohort I α = .78; Cohort II α = .75).
Child impulsivity/activation.
In Cohort I, child impulsivity/activation was assessed using the adoptive mother report of the Children’s Behavior Questionnaire, CBQ (Rothbart et al., 2001) and adoptive mother reports of the Behavioral Inhibition Scale/Behavioral Activation Scale, BAS (Blair et al., 2004) at age 4.5 years, as used in Harold et al., 2013 (see Harold et al., 2013 for further details of this measure). The CBQ included a 13-item impulsivity subscale where mothers reported on a range of child reactions in various scenarios over the past six months on a 7-point scale ranging from ‘extremely untrue’ to ‘extremely true.’ Internal consistency estimates were good (α = .78). Mothers also reported on three subscales of the BAS to assess child drive, reward responsiveness, and fun seeking. Responses to items are on a 7-point scale ranging from ‘extremely untrue’ to ‘extremely true.’ Internal consistency estimates for the three scales were good (drive α = .81, reward responsiveness α = .71, fun seeking α = .70). The CBQ impulsivity subscale was significantly correlate with the three BAS subscales (r = .29–.66). The scales were standardized and summed into a single measure representing child impulsivity and activation (see Harold et al., 2013) which had good internal consistency (α = .87). To assess impulsivity/activation in Cohort II the BAS was also used in conjunction with the CBQ-Short Form (Putnam & Rothbart, 2006), administered at age 4.5 years. Impulsivity items were selected from the short version of the CBQ (internal consistency estimates were good, α = .68). Mothers also reported on three subscales of the BAS (drive α = .73, reward responsiveness α = .61, fun seeking α = .72). The CBQ impulsivity subscale was significantly correlated with the three BAS subscales (r = .26 −.48). The scales were standardized and summed into a single measure representing child impulsivity/activation.
Child ADHD symptoms.
In Cohorts I and II, child ADHD symptoms were assessed using adoptive father reports on the Conner’s Abbreviated Parent Questionnaire (Conners, 1973) and items from the Revised DuPaul Child ADHD Rating Scale (DuPaul 1991; Thapar et al., 2000) at child age 6 years. Father’s reported on a 4-point scale ranging from ‘not at all’ to ‘very much’. Higher scores indicated greater hyperactivity and inattentiveness (Cohort I α = .89; Cohort II α = .90).
Child aggression was measured at age 6 years using adoptive father reports on the aggression subscale of the Child Behavior Checklist, using a 3-point scale ranging from ‘not true to ‘very true’ (Achenbach & Rescorla, 2001). Cohort I used the version for children aged 1 ½ year to 5 years, and Cohort II used the version for children aged 6-18 years. Higher scores indicated greater levels of aggression (Cohort I α = .93; Cohort II α = .89). In each cohort, scores were converted into age-standardized T-scores (M = 50; SD = 10) to allow comparability across cohorts.
Covariates:
To control for any similarities between birth and adoptive families resulting from adoption openness (e.g., contact and contact between adoptive and birth families, and birth parent knowledge of adoptive families), we included the level of openness in the adoption at 9 months as a covariate (Ge et al., 2008). We also controlled for perinatal complications to attempt to disentangle genetic influences from prenatal environment (Marceau et al., 2016).
Analytic Approach
Path analysis examined the role of biological mother ADHD symptoms as a predictor of adopted children’s early impulsivity/activation and associations with adoptive mother hostility and depression symptoms, thereby allowing examination of evocative rGE processes in a genetically sensitive design where passive rGE has been removed. Maternal hostility and depressive symptoms were in turn hypothesized to predict children’s ADHD symptom course and aggression (see Figure 1). Analyses were conducted using Cohort I. Cross-validation analyses were conducted with Cohort II. Multi-group (by cohort) structural equation modelling (SEM) then examined whether specific pathways differed in magnitude between Cohort I and Cohort II by constraining specific pathways to be equal (e.g., constraining paths from birth mother ADHD symptoms to child impulsivity/activation to be equal between Cohorts I and II) and examining the change in model fit (Δ χ2).
A number of variables were transformed to correct for moderate but significant skew. Model fit was examined using chi-square test, Root Mean Square Error of Approximation (RMSEA), Confirmatory Fit Index (CFI) and Standardized Root Mean Square Residual (SRMR). Good model fit was indicated by a non-significant χ2 statistic, an RMSEA fit statistic of ≤.05, CFI ≥.98, and an SRMR close to zero (Kline, 2005).
In Cohort I, of the eligible sample, missing data ranged from 17.4% (59/340) for maternal reports of depressive symptoms, to 31% (107/340) for father reports of child aggression at age 6 years. In Cohort II, of the eligible sample, missing data ranged from 16% (29/178) for birth mother symptoms of ADHD to 45% (81/178) for father reports of child aggression at age 6 years. The Little’s test of missing data indicated that data were not missing completely at random in Cohort I (Little’s MCAR test (87) = 119.04, p = .013) or Cohort II (Little’s MCAR test (36) = 54.25, p = .026). Higher levels of maternal hostility and greater maternal depressive symptoms were associated with missingness at child age 6 years. Under assumptions of Missing at Random (MAR), multiple imputation reduces bias even when the proportion of missing data is large (Madley-Dowd, Hughes, Tilling, & Heron, 2019). We therefore conducted multiple imputation utilizing additional auxiliary variables (e.g., earlier indicators of: maternal depressive symptoms; maternal hostility; father reports of child aggression and ADHD symptoms) to make the assumption of MAR as plausible as possible (White et al., 2011).
To account for attrition, missing data were imputed using multivariate chained equations (Van Buuren & Oudshoom, 2000). Imputation models were run using linear regression. All variables with missing data used in analyses were imputed up to the maximum sample size (Cohort I n = 340; Cohort II n = 178). Twenty imputed datasets were derived each with 10 cycles of regression switching and then all analyses were conducted on the imputed datasets (White et al., 2011). Analyses were conducted using MPlus (Muthén & Muthén, 1998), using maximum likelihood estimation procedures. Indirect effects were estimated with bias corrected bootstrapping (using the MODEL INDIRECT command in MPlus). Indirect effects were considered significant if the 95% confidence intervals did not include zero (Hayes, 2009; Preacher & Hayes, 2008). Bias-corrected bootstrapping is a robust way of testing indirect effects (see MacKinnon et al., 2004). All analyses presented show the results using the imputed sample. Complete case analyses were also conducted.
Results
Correlations, means, and standard deviations are presented in Table 1, which shows similar patterns of associations observed in Cohorts I and II. Figure 2 shows the results for the full model estimated, examining the role of birth mother ADHD symptoms, child impulsivity/activation, adoptive mother hostility and depressive symptoms on later child ADHD symptoms and aggression, with estimates and 95% confidence intervals shown in Table 2.
Table I:
Correlations, means, and standard deviations among constructs for Cohort I (lower diagonal) and Cohort II (upper diagonal)
| 1 | 2 | 3 | 4 | 5 | 6 | Mean (SD) | |
|---|---|---|---|---|---|---|---|
| 1. BM ADHD symptoms a | _ | .12 | −.15 | .11 | .19* | .23* | −.13 (1.72) |
| 2. AC impulsivity/ activation a | .18* | _ | .21** | .20** | .37** | .27** | −.12 (2.92) |
| 3. AM hostility | −.04 | .24** | - | .21* | .29* | .25** | 10.15 (3.21) |
| 4. AM depressive symptoms a | −.16 | −.01 | .14* | - | .18* | .13 | 0.00 (1.00) |
| 5. AC ADHD symptoms | −.02 | .28** | .33** | .01 | - | .63** | 10.27 (5.63) |
| 6. AC aggression b | −.04 | .23* | .44** | −.01 | .66** | - | 54.73 (5.66) |
| Mean (SD) | 0.15 (1.75) | .01 (3.08) | 11.03 (3.09) | 0.00 (1.00) | 8.19 (5.50) | 52.28 (5.36) | - |
Cohort I is shown on the lower diagonal and Cohort II is shown on the upper diagonal. BM: Birth Mother; AC: Adopted Child; AM: Adoptive mothers.
p < .05
p <.01.
Standardized scores
t-scores
Figure 2:
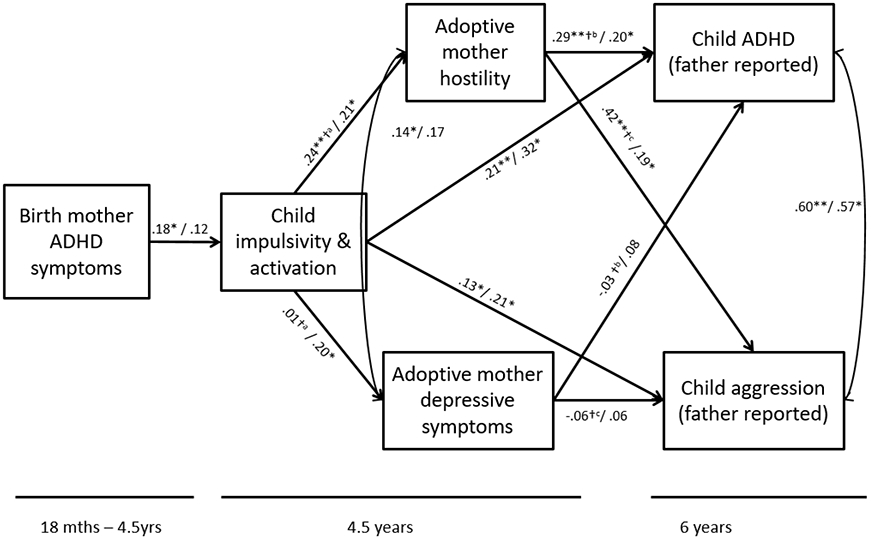
Model examining the relationship between birth mother ADHD symptoms, child impulsivity/activation, adoptive mother depressive symptoms and hostility, child ADHD symptoms and child aggression.
Cohort I before the slash, followed by results from Cohort II. *p < .05; † significant difference between pathways
Table II:
Results from path analyses with 95% confidence intervals for Cohort I and Cohort II
| Path label (figure 1) |
Paths in model | Cohort I (n = 340) |
Cohort II (n = 178) |
||
|---|---|---|---|---|---|
| β | 95% CIs | β | 95% CIs | ||
| a | AM hostility to child ADHD symptoms | .29** | .16, .42 | .20* | .04, .36 |
| b | AM hostility to child aggression | .42** | .26, .58 | .19* | .03, .45 |
| c | AM depressive symptoms to child aggression | −.06 | −.19, .07 | .06 | −.17, .29 |
| d | AM depressive symptoms to child ADHD symptoms | −.03 | −.15, .09 | .08 | −.26, .26 |
| e | BM ADHD symptoms to child impulsivity/activation | .18* | .05, .31 | .12 | −.05, .29 |
| f | Child impulsivity/activation to child ADHD symptoms | .21** | .08, .34 | .32** | .13, .51 |
| g | Child impulsivity/activation to child aggression | .13* | .02, .25 | .21* | .05, .36 |
| h | Child impulsivity/activation to AM hostility | .24** | .12, .36 | .21* | .05, .37 |
| i | Child impulsivity/activation to AM depressive symptoms | .01 | −.11, .13 | .20* | .03, .38 |
| j | AM hostility with AM depressive symptoms | .14* | .03, .25 | .17* | .02, .35 |
| k | Child ADHD symptom with child aggression | .60** | .52, .68 | .57** | .43, .71 |
p < .05
p <.01. BM: Birth mother; AM: Adoptive mother
Model fit indices indicated a satisfactory fit to the data in Cohort I (χ2 (4) = 6.34, p = .175; RMSEA = .04 (.00, .09); CFI = 0.99; SRMR = .043). In Cohort I, Adoptive mother depressive symptoms and adoptive mother hostility at 4.5 years were correlated (r = .14, p = .024). Maternal hostility at age 4.5 years predicted both child aggression (β = .42, p = <.001) and child ADHD symptoms (β = .29, p = <.001) at age 6 years. In contrast, maternal depressive symptoms at 4.5 years were not associated with either child aggression or ADHD symptoms at 6 years (β = −.06, p = .390; β = −.03, p = .593 respectively). Constraining the paths between maternal depressive symptoms and maternal hostility on child outcomes to be equal suggested that maternal depressive symptoms may be less important for the developmental course of aggression (Δ df = 1; Δ χ2 = 5.56), relative to maternal hostility. However, paths did not significantly differ for ADHD symptoms (Δ df = 1; Δ χ2 = 2.96). Early child impulsivity/activation at 4.5 years was associated with child ADHD symptoms at 6 years after partialing out the effects of child aggression (β = .21, p = .002), and was also associated with child aggression at 6 years after partialing out the effects of child ADHD symptoms (β = .13, p = .040). Child ADHD symptoms and aggression at 6 years were also correlated (r = .60, p <.001).
Birth mother ADHD symptoms significantly predicted child impulsivity/activation at 4.5 years (β = .18, p = .010). Furthermore, birth mother ADHD symptoms had an indirect effect on maternal hostility via child impulsivity/activation, suggesting evocative rGE (indirect effect: β = .05, 95% CI .02, .08, p = .046; as identified in Harold et al., 2013), but there was no evidence of an indirect effect on adoptive mother depressive symptoms via child ADHD impulsivity/activation (indirect effect: β = .003, 95% CI −.022, .028, p = .834).
Cross-validation analyses examined this path model in Cohort II (Figure 2). Model fit statistics suggested an adequate fit to the data (χ2 (4) = 8.78, p =.067; RMSEA = .08 (.00, .16); CFI = .94; SRMR = .064). The pattern of results was similar to results for Cohort I, with the exception that the path from birth mother ADHD symptoms to early child ADHD impulsivity/activation (at 4.5 years) was marginally significant (β = .12, p = .072). In addition, the path from child ADHD impulsivity/activation to maternal depressive symptoms was significant (β = .20, p = .033).
Prior to multi-group SEM procedures, we examined whether measures that differed between the cohorts were invariant by constraining the variance to be equal between the two groups. These measures were found to be invariant across Cohorts I and II (Δ df = 3; Δ χ2 = 0.76). Multi-group (by cohort) SEM procedures then examined whether specific pathways differed in magnitude between Cohorts I and II by constraining paths to be equal across the two cohorts. This did not result in a significantly worse model fit, suggesting that paths did not significantly differ in magnitude across the two cohorts (path from birth mother ADHD to child impulsivity/activation: Δ df = 1; Δ χ2 = 0.17; path from child impulsivity/activation to maternal depressive symptoms: Δ df = 1; Δ χ2 = 1.16; path from child impulsivity/activation at age 4.5 years to child aggression at age 6 years Δ df = 1; Δ χ2 = 0.33).
Complete Case Analyses
Although the pattern of results was similar, there were some differences noted in the complete case analysis (see supplementary material, S1). In Cohort I, the association between child ADHD impulsivity/activation and later aggression was reduced to non-significant (β = .11, p = .184). The association between adoptive mother hostility and child ADHD symptoms was no longer significant (β = .13, p = .113). In addition, the correlation between adoptive mother hostility and depressive symptoms was no longer significant (β = .11, p =.100). In Cohort II, the association between child ADHD impulsivity/activation and later aggression was reduced to non-significant (β = .17, p = .125). These results should be interpreted with caution given that the data were not MCAR, and both higher levels of hostility and depressive symptoms were associated with missingness, suggesting that associations with these variables may be underestimated. Furthermore, complete case analyses substantially reduced sample size, which will have reduced the ability to detect significant effects.
Discussion
The aim of the present study was to examine the interplay between genetic and rearing environmental processes (specifically maternal hostility and depressive symptoms) involved in the developmental course of ADHD symptoms and aggression, thus the effects of aggression were partialled out of the estimate of maternal hostility and depressive symptoms on later child ADHD symptoms, and vice versa. As part of the study design, adoptive parents and children were genetically unrelated, allowing the examination of these associations removing the possible confound of passive rGE. Furthermore, this study allowed the examination of evocative rGE of maternal hostility or depressive symptoms, whereby genetic risk for ADHD and aggression (indexed by biological mother ADHD symptoms) may evoke particular responses (maternal hostility or depressive symptoms). Finally, by examining these questions in Cohorts I and II separately, we were able validate the findings across cohorts that utilized slightly different measures to assess the same constructs, thus providing greater confidence in the findings.
Consistent with our first hypothesis, the current study indicated that maternal hostility was associated with both aggression and ADHD symptom course (after taking into account co-occurring symptoms) in both cohorts. As adoptive mothers and adopted children were genetically unrelated to each other, the association between maternal hostility and later child behavior problems cannot be attributed to passive rGE. This suggests that hostile parenting represents an important rearing environmental factor in the developmental course of ADHD symptoms and aggression. Further, this pattern of findings was identified using a cross-rater approach (father ratings of child ADHD and aggression), strengthening the rigor of the analytic approach. Such findings are in accord with a growing body of literature highlighting the role of parent hostility as an important environmental process, for the development of aggression and ADHD developmental course (Burt et al., 2005; Caspi et al., 2004; Harold et al., 2013; Lifford, et al., 2008; Shaw, et al., 2005).
Findings demonstrated that maternal depressive symptoms may be less important for the developmental course of aggression, relative to maternal hostility, with associations being significantly stronger between maternal hostility and child outcomes than between maternal depressive symptoms and child outcomes in Cohort I. However, it is important to note that maternal depressive symptoms were associated with concurrent measures of hostility in each cohort. This is consistent with previous research examining family processes and parental depression, where parent depression has been found to be associated with impairments in family functioning, including parent hostility (Goodman & Gotlib, 1999; Keenan-Miller et al., 2010; Lovejoy, et al., 2000). Therefore, maternal depressive symptoms may influence risk for child behavior problems indirectly via parenting processes. Consistent with this possibility, parents with high levels of depressive symptoms are more likely to display hostile parenting, which in turn increases risk for child psychopathology (Buehler & Gerard, 2002; Cummings et al., 2005; Giallo et al., 2014). Additional research is needed to understand the mechanisms through which maternal depressive symptoms may impact the development and continuity of child ADHD symptoms and aggression.
Consistent with our second hypothesis, findings also suggested that genetically influenced (indexed by birth mother symptoms of ADHD) attributes in the child (liability to ADHD) had a direct effect on later behavior problems, being associated with ADHD symptoms after partialing out the effect of aggression. Early child impulsivity/activation was also associated with later child aggression after partialing out the effect of ADHD symptoms, suggesting that this measure of early child liability to ADHD may not be specific to risk for later ADHD symptoms, but may be associated with risk for multiple child outcomes. This is in accord with previous research suggesting that comorbidity between ADHD and aggression may result, at least in part, from heritable mechanisms (Seroczynski et al., 1999; Nadder et al., 1998; Nadder et al., 2002; Thapar, et al., 2001). Furthermore, the current findings are in accord with previous research suggesting that early impulsivity may predispose children to behavioral difficulties (Beauchaine et al., 2010; García-Forero et al., 2009; Bezdjian et al., 2011; Perry et al., 2018). We extended previous research by considering earlier child characteristics and in the context of co-occurring symptomatology of ADHD symptoms and aggression).
The current study additionally considered evocative rGE in our third hypothesis, furthering the understanding of possible child effects of early child characteristics (specifically impulsivity/activation) on parental hostility (Harold et al.., 2013; Schermerhorn et al., 2012) and parent depressive symptoms (Bagner et al., 2013; Gross et al., 2008; Kouros & Garber, 2010; Raposa et al., 2011). In Cohort I, birth mother ADHD symptoms had an indirect effect on adoptive mother hostility via child impulsivity/activation to later ADHD, as found in a previous study employing this dataset (Harold et al., 2013), providing evidence of evocative rGE. The magnitude of the association was similar across the two cohorts. Whilst the association between birth mother ADHD symptoms and child impulsivity/activation was not significant in Cohort II, the sample size of Cohort II is smaller than Cohort I, which may have reduced power to detect such effects. Overall, the pattern of findings suggests that genetically-influenced behaviors in children can impact family functioning, specifically maternal hostility (Harold et al., 2013).
The association between early child impulsivity/activation and maternal depressive symptoms was inconsistent across Cohorts I and II. There was no evidence of such evocative effects on maternal depressive symptoms in Cohort I. However, there was a significant association between early child impulsivity/activation and maternal depressive symptoms in Cohort II. It is important to consider that different measures were used to assess maternal depressive symptoms in the two cohorts: these were standardized within cohort to allow comparisons across cohorts. Cohort I employed the BDI (Beck et al., 1979), whereas Cohort II employed the CES-D (Radloff, 1977). The BDI and the CES-D represent two of the most widely used assessments of depression (Shafer, 2006). However, although both assess the severity of depressive symptoms, these two questionnaires were initially designed to assess depression in different populations: The BDI originated from the clinical domain to assess depression severity in individuals who already had a diagnosis of depression, whereas the CES-D was developed to assess depression symptom severity within epidemiological samples (Choi et al., 2014; Santor et al., 1995). As such, the BDI retains a focus on cognitive symptoms, whereas the CES-D focuses on affective symptoms (Choi et al., 2014; Santor et al., 1995; Shafer, 2006; Skorikov & VanderVoort, 2003). Differences in associations between child impulsivity/activation and maternal depressive symptoms in the two cohorts may reflect these differences in measurement. This highlights the importance of cross-validation research to allow convergence (or not) of findings that employ different measures to assess the same construct (in this case, depressive symptoms). It is possible that child liability to ADHD may have a greater impact on maternal affective symptoms rather than cognitive symptoms. It is too early to conclude that early child liability to ADHD does not impact maternal depressive symptoms, given association between these constructs in Cohort II (using the CES-D). However, further research is needed to understand these associations.
Limitations and Future Directions
The current findings should be considered in light of some limitations. First, different measures were used for some constructs in Cohort I and II. For example, Cohort II used a modified version of the CBQ – the CBQ Short form (in conjunction with the BAS) compared to Cohort I to assess child impulsivity/activation. Cohorts I and II also used different versions of the CBCL to assess aggression (Cohort I used the version for children aged 1 ½ year to 5 years, and Cohort II used the version for children aged 6-18 years). As noted above, different measures of maternal depressive symptoms were also used. Despite these measurement differences, measures were found to be statistically invariant and findings were broadly similar across the two cohorts. Furthermore, pathways did not significantly differ in magnitude across the two cohorts suggesting that caution is needed in interpreting non-significant paths, particularly in Cohort II, where sample size is smaller than in Cohort I. This cross-cohort validation thus adds confidence to the interpretation of the findings.
Second, there were some differences in complete case analyses (see supplementary material) and imputed data. However, caution is needed when interpreting complete case analyses, particularly given that the data were shown to not be MCAR, and both higher levels of maternal hostility and maternal depressive symptoms were associated with missingness, therefore complete case analysis may produce biased estimates, making multiple imputation more appropriate (Graham, 2009). Furthermore, small sample sizes reduce power to detect associations in complete case analyses. Multiple imputation was used to overcome this limitation. We conducted multiple imputation utilizing auxiliary variables to make the assumption of MAR more plausible (White et al., 2011). Under this assumption, multiple imputation produces less biased estimates compared to complete cases analyses, even when proportion of missing data is large (greater than 50%; Madley-Dowd et al., 2019). A third limitation is that early child impulsivity/activation was measured at the same time as adoptive mother hostility and depressive symptoms. Future research should examine potential bidirectional effects between early child liability to ADHD and parent characteristics.
Fourth, the current analyses did not examine the role of adoptive father hostility or depressive symptoms. Research suggests that both hostility and depression in fathers have detrimental effects on child psychopathology (Connell & Goodman, 2002; Kane & Garber, 2004, 2009; Wilson & Durbin, 2010; Pemberton et al., 2010; Sellers et al., 2019) and that effects may by differ by parent gender (Cummings et al., 2005; Harold et al., 2013; Sturge-Apple et al., 2004). Future research should examine these effects on child psychopathology (in contexts where passive rGE have been controlled for), as well as examine any possible evocative rGE effects on paternal psychopathology and parenting processes. Fifth, it is important to consider that although the association between birth parent and adopted child impulsivity/activation was a measure of heritable risk, prenatal factors may also contribute to this association. We controlled for perinatal complications, but alternative research designs (e.g., children born via assisted conception: Rice et al., 2009) are needed to disentangle genetic influences from prenatal environments. Such studies evidence that prenatal factors such as smoking in pregnancy are explained by genetic factors rather than prenatal environmental risk (Langley et al., 2012; Thapar et al., 2009), but further research is needed to examine additional prenatal environmental factors.
Sixth, it is likely that we did not fully capture ADHD genetic liability with the index of biological mother ADHD alone: birth father ADHD symptoms were not included due to limited data available from birth fathers, which may have underestimated (or overestimated) the magnitude of the association between birth parent ADHD symptoms and child impulsivity/activation. In addition, ADHD can desist by adult life, and recent research suggests that the late emergence of ADHD might represent a different type of phenotype (Cooper et al., 2018; Asherson & Agnew-Blais, 2019). Also, there is recent evidence showing strong genetic overlap between different types of mental health problems with ADHD showing especially strong genetic correlation with depression (Thapar et al., 2013). Thus it is likely that genetic liability to ADHD needs to be indexed by multiple measures of mental health difficulties in the biological parent, as well as genetic risk scores in the future. We conducted exploratory analyses to examine this issue by employing a broader measure of birth mother psychopathology (encompassing depressive and anxiety symptoms, in addition to symptoms of ADHD and delinquency). This broader measure of birth mother psychopathology was associated with neither early child impulsivity at age 4.5 years nor with child symptoms of ADHD or aggression at age 6 years (results available on request), suggesting some specificity relative to measures available in the current study.
Seventh, the majority of measures were derived from parent report. However, we used a cross-rater approach whereby mothers reported on their hostility towards the child, and depressive symptoms, and fathers reported on child ADHD symptoms and aggression, reducing the likelihood that the associations were due to shared rater bias. It is important to consider that although mother and father agreement is often high, mothers tend to report more behavior problems than fathers (Duhig et al, 2000; Sollie et al., 2013; Mayfield et al., 2018; Caye et al., 2017; van der Veen-Mulders et al., 2017). This suggests that the father-reported estimates of child ADHD and aggression in the current study are likely to be conservative. Supplementary analyses therefore examined the validity of father reports of child symptomatology. We examined: (i) the association between mother and father reports of child symptoms; (ii) the full model employing multiple reporters (mother and father reports) of child ADHD symptoms and aggression using a latent variable approach and; (iii) whether father reports of symptomatology predicted subsequent diagnoses (of ADHD and conduct disorder at age 7 year). Findings suggested moderate levels of agreement between mothers and fathers (see Supplementary material S2), in accord with previous studies (Duhin et al., 2000). Father reports of symptomatology were also associated with later diagnoses of ADHD and conduct disorder (see Supplementary material S2). This is in line with previous studies suggesting that father reports of child ADHD symptoms may be equally valid as mother reports (Martell et al., 2015). Further research is needed to better understand rater disagreement and associations with child outcomes.
Finally, the current study focused on child outcomes at the age of 6 years. It is important to note that the associations between parenting processes may be different at later stages in development. Research employing biologically related parents and children suggest that hostility and conflict in the mother-child relationship continues to be associated with child ADHD symptoms later in child development (Garcia et al., 2019; Giannotta & Rydell, 2017; Choenni et al., 2019). However, more research needed in genetically informative designs examining associations between family-level variables and child ADHD symptoms course across development.
Conclusions
This study provides novel insights into the genetic and environmental underpinnings of ADHD developmental course and aggression. We found genetic liability influences early child temperamental attributes of impulsivity/activation that showed continuity with later ADHD and aggression. Early child impulsivity/activation evoked maternal hostility that contributed to both ADHD and aggression (after mutually adjusting for co-occurring symtpoms), with some evidence for evocative processes on adoptive mother depressive symptoms (Cohort II only). Interventions focusing on parent-child relationship could help modify the course of ADHD.
Supplementary Material
Acknowledgements
This project was supported by grants R01 HD042608 from the National Institute of Child Health and Human Development and the National Institute on Drug Abuse, NIH, U.S. PHS (PI Years 1–5: Reiss; PI Years 6–10: Leve); R01 DA020585 from the National Institute on Drug Abuse, the National Institute of Mental Health and OBSSR, NIH, U.S. PHS (PI: Neiderhiser); UG3/UH3 OD023389 from the Office of the Director, NIH, U.S. PHS (PIs: Leve, Neiderhiser, Ganiban); and R01 MH092118 from the National Institute of Mental Health (PIs: Neiderhiser, Leve). Sellers and Harold were supported by Economic and Social Research Council project grant awards (ES/N003098/1 and ES/L014718/1 respectively). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Eunice Kennedy Shriver National Institute of Child Health and Human Development or the National Institutes of Health.
Footnotes
Ethical Approvals
Ethics approval for this study was granted by was granted by the University of Oregon Institutional Review Board (protocol number: 04262013.036).
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- Achenbach TM, & Rescorla LA (2001). Manual for Aseba School-Age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families. [Google Scholar]
- Allen JP, Manning N, & Meyer J (2010). Tightly Linked Systems: Reciprocal relations between maternal depressive symptoms and maternal reports of adolescent externalizing behavior. Journal of Abnormal Psychology, 119(4), 825 – 835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). American Psychiatric Pub. [Google Scholar]
- Angold A, Costello E, & Erkanli A (1999). Comorbidity. Journal of Child Psychology and Psychiatry and Allied Disciplines, 40(1), 57 – 87. [PubMed] [Google Scholar]
- Asherson P, & Agnew-Blais J (2019). Annual Research Review: Does Late-onset Attention-Deficit/Hyperactivity Disorder Exist?. Journal of Child Psychology and Psychiatry, 60(4), 333–352. [DOI] [PubMed] [Google Scholar]
- Bagner DM, Pettit JW, Lewinsohn P, Seeley J, & Jaccard J (2013). Disentangling the Temporal Relationship between Parental Depressive Symptoms and Early Child Behavior Problems: A transactional framework. Journal of Clinical Child and Adolescent Psychology, 42(1), 78 – 90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barkley RA, Fischer M, Edelbrock C, & Smallish L (1991). The Adolescent Outcome of Hyperactive Children Diagnosed by Research Criteria-III. Mother–Child Interactions, Family Conflicts and Maternal Psychopathology. Journal of Child Psychology and Psychiatry, 32, 233 – 255. [DOI] [PubMed] [Google Scholar]
- Bartels M, Hendriks A, Mauri M, Krapohl E, Whipp A, Bolhuis K, … & Roetman P (2018). Childhood Aggression and the Co-occurrence of Behavioural and Emotional Problems: Results across ages 3–16 years from multiple raters in six cohorts in the EU-ACTION Project. European child & adolescent psychiatry, 27(9), 1105–1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, & Emery G (1979). Cognitive Therapy of Depression. New York: Guilford Press. [Google Scholar]
- Beauchaine TP, Hinshaw SP, & Pang KL (2010). Comorbidity of Attention-Deficit/Hyperactivity Disorder and Early-onset Conduct Disorder: Biological, environmental, and developmental mechanisms. Clinical Psychology: Science and Practice, 17(4), 327–336. [Google Scholar]
- Bezdjian S, Baker LA, & Tuvblad C (2011). Genetic and Environmental Influences on Impulsivity: A meta-analysis of twin, family and adoption studies. Clinical psychology review, 31(7), 1209–1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Mick E, Spencer T, Wilens T, Kiely K, Guite J, Ablon JS, Reed E, & Warburton R (1995). High Risk for Attention Deficit Hyperactivity Disorder among Children of Parents with Childhood Onset of the Disorder: A pilot study. American Journal of Psychiatry, 152(3), 431 – 435. [DOI] [PubMed] [Google Scholar]
- Biederman J, Newcorn J, & Sprich S (1996). Comorbidity of Attention Deficit Hyperactivity Disorder with Conduct, Depressive, Anxiety, and Other Disorders. American Journal of Psychiatry, 148(5), 564 – 577. [DOI] [PubMed] [Google Scholar]
- Bjørnebekk G, Kjøbli J, & Ogden T (2015). Children with Conduct Problems and Co-Occurring Adhd: Behavioral improvements following parent management training. Child and Family Behavior Therapy, 37(1), 1 – 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair C, Peters R, & Granger D (2004). Physiological and Neuropsychological Correlates of Approach/Withdrawal Tendencies in Preschool: Further examination of the Behavioral Inhibition System/Behavioral Activation System scales for young children. Developmental Psychobiology, 45, 113 – 124. [DOI] [PubMed] [Google Scholar]
- Brooker RJ, Neiderhiser JM, Leve LD, Shaw DS, Scaramella LV, & Reiss D (2015). Associations between Infant Negative Affect and Parent Anxiety Symptoms are Bidirectional: Evidence from mothers and fathers. Frontiers in Psychology, 6, 1875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buehler C, & Gerard JM (2002). Marital Conflict, Ineffective Parenting, and Children's and Adolescents' Maladjustment. Journal of Marriage and Family, 64(1), 78–92. [Google Scholar]
- Burt SA (2009). Rethinking Environmental Contributions to Child and Adolescent Psychopathology: A meta-analysis of shared environmental influences. Psychological Bulletin, 135(4) [DOI] [PubMed] [Google Scholar]
- Burt SA, Krueger RF, Mcgue M, & Iacono WG (2001). Sources of Covariation Among Attention-deficit/hyperactivity disorder, Oppositional Defiant Disorder, and Conduct Disorder: The importance of shared environment. Journal of Abnormal Psychology, 110(4) [DOI] [PubMed] [Google Scholar]
- Burt SA, McGue M, Krueger RF, & Iacono W (2005). How Are Parent–Child Conflict and Childhood Externalizing Symptoms Related over Time? Results from a genetically informative cross-lagged study. Development and Psychopathology, 17(1), 145 – 165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caron C, & Rutter M (1991). Comorbidity in Child Psychopathology: Concepts, issues and research strategies. Journal of Child Psychology and Psychiatry and Allied Disciplines, 32(7), 1063 – 1080. [DOI] [PubMed] [Google Scholar]
- Caspi A, Moffitt TE, Morgan J, Rutter M, Taylor A, Arseneault L, Tully L, Jacobs C, Kim-Cohen J, & Polo-Tomas M (2004). Maternal Expressed Emotion Predicts Children's Antisocial Behavior Problems: Using monozygotic-twin differences to identify environmental effects on behavioral development. Developmental Psychology, 40(2), 149 – 161. [DOI] [PubMed] [Google Scholar]
- Caye A, Machado JD, & Rohde LA (2017). Evaluating Parental Disagreement in ADHD Diagnosis: Can we rely on a single report from home?. Journal of Attention Disorders, 21(7), 561–566. [DOI] [PubMed] [Google Scholar]
- Cheung K, Aberdeen K, Ward MA, & Theule J (2018). Maternal Depression in Families of Children with ADHD: A meta-analysis. Journal of Child and Family Studies, 27(4), 1015–1028. [Google Scholar]
- Choenni V, Lambregtse-van den Berg MP, Verhulst FC, Tiemeier H, & Kok R (2018). The Longitudinal Relation between Observed Maternal Parenting in the Preschool Period and the Occurrence of Child ADHD Symptoms in Middle Childhood. Journal of Abnormal Child Psychology, 47(5), 755–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi SW, Schalet B, Cook KF, & Cella D (2014). Establishing a Common Metric for Depressive Symptoms: Linking the BDI-II, CES-D, and PHQ-9 to PROMIS Depression. Psychological Assessment, 26(2), 513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conger RD, Patterson GR, & Ge X (1995). It takes two to replicate: A mediational model for the impact of parents' stress on adolescent adjustment. Child Development, 66(1), 80–97. [DOI] [PubMed] [Google Scholar]
- Congdon E, & Canli T (2005). The Endophenotype of Impulsivity: Reaching consilience through behavioral, genetic, and neuroimaging approaches. Behavioral and Cognitive Neuroscience Reviews, 4(4), 262–281 [DOI] [PubMed] [Google Scholar]
- Connell AM, & Goodman SH (2002). The Association between Psychopathology in Fathers versus Mothers and Children's Internalizing and Externalizing Behavior Problems: A meta-analysis. Psychological Bulletin, 128(5), 746. [DOI] [PubMed] [Google Scholar]
- Conners CK (1973) Rating scales for use in drug studies with children. Psychopharmacol Bull [Special issue on children], 24–42. [Google Scholar]
- Cooper M, Hammerton G, Collishaw S, Langley K, Thapar A, Dalsgaard S, … & O'Donovan M (2018). Investigating late-onset ADHD: a population cohort investigation. Journal of Child Psychology and Psychiatry, 59(10), 1105–1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings ME, Kellers PS, Davies PT (2005). Towards a Family Process Model of Maternal and Paternal Depressive Symptoms: Exploring multiple relations with child and family functioning. Journal of Child Psychology and Psychiatry, 46(5), 479–489. [DOI] [PubMed] [Google Scholar]
- Daley D, Van Der Oord S, Ferrin M, Cortese S, Danckaerts M, Doepfner M, … & Banaschewski T (2018). Practitioner Review: Current best practice in the use of parent training and other behavioural interventions in the treatment of children and adolescents with Attention Deficit Hyperactivity Disorder. Journal of Child Psychology and Psychiatry, 59(9), 932–947. [DOI] [PubMed] [Google Scholar]
- Deault LC (2010). A Systematic Review of Parenting in Relation to the Development of Comorbidities and Functional Impairments in Children with Attention-Deficit/Hyperactivity Disorder (ADHD). Child Psychiatry & Human Development, 41(2), 168–192. [DOI] [PubMed] [Google Scholar]
- Demontis D, Walters RK, Martin J, Mattheisen M, Als TD, Agerbo E, … & Cerrato F (2019). Discovery of the First Genome-wide Significant Risk Loci for Attention Deficit/Hyperactivity Disorder. Nature Genetics, 51(1), 63–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duhig AM, Renk K, Epstein MK, & Phares V (2000). Interparental Agreement on Internalizing, Externalizing, and Total Behavior Problems: A meta-analysis. Clinical Psychology: Science and Practice, 7(4), 435–453. [Google Scholar]
- DuPaul GJ (1991). Parent and teacher ratings of ADHD symptoms: psychometric properties in a community-based sample. Journal of Clinical Child and Adolescent Psychology, 20(3), 245–253. [Google Scholar]
- Elam KK, Harold GT, Neiderhiser JM, Reiss D, Shaw DS, Natsuaki MN, … & Leve LD (2014). Adoptive Parent Hostility and Children’s Peer Behavior Problems: Examining the role of genetically informed child attributes on adoptive parent behavior. Developmental Psychology, 50(5), 1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eley TC, Lichtenstein P, & Stevenson J (1999). Sex Differences in the Etiology of Aggressive and Nonaggressive Antisocial Behavior: Results from two twin studies. Child Development, 70(1), 155–168. [DOI] [PubMed] [Google Scholar]
- Eley TC, Lichtenstein P, & Moffitt TE (2003). A Longitudinal Behavioral Genetic Analysis of the Etiology of Aggressive and Nonaggressive Antisocial Behavior. Development and Psychopathology, 15(2), 383–402 [DOI] [PubMed] [Google Scholar]
- Elgar FJ, Curtis LJ, McGrath PJ, Waschbusch DA, & Stewart SH (2003). Antecedent-Consequence Conditions in Maternal Mood and Child Adjustment: A four-year cross-lagged study. Journal of Clinical Child and Adolescent Psychology, 32(3), 362–374 [DOI] [PubMed] [Google Scholar]
- Faraone SV, Biederman J, Spencer T, Wilens T, Seidman LJ, Mick E, & Doyle AE (2000). Attention-Deficit/Hyperactivity Disorder in Adults: An Overview. Biological Psychiatry, 48(1), 9 – 20. [DOI] [PubMed] [Google Scholar]
- Foley M, McClowry SG, & Castellanos FX (2008). The Relationship Between Attention Deficit Hyperactivity Disorder and Child Temperament. Journal of Applied Developmental Psychology, 29(2), 157–169. [Google Scholar]
- Frick MA, Forslund T, & Brocki KC (2019). Can Reactivity and Regulation in Infancy Predict Inattentive and Hyperactive/Impulsive Behavior in 3-year-olds?. Development and Psychopathology, 31(2), 619–629. [DOI] [PubMed] [Google Scholar]
- Garcia AM, Medina D, & Sibley MH (2019). Conflict between Parents and Adolescents with ADHD: Situational triggers and the role of comorbidity. Journal of Child and Family Studies, 28(12), 3338–3345. [Google Scholar]
- García-Forero C, Gallardo-Pujol D, Maydeu-Olivares A, & Andrés-Pueyo A (2009). Disentangling Impulsiveness, Aggressiveness and Impulsive Aggression: An empirical approach using self-report measures. Psychiatry Research, 168(1), 40–49 [DOI] [PubMed] [Google Scholar]
- Ge X, Natsuaki MN, Martin DM, Leve LD, Neiderhiser JM, Shaw DS, Villareal G, Scaramella L, Reid JB and Reiss D (2008). Bridging the Divide: Openness in adoption and postadoption psychosocial adjustment among birth and adoptive parents. Journal of Family Psychology, 22(4), 529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelhorn HL, Stallings MC, Young SE, Corley RP, Rhee SH, & Hewitt JK (2005). Genetic and Evironmental Influences on Conduct Disorder: Symptom, domain and full-scale analyses. Journal of Child Psychology and Psychiatry, 46(6), 580–591. [DOI] [PubMed] [Google Scholar]
- Giallo R, Cooklin A, Wade C, D'Esposito F, & Nicholson JM (2014). Maternal Postnatal Mental Health and Later Emotional–Behavioural Development of Children: The mediating role of parenting behaviour. Child: Care, Health and Development, 40(3), 327–336. [DOI] [PubMed] [Google Scholar]
- Giannotta F, & Rydell AM (2017). The Role of the Mother-Child Relationship in the Route from Child ADHD to Adolescent Symptoms of Depressed Mood. Journal of Adolescence, 61, 40–49. [DOI] [PubMed] [Google Scholar]
- Goodman SH, & Gotlib IH (1999). Risk for Psychopathology in the Children of Depressed Mothers: A developmental model for understanding mechanisms of transmission. Psychological Review, 106(3), 458 – 490. [DOI] [PubMed] [Google Scholar]
- Graham JW (2009). Missing Data Analysis: Making it work in the real world. Annual Review of Psychology, 60, 549–576. [DOI] [PubMed] [Google Scholar]
- Gross H, Shaw D, Moilanen K, Dishion T, & Wilson M (2008). Reciprocal Models of Child Behavior and Depressive Symptoms in Mothers and Fathers in a Sample of Children at Risk for Early Conduct Problems. Journal of Family Psychology, 22(5), 742 – 751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harold GT, Leve LD, Barrett D, Elam K, Neiderhiser JM, Natsuaki MN, Shaw DS, Reiss D, & Thapar A (2013). Biological and Rearing Mother Influences on Child Adhd Symptoms: Revisiting the developmental interface between nature and nurture. Journal of Child Psychology and Psychiatry, 54(10), 1038 – 1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2009). Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication monographs, 76(4), 408–420. [Google Scholar]
- Hendriks AM, Bartels M, Colins OF, & Finkenauer C (2018). Childhood Aggression: a synthesis of reviews and meta-analyses to reveal patterns and opportunities for prevention and intervention strategies. Neuroscience & Biobehavioral Reviews, 91, 278–291. [DOI] [PubMed] [Google Scholar]
- Johnston C, & Mash EJ (2001). Families of Children with Attention-Deficit/Hyperactivity Disorder: Review and recommendations for future research. Clinical Child and Family Psychology Review, 4, 183 – 207. [DOI] [PubMed] [Google Scholar]
- Kane P, & Garber J (2004). The Relations among Depression in Fathers, Children's Psychopathology, and Father–Child Conflict: a meta-analysis. Clinical Psychology Review, 24(3), 339–360. [DOI] [PubMed] [Google Scholar]
- Kane P, & Garber J (2009). Parental Depression and Child Externalizing and Internalizing Symptoms: Unique effects of fathers’ symptoms and perceived conflict as a mediator. Journal of Child and Family Studies, 18(4), 465–472. [Google Scholar]
- Keenan-Miller D, Hammen C, & Brennan PA (2010). Mediators of Aggression among Young Adult Offspring of Depressed Mothers. Journal of Abnormal Psychology, 119(4), 836 – 849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klahr AM, Klump KL, & Burt SA (2014). The Etiology of the Association between Child Antisocial Behavior and Maternal Negativity varies across Aggressive and Non-aggressive Rule-breaking forms of Antisocial Behavior. Journal of Abnormal Child Psychology, 42(8), 1299–1311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline R (2005). Principles and Practice of Structural Equation Modelling. New York: Guilford Press. [Google Scholar]
- Kouros CD, & Garber J (2010). Dynamic Associations between Maternal Depressive Symptoms and Adolescents’ Depressive and Externalizing Symptoms. Journal of Abnormal Child Psychology, 38(8), 1069 – 1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lange G, Sheerin D, Carr A, Dooley B, Barton V, Marshall D, Mulligan A, Lawlor M, Belton M, & Doyle M (2005). Family Factors Associated with Attention Deficit Hyperactivity Disorder and Emotional Disorders in Children. Journal of Family Therapy, 27, 76 – 96. [Google Scholar]
- Langley K, Heron J, Smith GD, & Thapar A (2012). Maternal and Paternal Smoking During Pregnancy and Risk of ADHD Symptoms in Offspring: Testing for intrauterine effects. American Journal of Epidemiology, 176(3), 261–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leve LD, Neiderhiser JM, Ganiban JM, Natsuaki MN, Shaw DS, & Reiss D (2019). The Early Growth and Development Study: A dual-family adoption study from birth through adolescence. Twin Research and Human Genetics, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lifford KJ, Harold GT, & Thapar A (2008). Parent–Child Relationships and ADHD Symptoms: A longitudinal analysis. Journal of Abnormal Child Psychology, 36(2), 285 – 296. [DOI] [PubMed] [Google Scholar]
- Lifford KJ, Harold GT, & Thapar A (2009). Parent–Child Hostility and Child ADHD Symptoms: A genetically sensitive and longitudinal analysis. Journal of Child Psychology and Psychiatry, 50(12), 1468–1476. [DOI] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O'Hare E, & Neuman G (2000). Maternal Depression and Parenting Behavior: A meta-analytic review. Clinical Psychology Review, 20(5), 561–592. [DOI] [PubMed] [Google Scholar]
- Lykken DT (1968). Statistical Significance in Psychological Research. Psychological Bulletin, 70(3p1), 151. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, & Williams J (2004). Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate behavioral research, 39(1), 99–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madley-Dowd P, Hughes R, Tilling K, & Heron J (2019). The Proportion of Missing Data should not be used to Guide Decisions on Multiple Imputation. Journal of Clinical Epidemiology, 110, 63–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marceau K, De Araujo-Greecher M, Miller ES, Massey SH, Mayes LC, Ganiban JM, Reiss D, Shaw DS, Leve LD & Neiderhiser JM (2016). The Perinatal Risk Index: Early risks experienced by domestic adoptees in the United States. PloS one, 11(3), e0150486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mars B, Collishaw S, Smith D, Thapar AK, Potter R, Sellers R, Harold GT, Craddock N, Rice F, & Thapar A (2012). Offspring of Parents with Recurrent Depression: Which features of parent depression index risk for offspring psychopathology? Journal of Affective Disorders, 136(1-2), 44 – 53. [DOI] [PubMed] [Google Scholar]
- Martel MM, Nigg JT, & Von Eye A (2009). How do Trait Dimensions Map onto ADHD Symptom Domains?. Journal of Abnormal Child Psychology, 37(3), 337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel MM, Schimmack U, Nikolas M, & Nigg JT (2015). Integration of Symptom Ratings from Multiple Informants in ADHD Diagnosis: A psychometric model with clinical utility. Psychological Assessment, 27(3), 1060 – 1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason DA, & Frick PJ (1994). The Heritability of Antisocial Behavior: A meta-analysis of twin and adoption studies. Journal of Psychopathology and Behavioral Assessment, 16(4), 301–323. [Google Scholar]
- Mayfield AR, Parke EM, Barchard KA, Zenisek RP, Thaler NS, Etcoff LM, & Allen DN (2018). Equivalence of Mother and Father Ratings of ADHD in Children. Child Neuropsychology, 24(2), 166–183. [DOI] [PubMed] [Google Scholar]
- Melby J, Conger R, Book R, Rueter M, Lucy L, Repinski D, Ahrens K, Black D, Huck S, Mutchler L, Rogers S, Ross J, & Stavros T (1993). The Iowa Family Interaction Rating Scale (2nd Edition): Iowa State University Centre for Family Research in Rural Mental health. [Google Scholar]
- Miller NV, Hane AA, Degnan KA, Fox NA, & Chronis-Tuscano A (2019). Investigation of a Developmental Pathway from Infant Anger Reactivity to Childhood Inhibitory Control and ADHD Symptoms: Interactive effects of early maternal caregiving. Journal of Child Psychology and Psychiatry, 60(7), 762–772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy KR, & Adler LA (2004). Assessing Attention-Deficit/Hyperactivity Disorder in Adults: Focus on rating scales. Journal of Clinical Psychiatry, 65(3), 12 – 17. [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998). Mplus User's Guide: The Comprehensive Modeling Program for Applied Researchers. Los Angeles, CA: Muthén and Muthén. [Google Scholar]
- Nadder TS, Rutter M, Silberg JL, Maes HH, & Eaves LJ (2002). Genetic Effects on the Variation and Covariation of Attention Deficit-Hyperactivity Disorder (ADHD) and Oppositional-Defiant Disorder/Conduct Disorder (ODD/CD) Symptomatologies across Informant and Occasion of Measurement. Psychological Medicine, 32(1), 39 – 53. [DOI] [PubMed] [Google Scholar]
- Nadder TS, Silberg JL, Eaves LJ, Maes HH, & Meyer JM (1998). Genetic Effects on ADHD Symptomatology in 7-to 13-year-old twins: Results from a telephone survey. Behavior Genetics, 28(2), 83–99 [DOI] [PubMed] [Google Scholar]
- Natsuaki MN, Shaw DS, Neiderhiser JM, Ganiban JM, Harold GT, Reiss D, & Leve LD (2014). Raised by Depressed Parents: Is it an environmental risk? Clinical Child and Family Psychology Review, 17, 357 – 367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neiderhiser JM, Marceau K, & Reiss D (2013). Four Factors for the Initiation of Substance use by Young Adulthood: A 10-year follow-up twin and sibling study of marital conflict, monitoring, siblings, and peers. Development and Psychopathology, 25(1), 133–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholson JS, Deboeck PR, Farris JR, Boker SM, & Borkowski JG (2011). Maternal Depressive Symptomatology and Child Behavior: Transactional relationship with simultaneous bidirectional coupling. Development and Psychopathology, 47(5), 1312–1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nigg JT (2006). Temperament and Developmental Psychopathology. Journal of Child Psychology and Psychiatry, 47(3-4), 395–422. [DOI] [PubMed] [Google Scholar]
- Nigg JT, Goldsmith HH, & Sachek J (2004). Temperament and Attention Deficit Hyperactivity Disorder: The development of a multiple pathway model. Journal of Clinical Child and Adolescent Psychology, 33(1), 42–53. [DOI] [PubMed] [Google Scholar]
- Nigg JT, & Hinshaw SP (1998). Parent Personality Traits and Psychopathology Associated with Antisocial Behaviors in Childhood Attention-Deficit Hyperactivity Disorder. The Journal of Child Psychology and Psychiatry and Allied Disciplines, 39(2), 145–159. [PubMed] [Google Scholar]
- Nikolas MA, & Burt SA (2010). Genetic and Environmental Influences on ADHD Symptom Dimensions of Inattention and Hyperactivity: A meta-analysis. Journal of Abnormal Psychology, 119(1) [DOI] [PubMed] [Google Scholar]
- O'Connor TG, Deater-Deckard K, Fulker D, Rutter M, & Plomin R (1998). Genotype–Environment Correlations in Late Childhood and Early Adolescence: Antisocial behavioral problems and coercive parenting. Developmental Psychology, 34(5), 970. [DOI] [PubMed] [Google Scholar]
- Patterson GR, DeBaryshe BD, & Ramsey E (1989). A Developmental Perspective on Antisocial Behavior. American Psychologist, 44(2), 329 – 335. [DOI] [PubMed] [Google Scholar]
- Pemberton CK, Neiderhiser JM, Leve LD, Natsuaki MN, Shaw DS, Reiss D, & Ge X (2010). Influence of Parental Depressive Symptoms on Adopted Toddler Behaviors: An emerging developmental cascade of genetic and environmental effects. Development and Psychopathology, 22(4), 803 – 818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peris TS, & Hinshaw SP (2003). Family Dynamics and Preadolescent Girls with ADHD: The relationship between expressed emotion, ADHD symptomatology, and comorbid disruptive behavior. Journal of Child Psychology and Psychiatry, 44(8), 1177–1190. [DOI] [PubMed] [Google Scholar]
- Perry NB, Calkins SD, Dollar JM, Keane SP, & Shanahan L (2018). Self-Regulation as a Predictor of Patterns of Change in Externalizing Behaviors from Infancy to Adolescence. Development and Psychopathology, 30(2), 497–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilowsky D, Wickramaratne P, Nomura Y, & Weissman M (2006). Family Discord, Parental Depression, and Psychopathology in Offspring: 20-Year follow-up. Journal of the American Academy of Child and Adolescent Psychiatry, 45(4), 452 – 460. [DOI] [PubMed] [Google Scholar]
- Plomin R, DeFries JC, & Loehlin JC . (1977). Genotype-Environment Interaction and Correlation in the Analysis of Human Behavior. Psychological Bulletin, 84(2), 309 – 322. [PubMed] [Google Scholar]
- Polanczyk GV, Willcutt EG, Salum GA, Kieling C, & Rohde LA (2014). ADHD Prevalence Estimates across Three Decades: An updated systematic review and meta-regression analysis. International Journal of Epidemiology, 43(2), 434–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior research methods, 40(3), 879–891. [DOI] [PubMed] [Google Scholar]
- Putnam SP & Rothbart MK (2006). Development of Short and Very Short Forms of the Children’s Behavior Questionnaire. Journal of Personality Assessment, Vol. 87(1), pp. 103–113. [DOI] [PubMed] [Google Scholar]
- Radloff LS (1977). The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385 – 401. [Google Scholar]
- Raposa EB, Hammen CL, & Brennan PA (2011). Effects of Child Psychopathology on Maternal Depression: The mediating role of child-related acute and chronic stressors. Journal of Abnormal Child Psychology, 39(8), 1177 – 1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice F, Harold GT, Boivin J, Hay DF, van den Bree M, & Thapar A (2009). Disentangling Prenatal and Inherited Influences in Humans with an Experimental Design. Proceedings of the National Academy of Sciences, 106(7), 2464–2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riggins-Caspers KM, Cadoret RJ, Knutson JF, & Langbehn D (2003). Biology-Environment Interaction and Evocative Biology-Environment Correlation: Contributions of harsh discipline and parental psychopathology to problem adolescent behaviors. Behavior Genetics, 33(3), 205–220. [DOI] [PubMed] [Google Scholar]
- Rothbart MK, Ahadi SA, & Evans DE (2000). Temperament and Personality: Origins and outcomes. Journal of Personality and Social Psychology, 78, 122 – 135. [DOI] [PubMed] [Google Scholar]
- Rothbart MK, Ahadi SA, Hershey KL, & Fisher P (2001). Investigations of Temperament at Three to Seven Years: The Children’s Behavior Questionnaire. Child Development, 72(5), 1394 – 1408. [DOI] [PubMed] [Google Scholar]
- Santor DA, Zuroff DC, Ramsay JO, Cervantes P, & Palacios J (1995). Examining Scale Discriminability in the BDI and CES-D as a Function of Depressive Severity. Psychological Assessment, 7(2), 131. [Google Scholar]
- Scarr S, & McCartney K (1983). How People make their own Environments: A theory of genotype→ environment effects. Child Development, 424–435 [DOI] [PubMed] [Google Scholar]
- Schermerhorn AC, D'Onofrio BM, Sluske WS, Emery RE, Turkheimer E, Harden KP, Heath AC, & Martin NG (2012). Offspring ADHD as a Risk Factor for Parental Marital Problems: Controls for genetic and environmental confounds. Twin Research and Human Genetics, 15(6), 700 – 713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott S, & Gardner F (2015). Parenting programs, in Thapar A, Pine DS, Leckman J, Snowling M, Scott S, Taylor E (Eds). Rutter’s Child and Adolescent Psychiatry (6th Edition), Oxford: John Wiley & Sons, 483–496. [Google Scholar]
- Sellers R, Hammerton G, Harold GT, Mahedy L, Potter R, Langley K, Thapar A, Rice F, Thapar A, & Collishaw S (2016). Examining Whether Offspring Psychopathology Influences Illness Course in Mothers with Recurrent Depression Using a High-Risk Longitudinal Sample. Journal of Abnormal Psychology, 125(2), 256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sellers R, Harold GT, Elam KK, Rhoades KA, Potter R, Mars B, Craddock N, Thapar A, & Collishaw S (2014). Maternal Depression and Co-Occurring Antisocial Behaviour: Testing maternal hostility and warmth as mediators of risk for offspring psychopathology. Journal of Child Psychology and Psychiatry, 55(2), 112 – 120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sellers R, Harold GT, Smith AF, Neiderhiser JM, Reiss D, Shaw D, … & Leve LD (2019). Disentangling nature from nurture in examining the interplay between parent–child relationships, ADHD, and early academic attainment. Psychological Medicine, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sellers R, Harold GT, Smith AF, Neiderhiser JM, Reiss D, Shaw D, … & Leve LD (2019). Disentangling Nature from Nurture in Examining the Interplay Between Parent–Child Relationships, ADHD, and Early Academic Attainment. Psychological Medicine, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seroczynski AD, Bergeman CS, & Coccaro EF (1999). Etiology of the Impulsivity/Aggression Relationship: Genes or Environment?. Psychiatry Research, 86(1), 41–57. [DOI] [PubMed] [Google Scholar]
- Shafer AB (2006). Meta-Analysis of the Factor Structures of Four Depression Questionnaires: Beck, CES-D, Hamilton, and Zung. Journal of Clinical Psychology, 62(1), 123–146. [DOI] [PubMed] [Google Scholar]
- Shaw D, Lacourse E, & Nagin DS (2005). Developmental Trajectories of Conduct Problems and Hyperactivity from Ages 2 to 10. Journal of Child Psychology and Psychiatry, 46(9), 931 – 942. [DOI] [PubMed] [Google Scholar]
- Silberg JL, Maes H, & Eaves LJ (2010). Genetic and Environmental Influences on the Transmission of Parental Depression to Children’s Depression and Conduct Disturbance: an extended children of twins study. Journal of Child Psychology and Psychiatry, 51(6), 734–744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skorikov VB, & VanderVoort DJ (2003). Relationships Between the Underlying Constructs of the Beck Depression Inventory and the Center for Epidemiological Studies Depression Scale. Educational and Psychological Measurement, 63(2), 319–335. [Google Scholar]
- Sollie H, Larsson B, & Mørch WT (2013). Comparison of Mother, Father, and Teacher Reports of ADHD Core Symptoms in a Sample of Child Psychiatric Outpatients. Journal of Attention Disorders, 17(8), 699–710. [DOI] [PubMed] [Google Scholar]
- Stergiakouli E, & Thapar A (2010). Fitting the Pieces Together: Current Research on the Genetic Basis of Attention-Deficit/Hyperactivity Disorder (ADHD). Neuropsychiatric Disease and Treatment, 6, 551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stover CS, Connell CM, Leve LD, Neiderhiser JM, Shaw DS, Scaramella LV, Conger R & Reiss D (2012). Fathering and Mothering in the Family System: Linking marital hostility and aggression in adopted toddlers. Journal of Child Psychology and Psychiatry, 53(4), 401–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sturge-Apple ML, Davies PT, Boker SM, & Cummings EM (2004). Interparental Dscord and Parenting: Testing the moderating roles of child and parent gender. Parenting: Science and Practice, 4(4), 361–380. [Google Scholar]
- Thapar A, Cooper M, Eyre O, & Langley K (2013). Practitioner Review: What have we learnt about the causes of ADHD?. Journal of Child Psychology and Psychiatry, 54(1), 3–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thapar A, Cooper M, Jefferies R, & Stergiakouli E (2012). What Causes Attention Deficit Hyperactivity Disorder? Archives of Disease in Childhood, 97, 260 – 265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thapar A, Harrington R, & McGuffin P (2001). Examining the Comorbidity of ADHD-Related Behaviours and Conduct Problems Using a Twin Study Design. British Journal of Psychiatry, 179, 224 – 229. [DOI] [PubMed] [Google Scholar]
- Thapar A, Harrington R, Ross K, & McGuffin P (2000). Does the definition of ADHD affect heritability?. Journal of the American Academy of Child & Adolescent Psychiatry, 39(12), 1528–1536. [DOI] [PubMed] [Google Scholar]
- Thapar A, Rice F, Hay D, Boivin J, Langley K, van Den Bree M, Rutter M, & Harold G (2009). Prenatal Smoking might not Cause Attention-Deficit/Hyperactivity Disorder: Evidence from a novel design. Biological Psychiatry, 66(8), 722–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Buuren S, & Oudshoom C (2000). Mice: Multivariate Imputation by Chained Equations (S Software for Missing Data Imputation). [Google Scholar]
- van der Veen-Mulders L, Nauta MH, Timmerman ME, van den Hoofdakker BJ, & Hoekstra PJ (2017). Predictors of Discrepancies Between Fathers and Mothers in Rating Behaviors of Preschool Children with and without ADHD. European Child & Adolescent Psychiatry, 26(3), 365–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vierikko E, Pulkkinen L, Kaprio J, Viken R, & Rose RJ (2003). Sex Differences in Genetic and Environmental Effects on Aggression. Aggressive Behavior: Official Journal of the International Society for Research on Aggression, 29(1), 55–68. [Google Scholar]
- Weissman M, Wickramaratne P, Nomura Y, Warner V, Pilowsky D, & Verdeli H (2006). Offspring of Depressed Parents: 20 years later. American Journal of Psychiatry, 163(6), 1001 – 1008. [DOI] [PubMed] [Google Scholar]
- Weisz JR (1978). Transcontextual validity in developmental research. Child Development, 1–12. [Google Scholar]
- White IR, Royston P, & Wood AM (2011). Multiple Imputation Using Chained quations: Issues and guidance for practice. Statistics in Medicine, 30(4), 377 – 399. [DOI] [PubMed] [Google Scholar]
- Willoughby MT, Gottfredson NC, Stifter CA, & Family Life Project Investigators. (2017). Observed Temperament from Ages 6 to 36 Months Predicts Parent-and Teacher-Reported Attention-Deficit/Hyperactivity Disorder Symptoms in First Grade. Development and Psychopathology, 29(1), 107–120 [DOI] [PubMed] [Google Scholar]
- Wilson S, & Durbin CE (2010). Effects of Paternal Depression on Fathers' Parenting Behaviors: A meta-analytic review. Clinical Psychology Review, 30(2), 167–180. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


