Abstract
Peritraumatic emotions are implicated in the elevated health risks associated with interpersonal trauma, but they have not been widely studied in the context of intimate partner abuse (IPA). To address this, community women with divorce histories completed IPA measures, along with an interview to assess posttraumatic stress symptoms and both DSM-IV A2 emotions (yes/no) and other emotions (free response) experienced during worst incidents of IPA. Anxiety/fright, helplessness, and horror were highly prevalent. Lexical analysis of the words women used to describe their other emotions revealed that anger and shame were the most prevalent, followed by dissociation and sadness. As predicted, chronicity of direct assault and frequency of verbal/emotional abuse showed significant, positive correlations with peritraumatic dissociation, and peritraumatic shame showed significant, positive correlations with current symptoms of effortful avoidance. Also, a negative correlation between frequency of dominance/isolation abuse—an indicator of coercive control—and peritraumatic anger approached statistical significance. Although limited by the cross-sectional, retrospective design, results contribute to the understanding of peritraumatic emotions in the context of IPA, and motivate continued efforts to examine their roles in the elevated health risks of interpersonal trauma.
Keywords: intimate partner abuse, peritraumatic emotion, dissociation, shame, posttraumatic stress
The toll of interpersonal trauma has been recognized for some time (Resnick, Kilpatrick, Dansky, Saunders, & Best, 1993), and by now numerous studies have documented the elevated health risks that follow exposure to interpersonal versus impersonal trauma (e.g., assault versus natural disaster). With respect to posttraumatic stress disorder (PTSD) alone, interpersonal trauma confers greater risk for lifetime PTSD (Resnick et al., 1993), for poorer remission from PTSD (Chapman et al., 2012), and for PTSD reactions triggered by subsequent trauma (Cougle, Resnick, & Kilpatrick, 2009). This pattern has sparked interest in uncovering the reasons for these elevated risks, with the longer-term goal of improving prevention and treatment for survivors of interpersonal trauma.
An emerging approach to this problem concerns emotional responses during or after a potentially traumatic event (termed “peritraumatic” and “posttraumatic” emotions, respectively, or posttrauma appraisals), and the possibility that they vary by trauma type (Amstadter & Vernon, 2008; Bovin & Marx, 2011; DePrince, Chu, & Pineda, 2011). The premise of this approach is that the qualitatively different biopsychosocial processes (e.g., cognitive appraisals, motivational tendencies, neurobiological responses) associated with different specific emotions (e.g., fear, anger, sadness) lead to different patterns of posttrauma adjustment. Emotions experienced during a traumatic event are implicated in this process, as are those that arise during posttrauma reflection and that are subsequently incorporated into the autobiographical event memory (Bovin & Marx, 2011; Rubin, Berntsen, & Bohni, 2008). Either way, measurement of peritraumatic emotion involves asking participants to report retrospectively on their subjective emotional responses at the time of the traumatic event. These felt emotions are assumed to indicate activation of various other emotion-related processes (Bovin & Marx, 2011).
In support of this approach, cross-sectional studies reveal different patterns of peritraumatic emotions (retrospectively reported or activated by memory recall) for interpersonal versus impersonal trauma, and for subtypes of interpersonal trauma, along with implications for trauma-related mental health. Compared to impersonal trauma, interpersonal trauma was associated with greater intensity of specific peritraumatic emotions such as anger and disgust (Badour et al., 2011) and shame and fear (La Bash & Papa, 2014), along with greater intensity of multiple, negative peritraumatic emotions (DePrince et al., 2011; Lancaster & Larsen, 2016). Regarding subtypes of interpersonal trauma, one month post-trauma, rape survivors were more likely than physical assault/robbery survivors to report feeling afraid, betrayed, detached, guilty, humiliated, and numb during the trauma, and they were less likely to report feeling calm (Kaysen, Morris, Rizvi, & Resick, 2005). Further, among college students reporting a history of sexual assault, physical assault, or impersonal trauma, the sexual assault group reported sharper increases in posttraumatic emotional intensity (i.e., “hours or days after the trauma when the participant felt the worst”) compared to the other two groups, especially for anger and shame (Amstadter & Vernon, 2008, p. 395). Finally, elevations in shame and fear, and in multiple negative peritraumatic emotions, have been implicated in the psychological functioning of interpersonal trauma survivors (e.g., posttraumatic stress (PTS) symptoms, depression, posttraumatic cognitions) (La Bash & Papa, 2014; Lancaster & Larsen, 2016).
Although the study of peritraumatic emotions shows promise for advancing understanding of the elevated health risks of interpersonal trauma, a notable gap is apparent: Intimate partner abuse (IPA) has not received specific attention. However, theory and research argue that IPA is an important subtype of interpersonal trauma that shapes peritraumatic emotions in specific ways, with potential consequences for mental health. For example, IPA has been conceptualized as a social subordination stressor, or a stressor that involves loss of social status and interpersonal degradation, which can lead to shame (Herman, 2012). In this perspective, abuse characterized by coercive control is singled out as a source of particularly extreme subordination, and therefore potentially stronger shame reactions. This proposition is consistent with other research that emphasizes the necessity of differentiating dimensions of IPA, particularly coercive control, to achieve clarity around emotional consequences (Hardesty et al., 2015).
Because it occurs in an intimate interpersonal relationship, IPA can also be conceptualized as a betrayal trauma, or a trauma that occurs in the context of a close relationship that is needed for security or survival (Platt & Freyd, 2015). According to betrayal trauma theory and research, such trauma promotes responses that protect one against awareness and realization of betrayal (i.e., dissociation) so as to not jeopardize a vital attachment. Recently, betrayal trauma theory and research were expanded to encompass responses that function to appease a threatening person in order to support “self-preservation” (i.e., shame, as part of a submissive behavioral response) (Platt & Freyd, 2015, p. 399). In contrast to subordination theory, betrayal trauma theory makes no predictions about the roles of specific IPA dimensions in dissociation or shame. However, in concert with related research, it supports predictions about the roles of dissociation and shame in specific PTSD symptom clusters. That is, both intimate interpersonal trauma (Forbes et al., 2014) and perceived betrayal in the context of trauma (Kelley, Weathers, Mason, & Pruneau, 2012) were distinguished from other trauma types and from perceived life threat by stronger links with more severe symptoms of effortful avoidance and emotional numbing. From the perspective of betrayal trauma theory, this implies a role for shame and dissociation in these specific PTSD symptoms.
Although a number of studies have examined associations between IPA or betrayal trauma and state or trait measures of shame or dissociation (e.g., Platt & Freyd, 2015), few have examined peritraumatic emotions per se other than fear. A consistent pattern has not yet emerged. Among help-seeking women, the extent of psychological, physical, or sexual IPA was positively correlated with peritraumatic betrayal, fear, or shame (DePrince et al., 2011) and with peritraumatic dissociation (Fleming & Resick, 2016), although the latter association was ultimately explained by childhood trauma. In contrast, when community women’s most distressing traumatic events were classified as high, low, or no betrayal based on the relationship with the perpetrator, there were no statistically significant associations between this classification and peritraumatic emotions (i.e., anger, alienation, fear, betrayal, shame, self-blame) (DePrince et al., 2011). Together, these findings suggest that measuring the degree of exposure to IPA or betrayal trauma may be necessary to detect associations with the predicted emotions. However, comparing only two studies that also differ on other parameters (e.g., sample source) makes it difficult to draw conclusions.
To advance understanding of peritraumatic emotions in the context of IPA, the present study examined women’s retrospective reports of peritraumatic emotions during the incident of intimate partner abuse that currently bothered them most. Three separate questions assessed the presence of DSM-IV A2 peritraumatic emotions (fear, helplessness, horror) (American Psychiatric Association, 2000). One free-response question (“Did you experience any other emotions”?) elicited reports of other emotions. To add to the limited information on this topic, the first aim was to characterize women’s reports of peritraumatic emotions during the worst incident of intimate partner abuse. To determine if IPA exposure has implications for specific peritraumatic emotions, the second aim was to examine correlations between peritraumatic emotions and chronicity or frequency of exposure to three dimensions of IPA: direct assault (physical and sexual), dominance/isolation (an indicator of coercive control), and emotional/verbal abuse. Subordination theory predicts positive associations between coercive control and shame, whereas betrayal trauma theory predicts positive correlations between IPA dimensions and peritraumatic shame and dissociation. Finally, to determine if peritraumatic emotions have symptom-specific links in the context of IPA, the third aim was to test whether peritraumatic emotions theorized to be particularly central to IPA (shame and dissociation) are positively correlated with symptoms that are uniquely severe following intimate interpersonal or betrayal trauma (effortful avoidance and emotional numbing).
Method
Participants
Healthy midlife women with histories of divorce or permanent separation from stressful relationships were recruited from the community to participate in a broader investigation of IPA, inflammation, and aging (Newton et al., 2011). Recruitment materials were varied to include women with a range of IPA exposure and severity (i.e, “stressful relationship,” “extremely stressful relationship,” “upsetting thoughts or unwanted memories of a past stressful relationship.”) A phone interview established initial eligibility (i.e., history of divorce or permanent separation, English language ability, not in a currently or previously abusive intimate relationship, no ongoing divorce-related legal issues, no recent psychiatric hospitalization) and biomedical eligibility (i.e., age 45 to 60 years, post-menopausal, no chronic medical conditions or use of substances or medications with inflammatory effects).
Out of 577 callers, 69 eligible and interested women attended two research visits, and were compensated $140.00. Study procedures were approved by the University of Louisville Institutional Review Board, and written informed consent was obtained from women at visit one.
Women reported on demographics (visit one) and lifetime IPA (visit two), and completed the Clinician Administered PTSD Scale for DSM-IV (CAPS, Blake et al., 2000) for assessment of peritraumatic emotions and PTSD symptoms (visit two) with respect to IPA or non-IPA events (see CAPS interview description below). Four women were inadvertently not asked the free-response question about other peritraumatic emotions. Of the remaining 65 women, 45 completed the CAPS for IPA events and served as the sample for the present study. Women’s mean age was 54.53 years (SD = 3.19). Most women self-identified as White (84%), were employed full-time or part-time (82%), and were currently divorced or permanently separated (76%). Forty-four percent of women had attained a college degree or higher, and 41% had an annual household income of $40,000.00 or above.
Measures
Intimate Partner Abuse
Direct assault was measured using 11 physical assault items and 2 sexual assault items from the Revised Conflict Tactics Scale (Hardesty et al., 2015; Straus, Hamby, & Warren, 2003). Women rated each item with respect to frequency of occurrence across all adult intimate relationships from which they had divorced (0 = never, 1 = once, 2 = twice, 3 = 3–5 times, 4 = 6–10 times, 5 = 11–20 times, 6 = more than 20 times). Items with response ranges were recoded as the midpoint (e.g., “3-5” was coded as “4”), “6” was recoded as “25,” and recoded values were summed to indicate direct assault chronicity.
Two 7-item subscales of the Psychological Maltreatment of Women Inventory—Short Form (Tolman, 1989) measured dominance/isolation (α = .76) and emotional/verbal abuse (α = .86). Women rated the frequency (1 = never, 5 = very frequently) for each item, considering all adult intimate relationships from which they had divorced. Frequency scores were calculated by summing item ratings. A cut score of 19 or above on the dominance/isolation subscale is validated to identify exposure to coercive control (Hardesty et al., 2015).
CAPS Interview
To identify a focus for the interview, women indicated which best applied to them: a list of IPA events (i.e., an intimate partner or ex-partner…threatened you with physical harm, hurt you physically, forced you or attempted to force you into unwanted sexual activity) or non-IPA events (i.e., accident, natural disaster, physical or sexual victimization by anyone other than intimate partner, mugging, illness, unexpected death of another, combat). The 45 women who chose either the list of IPA events or both lists completed the CAPS with respect to IPA events.
Peritraumatic Experiences and Emotions.
Women called to mind the specific IPA incident that bothered them most at the time of the interview. They reported how long ago the incident occurred, and whether they experienced (0 = no, 1 = yes) the following during the incident: three DSM-IV A1 experiences (i.e., perceived life threat; concern about serious injury; threat to physical integrity), and three DSM-IV A2 emotions (i.e., anxious or frightened, helpless, horrified). Women were then asked one free-response question: “Did you experience any other emotions?” Responses were recorded verbatim and submitted to lexical analysis (described below).
PTSD Symptoms.
Separate frequency and intensity ratings (0 to 4) for each of the 17 PTSD symptoms were summed to form symptom severity scores. The 17 symptom severity scores were summed to form a total symptom severity score (α = 0.83), and symptom cluster severity scores: intrusive re-experiencing (5 items, α = .78), effortful avoidance (2 items, α = .75), emotional numbing (5 items, α = .72), hyperarousal (5 items, α = .02). The hyperarousal cluster was dropped from further analysis because of low internal consistency. All CAPS interviews were audiotaped, and 20% were selected for reliability coding. The intraclass correlation coefficient for overall symptom severity was 0.93.
Lexical Analysis
An initial review of women’s responses to the free-response question (“Did you experience any other emotions?”) revealed that existing lexicons were not sufficient to classify the words women used to describe their emotions, for multiple reasons. First, this study required classification of words by specific emotions, but existing lexicons do not necessarily take this approach. For example, although the default lexicon of Linguistic Inquiry and Word Count text analysis program (LIWC2015, Pennebaker, Boyd, Jordan, & Blackburn, 2015) identifies three specific emotions (anxiety, anger, sadness), it classifies the words “shame” and “embarrassment” as anxiety, and the word “humiliated” as anxiety and anger. Second, although there is a freestanding lexicon for shame (McGregor, 2010), it uses words that directly indicate shame (e.g., ashamed, degraded). However, some theorists conceptualize shame as including a broader family of words that “signal shame without calling it by name” (e.g., rejected, disrespected, p. 1107, Retzinger, 1995), and these indirect indicators were commonly reported by women in the present study. Third, although not typically classified as an emotion per se, women reported dissociation-related words (e.g., confusion, shutdown) when asked about their emotions, but a lexicon that included dissociation was not identified.
Accordingly, using words reported by the full sample of 65 women in response to the free-response question, a lexicon was developed using the following iterative approach. First, words reported by all 65 women were classified using an existing lexicon for guilt and shame (direct indicators) (McGregor, 2010). Second, two raters determined whether words unclassified in step one matched any indirect indicators of shame from three categories of the broader shame family (abandonment or “feelings of not belonging or otherwise being separated from significant others”; ridicule or “feeling emotionally hurt or threatened; being put down or made to look foolish or different”; inadequate or feeling “one does not measure up to one’s own or other’s ideal image”) (Retzinger, 1995, p. 1108). Inter-rater agreement was strong (K = 0.88). Third, two raters determined whether words unclassified in steps one and two were specific and unambiguous examples of either anxiety, anger, or sadness. Inter-rater agreement was moderate (K = 0.53). Fourth and finally, two raters determined whether words unclassified in steps one through three matched 37 feelings related to dissociation—19 from the Shutdown Dissociation Scale (Shut-D, Schalinski, Schauer, & Elbert, 2015), and 18 from the Peritraumatic Dissociative Experiences Questionnaire (PDEQ, Marmar, Weiss, & Metzler, 1997). Inter-rater agreement was strong (K = 0.75). Raters resolved all disagreements through discussion.
The resulting lexicon (see Appendix) was loaded into the LIWC2015 program and used to classify the words of the 45 women who described their other emotions in response to worst incidents of IPA. Using the lexicon, their words were classified into seven peritraumatic emotions: guilt, shame (direct and indirect indicators), anxiety, anger, sadness, dissociation (feelings from the Shut-D and PDEQ), and unclassified (words for which raters did not agree about classification).
Data Analytic Strategy
Because some continuous variables were non-normally distributed, associations between continuous variables were tested using Spearman’s rank-order correlation coefficients (rs). Similarly, associations between dichotomous and continuous variables were conducted using rank-biserial correlation coefficients (rrb), with tests of statistical significance derived from the Wilcoxon rank-sum test (Willson, 1976). All tests of statistical significance (two-tailed) were evaluated at p < .05. Some tests of associations were conducted to confirm hypotheses, whereas others were conducted to generate hypotheses, given the lack of evidence in this area. Therefore, corrections for multiple comparisons were not used.
Results
IPA Characteristics
All but two women reported at least once instance of direct assault. The median score for direct assault chronicity was 22.00 times (IQR = 35.00). Mean frequency scores for dominance/isolation abuse and emotional/verbal abuse were 20.16 (SD = 5.71) and 23.58 (SD = 6.76), respectively. Applying the recommended cut score to the dominance/isolation subscale, 60% of women had been exposed to coercive control (Hardesty et al., 2015). There were statistically significant positive correlations between direct assault chronicity and both dominance/isolation (rs = 0.35, p =.019) and emotional/verbal abuse (rs = 0.40, p = .006), and between both types of psychological abuse (rs = 0.65, p < .0001).
Women’s worst incidents of IPA occurred from 1.5 to 41 years before study participation, with a median of 16 years (IQR = 20). During worst incidents, 58% of women perceived life threat, 80% had concern about serious injury, and 80% perceived threat to physical integrity.
Lexical Analysis
Figure 1a shows the classification of the 52 unique words women used to describe their other emotions in response to worst incidents of IPA. Words pertaining to shame were the most common, followed by anger and dissociation, anxiety, sadness, and guilt. Seven unique words were unclassified because raters did not agree about category fit. Of words classified as shame, 32% were direct indicators, and 68% were indirect indicators. Of words classified as dissociation, equal numbers were from the Shut-D and the PDEQ.
Figure 1.
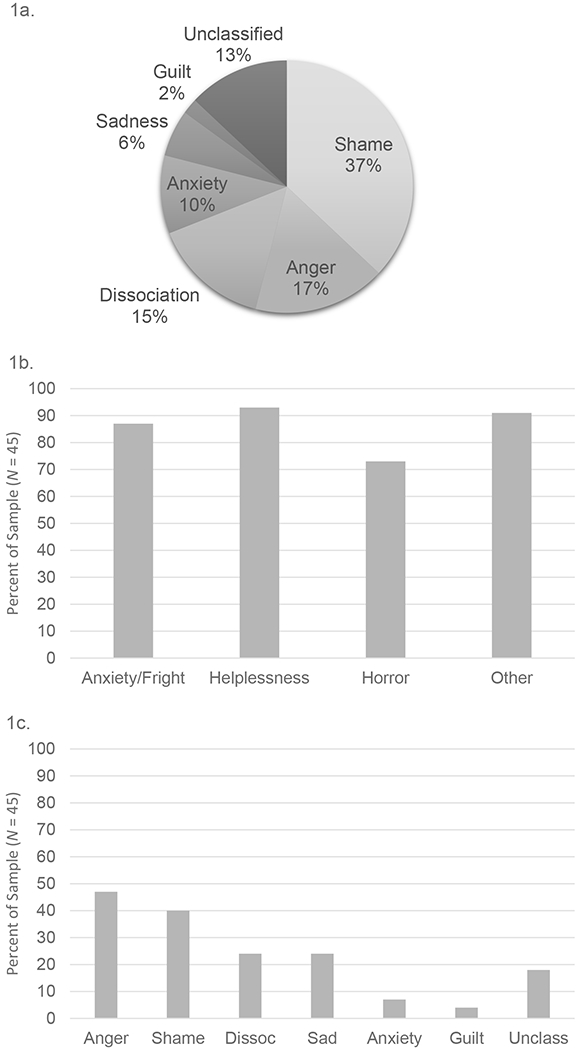
a) Classification of words used to describe emotional responses to worst incidents of IPA; b) Prevalence of three DSM-IV A2 peritraumatic emotions and any other peritraumatic emotion identified by lexical analysis; c) Prevalence of specific other peritraumatic emotions identified by lexical analysis (Dissoc = dissociation, Unclass = unclassified).
Peritraumatic Emotions
Most women reported experiencing each DSM-IV A2 peritraumatic emotion (anxiety/fright, helplessness, and horror) and at least one other peritraumatic emotion identified by lexical analysis (inclusive of unclassified emotions) during worst incidents of IPA (see Figure 1b). Twenty-one women reported one other peritraumatic emotion, 18 reported two or three other emotions, and two reported four other emotions.
Categorical variables were computed to indicate the presence (1) or absence (0) of each of the specific peritraumatic emotions identified by lexical analysis (inclusive of unclassified emotions). As shown in Figure 1c, anger and shame were most prevalent in response to worst incidents of IPA, followed by dissociation and sadness, which were equally prevalent. Anxiety and guilt were less prevalent. Also, 18% of women reported an unclassified emotion. When peritraumatic shame was defined based on direct versus indirect indicators, prevalence rates were similar (20% and 29% of women, respectively). When peritraumatic dissociation was defined based on feelings from the Shut-D versus the PDEQ, prevalence rates were similar (11% and 16% of women, respectively).
Anxiety was dropped from further analysis because of low variability (i.e., most women reported DSM-IV A2 anxiety/fright, and few women reported anxiety when asked about other emotions). Helplessness and guilt were dropped from further analysis for similar reasons.
Associations with IPA Dimensions
As shown in Table 1, there were statistically significant, positive correlations between chronicity of direct assault and frequency of verbal/emotional abuse and the presence of dissociation during the worst incident of IPA. Further, a negative association between frequency of dominance/isolation—an indicator of coercive control—and the presence of anger during the worst incident of IPA approached statistical significance. No other associations were statistically significant, including the predicted association with shame (ps > .11). Similarly, when peritraumatic shame was defined based on direct shame indicators only, no statistically significant associations with IPA dimensions were observed (rrb = −.23 to −.05, ps > .30).
Table 1.
Peritraumatic Emotions During Worst Incidents of IPA: Correlations (rrb) with IPA Dimensions and PTS Symptoms
| IPA Dimensions | PTS Symptoms | ||||||
|---|---|---|---|---|---|---|---|
| Peritraumatic Emotions | Direct assault chronicity | Dominance/isolation abuse frequency | Verbal/emotional abuse frequency | Intrusions | Effortful avoidance | Numbing | Total severity |
| Anger | .07 | −.34 * | −.15 | .06 | −.13 | .01 | −.07 |
| Shame | −.28 | −.21 | −.10 | .20 | .32 ** | −.07 | .12 |
| Dissociation | .45 ** | .26 | .45 ** | .05 | .00 | .14 | .09 |
| Sadness | .05 | −.06 | .04 | .03 | .10 | .10 | .17 |
| Horror | .06 | .19 | −.02 | −.14 | −.31 | −.23 | −.33 |
Note:
p ≤ .037
p = .052.
For peritraumatic emotions, absence = 0, presence = 1. IPA = intimate partner abuse. PTS = posttraumatic symptoms.
These associations were followed up by examining whether IPA dimensions were linked with A1 characteristics during worst incidents (i.e., perceived life threat, concern about serious injury, threat to physical integrity), and whether A1 characteristics were linked with peritraumatic dissociation and anger. Rank-biserial correlations and chi-square tests of association, respectively, revealed no statistically significant effects (ps ≥ .08), with two exceptions: more frequent exposure to dominance/isolation abuse was positively correlated with threat to physical integrity (rrb = 0.55, p = .01), and perceived life threat was negatively correlated with peritraumatic anger (φ = −0.37, p = .01).
Associations with Current Posttraumatic Stress Symptoms
For total PTS symptom severity related to the worst incident of IPA (Mdn = 6.00, IQR = 15), no women exceeded the cut score of 65 recommended to identify syndromal PTSD, and three met or exceeded the more lenient cut score of 45 (Weathers, Ruscio, & Keane, 1999). Scores for the PTS symptoms clusters were as follows: intrusive re-experiencing (Mdn = 0, IQR = 4), effortful avoidance (Mdn = 0, IQR = 4), emotional numbing (Mdn = 0, IQR = 5). As shown in Table 1, there was a statistically significant, positive association between the presence of shame during the worst incident of IPA and current symptoms of effortful avoidance. No other statistically significant associations were observed (ps > .06).
Discussion
Interpersonal trauma confers high risk for mental health problems compared to other trauma types, but the reasons for this remain unknown. Peritraumatic emotions, and whether they vary by trauma type and contribute to differences in posttrauma adjustment, offer one approach to this problem. Unfortunately, IPA has received limited attention in this regard, despite theory and research that support specific predictions.
To begin to address this gap, the present study identified emotions that women remembered feeling during worst incidents of IPA and examined their prevalence. Most women reported experiencing the DSM-IV A2 emotions and at least one other peritraumatic emotion. The DSM-IV A2 emotions were more prevalent than the specific emotions identified by lexical analysis of women’s own words, but this might be explained by different assessment approaches (i.e., recognition versus recall). Among the specific emotions identified by lexical analysis, shame and anger were most prevalent (reported by 40-47% of the sample). Sadness and dissociation were roughly half as prevalent as anger and shame. Guilt was not prevalent, despite being a specific focus in some treatments for IPA-related PTSD (Kubany et al., 2004). However, if guilt arises from reflecting on a trauma and its aftermath, assessment of guilt might require asking participants about emotions that arose after, as opposed to during, the worst incident of IPA. With respect to specific words used by women, indirect indicators of shame (i.e., feelings of abandonment, ridicule, and inadequacy) were more common than direct indicators. Feelings of dissociation from the PDEQ and the Shut-D were equally common. Thus, attention to women’s own words reveals that studies of IPA and peritraumatic emotions will benefit from taking broad views of both shame and dissociation.
To assess the role of IPA exposure in peritraumatic emotions during worst incidents of IPA, predictions motivated by subordination theory and betrayal trauma theory were tested. Both theories predict positive correlations between IPA and shame, but for somewhat different reasons (i.e., as a response to interpersonal degradation, or as part of appeasement and self-preservation in response to threat, respectively). Moreover, subordination theory predicts that coercive control specifically will be linked to shame. Contrary to all of these predictions, there were no statistically significant associations between any IPA dimension, including an indicator of coercive control, and peritraumatic shame. This was true despite the prevalence of both peritraumatic shame and coercive control, and it held when analyses were limited to direct indicators of shame.
One possible explanation for the lack of association between IPA and shame hinges on study design. The observed high prevalence of peritraumatic shame might be consistent with predictions from betrayal trauma theory, but detection of this effect could require comparison with non-IPA or low-betrayal traumas. However, the absence of positive associations between IPA frequency or chronicity and peritraumatic shame is still surprising; betrayal trauma theory and research specifically highlight the role of betrayal trauma exposure history in amplifying this emotional response to interpersonal threat (Platt & Freyd, 2015). Another possible explanation hinges on measurement. The present study examined the presence of shame and other emotions, whereas other studies of trauma type and emotion have focused on emotional intensity (e.g., Amstadter & Vernon, 2008; Platt & Freyd, 2015). In discussion of subordination theory, Herman (2012, p. 162) noted that “mild experiences of shame are part of ordinary life; but in its extreme forms, shame is a reaction to being degraded.” Thus, to detect associations with IPA exposure, it may be necessary to measure the intensity of peritraumatic shame, rather than its presence or absence. This could be addressed by incorporating ratings of valence and arousal into analysis of specific peritraumatic emotions.
Unexpectedly, a negative correlation between frequency of dominance/isolation abuse and the presence of peritraumatic anger during worst incidents of IPA approached statistical significance. Follow-up analyses suggested a role for perceived threat (inclusive of life threat, and threat to physical integrity) in this correlation. Dominance/isolation abuse was associated with more perceived threat during worst IPA incidents, and perceived threat was associated with the absence of peritraumatic anger. To understand this unexpected pattern, two lines of research are relevant, along with remembering that dominance/isolation is an indicator of coercive control, which in turn is central to subordination theory of IPA. First, research on IPA subtypes argues that coercive control, compared to relationship violence without a coercive component, functions to “suppress rather than resolve” relationship conflict (Stark, 2006, p. 1024). Second, research on interpersonal hierarchies and emotion shows that lower power persons minimize or suppress direct expression of anger to reduce opportunities for conflict or retaliation (van Kleef & Lange, 2020). Through frequent exposure to control and subordination, and perhaps particularly when threat is perceived, this process could conceivably become automatic such that angry feelings themselves are suppressed (Mauss, Bunge, & Gross, 2007). This post hoc interpretation is consistent with subordination theory of IPA, although not explicitly predicted by it, and requires evaluation in future research.
In contrast to results for shame and anger, chronicity/frequency of IPA exposure was positively correlated with peritraumatic dissociation. This is consistent with betrayal trauma research and theory, which predicts that betrayal trauma history exacerbates dissociation, including in response to subsequent exposure to interpersonal threat (Platt & Freyd, 2015). From this perspective, dissociation involves detaching from awareness of abuse in order to maintain a vital attachment. Measuring perceived dependence or potential indicators of dependence (e.g., unemployment, number of young children) in future research will help bolster this interpretation (Babcock & Deprince, 2013). Betrayal trauma theory makes no predictions about the IPA dimensions most likely to be associated with dissociation. Here, direct assault and emotional/verbal abuse showed similar associations with peritraumatic dissociation. Research with larger samples will be needed to determine whether their shared or unique variance is linked to peritraumatic dissociation, and to understand the relative roles of physical and emotional IPA in betrayal trauma.
Conceptualizing IPA as a either a subordination stressor or a betrayal trauma yields more precise predictions about the pattern of peritraumatic emotions expected after IPA incidents. However, this has clinical import only to the extent that such emotions are connected to longer-term functioning. Consequently, this study tested hypothesized linkages between peritraumatic emotions proposed to be prominent in IPA (shame, dissociation) and symptom clusters that are prominent in intimate interpersonal trauma (effortful avoidance, emotional numbing). Hypotheses were partially supported. A positive association between the presence of peritraumatic shame during the worst incident of IPA and current severity of interview-assessed effortful avoidance linked to the same worst incident was observed. In contrast, there were no statistically significant associations involving peritraumatic dissociation, or the emotional numbing symptom cluster. The low level of PTSD symptom severity in the present sample may have limited the ability to detect associations. Nevertheless, these preliminary results reveal that peritraumatic emotions may help explain the mental health sequelae of interpersonal trauma. They specifically suggest the presence of shame-based effortful avoidance in the context of IPA exposure.
This study has several limitations. The sample of healthy midlife women was small and unrepresentative; women were predominantly White and experienced IPA in the context of a heterosexual relationship. Replication in a larger sample that is diverse with respect to health status and sociodemographics is necessary. The associations reported here may underestimate those that will be observed among more symptomatic persons. The present results should not be assumed to generalize to all past intimate relationship statuses (i.e., married, cohabiting, dating). Although an entirely uniform pattern has not emerged, these statuses affect IPA severity, which could in turn affect the quality of worst incidents and ensuing emotional reactions (Brownridge et al., 2008; Krienert & Walsh, 2018; Sorenson & Spear, 2018). For methodological reasons, peritraumatic fear or anxiety had low variability and could not be adequately examined; for both practical and theoretical reasons, it will be critical to address this in future research. In terms of study design, a comparison condition (e.g., non-IPA trauma) was not included, limiting the ability to draw strong conclusions about IPA per se. Further, while the present study was motivated by an implicit model in which IPA experiences lead to peritraumatic emotions, and emotions lead to PTSD symptoms, no conclusions about causal direction can be drawn from this cross-sectional study. Finally, women’s retrospective reports of IPA and peritraumatic emotions spanned years to decades. Because event memories are important for mental health, this does not diminish the relevance of the study (Rubin et al., 2008). However, measures taken closer in time to trauma exposure may yield different results, given that memories can change over time as a function of various mechanisms (Levine, Lench, & Safer, 2009).
The present findings contribute to the limited understanding of peritraumatic emotions in the context of IPA and have broader implications for research and clinical practice. Regarding research, widely used lexicons were not adequate to classify the words women used to describe their peritraumatic emotions. Existing lexicons could be enriched by including the emotional experiences of trauma-exposed persons, by being modified for assessment of specific emotions, and by incorporating valence and arousal ratings to assess emotional intensity. Regarding clinical practice, peritraumatic shame may be common among IPA survivors, but it may often be expressed indirectly. Also, in clinical work with IPA survivors, the possibility of shame-based effortful avoidance should be considered, even among less symptomatic persons.
Acknowledgments
This research was supported by funding from the National Institute on Aging.
Appendix. Classification of Words Used to Describe Other Emotions
| Peritraumatic Emotion Classification | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Guilt | Shame | Anxiety | Anger | Sadness | Dissociation | Unclassified | |||
| Women’s Words | Directa | Indirectb | Shut-D | PDEQ | |||||
| *alone | X | ||||||||
| *anger | X | ||||||||
| *angry | X | ||||||||
| anxious | X | ||||||||
| *ashamed | X | ||||||||
| *betrayed | X | ||||||||
| *breathless | X | ||||||||
| *combative | X | ||||||||
| *compliant | X | ||||||||
| *confused | X | ||||||||
| *confusion | X | ||||||||
| *cried | X | ||||||||
| daze | X | ||||||||
| depressed | X | ||||||||
| *detached | X | ||||||||
| devastated | X | ||||||||
| disappointed | X | ||||||||
| *disbelief | X | ||||||||
| *disgust | X | ||||||||
| disorientation | X | ||||||||
| *disrespected | X | ||||||||
| *dissociated | X | ||||||||
| distraught | X | ||||||||
| *embarrassed | X | ||||||||
| *embarrassment | X | ||||||||
| *empty | X | ||||||||
| fainted | X | ||||||||
| *fear | X | ||||||||
| floundering | X | ||||||||
| *fought | X | ||||||||
| *freeze | X | ||||||||
| frustrated | X | ||||||||
| *gaveup | X | ||||||||
| *guilt | X | ||||||||
| *hate | X | ||||||||
| *hatred | X | ||||||||
| *hollered | X | ||||||||
| hopeless | X | ||||||||
| *humiliated | X | ||||||||
| *humiliation | X | ||||||||
| *hurt | X | ||||||||
| *hysterical | X | ||||||||
| *inconsequential | X | ||||||||
| *indecision | X | ||||||||
| infuriated | X | ||||||||
| insulted | X | ||||||||
| *loss | X | ||||||||
| *meek | X | ||||||||
| meltdown | X | ||||||||
| *nondeserving | X | ||||||||
| *numb | X | ||||||||
| *panic | X | ||||||||
| *powerful | X | ||||||||
| prayed | X | ||||||||
| *rejected | X | ||||||||
| sad | X | ||||||||
| *sadness | X | ||||||||
| scared | X | ||||||||
| *shame | X | ||||||||
| *shock | X | ||||||||
| *shocked | X | ||||||||
| *shutdown | X | ||||||||
| *startled | X | ||||||||
| stunned | X | ||||||||
| *stupid | X | ||||||||
| *surprised | X | ||||||||
| uncertain | X | ||||||||
| unreality | X | ||||||||
| *upset | X | ||||||||
| *wornout | X | ||||||||
| worried | X | ||||||||
| *worthless | X | ||||||||
| *yelled | X | ||||||||
Note. N = 65.
Words used to describe emotion in response to worst incidents of IPA (n = 45); all other words were used to describe emotion in response to a variety of non-IPA events (n = 20).
Based on McGregor (2010);
Based on Retzinger (1995);
PDEQ = Peritraumatic Dissociative Experiences Questionnaire; Shut-D = Shutdown Dissociation Scale.
References
- Amstadter AB, & Vernon LL (2008). Emotional reactions during and after trauma: A comparison of trauma types. Journal of Aggression, Maltreatment, & Trauma, 16(4), 391–408. doi: 10.1080/10926770801926492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2000). Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, D.C.: American Psychiatric Association. [Google Scholar]
- Babcock RL, & Deprince AP (2013). Factors contributing to ongoing intimate partner abuse: childhood betrayal trauma and dependence on one’s perpetrator. Journal of Interpersonal Violence, 28(7), 1385–1402. doi: 10.1177/0886260512468248 [DOI] [PubMed] [Google Scholar]
- Badour CL, Feldner MT, Babson KA, Smith RC, Blumenthal H, Trainor CD, Bunaciu L, & Olatunji BO (2011). Differential emotional responding to ideographic cues of traumatic interpersonal violence compared to non-interpersonal traumatic experiences. Journal of Experimental Psychopathology, 2(3), 400–417. doi: 10.5127/jep.014711 [DOI] [Google Scholar]
- Blake D, Weathers F, Nagy L, Kaloupek D, Klauminzer D, Charney D, Keane T, & Buckley TC (2000). Instruction Manual: Clinician Administered PTSD Scale (CAPS). Behavioral Sciences Division and Neurosciences Division, National Center for Posttraumatic Stress Disorder. Boston, MA and West Haven, CT. [Google Scholar]
- Bovin MJ, & Marx BP (2011). The importance of the peritraumatic experience in defining traumatic stress. Psychological Bulletin, 137(1), 47–67. doi: 10.1037/a0021353 [DOI] [PubMed] [Google Scholar]
- Brownridge DA, Chan KL, Hiebert-Murphy D, Ristock J, Tiwari A, Leung WC, & Santos SC (2008). The elevated risk for non-lethal post-separation violence in Canada: A comparison of separated, divorced, and married women. Journal of Interpersonal Violence, 23(1), 117–135. doi: 10.1177/0886260507307914 [DOI] [PubMed] [Google Scholar]
- Chapman C, Mills K, Slade T, McFarlane AC, Bryant RA, Creamer M, Silove D, & Teesson M (2012). Remission from post-traumatic stress disorder in the general population. Psychological Medicine, 42(8), 1695–1703. doi: 10.1017/S0033291711002856 [DOI] [PubMed] [Google Scholar]
- Cougle JR, Resnick H, & Kilpatrick DG (2009). Does prior exposure to interpersonal violence increase risk of PTSD following subsequent exposure? Behaviour Research and Therapy, 47(12), 1012–1017. doi: 10.1016/j.brat.2009.07.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DePrince AP, Chu AT, & Pineda AS (2011). Links between specific posttrauma appraisals and three forms of trauma-related distress. Psychological Trauma: Theory, Research, Practice, and Policy, 3(4), 430–441. doi: 10.1037/a0021576 [DOI] [Google Scholar]
- Fleming CJ, & Resick PA (2016). Predicting three types of dissociation in female survivors of intimate partner violence. Journal of Trauma and Dissociation, 17(3), 267–285. doi: 10.1080/15299732.2015.1079807 [DOI] [PubMed] [Google Scholar]
- Forbes D, Lockwood E, Phelps A, Wade D, Creamer M, Bryant RA, McFarlane A, Silove D, Rees S, Chapman C, Slade T, Mills K, Teesson M, & O’Donnell M (2014). Trauma at the hands of another: distinguishing PTSD patterns following intimate and nonintimate interpersonal and noninterpersonal trauma in a nationally representative sample. Journal of Clinical Psychiatry, 75(2), 147–153. doi: 10.4088/JCP.13m08374 [DOI] [PubMed] [Google Scholar]
- Hardesty JL, Crossman KA, Haselschwerdt ML, Raffaelli M, Ogolsky BG, & Johnson MP (2015). Toward a standard approach to operationalizing coercive control and classifying violence types. Journal of Marriage and Family, 77(4), 833–843. doi: 10.1111/jomf.12201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman JL (2012). Shattered shame states and their repair. In Yellin J & White K (Eds.), Shattered States: Disorganized Attachment and its Repair (pp. 157–170). London: Karnac. [Google Scholar]
- Kaysen D, Morris MK, Rizvi SL, & Resick PA (2005). Peritraumatic responses and their relationship to perceptions of threat in female crime victims. Violence Against Women, 11(12), 1515–1535. doi: 10.1177/1077801205280931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley LP, Weathers FW, Mason EA, & Pruneau GM (2012). Association of life threat and betrayal with posttraumatic stress disorder symptom severity. Journal of Traumatic Stress, 25(4), 408–415. doi: 10.1002/jts.21727 [DOI] [PubMed] [Google Scholar]
- Krienert JL, & Walsh JA (2018). An examination of intimate partner sexual violence: Comparing marital and nonmarital incidents employing NIBRS Data, 2008-2012. Partner Abuse, 9(1), 41–57. [Google Scholar]
- Kubany ES, Hill EE, Owens JA, Iannce-Spencer C, McCaig MA, Tremayne KJ, & Williams PL (2004). Cognitive trauma therapy for battered women with PTSD (CTT-BW). Journal of Consulting and Clinical Psychology, 72(1), 3–18. doi: 10.1037/0022-006X.72.1.3 [DOI] [PubMed] [Google Scholar]
- La Bash H, & Papa A (2014). Shame and PTSD symptoms. Psychological Trauma: Theory, Research, Practice, and Policy, 6(2), 159–166. doi: 10.1037/a0032637 [DOI] [Google Scholar]
- Lancaster SL, & Larsen SE (2016). Profiles of peritraumatic emotions. Journal of Aggression, Maltreatment & Trauma, 25(9), 1006–1018. doi: 10.1080/10926771.2016.1219802 [DOI] [Google Scholar]
- Levine LJ, Lench HC, & Safer MA (2009). Functions of remembering and misremembering emotion. Applied Cognitive Psychology, 23(8), 1059–1075. doi: 10.1002/acp.1610 [DOI] [Google Scholar]
- Marmar CR, Weiss DS, & Metzler TJ (1997). The Peritraumatic Dissociative Experiences Questionnaire. In Wilson JP & Keane TM (Eds.), Assessing Psychological Trauma and PTSD (pp. 412–428). New York: Guilford Press. [Google Scholar]
- Mauss IB, Bunge SA, & Gross JJ (2007). Automatic emotion regulation. Social and Personality Psychology Compass, 1, 146–167. doi: 10.1111/j.1751-9004.2007.00005.x [DOI] [Google Scholar]
- McGregor SA (2010). The analysis of personality through language: Narcissism predicts use of shame-related words in narratives. (Honors thesis). University of Michigan, Retrieved from https://deepblue.lib.umich.edu/bitstream/handle/2027.42/77645/staceymc.pdf;sequence=1 [Google Scholar]
- Newton TL, Fernandez-Botran R, Miller JJ, Lorenz DJ, Burns VE, & Fleming KN (2011). Markers of inflammation in midlife women with intimate partner violence histories. Journal of Women’s Health, 20(12), 1871–1880. doi: 10.1089/jwh.2011.2788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pennebaker JW, Boyd RL, Jordan K, & Blackburn K (2015). The development and psychometric properties of LIWC2015. University of Texas at Austin. Austin, TX. [Google Scholar]
- Platt MG, & Freyd JJ (2015). Betray my trust, shame on me: Shame, dissociation, fear, and betrayal trauma. Psychological Trauma: Theory, Research, Practice, and Policy, 7(4), 398–404. doi: 10.1037/tra0000022 [DOI] [PubMed] [Google Scholar]
- Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, & Best CL (1993). Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. Journal of Consulting and Clinical Psychology, 61(6), 984–991. [DOI] [PubMed] [Google Scholar]
- Retzinger SM (1995). Identifying shame and anger in discourse. American Behavioral Scientist, 38(8), 110–1113. [Google Scholar]
- Rubin DC, Berntsen D, & Bohni MK (2008). A memory-based model of posttraumatic stress disorder: Evaluating basic assumptions underlying the PTSD diagnosis. Psychological Review, 115(4), 985–1011. doi: 10.1037/a0013397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schalinski I, Schauer M, & Elbert T (2015). The shutdown dissociation scale (Shut-D). European Journal of Psychotraumatology, 6, 25652. doi: 10.3402/ejpt.v6.25652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorenson SB, & Spear D (2018). New data on intimate partner violence and intimate relationships: Implications for gun laws and federal data collection. Preventive Medicine, 107, 103–108. doi: 10.1016/j.ypmed.2018.01.005 [DOI] [PubMed] [Google Scholar]
- Stark E (2006). Commentary on Johnson’s “Conflict and control: Gender symmetry and asymmetry in domestic violence”. Violence Against Women, 12(11), 1019–1025. doi: 10.1177/1077801206293329 [DOI] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, & Warren WL (2003). The Conflict Tactics Scales Handbook. Los Angeles, CA: Western Psychological Services. [Google Scholar]
- Tolman RM (1989). The development of a measure of psychological maltreatment of women by their male partners. Violence and Victims, 4(3), 159–177. [PubMed] [Google Scholar]
- van Kleef GA, & Lange J (2020). How hierarchy shapes our emotional lives: Effects of power and status on emotional experience, expression, and responsiveness. Current Opinion in Psychology, 33, 148–153. doi: 10.1016/j.copsyc.2019.07.009 [DOI] [PubMed] [Google Scholar]
- Weathers FW, Ruscio AM, & Keane TM (1999). Psychometric properties of the nine scoring rules for the Clinician-Administered Posttraumatic Stress Disorder Scale. Psychological Assessment, 11, 124–133. [Google Scholar]
- Willson VL (1976). Critical values of the rank-biserial correlation coefficient. Educational and Psychological Measurement, 36, 297–300. [Google Scholar]


