Abstract
Both social disconnection and suicide are significant public health concerns among older adults, and social disconnection is associated with greater risk for suicide-related thoughts and behaviors in late life. We present a synthesis of research discussed during a workshop hosted by the NIMH on social disconnection and late-life suicide. Social disconnection is related to suicide risk in late life via a variety of mechanisms, including biological, behavioral, and psychological correlates. Researchers in several scientific fields have begun to establish these connections and identify targets for interventions to reduce risk in late life. While research has demonstrated that social connection is amenable to change, there is little research to date on the most evidence-based interventions to mitigate social disconnection or the related risks. However, there are several promising biological, behavioral, and psychological interventions that may target various mechanisms, as well as social disconnection itself. With a relative paucity of research in this area, these lines of study are ripe for innovative investigation. In order to most effectively advance the field, we must establish more consistent definitions of social connection and disconnection; more accurately measure and assess older adults’ social needs; examine the most effective approaches and modalities for assessment and intervention; take into account important contextual factors; and apply a translational, convergent scientific approach.
Keywords: older adults, geriatric, social connectedness, loneliness, isolation, depression
In the United States and internationally, the number of older adults is increasing: projections suggest one-fifth of the US population will be 65 years or older by 2030, with this population nearly doubling from approximately 40 million in 2010 to approximately 72 million by 2030.1,2 In response to this changing makeup of the population, more attention to public health concerns related to aging is necessary. Two significant and related public health concerns for the aging population are suicide deaths and social disconnection. In the US and in many regions of the world, older adults exhibit the highest rates of suicide deaths.3,4 In 2018, the most recent year for which US national data are available, the suicide rate for adults age 65 and older was 17.36 per 100,000, compared to 14.21 in the general population.3 The highest rates were among those age 85 and older, particularly among white men age 85 and older, with a suicide death rate of 51.85 per 100,000.3 Social disconnection is associated with suicide ideation, attempts, and deaths in later life and has been identified as a modifiable intervention target to reduce suicide risk, but few research studies have examined social connection as a means of suicide prevention. We describe a workshop sponsored by the National Institute of Mental Health (NIMH) involving experts in this field to discuss current and future directions in research for examining the associations between social connection and suicide in late life, and to work toward identifying mechanisms, treatment targets, and interventions to effectively improve social connection and reduce suicide risk in late life.
Terms for suicide-related thoughts and behaviors used in this paper are those from the CDC’s uniform definitions for self-directed violence5 as well as from research conducted to develop the Columbia Suicide Severity Rating Scale, a commonly used instrument for assessing suicide ideation and behavior in clinical trials.6 Suicidal ideation refers to thoughts about suicide, and may range in severity from wishing for death (i.e., passive ideation) to active thoughts of ending one’s life, consideration of methods, and active intent and specific plans to end one’s life. Suicide attempt refers to non-fatal self-directed potentially injurious behavior, which may or may not result in injury, with at least some intent to die. Death by suicide refers to fatal self-directed behavior with at least some intent to die. Risk and protective factors for any of the types of suicide-related thoughts and behaviors defined above can differ, and each presents unique challenges to researchers (e.g., suicide deaths occur at a low base rate, making power an issue for many studies on suicide).7,8 This NIMH workshop did not examine physician aid in dying.
The terms “social connection” and “social disconnection” encompass a number of dimensions of social relationships, including structural (e.g., size of social networks, marital status, living situation, social isolation), functional (e.g., received and perceived social support, loneliness), and quality-related (e.g., satisfaction with relationships, conflict) aspects of one’s social world.9 While societal-level variables (e.g., oppression, social capital, discrimination, policy) are relevant to suicide prevention, they were outside of the scope of the NIMH workshop. Lifespan developmental theories and research, including the socioemotional selectivity theory, posit a key role for social relationships in healthy aging and studies show generally increasing quality and satisfaction in social relationships in later life, though size of social networks may be somewhat reduced, due to greater selectivity and focus on more valued relational experiences.10 Despite misconceptions that older age is associated with loneliness and/or isolation, social disconnection is not considered normative, and loneliness may even decrease in later life.11 However, among some older adults, factors such as physical health and disability that limit opportunities for social activities, mental health and cognitive functioning, loss of partners, negative perceptions, and ageist stereotypes can lead to increased loneliness.12,13 While some risk factors for loneliness may be more prevalent in later life, social disconnection (e.g., loneliness) is not inevitable among older adults. The National Academy of Sciences has called for more robust research on interventions for social disconnection in later life, with a goal of translating that research into clinical practice to improve the health of older adults.14
Social disconnection is associated with suicide risk at all ages and the importance of social disconnection in suicidal behavior has been posited by theorists for more than a century,15,16 including Émile Durkheim’s work on social factors in suicidal behavior in the late 19th century.17 A contemporary psychological theory, the Interpersonal Theory of Suicide, posits that an unmet need to belong—termed low belonging—and feeling like a burden on others increase risk for suicide ideation.16 Other contemporary theories, including the Three-Step Theory of Suicide18 and the Motivational-Volitional Theory of Suicide19, also posit central roles for social disconnection in suicide risk.
Structural, functional, and quality-related dimensions of social disconnection, measured using both objective and subjective indicators, are related to suicidal ideation, attempts, and deaths.15,20,21 Indices of social connection, such as degree of social integration are associated with reduced risk of suicide deaths20,21, and indices of social disconnection, such as loneliness, are associated with increased risk of suicide death.15 Several dimensions of social disconnection, such as loneliness, relationship conflict, and social network size are associated with passive and active suicidal ideation, attempts, and suicide deaths among older adults, with less precise indicators of social connection, such as marital status, producing mixed findings.15,22,23 The most reliable findings linking social disconnection to suicide deaths (as well as all-cause mortality) come from studies using measures of social integration, which capture a range of aspects of an individual’s social experience, including network size, frequency of contact, and involvement in social groups.24
Though there is evidence that social disconnection is likely amenable to intervention25, there is little knowledge of what types of interventions may improve different aspects of social connection, and the evidence on the effectiveness of any particular intervention is limited, particularly in late life.25-31 However, social connections and processes have been identified as important mechanisms for explaining behavior, mental disorders, and intervention effects, including by the NIMH Research Domain Criteria (RDoC),32 which includes a social processes domain.33,34 Research to date has also suggested that constructs falling under this social processes RDoC domain are associated with suicide-related thoughts and behaviors.35
Due to public health concerns regarding social disconnection and suicide in late life, the NIMH convened a virtual workshop titled “Social Disconnection in Late Life Suicide: Mechanisms, Treatment Targets, and Interventions” on September 17-18, 2020, involving experts in related fields, including clinician scientists, behavioral scientists, neuroscientists, epidemiologists, and implementation scientists. The aims of the workshop were 1) to advance understanding of the mechanisms by which social disconnection may be associated with late life suicide, 2) to identify candidate targets for promising interventions to address social disconnection and suicide in late life, and 3) to discuss translation to develop and implement interventions and provide services to socially disconnected older adults at risk for suicide. Scientists in each of these areas presented current work, and breakout discussion sessions were conducted to discuss the state of the research and priorities for future research. Finally, a synthesis session was conducted to summarize the discussions. Presentations and sessions were recorded (available at https://www.nimh.nih.gov/news/events/2020/virtual-workshop-social-disconnection-and-late-life-suicide-mechanisms-treatment-targets-and-interventions.shtml). There were 47 documented active attendees/participants (chairs, organizers, presenters, moderators, panelists, and discussants). The presentations were open to a live audience that did not actively participate in the live discussion; over 350 audience members were in attendance. We present a summary of the research discussed during the workshop as well as gaps in knowledge and priorities for future research identified. We aim to integrate the ideas put forth at the workshop and the group’s consensus regarding research priorities.
We organize the research discussed during the workshop within an experimental therapeutics framework, which involves a process for developing and testing mental health interventions by specifying potentially modifiable mechanisms associated with mental health outcomes that can be ‘targeted’ by interventions to produce clinical and functional effects. The NIMH RDoC initiative is compatible with experimental therapeutics.36 We first discuss research on biopsychosocial mechanisms in the causal pathway between social disconnection and suicide; second, we discuss mechanisms that are potentially modifiable by interventions (i.e., target mechanisms); and finally, we discuss potential interventions that may ‘engage’ these targets. Figure 1 presents a conceptual model of mechanisms, targets, and intervention strategies discussed. Some, but not all, mechanisms may be potentially modifiable through intervention. Targets are selected from potentially modifiable mechanisms, and examples of intervention strategies to engage these selected targets are provided.
Figure 1.
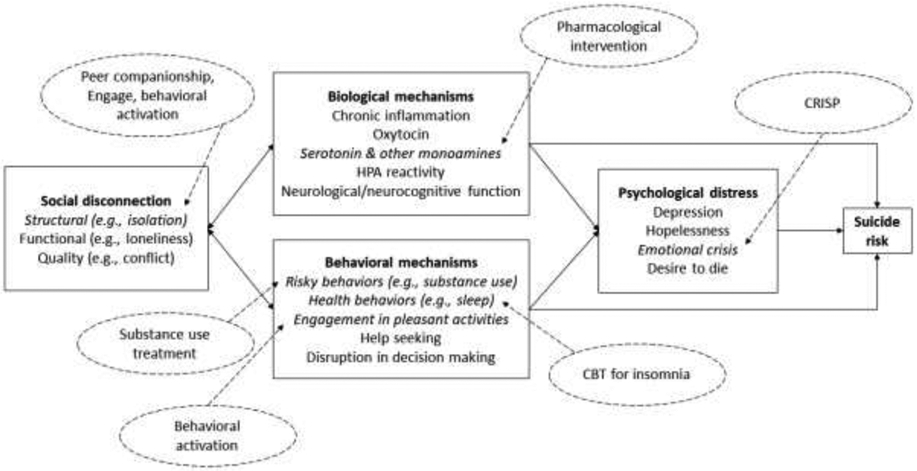
Model of causal pathway from social disconnection to suicide in late life. Includes mechanisms of this pathway (in solid boxes), as well as potential interventions (in dashed ovals). Examples are provided for all categories; list of examples is not comprehensive. Italicized items are examples of potential targets for intervention discussed in this paper; this is not a comprehensive representation of all mechanisms that may be targeted.
Mechanisms Underlying Social Disconnection and Late Life Suicide
Social disconnection likely influences suicide-related thoughts and behaviors by contributing to biological/physiological mechanisms, behavioral mechanisms, and psychological distress, while social connection may serve as a protective factor against suicide by strengthening an individual’s resilience to risk factors for suicide.
Biological mechanisms
Some have argued that social connection, or reducing loneliness, is a biological drive akin to hunger, motivating people to connect. Workshop participants discussed studies demonstrating that 10 hours of isolation was associated with a similar neural response pattern (via fMRI) as 10 hours without food37 and that ‘social pain’ (i.e., rejection) triggers physical pain-related neural regions.38 The Social Baseline Theory posits that the normal, or baseline, adaptive human neurological state is predicated on social proximity to and relationships with others as a necessary resource, whereas lack of social relationships puts the neurological system into an alert state due to an implied or perceived increased risk and increased level of effort needed to reach goals.39 When this state is prolonged, it can lead to depletion in neurological and physical resources and function. Physiological changes of this type may be associated with suicide risk. For example, chronic loneliness or exclusion is associated with chronic inflammation40, which in turn is associated with negative mental health outcomes such as depression.41,42 Oxytocin (which is key to social bonding, released with close social contact such as hugging, and impacted by social exclusion) has a complex association with risk for suicide attempts as well.43,44
Animal research suggests that potential neurobiological mechanisms include monoamine neurotransmitter levels and hypothalamic-pituitary-adrenal (HPA) axis activation. Social isolation has been shown to contribute to differences in monoamine neurotransmitter presentations in social animals; for example, isolation affects 5HT (serotonin)-related receptor gene transcription, serotonin levels throughout the brain, and excitability of serotonin neurons in studies of rodents and zebrafish.45-47 Social isolation may also affect levels of dopamine; serotonin and dopamine have effects on aggression, depressive behaviors, and anxiety behaviors.45-48 HPA axis response to acute stressors is greater in socially isolated rats compared to non-isolated rats.49 In human adults age 60 to 64 years, social isolation as measured by recent widowhood or newly living alone was associated with higher nighttime cortisol levels.50 In middle-aged adults, social isolation was associated with a greater increase in cortisol upon awakening at the beginning of the day, as well as higher cortisol output throughout the day.51 Other neurobiological systems may be associated with social disconnection and contribute to psychological distress and suicide-related thoughts and behaviors, including neuroinflammation, glutamatergic, and neuroplasticity processes.52 Further research on whether these processes mediate the associations between social disconnection and suicide in late life may identify additional mechanisms and targets for preventive intervention.
Research on the associations between dementia-related neuropathologies and social disconnection suggests other potential mechanisms. Dementia is associated with changes in social functioning and increased loneliness,53,54 and social changes have also been identified in preclinical, cognitively normal older adults presenting with dementia-related neuropathologies. Social engagement declined more over three years in cognitively normal older adults who present with higher beta-amyloid levels in the brain, a risk factor for Alzheimer’s disease, compared to those with lower beta-amyloid.55 In the group of participants with higher beta-amyloid, those with low baseline social engagement also exhibited faster decline in cognitive functioning over time compared to those who were more socially engaged.55 Cross-sectionally, greater beta-amyloid burden in the brain is associated with greater loneliness among cognitively normal older adults, even after controlling for objective social network.56 Greater tau pathology in the right entorhinal cortex is also associated with greater loneliness among cognitively normal older adults.57 These studies suggest specific brain pathologies associated with cognitive disorder in older adults may also be related to social engagement and perceived loneliness, independent of objective social support or social network. Social disconnection and suicide risk may also be linked with preclinical or mild neurobiological and neuro cognitive changes; although severe or late-stage cognitive impairment is associated with lower risk of death by suicide in several studies, mild or early-stage cognitive impairment can be a risk factor for suicide.58-60 Additionally, impairment in specific neurocognitive functions, such as executive functioning, are associated with suicide risk61,62 and may be related to neurocognitive processes such as those involved in reward learning that are discussed in the next section.
Behavioral mechanisms
Social connections are linked to healthier behaviors, whereas social disconnection has been linked to riskier and/or less healthy behaviors such as substance use and poor sleep patterns/habits,63-66 which in turn are associated with suicide-related thoughts and behaviors. For example, substance use is strongly associated with suicide risk at all ages, including late life.67 Sleep problems such as insomnia are related to suicide risk.68 Social connections may also be linked to engagement in pleasant activities, which are protective against depression69; in one study of community-dwelling older adults, engagement in pleasant activities mediated the association between physical disability and depression.70 These behavioral mechanisms are likely modifiable, and therefore may be intervention targets.
Another behavioral mechanism by which social connection may influence suicide risk is via coping and help seeking behaviors. According to lifespan developmental theories, such as the Selection, Optimization, and Compensation model (SOC)71 and the Motivational Theory of Lifespan Development72, with age people experience changes in functioning that affect their ability to reach their goals. When this occurs, they must utilize different coping strategies to optimize ability to reach goals. One important coping strategy may be seeking help from others. The use of compensatory strategies such as help seeking among those with functional limitations is associated with reduced suicidal ideation.73 The ability to seek and receive help as a compensatory strategy, however, may be somewhat dependent upon the availability and willingness of one’s social network to provide such support. In addition, receiving help that is inconsistent with one’s perceived need or values (e.g., receiving care when one places high value on independence) may be detrimental rather than helpful.74
Behaviors involved in decision making that may impact social interactions include reinforcement learning and expected reward value calculations in making social choices. Social adaptation and particularly the ability to reciprocate depend on cortico-striato-thalamic reinforcement learning.75 In turn, impaired reinforcement learning and value-based decision-making have also been linked to suicidal behavior and lethality of suicide attempts in late life.76-80 Further, while suicidal behavior was previously understood in terms of short-sighted preferences, recent work suggests that older high-lethality suicide attempters display inconsistent reward valuation, rather than a true stable preference for immediate rewards.81,82 The interplay of age-related social demands and decision-making deficits may serve to further explain suicide risk in late life.
Psychological distress and mental disorders
As mentioned above, later life is generally associated with improved emotional well-being due to greater selectivity around rewarding, close social relationships.10 Research has shown that maintaining such close, intimate social relationships, even while pruning less-close or peripheral relationships, in late life is associated with greater emotional well-being.10,83 However, emotional or psychological distress may still occur among those who lack or have lost closer social partners.10 On the other hand, variety in types of social contacts, and particularly more peripheral/weak ties, may also have benefits in late life.84
Depression and other forms of psychological distress are the most commonly identified risk factors for suicide in late life.85 Therefore, one mechanism through which social disconnection may contribute to suicide risk is through increases in psychological distress. Many studies discussed above on biological and behavioral mechanisms have demonstrated effects on depression, suggesting direct and indirect effects of social disconnection on psychological distress. Workshop participants discussed research on associations between social disconnection and depression. For example, research with African American older adults has shown that emotional support is negatively associated with depressive symptoms, while negative social interactions are positively associated with depressive symptoms.86 Examining the difference between subjective and objective social isolation, research has shown that subjective isolation is most consistently associated with depressive symptoms and psychological distress in older African American, Black Caribbean, and non-Hispanic White adults.87 These results show how various aspects of social connection can be associated with psychological distress, and the importance of examining the influence of cultural factors in shaping the experience of social connections and their impact on mental health.
Gaps in knowledge & future directions
Observational studies have demonstrated associations between diverse indices of social connection and suicide risk in later life, but few studies have focused on the mechanisms that explain the association between social disconnection and suicide in late life, and very little is known about the extent to which indices of social connection are modifiable via intervention. Research is needed to identify which dimensions of social disconnection are most strongly linked with suicide-related thoughts and behaviors, and the causal pathways by which risk is affected. A challenge for this work is both 1) examining multidimensional measures of social connection/disconnection and associations between varied mechanisms for the purpose of understanding the structure of risk, and 2) disentangling the specific effects of individual mechanisms for the purpose of targeted intervention. Multidimensional measures that include and differentiate diverse aspects of social connection, including structural, functional, and quality measures, may be especially useful indicators of those at risk for suicide,9 but it is not known if these measures are suitable for assessing intervention effects over time, nor if they identify useful targets. Translational science may also be particularly beneficial in examining interactions between the biopsychosocial mechanisms discussed above and in examining pathways from mechanisms to clinical outcomes, rather than examining only segments of the paths. Advances in theories of suicide may facilitate this integrative work.88 Greater understanding of the degree to which social disconnection contributes to suicide risk versus the presence of social connection mitigating the effect of other mechanisms may identify the most useful intervention targets and increase understanding of the etiology of suicide. Research on cultural and social differences in groups at lower risk for suicide, sometimes even despite arguably greater exposure to stressors (e.g., older Black women who exhibit some of the lowest suicide rates in the U.S.3), can inform our understanding of the roles of risk and protective mechanisms. The most potent mechanisms of risk and intervention targets may differ across cultural and sociodemographic groups.
Data science and examining big data may inform the study of mechanisms in the association between social connections and suicide in late life. The Veterans Affairs (VA) healthcare system, as the largest integrated health care system in the U.S., offers an example of using large-scale health data to examine predictors of suicidal behavior and death by suicide. The VA screens patients for suicidal ideation and several risk factors at patient visits, and VA health care data can also be linked with cause-specific mortality data. Research on risk and comorbidity/diagnosis profiles of older adults last seen in primary care before a suicide attempt (fatal and non-fatal) has shown that profiles characterized by chronic pain or by minimal comorbidity (both with low occurrence of depression diagnoses) were associated with more fatal attempts (mostly with firearms) than profiles characterized by higher comorbidity.89 Such results may reflect lower engagement with the health care system among the lower comorbidity/diagnosis groups, differences in methods used for attempts, and limitations in assessment for and diagnosis of depression in primary care settings. More effective engagement and interaction of Veterans with services may help to mitigate suicide risk. Other research has found that major life transitions (e.g., release from prison) are also associated with greater suicidal behavior in late life.90 A factor in this phenomenon may be disconnection from one’s social network while incarcerated and difficulty transitioning without adequate social support; increasing supportive services upon release/transition may reduce risk. These examples demonstrate how big data can be utilized to identify risk factors for late-life suicide that may be influenced by social processes. One important consideration for big data research is assessment and access. These lines of research are highly dependent upon the types and reliability of data collected by large health care systems, and data on social connections and social processes are rarely collected and documented in primary care and other health care settings on a consistent basis. Policy changes rooted in the public health implications of social disconnection may facilitate greater attention to and collection of social data in health care. The Institute of Medicine and the National Academy of Sciences recommend assessment of social determinants of health, including social connection, in health care settings,14,91 which would make more data available regarding social connection in large portions of the population.
Engaging Targets – Development and Implementation of Interventions
As research moves from the examination of potential target mechanisms through which social disconnection may influence suicide risk in late life, toward the development of interventions to improve social connection and reduce suicide risk, several considerations will be critical. Attendees at the NIMH workshop discussed several issues involved in applying what is known about social disconnection as a mechanism in suicide risk in later life to intervening on social connection as a target of behavioral interventions: assessment and intervention outside research contexts, the role of interventions to reduce psychological distress, the role of interventions to increase social engagement, and the use of digital technology. The discussion also covered lessons learned and new questions highlighted by the current COVID-19 pandemic.
Assessing social connection in the context of interventions involves several decisions: 1) what dimension of social disconnection will identify a population at risk; 2) how is the dimension best operationalized; 3) what language around social disconnection is understandable and acceptable to older adults (including sub-populations such as those with cognitive impairment); 4) what dimension of social connection is hypothesized to change from the intervention and over what period of time; and 5) what organizational factors of the community and/or context where the intervention will be delivered might impact assessment selection (e.g., administration time and availability in the electronic medical record). A person-centered perspective may be especially useful in the context of intervening on social connections, as older adults vary with regards to aspects of social connection that are most important to them; acceptability of interventions will be impacted by such values and preferences.92 Assessing barriers to social connections may also be useful in an intervention context. For example, older adults living in high-crime neighborhoods may be hesitant to engage socially when there are significant barriers related to safety and opportunity.93 Two promising assessment methods include the PROMIS patient-reported outcomes measurement system94 and the Berkman-Syme measure endorsed by the Institute of Medicine.91 Both include social health domains, have established population norms, and can be integrated into electronic medical records in the context of assessing social determinants of health, consistent with Age Friendly Health System95 approaches.
Several of the biological, psychological, and behavioral mechanisms discussed above are potentially modifiable, with evidence-based treatments available. For example, given the availability of several types of pharmacological treatments for regulating serotonin and other monoamines, this may be a modifiable biological target for targeting social disconnection or mitigating risk among socially disconnected older adults. However, preferences of older adults should be considered given that many older patients prefer psychotherapies over medications, and psychotropic medications and polypharmacy come with critical challenges in late life (e.g., increased risk for falls and other adverse events).96 Behavioral interventions may also effectively target behavioral and biological mechanisms, such as evidence-based interventions for depression (e.g., behavioral activation97), substance abuse, and insomnia (e.g., cognitive behavioral therapy for insomnia98), which may mitigate suicide risk, in part by improving social relationships. Psychotherapeutic interventions for suicide risk in later life may also work, in part, by disrupting the pathway from social disconnection to suicide risk via psychological and behavioral mechanisms. Cognitive Reappraisal Intervention for Suicide Prevention (CRISP) targets emotion dysregulation and psychological distress for middle-aged and older adults at risk for suicide.99 Safety Planning is another intervention that holds promise for older adults and can be adapted to emphasize aspects of social connection that are relevant to suicide in later life.100
Interventions to directly target social connection are also available and evidence supporting them is increasing. Such interventions may be implemented at the level of the individual (e.g., increasing social engagement, improving social support, reducing loneliness), the structural level (e.g., addressing social connection as an important outcome within the health care system), and from the perspective of prevention (e.g., teaching patients to maintain healthy relationships).92 Behavioral interventions directly targeting aspects of social connection such as engagement in social activities, improving social skills, and contributing or volunteering can provide opportunities to improve connection and therefore reduce risk for suicide. Though studies have provided evidence that behavioral interventions can reduce loneliness,25 to date it is unclear what behavioral interventions are most effective in later life, which are preferred by older adults (especially those at risk for suicide), and by what mechanisms they work. Many interventions for social connection have not been tested in older adults who report social disconnection and even fewer among those at risk for suicide. The evidence for the effectiveness of any given intervention targeting social connection in late life is modest, with a number of interventions in need of standardized protocols and replication of efficacy and effectiveness studies to be better established.26-31 Some interventions have shown promise in randomized trials with older adults who report social disconnection. A trial of the Senior Connection, a program in which older adults are matched with volunteer peer companions (available nationwide through the AmeriCorps Senior program), showed greater reduction in perceived burdensomeness, depression, and anxiety (versus care-as-usual), but no effect on feelings of belonging or suicide ideation.101 Psychotherapeutic approaches also hold promise. Behavioral activation modified to target social connection has been shown to increase social interactions and support and decrease loneliness among homebound older adults 102,103 and Engage psychotherapy for depression in later life104 was shown to be especially effective for depression when social engagement was addressed.105 Engage has also been adapted to focus specifically on increasing social engagement to reduce suicide risk in later life.105
Digital technologies hold promise as an intervention modality. Internet-based and app-based interventions show some effect on prevention and intervention for suicide-related thoughts and behaviors.106,107 Among older adults, digital modalities such as specialized software systems (e.g., PRISM) have shown some promise for improving social connection in late life.108 Automated digital modalities may be used to coach older adults on social skills; further trials are needed to accurately determine the effectiveness of this type of program.109 Emotion regulation interventions may also be effectively implemented via technology, such as through cell phone or tablet applications; the VA offers a number of mental health apps, with research being conducted with older adults on feasibility and educational materials to encourage use.110,111 However, digital modalities present with design challenges that can make them more difficult to implement in late life, including limits in technological knowledge, hesitancy to engage with technology, and subpopulations (e.g., lower socioeconomic strata) with limited access to technology or needed internet services.112 When newer or more complex technologies are unfamiliar to older adults, lack of technology efficacy can be a barrier.113,114 However, when provided with technologies that are perceived as valuable and easy to use, or offered training in using them, older adults express willingness to engage with them.114 Finally, though older adults tend to exhibit lower rates of use of computers, internet, and smartphones than younger adults, Pew Research showed in 2017 that approximately two-thirds of older adults used the internet, and over 40% owned smartphones; these numbers are likely increasing with time and demonstrate that a significant portion of the older population does have access to and utilizes digital technologies.115 More research in this area can identify the utility and effectiveness of digital interventions to improve social connections and reduce suicide risk among older adults. Importantly, for digital solutions to be effective, devices must be designed using a user-centered approach. Other recent research has begun to study identification of suicide risk via analysis of digital data such as social media posts and search engine inputs; little has been published yet on this in regard to older adults, but this line of research represents another opportunity to study identification of social disconnection and suicide risk in this population.
Gaps in knowledge & future directions
Challenges to developing and testing social connection interventions for suicide prevention among older adults include determining how effectively such interventions reduce suicide risk (largely unknown at this time), and engaging the most socially disconnected older adults in interventions and research studies, given that these older adults may have little to no interaction with formal mental health services, aging services, or social services. Partnering with organizations or systems that are more likely to make contact with these individuals, such as home-delivered meal services, visiting nurses, other home care services, primary care providers, etc. may allow greater access to those most at risk as well as better scalability for effective interventions. Another challenge is that social disconnection has numerous dimensions and causes, raising the possibility that individualized intervention strategies may be needed (or preferred) by older adults. One hypothesis is that the most effective intervention strategy will engage the target(s) most relevant to the individual, and therefore an evidence base of interventions that engage a variety of targets, accompanied by assessment approaches to determine the most appropriate target, may provide an effective approach. However, this individualized approach may be resource-intensive and could incur challenges in scalability. Research is needed to examine the relative costs and benefits of personalized strategies. Additional challenges for improving social connection given that this intervention target is not a mental health condition include identifying optimal settings and interventionists (e.g., social workers, care managers, nurses in primary care, community health workers, peers), selecting the mode of delivery (e.g., individual or group sessions, in person, or via digital technology), as well as optimal dose to increase connection and reduce suicide risk (e.g., number of sessions, over how much time).
The COVID-19 pandemic and need for physical distancing has increased the saliency of remote and/or digital interventions. The comparative effectiveness of in-person social connection and suicide interventions versus virtual/remote interventions is an area for future study and will require attention to digital health literacy, access to technology (including for socioeconomically disadvantaged groups), protection of privacy and data security, as well as preferences of older adults. Older adult-friendly technologies are available, including cell phones and tablets designed specifically for older adults, social robots/robotic pets, and artificial intelligence (AI) devices, though there is little scientific research on the use of these technologies for promoting mental health.
Synthesis and Future Directions
Figure 1 provides a simplified visual representation of the variety of mechanisms and potential intervention targets (some more established, others hypothesized) that we have discussed and related types of interventions that may engage these targets. This model could generate research questions to advance the science of social connections and suicide risk in later life. We posit that social disconnection of a variety of types – including structural, functional, and quality – leads to increased suicide risk via biological (e.g., impairments in neurocognitive functioning, chronic inflammation) and behavioral mechanisms (e.g., increased risky behaviors, decreased engagement in positive activities), which each increase suicide risk directly and/or by increasing psychological distress. Prevention and intervention efforts could target any of these mechanisms, depending upon individual and contextual factors and the need to prevent social disconnection versus reducing risk among those already experiencing social disconnection or suicide-related thoughts and behaviors. Interventions can directly target social connection (e.g., peer companionship or increasing social activities); mitigate some of the biological effects of social disconnection (e.g., medications treating the corollaries of HPA axis activation or chronic inflammation or targeting monoamines); address behavioral mechanisms (e.g., reduction of risky behaviors, treating sleep problems, improving problem solving and decision making, or behavioral activation to increase pleasant activities); or mitigate psychological distress (e.g., psychotherapies to reduce depression, implementation of emotion regulation strategies). The creative and novel research described in this report has highlighted a number of areas in which more scientific study can help to clarify etiological trajectories and establish effectiveness of interventions.
Considerations to shape the development of research questions are outlined in Table 1 and include the necessity of considering cultural contexts and recruitment of all populations of older adults at risk. In the U.S., older white men exhibit the highest rates of suicide. However, older men are often underrepresented in research studies on these topics, and may be more difficult to engage and retain in interventions.116 Other contextual factors such as current events (e.g., the COVID-19 pandemic) and individual circumstances (e.g., level of functioning, comorbidities) may greatly affect findings and intervention strategies. Greater consistency in the conceptualization, definition, and assessment of social connection is necessary for the integration of findings across studies. Older adults themselves may define these constructs in idiographic ways; the terms “lonely” or “isolated” may hold different meanings and connotations for each individual. The development of measures that include and differentiate between multiple components of social connection may provide more accurate and representative conceptualizations of older adults’ social needs. Measures developed to be responsive to the unique needs of older adults and with age-specific norms or clinically-meaningful cut scores are needed to identify older adults at elevated risk and measure response to intervention.
Table 1.
Important considerations and future research directions
Contextual/Cultural Factors
|
Measurement & Definitions of Social
Disconnection
|
Individualization
|
Intervention Modality
|
Transdisciplinary/Convergence
Science
|
Social disconnection has numerous dimensions, which suggests tailored intervention strategies may be useful; however, tailored treatment strategies are resource-intensive and their potential incremental benefit should be studied. Costs and benefits of various settings and modalities for interventions, including digital technology, should also be studied given potential implications for acceptability, feasibility, accessibility, scalability of interventions. For example, a large proportion of older adults who die by suicide are in contact with a primary care physician within the prior year or prior month;117 assessment of social connection and implementation of simple interventions or referral for intervention may have significant impact in a primary care setting.
Finally, research that considers mechanisms at multiple levels of analysis could advance the science of social connection and suicide risk, in line with NIMH’s RDoC strategy that emphasizes research on domains (including social processes) from multiple levels, from genetic influences to neural circuits to behavior and self-reported symptoms and experiences.34 Such study designs may generate testable hypotheses that result in actionable next steps to promote more rapid progression of basic science on social connection to intervention efficacy, to dissemination and implementation of suicide risk interventions at scale.
Highlights.
We present a synthesis of research discussed during an NIMH workshop on mechanisms, treatment targets, and interventions related to social disconnection and late-life suicide.
Social disconnection is related to suicide risk in late life via biological, behavioral, and psychological mechanisms. Social connection is amenable to change, and there are several promising interventions that may target various mechanisms in the association between social disconnection and suicide, as well as social disconnection itself.
More research is needed in this area, and we outline several important considerations for future research.
Acknowledgments
We would like to acknowledge and thank Elizabeth Necka, PhD, and Jovier Evans, PhD, at NIMH for organizing this workshop. This paper does not reflect the opinions or views of the United States Government or the National Institute of Mental Health.
Conflicts of Interest and Source of Funding:
J. Lutz was supported by funding from the National Institute of Mental Health (T32 MH20061, PI: Conwell). K.A. Van Orden and Y. Conwell were supported by the National Institute on Aging (P30AG064103, Heffner, Van Orden, MPI). M.L. Bruce was supported by funding from the AARP Foundation.
Appendix
a Members listed in alphabetical order within categories. Chairs: Martha L. Bruce, PhD, MPH, Yeates Conwell, MD. Presenters: Patricia Areán, PhD, Amy Byers, PhD, MPH, Laura Carstensen, PhD, Alexandre Dombrovski, MD, Nancy Donovan, MD, Amy Fiske, PhD, Josh Gordon, MD, PhD, Julianne Holt-Lunstad, PhD, Dimitris Kiosses, PhD, Sarah Hollingsworth Lisanby, MD, Maria A. Oquendo, MD, PhD, Carla Perissinotto, MD, MHS, Robert Joseph Taylor, PhD, Kimberly A. Van Orden, PhD. Moderators/Panelists: George Alexopoulos, MD, Eric D. Caine, MD, Vonetta Dotson, PhD, Jane Pearson, PhD, Charles F. Reynolds III, MD, Jo Anne Sirey, PhD, Barbara Stanley, PhD. Discussants: Lisa Barry, PhD, MPH, Emmy Betz, MD, Lisa Brenner, PhD, Sara Czaja, PhD, XinQi Dong, MD, MPH, Paul Duberstein, PhD, Daniel Jiminez, PhD, Julie Lutz, PhD, Paul Maciejewski, PhD, Briana Mezuk, PhD, Sean Mitchell, PhD, Ann W. Nguyen, PhD, Olivia I. Okereke, MD, MS, Wilfred R. Pigeon, PhD, Holly Prigerson, PhD, Patrick Raue, PhD, Jerry Reed, PhD, MSW, Timothy Schmutte, PsyD, Caroline Silva, PhD, Katalin Szanto, MD, Harry Owen Taylor, PhD, Sara Weisenbach, PhD.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Julie Lutz, Center for the Study and Prevention of Suicide, Department of Psychiatry, University of Rochester Medical Center.
Kimberly A. Van Orden, Center for the Study and Prevention of Suicide, Department of Psychiatry, University of Rochester Medical Center.
Martha L. Bruce, Department of Psychiatry, Geisel School of Medicine, Dartmouth.
Yeates Conwell, Center for the Study and Prevention of Suicide, Department of Psychiatry, University of Rochester Medical Center.
References
- 1.U.S. Department of Health and Human Services. A Profile of Older Americans: 2010. Administration on Aging, U.S. Department of Health and Human Services;2010. [Google Scholar]
- 2.Anderson LA, Goodman RA, Holtzman D, Posner SF, Northridge ME. Aging in the United States: opportunities and challenges for public health. Am J Public Health. 2012;102(3):393–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention NCfIPaC. Web-based Injury Statistics Query and Reporting System (WISQARS). https://www.cdc.gov/injury/wisqars/index.html. Published 2021. Accessed.
- 4.World Health Organization. Preventing suicide: A global imperative. 2014.
- 5.Crosby AE, Ortega L, Melanson C. Self-directed violence surveillance: Uniform definitions and recommended data elements. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, Division of Violence Prevention;2011. [Google Scholar]
- 6.Posner K, Brown GK, Stanley B, et al. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168(12):1266–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Turecki G, Brent DA. Suicide and suicidal behaviour. The Lancet. 2016;387(10024):1227–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Klonsky ED, May AM, Saffer BY. Suicide, Suicide Attempts, and Suicidal Ideation. Annu Rev Clin Psychol. 2016;12:307–330. [DOI] [PubMed] [Google Scholar]
- 9.Holt-Lunstad J, Robles TF, Sbarra DA. Advancing social connection as a public health priority in the United States. Am Psychol. 2017;72(6):517–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Charles ST, Carstensen LL. Social and emotional aging. Annu Rev Psychol. 2010;61:383–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bruce LD, Wu JS, Lustig SL, Russell DW, Nemecek DA. Loneliness in the United States: A 2018 National Panel Survey of Demographic, Structural, Cognitive, and Behavioral Characteristics. Am J Health Promot. 2019;33(8):1123–1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pikhartova J, Bowling A, Victor C. Is loneliness in later life a self-fulfilling prophecy? Aging Ment Health. 2016;20(5):543–549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Qualter P, Vanhalst J, Harris R, et al. Loneliness across the life span. Perspect Psychol Sci. 2015;10(2):250–264. [DOI] [PubMed] [Google Scholar]
- 14.National Academies of Sciences Engineering and Medicine. Social isolation and loneliness in older adults: Opportunities for the health care system. Washington, DC: The National Academies Press; 2020. [PubMed] [Google Scholar]
- 15.Calati R, Ferrari C, Brittner M, et al. Suicidal thoughts and behaviors and social isolation: A narrative review of the literature. J Affect Disord. 2019;245:653–667. [DOI] [PubMed] [Google Scholar]
- 16.Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE Jr. The interpersonal theory of suicide. Psychol Rev. 2010;117(2):575–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Durkheim E. Suicide: A study in sociology. London: Routledge & K. Paul; 1952. [Google Scholar]
- 18.Klonsky ED, May AM. The Three-Step Theory (3ST): A New Theory of Suicide Rooted in the “Ideation-to-Action” Framework. International Journal of Cognitive Therapy. 2015;8(2):114–129. [Google Scholar]
- 19.O’Connor RC, Kirtley OJ. The integrated motivational-volitional model of suicidal behaviour. Philos Trans R Soc Lond B Biol Sci. 2018;373(1754). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tsai AC, Lucas M, Sania A, Kim D, Kawachi I. Social integration and suicide mortality among men: 24-year cohort study of U.S. health professionals. Ann Intern Med. 2014;161(2):85–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tsai AC, Lucas M, Kawachi I. Association Between Social Integration and Suicide Among Women in the United States. JAMA Psychiatry. 2015;72(10):987–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fassberg MM, van Orden KA, Duberstein P, et al. A systematic review of social factors and suicidal behavior in older adulthood. Int J Environ Res Public Health. 2012;9(3):722–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Szanto K, Dombrovski AY, Sahakian BJ, et al. Social emotion recognition, social functioning, and attempted suicide in late-life depression. Am J Geriatr Psychiatry. 2012;20(3):257–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7(7):e1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Masi CM, Chen HY, Hawkley LC, Cacioppo JT. A meta-analysis of interventions to reduce loneliness. Pers Soc Psychol Rev. 2011;15(3):219–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Findlay RA. Interventions to reduce social isolation amongst older people: where is the evidence? Ageing and Society. 2003;23(5):647–658. [Google Scholar]
- 27.Hagan R, Manktelow R, Taylor BJ, Mallett J. Reducing loneliness amongst older people: a systematic search and narrative review. Aging Ment Health. 2014;18(6):683–693. [DOI] [PubMed] [Google Scholar]
- 28.Cohen-Mansfield J, Perach R. Interventions for alleviating loneliness among older persons: a critical review. Am J Health Promot. 2015;29(3):e109–125. [DOI] [PubMed] [Google Scholar]
- 29.Cattan M, White M, Bond J, Learmouth A. Preventing social isolation and loneliness among older people: a systematic review of health promotion interventions. Ageing and Society. 2005;25(01):41–67. [DOI] [PubMed] [Google Scholar]
- 30.Dickens AP, Richards SH, Greaves CJ, Campbell JL. Interventions targeting social isolation in older people: a systematic review. BMC Public Health. 2011;11:647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.O’Rourke HM, Collins L, Sidani S. Interventions to address social connectedness and loneliness for older adults: a scoping review. BMC Geriatr. 2018;18(1):214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Insel T, Cuthbert B, Garvey M, et al. Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. Am J Psychiatry. 2010;167(7):748–751. [DOI] [PubMed] [Google Scholar]
- 33.Cuthbert BN, Insel TR. Toward the future of psychiatric diagnosis: the seven pillars of RDoC. BMC Med. 2013;11:126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Morris SE, Cuthbert B. Research Domain Criteria: cognitive systems, neural circuits, and dimensions of behavior. Dialogues Clin Neurosci. 2012;14:29–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Glenn CR, Kleiman EM, Cha CB, Deming CA, Franklin JC, Nock MK. Understanding suicide risk within the Research Domain Criteria (RDoC) framework: A meta-analytic review. Depress Anxiety. 2018;35(1):65–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lewandowski KE, Ongur D, Keshavan MS. Development of novel behavioral interventions in an experimental therapeutics world: Challenges, and directions for the future. Schizophr Res. 2018;192:6–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tomova L, Wang K, Thompson T, et al. The need to connect: Acute social isolation causes neural craving responses similar to hunger. bioRxiv. 2020. [Google Scholar]
- 38.Eisenberger NI. The neural bases of social pain: evidence for shared representations with physical pain. Psychosom Med. 2012;74(2):126–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Coan JA, Sbarra DA. Social Baseline Theory: The Social Regulation of Risk and Effort. Curr Opin Psychol. 2015;1:87–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Leschak CJ, Eisenberger NI. Two Distinct Immune Pathways Linking Social Relationships With Health: Inflammatory and Antiviral Processes. Psychosom Med. 2019;81(8):711–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Leonard BE. Inflammation and depression: a causal or coincidental link to the pathophysiology? Acta Neuropsychiatr. 2018;30(1):1–16. [DOI] [PubMed] [Google Scholar]
- 42.Lee CH, Giuliani F. The Role of Inflammation in Depression and Fatigue. Front Immunol. 2019;10:1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Parris MS, Grunebaum MF, Galfalvy HC, et al. Attempted suicide and oxytocin-related gene polymorphisms. J Affect Disord. 2018;238:62–68. [DOI] [PubMed] [Google Scholar]
- 44.Chu C, Hammock EAD, Joiner TE. Unextracted plasma oxytocin levels decrease following in-laboratory social exclusion in young adults with a suicide attempt history. J Psychiatr Res. 2020;121:173–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bibancos T, Jardim DL, Aneas I, Chiavegatto S. Social isolation and expression of serotonergic neurotransmission-related genes in several brain areas of male mice. Genes Brain Behav. 2007;6(6):529–539. [DOI] [PubMed] [Google Scholar]
- 46.Shams S, Chatterjee D, Gerlai R. Chronic social isolation affects thigmotaxis and whole-brain serotonin levels in adult zebrafish. Behav Brain Res. 2015;292:283–287. [DOI] [PubMed] [Google Scholar]
- 47.Oliver DK, Intson K, Sargin D, et al. Chronic social isolation exerts opposing sex-specific consequences on serotonin neuronal excitability and behaviour. Neuropharmacology. 2020; 168:108015. [DOI] [PubMed] [Google Scholar]
- 48.Shams S, Amlani S, Buske C, Chatterjee D, Gerlai R. Developmental social isolation affects adult behavior, social interaction, and dopamine metabolite levels in zebrafish. Dev Psychobiol. 2018;60(1):43–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Serra M, Sanna E, Mostallino MC, Biggio G. Social isolation stress and neuroactive steroids. Eur Neuropsychopharmacol. 2007;17(1):1–11. [DOI] [PubMed] [Google Scholar]
- 50.Stafford M, Gardner M, Kumari M, Kuh D, Ben-Shlomo Y. Social isolation and diurnal cortisol patterns in an ageing cohort. Psychoneuroendocrinology. 2013;38(11):2737–2745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Grant N, Hamer M, Steptoe A. Social isolation and stress-related cardiovascular, lipid, and cortisol responses. Ann Behav Med. 2009;37(1):29–37. [DOI] [PubMed] [Google Scholar]
- 52.Oquendo MA, Sullivan GM, Sudol K, et al. Toward a biosignature for suicide. Am J Psychiatry. 2014;171(12):1259–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Holmén K, Ericsson K, Winblad B. Social and emotional loneliness among non-demented and demented elderly people. Archives of Gerontology and Geriatrics. 2000;31(3):177–192. [DOI] [PubMed] [Google Scholar]
- 54.Desmarais P, Lanctot KL, Masellis M, Black SE, Herrmann N. Social inappropriateness in neurodegenerative disorders. Int Psychogeriatr. 2018;30(2):197–207. [DOI] [PubMed] [Google Scholar]
- 55.Biddle KD, d’Oleire Uquillas F, Jacobs HIL, et al. Social Engagement and Amyloid-beta-Related Cognitive Decline in Cognitively Normal Older Adults. Am J Geriatr Psychiatry. 2019;27(11):1247–1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Donovan NJ, Okereke OI, Vannini P, et al. Association of Higher Cortical Amyloid Burden With Loneliness in Cognitively Normal Older Adults. JAMA Psychiatry. 2016;73(12):1230–1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.d’Oleire Uquillas F, Jacobs HIL, Biddle KD, et al. Regional tau pathology and loneliness in cognitively normal older adults. Transl Psychiatry. 2018;8(1):282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Serafini G, Calcagno P, Lester D, Girardi P, Amore M, Pompili M. Suicide Risk in Alzheimer’s Disease: A Systematic Review. Curr Alzheimer Res. 2016;13(10):1083–1099. [DOI] [PubMed] [Google Scholar]
- 59.Haw C, Harwood D, Hawton K. Dementia and suicidal behavior: a review of the literature. Int Psychogeriatr. 2009;21(3):440–453. [DOI] [PubMed] [Google Scholar]
- 60.Tu YA, Chen MH, Tsai CF, et al. Geriatric Suicide Attempt and Risk of Subsequent Dementia: A Nationwide Longitudinal Follow-up Study in Taiwan. Am J Geriatr Psychiatry. 2016;24(12):1211–1218. [DOI] [PubMed] [Google Scholar]
- 61.Saffer BY, Klonsky ED. The Relationship of Self-reported Executive Functioning to Suicide Ideation and Attempts: Findings from a Large U.S.-based Online Sample. Arch Suicide Res. 2017;21(4):577–594. [DOI] [PubMed] [Google Scholar]
- 62.Gujral S, Dombrovski AY, Butters M, Clark L, Reynolds CF 3rd, Szanto K. Impaired Executive Function in Contemplated and Attempted Suicide in Late Life. Am J Geriatr Psychiatry. 2014;22(8):811–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kobayashi LC, Steptoe A. Social Isolation, Loneliness, and Health Behaviors at Older Ages: Longitudinal Cohort Study. Ann Behav Med. 2018;52(7):582–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ingram I, Kelly PJ, Deane FP, et al. Loneliness among people with substance use problems: A narrative systematic review. Drug Alcohol Rev. 2020;39(5):447–483. [DOI] [PubMed] [Google Scholar]
- 65.Griffin SC, Williams AB, Mladen SN, Perrin PB, Dzierzewski JM, Rybarczyk BD. Reciprocal Effects Between Loneliness and Sleep Disturbance in Older Americans. J Aging Health. 2019:898264319894486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Shankar A. Loneliness and sleep in older adults. Soc Psychiatry Psychiatr Epidemiol. 2020;55(2):269–272. [DOI] [PubMed] [Google Scholar]
- 67.Bohnert KM, Ilgen MA, Louzon S, McCarthy JF, Katz IR. Substance use disorders and the risk of suicide mortality among men and women in the US Veterans Health Administration. Addiction. 2017;112(7):1193–1201. [DOI] [PubMed] [Google Scholar]
- 68.Bernert RA, Nadorff MR. Sleep Disturbances and Suicide Risk. Sleep Med Clin. 2015;10(1):35–39. [DOI] [PubMed] [Google Scholar]
- 69.Fiske A, Wetherell JL, Gatz M. Depression in older adults. Annu Rev Clin Psychol. 2009;5:363–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bamonti PM, Fiske A. Engaging in pleasant events explains the relation between physical disability and mental health outcomes in older adults. Aging Ment Health. 2019:1–9. [DOI] [PubMed] [Google Scholar]
- 71.Baltes P. On the incomplete architecture of human ontology: selection, optimization, and compensation as foundation of developmental theory. Am Psychol. 1997;52(4):366–380. [DOI] [PubMed] [Google Scholar]
- 72.Heckhausen J, Wrosch C, Schulz R. A motivational theory of life-span development. Psychol Rev. 2010;117(1):32–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Fiske A, Bamonti PM, Nadorff MR, Petts RA, Sperry JA. Control strategies and suicidal ideation in older primary care patients with functional limitations. Int J Psychiatry Med. 2013;46(3):271–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Matire LM, Stephens MAP, Druley JA, Wojno WC. Negative reactions to received spousal care: Predictors and consequences of miscarried support. Health Psychology. 2002;21(2):167–176. [PubMed] [Google Scholar]
- 75.Vanyukov PM, Hallquist MN, Delgado M, Szanto K, Dombrovski AY. Neurocomputational mechanisms of adaptive learning in social exchanges. Cogn Affect Behav Neurosci. 2019;19(4):985–997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Dombrovski AY, Hallquist MN, Brown VM, Wilson J, Szanto K. Value-Based Choice, Contingency Learning, and Suicidal Behavior in Mid- and Late-Life Depression. Biol Psychiatry. 2019;85(6):506–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Clark L, Dombrovski AY, Siegle GJ, et al. Impairment in risk-sensitive decision-making in older suicide attempters with depression. Psychol Aging. 2011;26(2):321–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Brown VM, Wilson J, Hallquist MN, Szanto K, Dombrovski AY. Ventromedial prefrontal value signals and functional connectivity during decision-making in suicidal behavior and impulsivity. Neuropsychopharmacology. 2020;45(6):1034–1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Dombrovski AY, Szanto K, Clark L, Reynolds CF, Siegle GJ. Reward signals, attempted suicide, and impulsivity in late-life depression. JAMA Psychiatry. 2013;70(10):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Vanyukov PM, Szanto K, Hallquist MN, et al. Paralimbic and lateral prefrontal encoding of reward value during intertemporal choice in attempted suicide. Psychol Med. 2016;46(2):381–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Dombrovski AY, Szanto K, Siegle GJ, et al. Lethal forethought: delayed reward discounting differentiates high- and low-lethality suicide attempts in old age. Biol Psychiatry. 2011;70(2):138–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tsypes A, Szanto K, Bridge J, Brown VM, Keilp J, Dombrovski A. Delay discounting in suicidal behavior: Myopic preference or inconsistent valuation? PsyArXiv. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.English T, Carstensen LL. Selective Narrowing of Social Networks Across Adulthood is Associated With Improved Emotional Experience in Daily Life. Int J Behav Dev. 2014;38(2):195–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Fingerman KL, Huo M, Charles ST, Umberson DJ. Variety Is the Spice of Late Life: Social Integration and Daily Activity. J Gerontol B Psychol Sci Soc Sci. 2020;75(2):377–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Conwell Y, Van Orden K, Caine ED. Suicide in older adults. Psychiatr Clin North Am. 2011;34(2):451–468, ix. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chatters LM, Taylor RJ, Woodward AT, Nicklett EJ. Social support from church and family members and depressive symptoms among older African Americans. Am J Geriatr Psychiatry. 2015;23(6):559–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Taylor HO, Taylor RJ, Nguyen AW, Chatters L. Social Isolation, Depression, and Psychological Distress Among Older Adults. J Aging Health. 2018;30(2):229–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Millner AJ, Robinaugh DJ, Nock MK. Advancing the Understanding of Suicide: The Need for Formal Theory and Rigorous Descriptive Research. Trends Cogn Sci. 2020;24(9):704–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Morin RT, Li Y, Mackin RS, Whooley MA, Conwell Y, Byers AL. Comorbidity Profiles Identified in Older Primary Care Patients Who Attempt Suicide. J Am Geriatr Soc. 2019;67(12):2553–2559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Barry LC, Steffens DC, Covinsky KE, Conwell Y, Li Y, Byers AL. Increased Risk of Suicide Attempts and Unintended Death Among Those Transitioning From Prison to Community in Later Life. Am J Geriatr Psychiatry. 2018;26(11):1165–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Institute of Medicine. Capturing social and behavioral domains and measures in electronic health records: Phase 2. Washington, DC: The National Academies Press; 2014. [PubMed] [Google Scholar]
- 92.Perissinotto C, Holt-Lunstad J, Periyakoil VS, Covinsky K. A Practical Approach to Assessing and Mitigating Loneliness and Isolation in Older Adults. J Am Geriatr Soc. 2019;67(4):657–662. [DOI] [PubMed] [Google Scholar]
- 93.Portacolone E, Perissinotto C, Yeh JC, Greysen SR. “I Feel Trapped”: The Tension Between Personal and Structural Factors of Social Isolation and the Desire for Social Integration Among Older Residents of a High-Crime Neighborhood. Gerontologist. 2018;58(1):79–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Cook KF, Jensen SE, Schalet BD, et al. PROMIS measures of pain, fatigue, negative affect, physical function, and social function demonstrated clinical validity across a range of chronic conditions. J Clin Epidemiol. 2016;73:89–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Institute for Healthcare Improvement. Age-Friendly Health Systems. http://www.ihi.org/Engage/Initiatives/Age-Friendly-Health-Systems/Pages/default.aspx. Accessed January 15, 2021. [Google Scholar]
- 96.Hartikainen S, Lonnroos E, Louhivuori K. Medication as a risk factor for falls: critical systematic review. J Gerontol A Biol Sci Med Sci. 2007;62(10):1172–1181. [DOI] [PubMed] [Google Scholar]
- 97.Polenick CA, Flora SR. Behavioral activation for depression in older adults: theoretical and practical considerations. Behav Anal. 2013;36(1):35–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Sadler P, McLaren S, Klein B, Harvey J, Jenkins M. Cognitive behavior therapy for older adults with insomnia and depression: a randomized controlled trial in community mental health services. Sleep. 2018;41(8). [DOI] [PubMed] [Google Scholar]
- 99.Kiosses DN, Alexopoulos GS, Hajcak G, et al. Cognitive Reappraisal Intervention for Suicide Prevention (CRISP) for Middle-Aged and Older Adults Hospitalized for Suicidality. Am J Geriatr Psychiatry. 2018;26(4):494–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Conti EC, Jahn DR, Simons KV, et al. Safety Planning to Manage Suicide Risk with Older Adults: Case Examples and Recommendations. Clin Gerontol. 2020;43(1):104–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Conwell Y, Van Orden KA, Stone DM, et al. Peer Companionship for Mental Health of Older Adults in Primary Care: A Pragmatic, Nonblinded, Parallel-Group, Randomized Controlled Trial. Am J Geriatr Psychiatry. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Choi NG, Pepin R, Marti CN, Stevens CJ, Bruce ML. Improving Social Connectedness for Homebound Older Adults: Randomized Controlled Trial of Tele-Delivered Behavioral Activation Versus Tele-Delivered Friendly Visits. Am J Geriatr Psychiatry. 2020;28(7):698–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Pepin R, Stevens CJ, Choi NG, Feeney SM, Bruce ML. Modifying Behavioral Activation to Reduce Social Isolation and Loneliness Among Older Adults. Am J Geriatr Psychiatry. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Alexopoulos GS, Arean P. A model for streamlining psychotherapy in the RDoC era: the example of ‘Engage’. Mol Psychiatry. 2014;19(1):14–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Solomonov N, Bress JN, Sirey JA, et al. Engagement in Socially and Interpersonally Rewarding Activities as a Predictor of Outcome in “Engage” Behavioral Activation Therapy for Late-Life Depression. Am J Geriatr Psychiatry. 2019;27(6):571–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Buscher R, Torok M, Terhorst Y, Sander L. Internet-Based Cognitive Behavioral Therapy to Reduce Suicidal Ideation: A Systematic Review and Meta-analysis. JAMA Netw Open. 2020;3(4):e203933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Torok M, Han J, Baker S, et al. Suicide prevention using self-guided digital interventions: a systematic review and meta-analysis of randomised controlled trials. The Lancet Digital Health. 2020;2(1):e25–e36. [DOI] [PubMed] [Google Scholar]
- 108.Czaja SJ, Boot WR, Charness N, Rogers WA, Sharit J. Improving Social Support for Older Adults Through Technology: Findings From the PRISM Randomized Controlled Trial. Gerontologist. 2018;58(3):467–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ali R, Hoque E, Duberstein P, et al. Aging and Engaging: A Pilot Randomized Controlled Trial of an Online Conversational Skills Coach for Older Adults. The American Journal of Geriatric Psychiatry. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Gould CE, Kok BC, Ma VK, Zapata AML, Owen JE, Kuhn E. Veterans Affairs and the Department of Defense mental health apps: A systematic literature review. Psychol Serv. 2019;16(2):196–207. [DOI] [PubMed] [Google Scholar]
- 111.Gould CE, Loup JR, Scales AN, et al. Development and refinement of educational materials to help older veterans use VA mental health mobile apps. Professional Psychology: Research and Practice. 2020;51(4):414–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Andrews JA, Brown LJ, Hawley MS, Astell AJ. Older Adults’ Perspectives on Using Digital Technology to Maintain Good Mental Health: Interactive Group Study. J Med Internet Res. 2019;21(2):e11694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Olson KE, O’Brien MA, Rogers WA, Charness N. Diffusion of Technology: Frequency of Use for Younger and Older Adults. Ageing Int. 2011;36(1):123–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Betts LR, Hill R, Gardner SE. “There’s Not Enough Knowledge Out There”: Examining Older Adults’ Perceptions of Digital Technology Use and Digital Inclusion Classes. J Appl Gerontol. 2019;38(8):1147–1166. [DOI] [PubMed] [Google Scholar]
- 115.Anderson M, Perrin A. Tech adoption climbs among older adults. Pew Research Center; May 17, 2017. 2017. [Google Scholar]
- 116.Anderson C, Seff LR, Batra A, Bhatt C, Palmer RC. Recruiting and Engaging Older Men in Evidence-Based Health Promotion Programs: Perspectives on Barriers and Strategies. J Aging Res. 2016;2016:8981435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicideL A review of the evidence. American Journal of Psychiatry. 2002;159:909–916. [DOI] [PMC free article] [PubMed] [Google Scholar]


