Abstract
Background/Aim: Positional uncertainty in spinal stereotactic body radiotherapy (SBRT) may cause fatal error, therefore, we investigated the intra-fractional spinal motion during SBRT and its time dependency. Patients and Methods: Thirty-one patients who received SBRT using CyberKnife were enrolled in the study. 2D kV X-ray spine images in two directions were taken before and during treatment. Image acquisition intervals during treatment were set at 35-60 sec. Automatic image matchings were performed between the reference digital reconstructed radiography (DRR) and live images, and the spinal position displacements were logged in six translational and rotational directions. If the displacements exceeded 2 mm or 1 degree, the treatment beam delivery was interrupted and the patient position was corrected by moving couch, and the couch adjustments were also logged. Based on the information, the time-dependent accumulated translational and rotational displacements without any couch adjustments were calculated. Results: Spinal position displacements in all translational and rotational directions were correlated with elapsed treatment time. Especially, Right-Left displacements of >1 mm and >2 mm were observed at 4-6 and 8-10 min after treatment initiation, respectively. Rotational displacements in the Yaw direction >1˚ were observed at 10-15 min after treatment initiation. Conclusion: The translational and rotational displacements systematically increased with elapsed treatment time. It is suggested that the spine position should be checked at least every 4-6 min or the treatment time should be limited within 4-6 minutes to ensure the irradiation accuracy within the millimeter or submillimeter range.
Keywords: Stereotactic body radiotherapy, spinal metastasis, intrafractional motion, setup margin
Developments in chemotherapy, molecular targeted therapy, and immunotherapy [e.g., programmed death-1 (PD-1)/Programmed death-ligand 1 (PD-L1) inhibitors] have contributed to the prolonged survival of patients with distant metastatic disease. Maintaining the quality of life (QOL) of patients by controlling distant metastatic lesions is an important challenge to address. The spine is one of the most common sites of metastasis, causing pain and negatively impacting QOL. Spinal metastases have been treated using palliative radiotherapy with a dose of 8 Gy in a single fraction or 20-30 Gy in 5-10 fractions using conventional two-dimensional radiotherapy (2DRT) or three-dimensional conformal radiotherapy (3DCRT). Stereotactic body radiotherapy (SBRT) is increasingly being used for oligometastases of the spine. SBRT enables the delivery of high radiation doses to the tumor specifically while minimizing the dose to the surrounding normal tissues, such as the spinal cord, which may provide longer pain relief and better tumor control when compared with conventional radiotherapy (1,2). Moreover, some studies have reported the effectiveness of re-irradiation using SBRT for recurrent spinal metastases after conventional radiotherapy (3).
Intra-fractional motion errors are critical in SBRT for spinal metastases. Therefore, various types of image-guided radiotherapy (IGRT) are performed in parallel to minimize the displacement of a patient’s position during treatment (4,5). Even so, it is difficult to perform real-time correction of a patient’s position during treatment in several treatment devices. The treatment duration of SBRT varies by i) the treatment device, ii) the site of irradiation, and iii) the prescribed dose, but is generally longer than that of a conventional 3DCRT. Regarding the treatment device, several studies on the treatment planning have reported the treatment time of approximately 10 min using TrueBeam (Varian Medical systems, Palo Alto, CA, USA) and 20-30 min using TomoTherapy (Accuray, Inc., Sunnyvale, CA, USA) (6,7). With an increased treatment duration, intra-fractional motion error may occur more frequently during SBRT. Therefore, the time dependent intra-fractional motion of the spine should be accurately assessed.
CyberKnife (Accuray, Inc.) has a room-mounted X-ray imaging system for tracking the spine during treatment, and the system logs the intra-fractional data of the translational and rotational displacements of the spine. In this study, we investigated the intra-fractional spinal motion during SBRT and its time dependency by analyzing the log data.
Patients and Methods
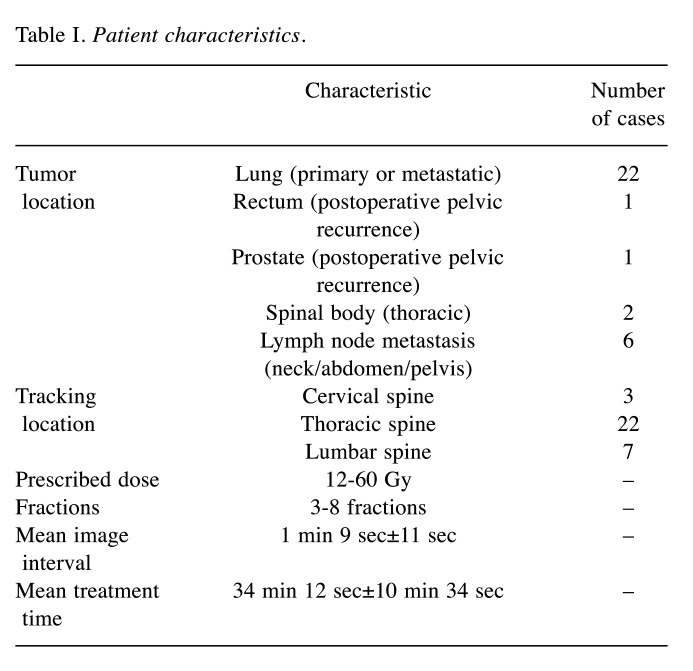
A total of 31 patients (32 plans) who received SBRT using CyberKnife at our hospital from April 2014 to March 2020 were enrolled in this study. Patient characteristics are summarized in Table I. Patients were immobilized using a vacuum bag and a cushion placed under the knees (Figure 1). All treatments were delivered with a real-time tracking system using the spinal body near the tumor as a landmark. Log data from 32 plans conducted as initial treatment were analyzed.
Table I. Patient characteristics.
Figure 1. Patient set-up. Patients were immobilized using patientspecific vacuum bags. Yellow arrows correspond to the direction of spine translations and rotations.
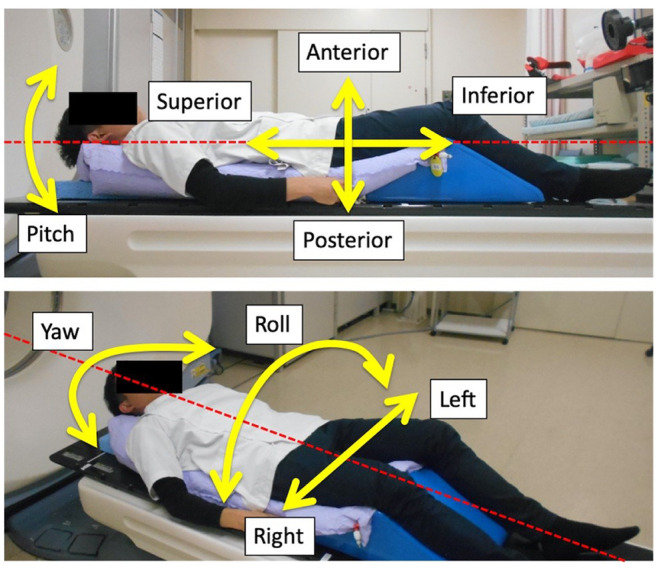
Two-dimensional kV X-ray spine images in two directions were taken before and during SBRT using a room-mounted X-ray imaging system (Accuray, Inc.) associated with the CyberKnife. Image acquisition intervals during treatment were set at 35-60 sec. Since the CyberKnife system did not allow imaging during treatment beam delivery, images were acquired approximately once a minute (Table I). The timestamps of each imaging were logged. Automatic image matching using the spinal body was performed between reference digitally reconstructed radiography (DRR) images and live images using the Xsight Spine Tracking System of CyberKnife. The mismatches between DRR and live images were logged in six translational and rotational directions [Right-Left (R-L), Superior-Inferior (S-I), Anterior-Posterior (A-P), Roll, Pitch, and Yaw] (Figure 1). If the displacements exceeded 2 mm or 1 degree, the treatment beam delivery was interrupted and the patient position was corrected by moving the couch, and the couch adjustments were also logged. Based on the information, the time-dependent accumulation of translational and rotational displacements without couch adjustments were analyzed. Positional displacements were calculated by averaging every 2 minutes for 0-10 minutes and every 5 minutes for 10-20 min. Pearson’s correlation coefficients (r) were used to evaluate correlations between spinal body displacements and elapsed treatment time. Values of p<0.05 were considered statistically significant. This study was approved by the Institutional Review Board of our institute (Approval number: 18-106).
Results
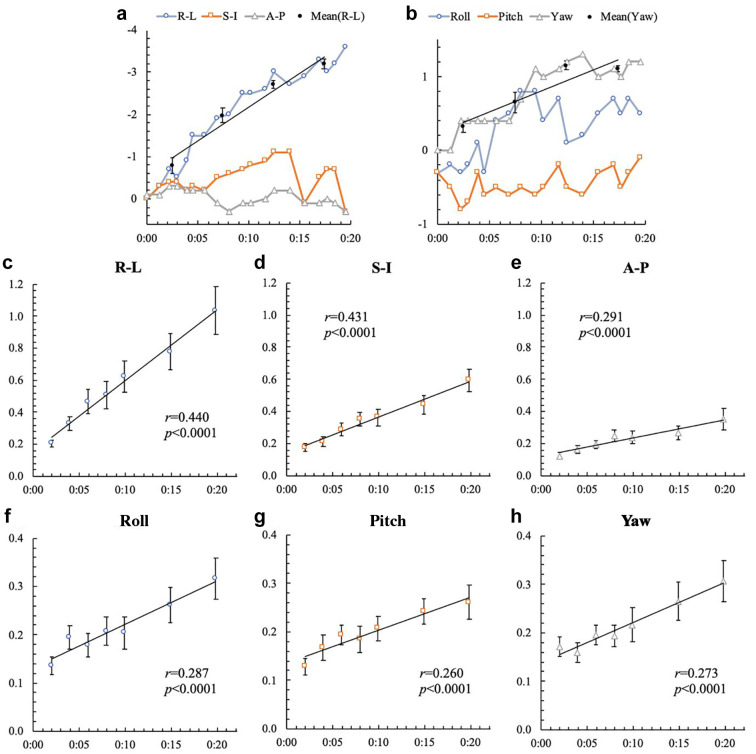
Figures 2a and b show the time-dependent accumulation of the spinal displacements in a case with the biggest movement. Relatively large displacements in the R-L and Yaw directions were observed in this case, and the displacements tended to increase with time. Figures 2c-h show the mean time-dependent accumulation of displacements in all cases. Spinal position displacements in all translational and rotational directions were correlated with elapsed treatment time. In particular, there was a moderate correction (r>0.4) between the R-L and S-I directions. Mean±1 SD maximum translational displacements within 20 min for all patients were 1.3±0.9 mm, 0.8±0.4 mm, and 0.6±0.4 mm in the R-L, S-I, and A-P directions, respectively, and mean±1 SD maximum rotational displacements in the Yaw, Pitch, and Roll directions were 0.6±0.3˚, 0.4±0.2˚, and 0.5±0.3˚, respectively.
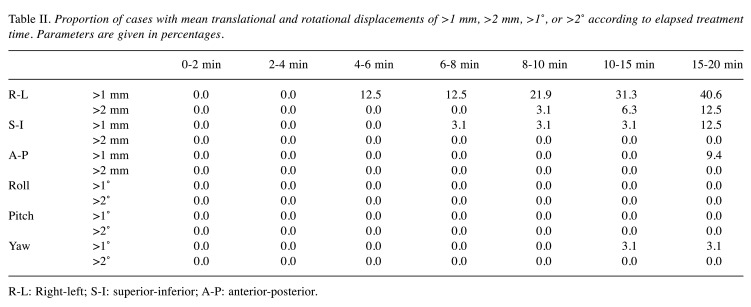
Table II shows the proportion of cases with mean translational and rotational displacements of >1 mm, >2 mm, >1˚, or >2˚ according to the elapsed treatment time. R-L displacements of >1 mm and >2 mm were observed at 4-6 and 8-10 minutes after treatment initiation, respectively. No displacement of >2 mm was observed within 20 min in the S-I and A-P directions. Rotational displacements in the Yaw direction of >1˚ were observed at 10-15 min after treatment initiation.
Table II. Proportion of cases with mean translational and rotational displacements of >1 mm, >2 mm, >1°, or >2° according to elapsed treatment time. Parameters are given in percentages.
R-L: Right-left; S-I: superior-inferior; A-P: anterior-posterior.
Discussion
Some studies evaluated the intra-fractional spinal motion during SBRT using ExacTrac (BrainLab, Heimstetten, Germany) (8) or Cone-Beam CT (9). These studies analyzed the spinal motion from the positional data of pre- and post-SBRT or those of very short period of time during SBRT. Therefore, they did not evaluate the continuous spinal motion during the entire treatment. Murphy et al. (10) and Chuang et al. (11) have measured the intra-fractional motion with the CyberKnife X-ray imaging system, but only analyzed positional displacements between consecutive image acquisitions taken in 1-2 min intervals, rather than the positional displacement over the entire treatment fraction. Although intra-fractional motions of the skull or metal markers have been reported, there is no report on the time-dependent intra-fractional spinal motion in SBRT (12).
Mean translational and rotational displacements were correlated with elapsed treatment time, indicating that the spine was systematically displaced during treatment and this displacement increased with time. Despite this, there was no case in which the maximum rotational displacement exceeded 1˚ within 10 min from the initiation of the treatment. Moreover, the influence of rotational displacement is considered to be limited in spinal SBRT. The reason is that the beam isocenter is set near the center of the target in most situations (12). In contrast, translational displacements, especially in the R-L direction, were relatively large, with displacements of >1 mm at 4-6 min and >2 mm at 8-10 min from the initiation of the treatment in some cases. Hoogeman et al. have recommended patient position matching at least every 5 minutes in order to achieve irradiation accuracy in the millimeter or sub-millimeter range for skull or metal marker tracking (12). Similar findings were obtained in the present study, suggesting the importance of frequent image guidance for spinal SBRT due to the close proximity of organs at risk (OARs), especially the spinal cord.
In SBRT, steep dose distributions are applied to deliver a large dose to the tumor while reducing it to the adjacent OARs (4). Serious adverse events could occur if large doses are delivered to the OARs due to the intra-fractional motion. Therefore, when treating patients with an IGRT device that does not allow for real-time positional correction during irradiation, an appropriate setup margin must be set to account for intra-fractional motion (13). However, expanding the setup margin may cause overlap between the PTV and OARs, making it difficult to irradiate the tumor with a sufficiently large dose. In the present study, increasing intra-fractional motion of the spine was observed as the treatment time elapsed. Therefore, it is required to either shorten the irradiation time or perform frequent image guidance.
This study has several limitations worth noting. First, the sample size was small, thus, we could not assess the influence of differences in tracking sites (cervical, thoracic, or lumbar spine). Depending on the fixation method, the cervical or upper thoracic spine may exhibit more positional displacements due to the curvature. Second, intra-fractional motion may change depending on the condition of the patient. When a patient has severe pain, for instance, the intra-fractional motion may be greater than the patients in the present study. Spinal SBRT sometimes requires the use of analgesics to maintain the patient’s posture during treatment (14).
In summary, both time-dependent translational and rotational displacements were observed in SBRT for spinal metastasis. The results of the present study suggest that spine position may be checked at least every 4-6 min during SBRT or the treatment time should be limited to 4-6 min to ensure the irradiation accuracy within the millimeter or submillimeter range.
Conflicts of Interest
The Authors declare that there are no conflicts of interest.
Authors’ Contributions
All Authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by RH and YO. The first draft of the manuscript was written by RH and all authors commented on previous versions of the manuscript. All Authors read and approved the final manuscript.
Acknowledgements
This study was approved by the Institutional Review Board of Saitama Medical University International Medical Center (Authorization number: 18-106). This was a retrospective study, and thus the requirement for written informed consent was waived.
A part of this study was presented at the 20th Asia-Oceania Congress on Medical Physics (AOCMP).
The Authors thank Jun Teranishi, Tomohito Nakada, Tohru Azami, and Haruka Yoshida (Division of Radiology, Saitama Medical University International Medical Center) for their assistance in data collection.
2. Time-dependent translational and rotational displacements of the spinal body. Graphs a and b show the time-dependent accumulation of the spinal displacements in a case with the biggest movement. Black dots correspond to mean displacements in increments of 5 min in the Right-Left (R-L) and Yaw directions, respectively. Relatively large displacements in the R-L and Yaw directions were observed in this case, and the displacements tended to increase with time. Graphs c-h show results of mean translational and rotational displacements of all cases according to elapsed time (0-10 min in 2-min increments, 10-20 min in 5-min increments). Error bars represent standard errors. R-L: Right-left; S-I: superiorinferior; A-P: anterior-posterior.
References
- 1.Kumar R, Nater A, Hashmi A, Myrehaug S, Lee Y, Ma L, Redmond K, Lo SS, Chang EL, Yee A, Fisher CG, Fehlings MG, Sahgal A. The era of stereotactic body radiotherapy for spinal metastases and the multidisciplinary management of complex cases. Neurooncol Pract. 2016;3(1):48–58. doi: 10.1093/nop/npv022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zeng KL, Tseng CL, Soliman H, Weiss Y, Sahgal A, Myrehaug S. Stereotactic body radiotherapy (SBRT) for oligometastatic spine metastases: an overview. Front Oncol. 2019;9:337. doi: 10.3389/fonc.2019.00337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Myrehaug S, Sahgal A, Hayashi M, Levivier M, Ma L, Martinez R, Paddick I, Régis J, Ryu S, Slotman B, De Salles A. Reirradiation spine stereotactic body radiation therapy for spinal metastases: systematic review. J Neurosurg Spine. 2017;27(4):428–435. doi: 10.3171/2017.2.SPINE16976. [DOI] [PubMed] [Google Scholar]
- 4.Benedict SH, Yenice KM, Followill D, Galvin JM, Hinson W, Kavanagh B, Keall P, Lovelock M, Meeks S, Papiez L, Purdie T, Sadagopan R, Schell MC, Salter B, Schlesinger DJ, Shiu AS, Solberg T, Song DY, Stieber V, Timmerman R, Tomé WA, Verellen D, Wang L, Yin FF. Stereotactic body radiation therapy: the report of AAPM Task Group 101. Med Phys. 2010;37(8):4078–4101. doi: 10.1118/1.3438081. [DOI] [PubMed] [Google Scholar]
- 5.Alaei P, Ding GX. Tennessee: American Association of Physicists in Medicine by Medical Physics Publishing. 2018. Overview of image guidance in radiation therapy. In: Alaei P, Ding GX (eds). Image guidance in radiation therapy: Techniques, accuracy, and limitations. 1st ed; p. pp. 1. [Google Scholar]
- 6.Gallo JJ, Kaufman I, Powell R, Pandya S, Somnay A, Bossenberger T, Ramirez E, Reynolds R, Solberg T, Burmeister J. Single-fraction spine SBRT end-to-end testing on TomoTherapy, Vero, TrueBeam, and CyberKnife treatment platforms using a novel anthropomorphic phantom. J Appl Clin Med Phys. 2015;16(1):5120. doi: 10.1120/jacmp.v16i1.5120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang J, Ma L, Wang XS, Xu WX, Cong XH, Xu SP, Ju ZJ, Du L, Cai BN, Yang J. Dosimetric evaluation of 4 different treatment modalities for curative-intent stereotactic body radiation therapy for isolated thoracic spinal metastases. Med Dosim. 2016;41(2):105–112. doi: 10.1016/j.meddos.2015.10.003. [DOI] [PubMed] [Google Scholar]
- 8.Jin JY, Ryu S, Rock J, Faber K, Chen Q, Ajlouni M, Movsas B. Evaluation of residual patient position variation for spinal radiosurgery using the Novalis image guided system. Med Phys. 2008;35(3):1087–1093. doi: 10.1118/1.2839097. [DOI] [PubMed] [Google Scholar]
- 9.Li W, Sahgal A, Foote M, Millar BA, Jaffray DA, Letourneau D. Impact of immobilization on intrafraction motion for spine stereotactic body radiotherapy using cone beam computed tomography. Int J Radiat Oncol Biol Phys. 2012;84(2):520–526. doi: 10.1016/j.ijrobp.2011.12.039. [DOI] [PubMed] [Google Scholar]
- 10.Murphy MJ, Chang SD, Gibbs IC, Le QT, Hai J, Kim D, Martin DP, Adler JR Jr. Patterns of patient movement during frameless image-guided radiosurgery. Int J Radiat Oncol Biol Phys. 2003;55(5):1400–1408. doi: 10.1016/s0360-3016(02)04597-2. [DOI] [PubMed] [Google Scholar]
- 11.Chuang C, Sahgal A, Lee L, Larson D, Huang K, Petti P, Verhey L, Ma L. Effects of residual target motion for image-tracked spine radiosurgery. Med Phys. 2007;34(11):4484–4490. doi: 10.1118/1.2790587. [DOI] [PubMed] [Google Scholar]
- 12.Hoogeman MS, Nuyttens JJ, Levendag PC, Heijmen BJ. Time dependence of intrafraction patient motion assessed by repeat stereoscopic imaging. Int J Radiat Oncol Biol Phys. 2008;70(2):609–618. doi: 10.1016/j.ijrobp.2007.08.066. [DOI] [PubMed] [Google Scholar]
- 13.Landberg T, Chavaudra J, Dobbs J, Gerard JP, Hanks G, Horiot JC, Johansson KA, Möller T, Purdy J, Suntharalingam N, Svensson H. Bethesda: ICRU Publications. 1999. International Commission on Radiation Units and Measurements (ICRU) report 62, prescribing, recording and reporting photon beam therapy (Supplement to ICRU Report 50) p. pp. 1. [Google Scholar]
- 14.Yang M, Timmerman R. Stereotactic ablative radiotherapy uncertainties: delineation, setup and motion. Semin Radiat Oncol. 2018;28(3):207–217. doi: 10.1016/j.semradonc.2018.02.006. [DOI] [PubMed] [Google Scholar]