Abstract
We present 3 cases reporting the normal appearance of the post COVID-19 vaccination on shoulder MRI exams. All 3 patients were imaged 1 to 5 days post-vaccination for unrelated MSK shoulder symptoms, and none reported any symptoms besides mild shoulder discomfort for a day or 2 following vaccine administration. All 3 patients demonstrated characteristic deltoid edema, quadrilateral space region edema and axillary nodal prominence. Vessel prominence with t2 and t1 increased signal draining to the approximate location of the quadrilateral space and axilla was an associated feature. The normal appearance of the covid-19 vaccine on shoulder MRI has not been previously described, and recognition by the radiologist will prevent erroneous differential diagnosis, unnecessary medical workups, and detract from the clinically relevant pathological imaging findings in patients with shoulder pain.
keywords: COVID-19, MRI, Quadrilateral Space, Vaccination, Shoulder
Introduction
Millions of COVID-19 vaccination doses have already been delivered and administered in the United States [1], most commonly into the belly of the deltoid muscle [2], [3], [4], [5]. The most common reported side effect is pain at the injection site (77.8%) followed by swelling (6.3%) and redness (5.9%), which are typically mild and transient [2]. Serious side effects are very unusual. Unliteral axillary adenopathy (and less commonly cervical adenopathy) has been reported following COVID vaccination, causing a particular diagnostic dilemma for breast radiologists and oncologists [6]. This axillary adenopathy has been estimated to generally resolve in 5 weeks [7]. However, the reported studies are often small studies and generally discuss patients imaged greater than a week following vaccine administration.
Imaging features of the COVID-19 vaccine on shoulder MRI have not been described. We present the imaging appearance of this vaccine injection in 3 patients; all imaged less than 5 days from vaccine administration. Characteristic features may allow the radiologist to diagnose or suggest a vaccine-related inflammatory reaction even in the absence of this relevant history.
Case Report
Case 1
A 21 year-old male with a history of right-sided shoulder pain acquired from old hockey injuries with persistent clicking obtained an MRI of his right shoulder 24 hours after receiving the second dose of his Pfizer-BioNTech Covid-19 vaccination in the right shoulder. The patient reported that 15 hours after his vaccination he noticed swelling anteriorly towards the axilla and some mild swelling of cervical lymph nodes. There was mild tenderness without discoloration. overlying the deltoid injection site. These injection symptoms subsided in two days. See Figure 1 for images and associated findings.
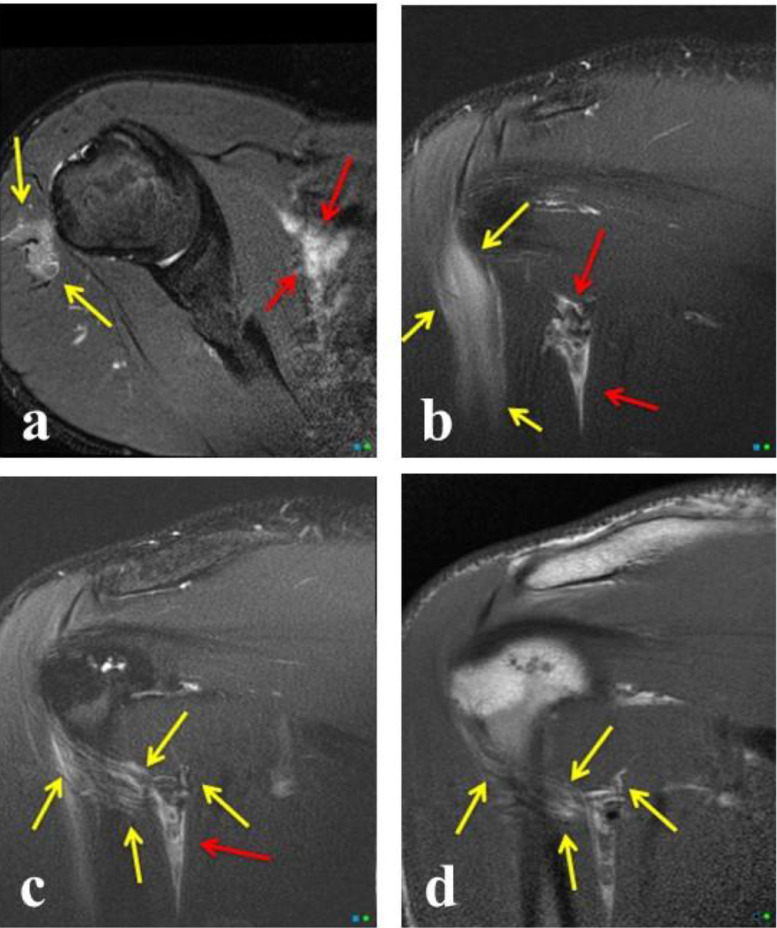
Fig. 1.
Shoulder imaging of a 21 year-old man 24 hours following COVID vaccine injection. (A) Axial PDFS demonstrates edema in the deltoid muscle secondary to the primary injection site (Yellow Arrow); there is also inflammation with mild early adenopathy in the axillary region (Red Arrows). (B) Coronal T2 FS demonstrates edema in the deltoid muscle secondary to the primary injection site (Yellow Arrows); there is inflammation in the approximate location of the quadrilateral space (Red Arrows). (C) Coronal T2FS demonstrates prominence draining vessels and/or lymphatics extending from the deltoid inflammation (Yellow Arrows) to the region of the quadrilateral space (Red Arrow). (D) Coronal T1 images demonstrate an unusual increased T1 signal in the vessels and/or lymphatics extending to the approximate region of the quadrilateral space (Yellow Arrows). Color version of figure is available online.
Case 2
A 26 year-old female received her first Pfizer-BioNTech Covid-19 vaccination four days before a left shoulder MRI for pain following an MVC 7 days prior. She reported only mild injection symptoms without any adenopathy that she noticed. On 1 month follow-up, she again reported no axillary swelling or any deltoid pain. See Figure 2 for images and associated findings.
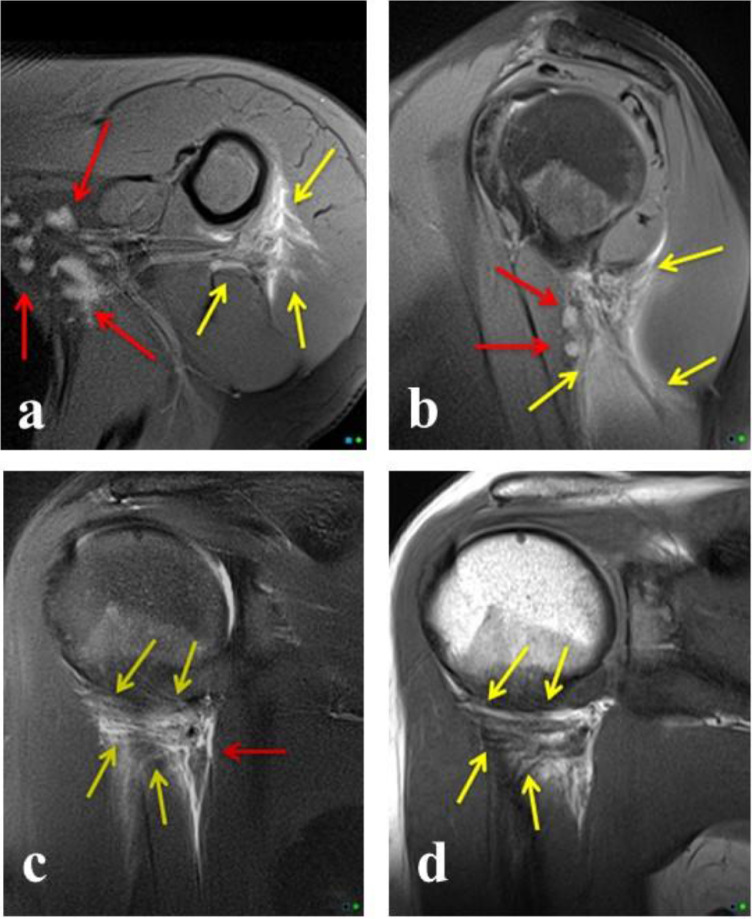
Fig. 2.
Shoulder imaging of a 26 year-old female 4 days following COVID vaccine injection. (A) Axial PDFS demonstrates edema in the deltoid muscle with extension to the approximate location of the quadrilateral space (Yellow Arrows); there is also adenopathy in the axillary region (Red Arrows). (B) Sagittal PDFS demonstrates edema in the region of the quadrilateral space, which surrounds the long head of the triceps (Yellow Arrows); there are small adjacent lymph nodes (Red Arrows). (C) Coronal T2FS demonstrates prominence draining vessels and/or lymphatics extending from the deltoid inflammation (Yellow Arrows) to the inflamed region of the quadrilateral space (Red Arrow). (D) Coronal T1 images demonstrate an unusual increased T1 signal in the vessels/lymphatics extending to the approximate region of the quadrilateral space (Yellow Arrows). Color version of figure is available online.
Case 3
A 34 year-old female received her second dose of the Pfizer-BioNTech COVID-19 vaccination 5 days before imaging for shoulder pain following an MVC 3 weeks prior. She reported some limited range of motion and mild shoulder pain following the MVC. She reported mild deltoid discomfort for ‘a day or two’ following the vaccination, but no symptoms she could relate to the injection at the time of imaging or on a follow-up call. See Figure 3 for images and associated findings.
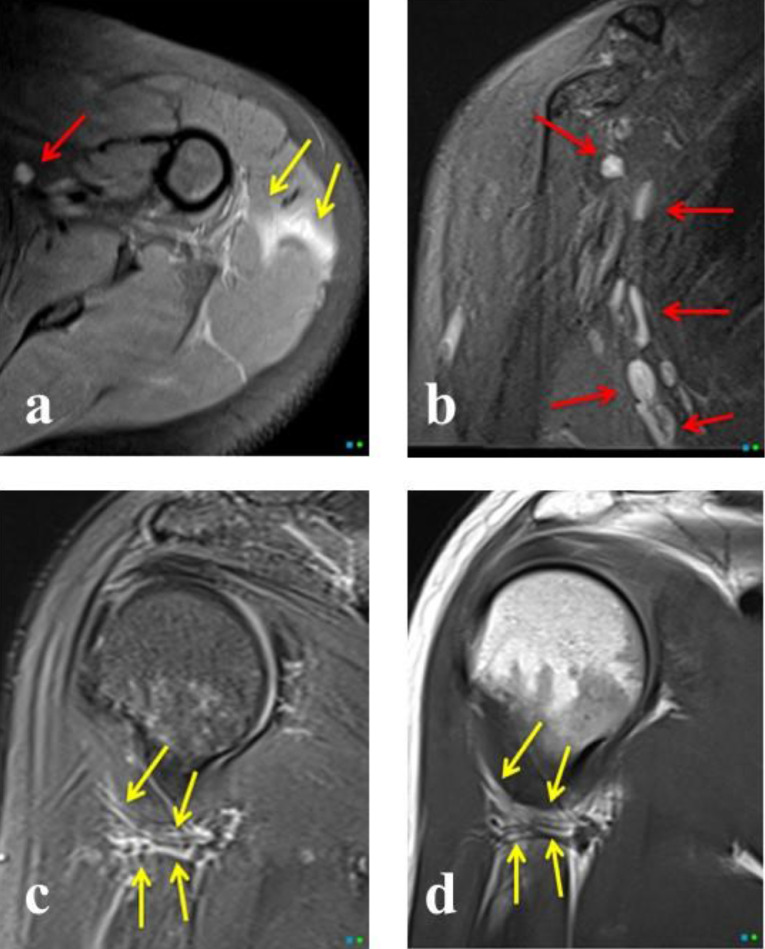
Fig. 3.
Shoulder imaging of a 34 year-old female 5 days following COVID vaccine injection. (A) Axial PDFS demonstrates edema in the deltoid muscle with extension to the approximate location of the quadrilateral space (Yellow Arrows); there is also adenopathy in the axillary region (Red Arrow). (B) Coronal T2FS demonstrates axillary adenopathy (Red Arrows). (C) Coronal T2FS demonstrates prominence draining vessels and/or lymphatics extending from the deltoid inflammation to the region of the quadrilateral space (Yellow Arrows). (D) Coronal T1 images demonstrate unusual increased T1 signal in the vessels and/or lymphatics extending to the approximate region of the quadrilateral space (Yellow Arrows). Color version of figure is available online.
Discussion
Axillary and cervical lymphadenopathy has been well described in patients receiving the COVID-19 vaccine [8,9]. Rare shoulder complications of the COVID-19 vaccine include myositis, calcific myositis, and subacromial-subdeltoid bursitis [10], [11], [12]. These complications have been previously described in pre-COVID vaccinations administration and have been termed ‘shoulder injury related to vaccine administration’ (SIRVA) [13]. No imaging features of these complications were present in our subjects.
Quadrilateral space region edema and inflammation following COVID injection has, to our knowledge, not been previously described and the approximate location of the quadrilateral space appears to be the intermediary station for lymphatic and/or venous drainage before extension to the axilla. There is a paucity of literature on lymphatic drainage of the right upper extremity and particularly of the deltoid [14]. The adjacent triangular intramuscular space has been described as a lymphatic station for upper back melanoma metastasis [15]. It is possible the inflammation we have described as centered in the quadrilateral space involves some of the adjacent spaces as definitive boundaries may be challenging by imaging. In our reported cases, patient 1 was imaged closest to the date of vaccine administration and demonstrated the greatest diffuse axillary edema and/or inflammation with only mild axillary nodal prominence compared to the patients imaged later. Whether the patient received the first or second dose did not seem to affect imaging features in our small cohort. The Pfizer-BioNTech and Moderna Covid-19 vaccinations are mRNA vaccinations that use pieces of mRNA within lipid nanoparticles that are injected intramuscularly [2,3]. Previous studies on lipid injections in the deltoid and biceps brachii demonstrated significant variability in the resolution of the lipid material on MRI ranging from 1 to 16 days depending on the dose and muscle injected with histologic evidence of residual lipid below the resolution of MRI [16,17]. All 3 patients demonstrated vessel prominence with increased T2 and unusual ill-defined increased T1 signal in some of the larger vessels extending from the deltoid region to the approximate region of the quadrilateral space. (Fig. 1, Fig. 2, Fig. 3)
All 3 patients demonstrated diffuse increased T2 signal in the deltoid muscle consistent with edema and/or inflammation and the direct injection of the COVID vaccine (Fig. 1, Fig. 2, Fig. 3). Imaging features of this vaccine inflammatory reaction in the deltoid could be erroneously interpreted as strain, tear, myositis, or denervation injury, depending on the imaging pattern. This edema tracked to the approximate location of the quadrilateral space, where all 3 demonstrated considerable edema and/or inflammation (Fig. 1, Fig. 2, Fig. 3). Imaging features of the inflammatory vaccine reaction in the approximate location of the quadrilateral space and axilla and associated lymphatics and/or vessels could be misinterpreted as regional muscle strain, DVT, brachial plexus injury, neoplasm, or nonspecific infectious and/or inflammatory conditions depending on imaging features [18,19].
With the millions of doses that have already been given and are continuing to increase each day, it is essential for radiologists to recognize the normal shoulder and axillary MRI appearance of patients who have recently received the COVID-19 vaccination to avoid further unnecessary testing and subtract from the actual underlying pathology in shoulders presenting with shoulder pain. This study may also add to the existing literature on deltoid lymphatic drainage.
Patient consent
Written informed consent was obtained by all patients present in study.
Footnotes
Acknowledgment: We would like to acknowledge Jean Jose D.O. for going above and beyond the standard in training MSK radiologists.
Competing Interest: None
References
- 1.CDC . CDC; 2021. COVID-19 Vaccinations in the United States. [Google Scholar]
- 2.FDA; 2021. Pfizer-BioNTech COVID-19 Vaccine EUA Amendment Review Memorandum. [Google Scholar]
- 3.FDA; 2020. Moderna COVID-19 Vaccine VRBPAC Briefing Document. [Google Scholar]
- 4.Behrens RH, Patel V. Avoiding shoulder injury from intramuscular vaccines. Lancet. 2021;397(10273):471. doi: 10.1016/S0140-6736(21)00192-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shay David K., MD, Gee Julianne, MPH, Su John R., MD, PhD, Myers Tanya, PhD, Marquez Paige, MSPH, Liu Ruiling., PhD Safety Monitoring of the Janssen (Johnson & Johnson) COVID-19 Vaccine. MMWR Morb Mortal Wkly Rep. 2021;70:680–684. doi: 10.15585/mmwr.mm7018e2. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tu W, Gierada DS, Joe BN. COVID-19 Vaccination-related lymphadenopathy: what to be aware of. Radiol Imaging Cancer. 2021;3(3) doi: 10.1148/rycan.2021210038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hanneman K, Iwanochko RM, Thavendiranathan P. Evolution of lymphadenopathy at PET/MRI after COVID-19 vaccination. Radiology. 2021;299(3) doi: 10.1148/radiol.2021210386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cellina M, Irmici G, Carrafiello G. Unilateral Axillary Lymphadenopathy After Coronavirus Disease (COVID-19) Vaccination. AJR Am J Roentgenol. 2021;216(5):W27. doi: 10.2214/AJR.21.25683. [DOI] [PubMed] [Google Scholar]
- 9.Keshavarz P, Yazdanpanah F, Rafiee F, Mizandari M. Lymphadenopathy Following COVID-19 Vaccination: Imaging Findings Review. Acad Radiol. 2021;28(8):1058–1071. doi: 10.1016/j.acra.2021.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cantarelli Rodrigues T, Hidalgo PF, Skaf AY, Serfaty A. Subacromial-subdeltoid bursitis following COVID-19 vaccination: a case of shoulder injury related to vaccine administration (SIRVA) Skeletal Radiol. 2021:1–5. doi: 10.1007/s00256-021-03803-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tawfeeq H, Witham F, Dulay GS. COVID-19 related calcific myositis cases. BJR Case Rep. 2021;7(1) doi: 10.1259/bjrcr.20200120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Theodorou DJ, Theodorou SJ, Axiotis A, Gianniki M, Tsifetaki N. COVID-19 vaccine-related myositis. QJM. 2021:1–2. doi: 10.1093/qjmed/hcab043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cross GB, Moghaddas J, Buttery J, Ayoub S, Korman TM. Don't aim too high: avoiding shoulder injury related to vaccine administration. Aust Fam Physician. 2016;45(5):303–306. [PubMed] [Google Scholar]
- 14.Ma CX, Pan WR, Liu ZA, Zeng FQ, Qiu ZQ, Liu MY. Deep lymphatic anatomy of the upper limb: an anatomical study and clinical implications. Ann Anat. 2019;223:32–42. doi: 10.1016/j.aanat.2019.01.005. [DOI] [PubMed] [Google Scholar]
- 15.Hennessy SA, Dengel LT, Hranjec T, Slingluff CL., Jr. A triangular intermuscular space sentinel node in melanoma: association with axillary lymphatic drainage. Ann Surg Oncol. 2010;17(9):2465–2470. doi: 10.1245/s10434-010-1018-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kalicharan RW, Baron P, Oussoren C, Bartels LW, Vromans H. Spatial distribution of oil depots monitored in human muscle using MRI. Int J Pharm. 2016;505(1-2):52–60. doi: 10.1016/j.ijpharm.2016.03.064. [DOI] [PubMed] [Google Scholar]
- 17.Kalicharan RW, Oussoren C, Schot P, de Rijk E, Vromans H. The contribution of the in-vivo fate of an oil depot to drug absorption. Int J Pharm. 2017;528(1-2):595–601. doi: 10.1016/j.ijpharm.2017.06.055. [DOI] [PubMed] [Google Scholar]
- 18.Dronkers CEA, Klok FA, van Haren GR, Gleditsch J, Westerlund E, Huisman MV. Diagnosing upper extremity deep vein thrombosis with non-contrast-enhanced Magnetic Resonance Direct Thrombus Imaging: A pilot study. Thromb Res. 2018;163:47–50. doi: 10.1016/j.thromres.2018.01.015. [DOI] [PubMed] [Google Scholar]
- 19.Morag Y, Jacobson JA, Miller B, De Maeseneer M, Girish G, Jamadar D. MR imaging of rotator cuff injury: what the clinician needs to know. Radiographics. 2006;26(4):1045–1065. doi: 10.1148/rg.264055087. [DOI] [PubMed] [Google Scholar]