Abstract
Purpose
Poverty and poor mental health are closely related and may need to be addressed together to improve the life chances of young people. There is currently little evidence about the impact of poverty-reduction interventions, such as cash transfer programmes, on improved youth mental health and life chances. The aim of the study (CHANCES-6) is to understand the impact and mechanisms of such programmes.
Methods
CHANCES-6 will employ a combination of quantitative, qualitative and economic analyses. Secondary analyses of longitudinal datasets will be conducted in six low- and middle-income countries (Brazil, Colombia, Liberia, Malawi, Mexico and South Africa) to examine the impact of cash transfer programmes on mental health, and the mechanisms leading to improved life chances for young people living in poverty. Qualitative interviews and focus groups (conducted among a subset of three countries) will explore the views and experiences of young people, families and professionals with regard to poverty, mental health, life chances, and cash transfer programmes. Decision-analytic modelling will examine the potential economic case and return-on-investment from programmes. We will involve stakeholders and young people to increase the relevance of findings to national policies and practice.
Results
Knowledge will be generated on the potential role of cash transfer programmes in breaking the cycle between poor mental health and poverty for young people, to improve their life chances.
Conclusion
CHANCES-6 seeks to inform decisions regarding the future design and the merits of investing in poverty-reduction interventions alongside investments into the mental health of young people.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00127-021-02043-7.
Keywords: Young people, Mental health, Poverty, Life chances, Cash transfer programme, Mixed-method study
Background
Mental health, poverty and life chances
Globally, one in four people are aged between 10 and 24 years, making up 1.8 billion of today’s world population [1]. Ninety percent of these young people live in low- and middle-income countries (LMICs) [2]. In LMICs, 20% live on less than $1.90 a day corresponding to about 385 million individuals [3]. Young people living in poverty face multiple forms of cumulative disadvantage—such as violence, crime, lack of educational or employment opportunities—which can significantly limit their future life chances and put them at higher risk of mental disorders [4–6]. Life chances are commonly regarded as a combination of factors that determine a young person’s opportunity to improve their quality of life [7], and have influenced current debates on child poverty and social mobility [6, 8, 9].
The nature of the relationship between poverty and mental health has been subject to academic research for decades [10]. Theories of social causation and social drift have been developed [11, 12] and—to some extent—empirically tested [13] to explain bi-directional links. The social causation theory describes how poverty leads to mental health problems by increasing exposure to violence and trauma or reducing access to social capital. Conversely, the social drift theory hypothesises that mental health problems lead to poverty because they can increase healthcare expenditure, risk of stigma, social exclusion, and loss of employment [11, 13]. Taken together, this relationship leads to a vicious cycle that makes it difficult for individuals to escape poverty and improve mental health. However, it is now widely understood that poverty is a complex multidimensional concept [14, 15] and the nature and strength of the relationship between mental health and poverty also depends on how poverty is conceptualised, measured and experienced [10].
Until now, research on poverty and mental health has focused predominantly on adult populations, and little is known about how the relationship applies to youth [16]. Yet, most mental disorders emerge during adolescence [17, 18]. Mental disorders are the leading contributor to the global disease burden for those aged 10–24 years, with self-harm and violence being the fourth [19]. Whilst mental health problems affect 10–20 per cent of children and young people worldwide [20], the burden is not equally distributed across socio-economic groups [21, 22]. It is estimated that those living in the poorest fifth of the population are twice as likely to develop mental health problems compared to those with average incomes [23].
Interventions
Adolescence is an important time to intervene to prevent mental health problems and poverty in adulthood [24]. Because these outcomes are linked to lifetime losses in employment, other productive activities and health-related quality of life, it has been argued that even if interventions were only able to modestly reduce the incidence or severity of symptoms, their return-on-investment could be substantial [25]. Both anti-poverty programmes and mental health interventions might offer opportunities to break the cycle of poverty and mental illness [26, 27].
There is emerging evidence for promotion, prevention and treatment interventions for mental health among young people in LMICs. Interventions that promote positive mental health can be implemented successfully in school or community settings in LMICs [28]. Mental health treatments have been shown to not only reduce mental health symptoms but also help people stay in or regain employment [27, 29–31]. Overall, there is little synthesised evidence of the full range of mental health interventions for young people living in poverty, and the types of short- and long-term economic outcomes they achieve [13, 32]. However, the need for interventions to address social determinants of mental health problems, including poverty, in LMIC settings is widely recognised [33, 34]. This includes social protection measures, such as cash transfer programmes (CTPs), which have been used to target young people in some countries, and which arguably have a role in improving their mental health whilst reducing poverty [35].
CTPs provide regular direct cash payments to individuals or families identified as living in poverty. Some enforce conditions that individuals need to adhere receive the payment, such as regular health checks or school attendance. In some countries, CTPs are the main vehicle for supporting people living in poverty. During the COVID-19 pandemic, they have been used to reach out to people previously not covered or extend payments to existing beneficiaries to provide a basic safety net for those at-risk of losing their livelihoods [35]. Although evidence is only emerging, CTPs have shown that they improve mental health, for example by reducing suicide rates among adults [36–38]. Among young people, evidence suggests that they can reduce depressive symptoms and psychological distress [16, 26, 39]. Evidence of the effects of CTPs is strongly context specific with outcomes depending on population characteristics as well as programme features [27, 40–43]. For example, they can depend on the amount, regularity and duration of payments [42, 44]. Programme conditionalities, and the way they are administered can also negatively impact young people’s mental health, especially when those are difficult to achieve for the young person, and when an important proportion of family income depends on it [45]. So far, the vast majority of programmes have not intentionally planned for such effects in their design. An exception to this is the Colombian ‘Jóvenes en Acción’ (‘Youth in Action’), which offers direct monthly payments to young people for attending and completing education programmes, and incorporates mental health promotion elements such as interpersonal skills building and emotional regulation. Whilst its impact on mental health has not yet been assessed, findings from its evaluation suggest that it can effectively improve their chances of entering formal employment [46], which is a likely contributor to improved long-term mental health.
Overall, important evidence gaps remain that prevent programme funders and designers from making decisions about allocating resources so that they contribute to breaking the cycle between poverty and poor mental health for young people, and improve their long-term outcomes. In particular, there is limited knowledge in regards to the impact of CTPs on youth mental health, and the mechanisms—such as programme features, population characteristics or contextual factors—at play [27, 40–43]. Whilst there is evidence of the adverse impact of children’s mental health problems on their life chances, including those related to future (mental) health, education, skills, engagement in the labour force, social function in terms of partnership, family formation and citizenship [5], this knowledge is largely from high income countries. Furthermore, while there have been some economic evaluations of the educational impact of CTPs [47], evidence on their cost-effectiveness for health outcomes is largely absent.
Based on the summarised evidence and evidence gaps, we hypothesise that CTPs can improve youth mental health and that mental health is an important factor on the path to improved life chances. Furthermore, we hypothesise that programme features and design alter mental health and life chances outcomes, and hence influence the cost-effectiveness of programmes.
Aims and objectives
The goal of CHANCES-6 is to advance current understanding of the dynamics between poverty, mental health and life chances in young people. We will do this by examining both the impact of poverty reduction policies on mental health, and the economic impact of mental health interventions on life chances and future risk of poverty. Findings will be used to inform decisions regarding the merits of investing in and future design of CTPs alongside investments into the mental health of young people in LMICs.
Running from September 2018 to November 2021, the project is funded by the United Kingdom’s (UK’s) Economic and Social Research Council and led by the Care Policy and Evaluation Centre at the London School of Economics and Political Science. It has partners in the UK (King’s College London) and three LMICs: Brazil (Universidade Presbiteriana Mackenzie), Colombia (Universidad de los Andes) and South Africa (University of Cape Town). Quantitative data analyses cover an additional three Latin American and African countries: Liberia, Mexico and Malawi.
CHANCES-6 seeks to address the following objectives:
To understand the impact of CTPs, and their specific components (e.g., conditionality, age at first receipt and length of receipt) on young people’s mental health and on outcomes in early adulthood that predict life chances (objective 1);
To understand the mechanisms and pathways from mental health and poverty to improved life chances; this includes understanding the relationship between poverty and mental health, and the extent to which improvements in mental health mediate or moderate the relationship between CTPs and life chances (objective 2);
To investigate the economic impact of CTPs (with and without a mental health component) (objective 3);
To understand the perspectives of professional groups involved in funding or running programmes, as well as the views and experiences of young people and their families who participate in CTPs; this includes understanding barriers in current provisions and opportunities for improving programmes (objective 4).
An overarching goal of CHANCES-6 is to inform policies and programmes. Thus, an additional study objective is:
To engage with stakeholders and young people to ensure that the knowledge is relevant to them and can inform national policies and the design and implementation of local programmes (Objective 5).
About the countries and their CTPs
In each of the six countries, one or several large datasets exist that are longitudinal in nature, measure the receipt of CTPs and include relevant mental health and life chances outcomes (Table 1). In Brazil, Colombia, South Africa and Mexico, CTPs refer to national programmes, whilst in Malawi and Liberia, the CTPs were introduced as part of experimental studies. Programmes in Colombia and Mexico are conditional, programmes in South Africa and Liberia unconditional and programmes in Brazil and Malawi are a combination of conditional and unconditional. An overview of the characteristics of the programmes is provided in Table 2.
Table 1.
Description of datasets used for quantitative analysis
| Dataset | Sample and youth age range for analysis | Mental health measures | Life chances measures | Cash transfer program data linkage |
|---|---|---|---|---|
| Itaboraí youth study—Brazil (Wave 1 + 2, 2014–2016) | N = 1409 youth (aged 6 to 16) Representative of Itaboraí city, Rio de Janeiro |
Child behaviour checklist Strengths and difficulties questionnaire Symptoms for post-traumatic stress disorder Self-harm, suicidality |
Dwelling characteristics School drop-out Extracurricular activities Exposure to violence, bullying and stressful life events Resilience Substance abuse Expectations about future |
Bolsa Familia program accessed by 30% of sample |
| Encuesta Longitudinal de la Universidad de Los Andes—Colombia (ELCA) 2010-ongoing | N = 11,914 households; Youth (aged 10 to 16): n = 4164 nationally representative sample | EQ-5D father’s and mother’s self- reported depression or anxiety |
Income, consumption Employment Educational achievement Access to financial services Substance use |
Familias en Acción accessed by sample, linkage to administrative register (includes information for youth supplement) |
| Malawi Schooling, Income, and Health Risk Impact Evaluation Household Survey (2007–2012), 4 waves | N = 3810 households female youth (aged 13–22) Rural town | General Health Questionnaire-12 Mental health inventory 5 |
Dwelling characteristics Household assets and durables, shocks and consumption Employment Educational attainment Physical health HIV/AIDS Marriage |
Randomised controlled trial with groups receiving (i) unconditional cash transfer programme, (ii) conditional cash transfer programme, (iii) nothing |
| South African National Income Dynamics Study (2008-ongoing), 5 waves | N = 28,000 households youth (aged 15–24) nationally representative | Centre for Epidemiological Studies Depression Scale (CES-D) |
Employment Educational attainment Income, expenditure, assets consumption, debt, savings |
Child Support Grant (aged 0–17) accessed by sample |
| Randomised controlled trial, Liberia (2010–2011), 2 waves | N = 999 men (aged 18–35); monrovia |
Anti-social behaviour including aggression, impulsiveness NEO-five factor personality inventory |
Income, assets, expenditure Criminal behaviour |
Randomly assigned: 25% cash transfer only, 28% Cognitive Behavioural Therapy only, 25% both, 22% nothing |
| Progresa/oportunidades, Mexico (1997–2012) 4 waves | N = 6,786 housholds Youth (aged 15–17) nationally representative |
Previously published depression index Subjective well-being18 |
36 parameters on micro-entrepreneurship, income, labour supply, expenditures, social status | Progresa/Oportunidades accessed by sample |
Table 2.
Description of cash transfer programmes included in CHANCES-6
| Colombiaa | Brazilb | South Africac | Liberiad | Malawie | Mexicof | |
|---|---|---|---|---|---|---|
| Name of cash transfer program | Familias en acción | Bolsa familia program | Child support grant | Cash transfer program provided to study participants for limited time | Zomba cash transfer programme | Progresa/oportunidades |
| Population (families, young people) | Families | Families | Children | Young men | Girls and young women | Families |
| Objectives | To overcome poverty and strengthen human capital | To promote social inclusion and strengthen human capital | To ensure basic needs of children < 18 years are met (as part of broader poverty reduction strategy) | To stimulate legal self-employment | To increase schooling and health of female adolescents and young adults | To improve child nutrition, health and education |
| Households/individuals reached (estimate) | 2.7 million families | 11 million households, 46 million people | 12 million children | Experimental: N = 999 male offenders aged 18–35 | Experimental: N = 3796 female adolescents and young adults | 5.8 million households |
| Coverage | 17.5% of total population | 20% of total population | 78% of eligible children | Not applicable | Not applicable | 20% of total population |
| Budget of programme as proportion of GDP | 0.19% | 0.5% | 7.5% | Not applicable | Not applicable | 0.5% |
| Benefits | USD 17 to USD 33 per month | USD 20 per month/person plus USD 10 per child and 15 per young person aged 16–17 (for conditional program); average USD 50 per family | USD 28 per month | USD 100 per month (two one off payments in 2 consecutive months) | USD 4 to 10 for parent; USD 1 to 5 for adolescent/ young adult; plus school fees | USD 10.5 to USD 66 per month |
| Recipient | Caregiver of child or young person | Caregiver of child or young person | Caregiver of child | Young person (male) | Caregivers, young person (female) | Female head of household |
| Eligibility | Families in poverty, displaced by internal conflict and/or from indigenous communities with members under 18 years old | Poor families: monthly per capita income < 40 USD (eligible for conditional part of programme) or < 20 USD (eligible for unconditional part of programme) | Child < 18 years; caregiver’s yearly income < USD 3,275 (single) or < USD 6,555 (combined with spouse) | High risk (defined by their involvement in drug use and dealing and other types of offences) | Age 13–22, never married, enrolled in primary/secondary school or recent dropout | Poor families with child < 18 years |
| Identification methods | Geographical; identification system (SISBEN) | Geographical; means test income threshold | Proxy means test | Not applicable | Not applicable |
Geographical; proxy means test (questionnaire ENCASEH) |
| Conditional or unconditional | Conditional | Mix: unconditional for extremely poor; conditional for poor families | Unconditional | Unconditional | Mix: conditional and unconditional arms in study | Conditional |
| Conditionalities | Child health checks; regular school attendance (80%) | Regular medical consultation, vaccinations, school attendance (75–85%) | Not applicable | Not applicable |
Conditional arm Regular school attendance (80%) |
Regular school attendance (85%); regular medical check ups |
| Monitoring | Information systems | Nutritional surveillance; vaccination monitoring | Not applicable | Not applicable | Self-reported; school attendance records | Compliance checks (attendance cards) |
aFiszbein A and Schady N (2009)[55]
bMinistério da Cidadania (2019), Soares S (2012) [56, 57]
cNIDS (2019), Seekings (2007) [58, 59]; South African Government website: https://www.gov.za/services/child-care-social-benefits/child-support-grant
dBlattman et al. (2016) [60]
eBaird S et al. (2011), Angeles et al. (2019) [26, 45]
fFiszbein A and Schady N (2009) [55]
With regards to the country context, in which programmes operate, population size varies substantially from 5 million (Liberia) to 205 million (Brazil), whilst the proportion of young people is relatively similar (16–22%) across countries. In terms of health risks for young people (15–24 years), leading factors include HIV (South Africa), binge drinking (Brazil), and child marriage and teenage pregnancies (Malawi and Liberia). Brazil ranks highest with regards to estimated burden of mental disorders (measured in disability adjusted life years) as well as investments into mental health service infrastructure. Table 3 presents an overview of the countries’ data for important mental health, poverty and life chances indicators.
Table 3.
Overview of population, poverty, mental health and life chances indicators for CHANCES-6 countries
| Brazil | Colombia | South Africa | Liberia | Malawi | Mexico | |
|---|---|---|---|---|---|---|
| Populationg | ||||||
| Total population | 205,962,108 | 48,228,697 | 55,291,225 | 4,499,621 | 18,143,315 | 125,890,949 |
| Population 15–24 years | 33,689,000 | 8,711,000 | 9,820,000 | 983,000 | 3,886,000 | 22,139,000 |
| Proportion 15–24 years, in % | 18 | 16 | 18 | 22 | 21 | 18 |
| Proportion (all ages) living in rural areas, in % | 15 | 23 | 35 | 50 | 84 | 21 |
| Poverty and income inequalityh | ||||||
| GDP per capita (2018), in USD | 8,921 | 6,651 | 6,374 | 674 | 389 | 9,698 |
| Poverty headcount ratio at USD 1.90 a day (2011 PPP), in % of population | 3.4 | 4.5 | 18.9 | 38.6 | 71.7 | 3.8 |
| GINI Index (2017) | 53.3 | 49.7 | 63 | 35.3 | 44.7 | 48.3 |
| Mental health (MH)i | ||||||
| MH expenditure per person, in USD | 1.4 | Not reported | 6.7 (12.4j) | 0.02 | Not reported | Not reported |
| Government’s expenditure on MH as proportion of total government health expenditure, in % | 1 | Not reported | 3 (5k) | 2.4 | Not reported | Not reported |
| Burden of mental disorders (DALYs); per 100,000 | 3,593 | 3,526 | 3,191 | 2,298 | Not reported | 2,368 |
| Plan or strategy for child and/or adolescent mental health | Yesl | Yes | Yes | Yes | Not reported | No |
| Suicide mortality rate; per 100,000 | 6.5 | 7.2 | 11.6 | 6.8 | Not reported | 5.1 |
| Psychiatrists per 100,000 | 3.16 | 1.84 | 1.52 (0.31 among uninsured populationm) | 0.04 | 0.01 | 0.21 |
| Child psychiatrists per 100,000 | (38n) | Not reported | 0.08 (0.02 among uninsured populationo) | Not reported | Not reported | 0.03 |
| Psychologists per 100,000 | 12.37 | Not reported | Not reported (0.97 among uninsured populationp) | Not reported | 0.02 | 3.46 |
| Other paid MH workers per 100,000 | 243 | Not reported | Not reported | 4.56 | Not reported | 0.25 |
| Total number of mental health professionals | 653,329 | 885 | Not reported | 560 | Not reported | 5,541 |
| Total number of mental health workers per 100,000 | 318 | 1.84 | Not reported | 12.45 | Not reported | 4.4 |
| Outpatient facilities for children and adolescents (total) | 223 | Not reported | Not reported | 6 | Not reported | 26 |
| Life chancesq | ||||||
| Not in education, employment or training (NEET), 15–14 years old, in % | 24 | 23 | 32 | Not reported | Not reported | 18 |
| Youth unemployment, in % | 29 | 19 | 53 | 3 | 7 | 7 |
| Labour force participation (ages 15–24) in % | 55 | 52 | 26 | 30 | 64 | 44 |
| Employment to population ratio, ages 15–24 total, in % | 39.5 | 42.9 | 11.9 | 55.6 | 27.4 | 40.7 |
| HIV prevalence (ages 15–24), in % | Female: 15–19 years 3.2, 20–24 years 10.3 Male: 15–19 years 7.0 20–24 years 36.2r | Female: 0.1 Male: 0.1 | Female: 11.3 Male: 3.7 | Female: 0.8 Male: 0.4 | Female: 4.3 Male: 2 | Female: 0.1 Male: 0.1 |
| Prevalence binge alcohol use (ages 15–19), in % | Female: 32.3 Male: 32.7 | Female: 20 Male: 29 | Female: 11.2 Male: 15.8 | Female: 13.4 Male: 17.8 | Female: 5.0 Male: 16.3 | Female: 11.8 Male: 21.6 |
| Adolescent life births per 1000, 15–19 years | 66.8 | 41.6 | 40.4 | 104.8 | 142.7 | 60.5 |
| Females (ages 20–24) in marriage before age 18 years, in % | 26s | 23.4 | Not reported | 35.9 | 42.1 | 26.1 |
gWorld Bank Group [61]
hIbid
iWorld Health Organisation [62]
jIn brackets a more recent figure is provided from Docrat et al. 2019 [63]. This figure is shown brackets because it is not from the same year or source as the figures for the other countries, which relate to 2017.
kIbid
lWhilst the WHO source states that no such plan is in place, the following documents have been produced by the Brazilian Ministry of Health (2011, 2014) http://bvsms.saude.gov.br/bvs/saudelegis/gm/2011/prt3088_23_12_2011_rep.html
http://bvsms.saude.gov.br/bvs/publicacoes/atencao_psicossocial_criancas_adolescentes_sus.pdf
mDocrat et al. 2019 [63]
nDemografia Médica no Brasil 2018. São Paulo, SP: FMUSP, CFM, Cremesp, 2018. 286 p. ISBN: 978–85-87,077–55-4; available from http://www.epsjv.fiocruz.br/sites/default/files/files/DemografiaMedica2018%20(3).pdf (last accessed 6 April 2020).
oIbid
pIbid
qWorld Bank Open Data [1]; Azzopardi et al. 2019 [2]
rMinistério de Saúde Brasil (2018), Boletim epidemiológico HIV/Aids 2018, http://www.aids.gov.br/pt-br/pub/2018/boletim-epidemiologico-hivaids-2018;
sPlan International (2019), Tirando o véu Estudo sobre casamento infantile no brasil https://plan.org.br/wp-content/uploads/2019/06/Estudo-Casamento-Infantil-Brasil_final.pdf
Methods
General approach
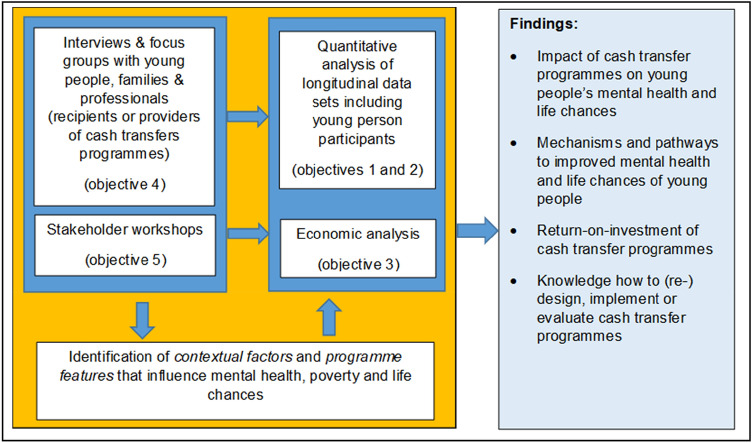
Our approach to addressing the five objectives involves a range of methods and work streams. The first two objectives will be addressed primarily through quantitative (statistical) analyses of data on recipients of CTPs. Important concepts emerging from the qualitative analysis, i.e., interviews and focus groups with providers and recipients of CTPs (objective 4), as well as from stakeholder consultations (objective 5) and the scientific literature will inform the interpretation of findings from quantitative analyses. This includes knowledge about contextual factors and programme features likely to explain differences in findings on impacts. Findings from the qualitative analysis will inform interpretation of results from the quantitative analysis. The economic analysis conducted (objective 3) will be informed by both the quantitative and qualitative analyses, as well as stakeholder consultation. Figure 1 provides an overview of the approach. This study will follow a triangulation design [48], in which quantitative and qualitative parts are conducted mainly in parallel and we use and analyse multiple sources of data together to more comprehensively address our research question and to increase validity of findings. The main interaction and integration between the quantitative and qualitative methods will take place in the analysis and interpretation of the quantitative findings. However, there are additional interaction points as triangulation follows a flexible approach that allows findings to emerge at different stages and from the different parts of the research to address interconnected questions of the role of contextual factors, mechanisms and impacts.
Fig. 1.
Overview of the general approach
Investigating the impact of CTPs (Objective 1)
In quantitative (statistical) analyses, we will explore effects of the CTPs on mental health and on life chances outcomes by first examining impacts overall and then by mental health status, adjusting for all relevant covariates. We will first conduct country-specific analysis on each CTP, and then conduct analysis based on data that are harmonised across all countries. The primary data sources for the quantitative analysis will be data from intervention and population panel studies in each of the six countries (Table 1). Table 4 presents the socio-demographic characteristics of young people and their households from the population panel studies in Brazilian, Colombian and South African, including a comparison of characteristics of young people with and without mental health problems.
Table 4.
Socio-demographic characteristics of young people and their households for Brazil, Colombia, South Africa; comparison of young people with and without mental health problems
| Brazila | Colombiab | South Africac | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total (N = 1189) | Mental health problemsd (N = 155) | No mental health problems (N = 1034) | Total (N = 6430) | Mental health problemsd (N = 642) | No mental health problems (N = 5788) | Total (N = 2452) | Mental health problemsd (N = 394) | No mental health problems (N = 2058) | |||||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | ||
| Single mother | 421 | 35 | 57 | 37 | 364 | 35 | – | – | – | – | – | – | – | – | – | – | – | – | |
| Socio-economic groupe | |||||||||||||||||||
| Low | 662 | 58 | 93 | 60 | 569 | 55 | 1136 | 18 | 302 | 47 | 2877 | 50 | – | – | – | – | – | – | |
| Middle | 458 | 39 | 54 | 35 | 404 | 39 | 1663 | 26 | 333 | 52 | 2818 | 49 | – | – | – | – | – | – | |
| High | 69 | 6 | 8 | 5 | 61 | 6 | 3534 | 56 | 7 | 1 | 93 | 2 | – | – | – | – | – | – | |
| Household income under poverty line | – | – | – | – | – | – | – | – | – | – | – | – | 1169 | 42 | 211 | 51 | 958 | 41 | |
| Mother’s education | |||||||||||||||||||
| No/basic | 464 | 39 | 65 | 42 | 399 | 39 | – | – | – | – | – | – | – | – | – | – | – | – | |
| Middle | 354 | 30 | 42 | 27 | 312 | 30 | – | – | – | – | – | – | – | – | – | – | – | – | |
| High | 371 | 31 | 48 | 31 | 323 | 31 | – | – | – | – | – | – | – | – | – | – | – | – | |
| Father’s or head of household education | |||||||||||||||||||
| No/basic | 511 | 43 | 73 | 47 | 438 | 43 | – | – | – | – | – | – | – | – | – | – | – | – | |
| Middle | 372 | 31 | 38 | 25 | 334 | 32 | – | – | – | – | – | – | – | – | – | – | – | – | |
| High | 303 | 26 | 44 | 28 | 259 | 25 | – | – | – | – | – | – | – | – | – | – | – | – | |
| Mother unemployment (paid work in the past 30 days) | 484 | 41 | 70 | 45 | 414 | 40 | 229 | 4 | 24 | 4 | 205 | 4 | – | – | – | – | – | – | |
| Father unemployment (paid work in the past 30 days) | 98 | 13 | 19 | 19 | 79 | 12 | 460 | 7 | 57 | 9 | 403 | 7 | – | – | – | – | – | – | |
| Ethnic group | |||||||||||||||||||
| Black African | – | – | – | – | – | – | – | – | – | – | – | – | 2091 | 84 | 348 | 91 | 1743 | 83 | |
| ‘Coloured’f | – | – | – | – | – | – | – | – | – | – | – | – | 310 | 8 | 41 | 6 | 269 | 9 | |
| Indian | – | – | – | – | – | – | – | – | – | – | – | – | 19 | 2 | 0 | 0 | 19 | 2 | |
| White | – | – | – | – | – | – | – | – | – | – | – | – | 32 | 5 | 5 | 3 | 27 | 6 | |
| Resides in rural area | – | – | – | – | – | – | – | – | – | – | – | – | 1446 | 46 | 246 | 53 | 1200 | 48 | |
| No health insurance | – | – | – | – | – | – | – | – | – | – | – | – | 2278 | 88 | 378 | 93 | 1900 | 87 | |
| Overcrowding | |||||||||||||||||||
| Average number of persons in one room | 1.1 | 57 | 1.3 | 77 | 1.0 | 52 | – | – | – | – | – | – | 1.7 | – | 2.1 | – | 1.7 | – | |
| Number of people in one room > 2 | – | – | – | – | – | – | 1466 | 23 | 153 | 24 | 1293 | 22 | – | – | – | – | – | – | |
| Quality of housing and access to house | |||||||||||||||||||
| Street to house not paved or asphalted | 801 | 67 | 115 | 74 | 40 | 66 | – | – | – | – | – | – | – | – | – | – | – | – | |
| Inadequate external wallsg | – | – | – | – | – | – | – | – | – | – | – | – | 565 | 19 | 90 | 22 | 475 | 19 | |
| Access to water and sanitary facilities, public utilities | |||||||||||||||||||
| No piped/running water access | 820 | 69 | 106 | 68 | 714 | 69 | 1336 | 21 | 113 | 18 | 1223 | 21 | – | – | – | – | – | – | |
| Without access to sanitary service | – | – | – | – | – | – | 842 | 13 | 113 | 18 | 827 | 14 | 386 | 12 | 76 | 15 | 310 | 11 | |
| Unimproved water systemg | – | – | – | – | – | – | – | – | – | – | – | – | 870 | 30 | 139 | 34 | 731 | 30 | |
| Unimproved sewage systemg | – | – | – | – | – | – | – | – | – | – | – | – | |||||||
| Child education | |||||||||||||||||||
| School attendance | 1174 | 99 | 151 | 97 | 1034 | 99 | – | – | – | – | – | – | – | – | – | – | – | – | |
| School drop–out | 10 | 1 | 3 | 2 | 7 | 1 | – | – | – | – | – | – | – | – | - | – | – | – | |
| School repetition | 151 | 13 | 28 | 19 | 123 | 12 | – | – | – | – | – | – | – | – | – | – | – | – | |
| Education (in years) | – | – | – | – | – | – | – | – | – | – | – | – | 9 | – | 8.9 | – | 9 | – | |
| ≥ 2 years behind expected grade | – | – | – | – | – | – | – | – | – | – | – | – | 1315 | 49 | 210 | 53 | 1105 | 54 | |
| Not in education, training or employment | – | – | – | – | – | – | – | – | – | – | – | – | 356 | 13 | 68 | 18 | 288 | 12 | |
aItaboraí Youth Study-Brazil: Comparison of socioeconomic characteristics among young people with and without mental health problems (2015); socioeconomic characteristics were only assessed at the second wave of the study
bEncuesta Longitudinal de la Universidad de Los Andes—Colombia (ELCA) 2016. Sample age 11–16
cSouth African National Income Dynamics Study (2008-ongoing), 5 waves Sample at Wave 3, age 15–19 (all populations). Estimates (percentages and standard deviations) are weighted using sampling weights from Wave 3
dBrazil and Colombia: Refers to standard cut-off scores of the Strengths and Difficulties Questionnaire (SDQ); young people without mental health problems include those scoring in the normal and borderline range; South Africa: Refers to the Centre for Epidemiological Studies Depression Scale (CES-D) and a cut off score of 12
eFor Colombia, socio-economic strata represents the official socio-economic classification used by the government. The Encuesta Longitudinal Colombiana (ELCA) data only includes households from the first 4 (out of 6) socio-economic strata
fIn South Africa, the term ‘coloured’ is used to identify a group of people with mixed black and white ethnicity who have a relatively distinct cultural identity, particularly in the Western Cape. In the apartheid era, these racial categories were used by the government to legitimise state-sponsored oppression of ‘black’ and ‘coloured’ people. As the effect of these practices on health and access to resources may still be apparent, these categories are used within the context of the study
gInadequate external walls refers to: exterior walls built of untreated wood, boards, planks, vegetation (e.g., guadua), zinc, cloth, cardboard, waste material or no exterior walls (urban household); exterior walls built of vegetation (e.g., guadua) zinc, cloth, cardboard, waste materials or no exterior walls (rural household). Unimproved water system refers to: no connection to public water systems; rural households: water used for the preparation of food obtained from wells, rainwater, spring sources, water tanks, water carriers or other sources. Unimproved sewage system refers to: no public sewer system; rural households: toilet without a sewer connection, latrine or no sewage system
All studies have used validated measures of poverty, mental health and life chances variables from well-established datasets. Based on these secondary datasets, we will investigate the impact of CTPs on mental health, and on life chances variables for young people. Different age ranges will be considered depending on eligibility criteria for the CTP and study design (Table 1). As much as this is possible mental health variables that indicate conditions will be analysed on a continuum “from mild, time-limited distress to chronic, progressive and severely disabling conditions” [18]. In addition to assessing mental health conditions, variables which focus on related positive aspects of mental health such as life satisfaction, self-esteem, self-efficacy, and resilience will be analysed. With regard to life chances, a range of variables are measured in studies that provide indicators of the present situation and future of young person participants. These include educational achievements, employment status, income, substance misuse, living arrangements and relationship status (Table 1). In terms of poverty, relevant variables exist in each of the datasets, which allows us to adopt a multi-dimensional approach to poverty.
Our data analysis strategies will be based on quasi-experimental evaluation techniques [49] and other epidemiological approaches. As examples of quasi-experimental techniques we will identify so-called ‘discontinuities’ in the eligibility criteria for CTPs (often based, in parts, on an income or poverty threshold) and use a regression discontinuity design [8]. For some programmes, we will use a difference-in-differences design, incorporating propensity score matching when appropriate. As for other epidemiological approaches, we will use different ways of estimating associations and causal effects of programs with cross-sectional and longitudinal data. The analytic method will be selected based on: (a) presence (or not) of necessary information/variables as well as number of observations for applying each quasi-experimental method and (b) verification of main identification assumptions underlying each method. Where the data meet the criteria of more than one method, we will compare results of all available methods.
Data harmonisation will include identifying commonalities and differences in mental health, life chances and poverty measures, and harmonising them across datasets, for example, using standardised percentile scores. Since datasets refer to different time periods, collected at different waves, and covering different age ranges, a selection will be made for the harmonised dataset, choosing data for time periods and age ranges most closely aligned with each other. The harmonisation process will involve collating shared variables (regarding the CTPs, mental health, life chances, poverty and socioeconomic status) and using the differences between programmes to answer key questions about their effect on mental health. This will allow comparisons across cultures and across CTPs (e.g., conditionality, age at receipt, length of receipt) to determine which features of the CTP are associated with better improvements in mental health and life chances. Online resource 2 provides an example of how data might be harmonised, by demonstrating this for selected datasets and indicators.
Delineating pathways and identifying mechanisms (Objective 2)
We will conceptualise and assess pathways that explain relationships between poverty, mental health and future life chances, and the influence CTPs have on them. This will be done primarily using quantitative analyses of datasets mentioned above (Table 1). As with the analysis of impact, parameters will be informed by qualitative findings, as well as scientific literature and stakeholder consultation. In addition, qualitative data could provide a broader conceptualisation of pathways and mechanisms, including those that cannot be tested quantitatively through our analyses (but that might inform future data collection and analyses).
First, we will carry out a systematic review of the literature on the impact of CTPs on mental health outcomes of young people, focusing on LMICs. We will then develop a conceptual framework of hypothesised pathways and mechanisms based on those contextual factors, conditionalities and features of CTPs identified as important in previous evaluations of CTPs and mental health programmes, other relevant scientific literature and views and experiences from young people and professionals involved in or knowledgeable of CTPs.
Overlaps between data gathered from the reviewed literature and our own knowledge (including knowledge based on data collected by that time) will be used to confirm the importance of pathways. Where data from different sources diverge, this will be also highlighted.
Next, where possible, we will test some of the mechanisms linking mental health and poverty to improved life chances. Potential variables to consider as having a role in those pathways include:
Contextual factors: e.g., unemployment, social cohesion, family functioning;
Conditionalities: e.g., school attendance and child health visits; and
Other programme features: e.g., amount of money; length of time receiving the cash transfer; ways of monitoring compliance
We will develop statistical models using recommended methods for mediation and moderation [50]. For example, we will examine whether CTPs are associated with improvements in mental health and if these improvements mediate any improvement in future life chances.
Simulating cost-effectiveness of CTPs and mental health interventions (Objective 3)
Decision analytical modelling will be conducted to estimate the return-on-investment to the public purse from investing in country specific CTPs given any potential association we identify with mental health outcomes and life chances. This will be compared with expected outcomes and public purse costs associated with no intervention. In addition, the return-on-investment from investing in CTPs will be compared with alternative or complementary investment in selected effective mental health interventions in LMIC contexts. Such interventions will be identified in published systematic reviews and meta-analyses.
Effect sizes identified in the statistical analysis in Objective 2 will be combined with longitudinal trajectories of mental health and life chances identified in each of the longitudinal data sources (Table 1) to estimate potential long-term outcomes. Long-term monetary values will be attached to different life chances outcomes where possible. An example would be to estimate the value of higher rates of school completion for wealth accumulation and income through to adulthood. We will draw on published literature, e.g., costs reported in previous economic analyses of CTPs [47], as well as statistical reports relating to CTPs in the six countries, to estimate their administrative costs. The specific time frame for the modelling will depend on data availability. Costs and outcomes beyond 1 year will be discounted and all monetary values will be reported in purchasing power parity adjusted international dollars.
Modelling will also take account of implementation and scale-up costs in line with previous work [51]. We will also vary underlying assumptions using both deterministic and probabilistic sensitivity analysis to reflect uncertainty on both effectiveness estimates and cost distributions. To increase policy relevance, and after engagement with stakeholders (Objective 5) we will also model specific conservative and optimistic scenarios. This could include varying assumptions on uptake rates to reflect themes in qualitative analysis with young people, families and professionals set out in Objective 4.
Understanding young people’s, families’ and professionals’ experiences (Objective 4)
We will conduct semi-structured interviews and focus groups with young people, families and professionals who use or deliver CTPs in the three countries in which our partners are based (Brazil, Colombia and South Africa). The aim of this qualitative research is to elicit information about:
-
(i)
Young people’s experiences and meaning of poverty and mental health in these diverse cultures and settings;
-
(ii)
Personal experiences of being involved in the CTP,
-
(iii)
Implementation barriers and facilitators of current programmes; and
-
(iv)
Ideas for future combined CTP and mental health interventions.
The interviews will allow us to gain an in-depth understanding of young people’s experiences with CTPs, how they experience mental health and poverty more generally, and how they view their future, whereas in focus groups we seek to get an understanding of the family and community context in which programmes operate. We will elicit views from young people, families and professionals about the local context and about how programmes operate, the role of programme features and how programmes can be improved to better support young people.
We plan to conduct between 15 and 20 interviews and 3 and 4 focus groups in each of the 3 countries. Sampling and recruitment strategies for interviews and focus group will be tailored to the country setting. Partners will build rapport with the community and potential participants beforehand, through community visits and meetings utilising relationships with community organisations, youth groups and non-government organisations.
For the interviews, we will invite young people who are past or current users of CTPs, and who received or applied for the cash transfer themselves or who received this via their parents. For the focus groups, we will recruit parents who receive cash transfers, practitioners involved in the delivery of programmes and youth leaders from youth organisations.
Focus groups and interviews will be conducted in the local language, audio-recorded, transcribed and translated into English. First, country-specific analysis will be conducted using the complete data (in the mother language where possible). Next, data (in English) will be harmonised across countries by identifying commonalities. We will apply a constant comparative approach towards the coding [48, 52], thus allowing for repeated explorations and reflections with colleagues across countries. Data will be analysed primarily using inductive methods in the form of a framework approach to thematic analysis.
Details on how data for interviews and focus groups will be gathered and analysed following COREQ recommended standards are presented in online resource 1 [53].
Engaging stakeholders and young people (Objective 5)
A key element of CHANCES-6 is to work in partnership with policy makers and influencers, and other national or local stakeholders. This includes various representatives in governmental and non-governmental organisations (NGOs) who have responsibilities for health and welfare funding, planning and delivery. We will organise high-level policy workshops in each of the countries where our partners are based (i.e., Brazil, Colombia and South Africa), one in the first and one in the last year of the project. In the first round of stakeholder workshops, we will raise awareness of the research aims, seek feedback on methods and approach, and understand interests and capacities in utilising and implementing findings from the research. In addition, we will gather information that will help us understand implementation barriers and facilitators of current programmes, and opportunities for combined provision of CTPs and mental health programmes. The main aim of the second stakeholder workshop will be to discuss implications of the CHANCES-6 findings for policies and programme development, implementation and evaluation. We will plan activities to stay engaged with stakeholders between workshops and identify new stakeholders throughout the project. Partners in each of the countries will facilitate an ongoing dialogue with stakeholders, so we can incorporate their feedback as the research develops based, for example, on policy changes (including in relation to COVID-19), and in the interpretation and presentation of findings.
Additionally, we will develop and use various (social) media channels, outputs and tools to create opportunities for engaging with stakeholders and influence policies in all six countries of the project and beyond. Information and updates on the project, including research findings as they become available during the project, will be provided on the project website (https://www.lse.ac.uk/cpec/chances-6). We will also engage with representatives from international development agencies such as the World Bank, World Health Organisation and UNICEF and with relevant international communities.
Our ultimate beneficiaries are young people living in poverty. Overall, we plan to work with young people throughout the project, by engaging with youth leaders and representatives of organisations which advocate for the rights of young people, locally or nationally. The approach towards engaging with youth will be context-specific, and build on existing partnerships. Young people will be invited to become involved in telling their stories through social media, and by participating in a short films. Young people will become involved in the project, for example in the roles of advisors, advocates, and research staff. This will include involving students from universities, and involving youth in the interpretation of findings of the research.
Discussion
CHANCES-6 is a multi-disciplinary, multi-site study, which spans six Latin American and African countries. Innovative data collection and analyses—combined with stakeholder engagement—will generate critical knowledge to inform policies and programme designs that consider young people’s mental health when seeking to optimise investment into CTPs. The ultimate aim of this project is to understand how to break the cycle of poverty and mental illness during adolescence to improve young people’s future life chances.
Investments into mental health—both in total as well as in proportion to total health expenditure—are very small in LMICs and treatment is available to very few people. CTPs on the other hand are available and reach a substantial proportion of the population. In the global mental health field, a considerable amount of research effort has gone into designing and evaluating treatment interventions in the past 10–15 years, whereas much less research has been concerned with addressing the social determinants of mental ill health [33]. CHANCES-6 is an opportunity to understand how widely implemented interventions such as cash transfer programmes influence mental health and to develop a more integrated approach to addressing mental health and its social determinants.
There is growing interest among international development agencies and governments in LMICs in understanding the role of poor mental health in maintaining poverty cycles [54]. In this context, CHANCES-6 is particularly salient, for a number of reasons. Firstly, we will generate knowledge on the role of mental health as a mediator and moderator for future life chances of young people living in poverty, and on the causal relationships between poverty and mental health in this population. This addresses an important gap in the evidence as most studies in this area have been descriptive and cross-sectional [40]. Secondly, we will contribute to the emerging evidence on the impact of CTPs on young people’s mental health, and the features of programmes that influence mental health. Thirdly, we will generate knowledge on the role of mental health interventions or support in augmenting the impact of CTPs on life chances. Findings from the economic analyses will provide policy stakeholders with the knowledge of the value of CTPs, and whether including access to mental health support as part of such programmes is likely to increase their economic value. Fourthly, we will generate knowledge about the feasibility, opportunities and barriers in relation to how programmes might be best delivered to improve young peoples’ mental health and life chances. Finally, CHANCES-6 will generate methodological advances for pooling data from diverse longitudinal data sources to estimate mental health and socio-economic effects that are locally relevant and internationally comparable.
Supplementary Information
Below is the link to the electronic supplementary material.
Funding
This study is supported by the UKRI’s Global Challenges Research Fund (Grant number ES/S001050/1). The support of the Economic and Social Research Council is gratefully acknowledged. A. Matijasevich receives support from the National Council for Scientific and Technological Development (CNPq), Brazil.
Data availability
The data sources for the quantitative analysis are secondary sources, which are already publicly available. For the qualitative data analysis, data are not fully shareable as some of the will contain identifiable information. However, findings from the analysis will be published together with details on the research methods and tools.
Code availability
Not applicable.
Compliance with ethical standards
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
Ethical approval was given by the appropriate ethics committees in accordance with the 1964 Declaration of Helsinki. This includes ethical approval by the Research Ethics Committee at the London School of Economics and Political Science (REC ref. 997). New data collection in Brazil, Colombia and South Africa had approval or is currently seeking approval from local ethical committees. South African ethics approval was obtained from the University of Cape Town Health Sciences Faculty Human Research Ethics Committee (HREC Ref: 396/2019). Brazilian ethics approval was obtained on July 10th 2019 from the National Ethics Committee (CONEP), CAEE: 06777318.2.0000.0084. Colombian ethical approval was granted by the Universidad de los Andes Ethics Committee (Ref: 02376-2019). Ethics approval for secondary analysis of quantitative data conducted at King’s College London was obtained from King’s College London Research ethics office (LRS-19/20-15050).
Consent to participate
Only persons who provide informed consent will be included in the study.
Consent for publication
All authors consent to the publication of the manuscript in Social Psychiatry and Psychiatric Epidemiology.
References
- 1.UNFPA (2014) State of world population 2014. United Nations population fund. https://www.unfpa.org/swop-2014. Accessed 13 July 2021
- 2.United Nations (2017) World Population Prospects . UN department for economic and social affairs (UN DESA) New York: Population Division; 2017. [Google Scholar]
- 3.UNICEF (2016) Ending extreme poverty: a focus on children. UNICEF and the World Bank Group. https://www.unicef.org/publications/index_92826.html. Accessed 13 July 2021
- 4.Goodman A, Joyce R, Smith JP. The long shadow cast by childhood physical and mental problems on adult life. Proc Natl Acad Sci. 2011;108(15):6032–6037. doi: 10.1073/pnas.1016970108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Richard R, Abbot R. Childhood mental health and life chances in post-war Britain. The Smith Institute: Insights from three national birth cohort studies; 2009. [Google Scholar]
- 6.Duncan GJ, Yeung WJ, Brooks-Gunn J, Smith JR. How much does childhood poverty affect the life chances of children? Am Sociol Rev. 1998;63(3):406–423. doi: 10.2307/2657556. [DOI] [Google Scholar]
- 7.Wright RA. RALF DAHRENDORF. Life chances: approaches to social and political theory Pp ix, 181. Chicago: the University of Chicago Press 1980. $15.00. Ann Am Acad Polit Soc Sci. 1980;451(1):193–194. doi: 10.1177/000271628045100150. [DOI] [Google Scholar]
- 8.Ludwig J, Miller DL. Does head start improve children's life chances? Evidence from a regression discontinuity design. Q J Econ. 2007;122(1):159–208. doi: 10.1162/qjec.122.1.159. [DOI] [Google Scholar]
- 9.Stewart K, Lupton R (2015) Social mobility under the coalition government: have the life chances of the poorest children improved? | British Politics and Policy at LSE. Accessed 13 July 2021
- 10.Lund C, Breen A, Flisher AJ, Kakuma R, Corrigall J, Joska JA, Swartz L, Patel V. Poverty and common mental disorders in low and middle income countries: a systematic review. Soc Sci Med (1982) 2010;71(3):517–528. doi: 10.1016/j.socscimed.2010.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dohrenwend BP, Levav I, Shrout PE, Schwartz S, Naveh G, Link BG, Skodol AE, Stueve A. Socioeconomic status and psychiatric disorders: the causation-selection issue. Science. 1992;255(5047):946–952. doi: 10.1126/science.1546291. [DOI] [PubMed] [Google Scholar]
- 12.Flisher AJ, Lund C, Funk M, Banda M, Bhana A, Doku V, Drew N, Kigozi FN, Knapp M, Omar M, Petersen I, Green A. Mental health policy development and implementation in four African countries. J Health Psychol. 2007;12(3):505–516. doi: 10.1177/1359105307076237. [DOI] [PubMed] [Google Scholar]
- 13.Lund C, Cois A. Simultaneous social causation and social drift: longitudinal analysis of depression and poverty in South Africa. J Affect Disord. 2018;229:396–402. doi: 10.1016/j.jad.2017.12.050. [DOI] [PubMed] [Google Scholar]
- 14.Alkire S, Santos ME. A multidimensional approach: poverty measurement and beyond. Soc Indic Res. 2013;112(2):239–257. doi: 10.1007/s11205-013-0257-3. [DOI] [Google Scholar]
- 15.Atkinson A. Multidimensional deprivation: contrasting social welfare and counting approaches. J Econ Inequal. 2003;1(1):51–65. doi: 10.1023/A:1023903525276. [DOI] [Google Scholar]
- 16.Baird SdH, Jocobus; Ozler, Berk (2011) Income shocks and adolescent mental health. Policy research working paper. The world bank development research group, poverty and inequality team, Washington D.C. World Bank Document. Accessed 13 July 2021
- 17.Patel V, Flisher AJ, Hetrick S, McGorry P. Mental health of young people: a global public-health challenge. Lancet. 2007;369(9569):1302–1313. doi: 10.1016/S0140-6736(07)60368-7. [DOI] [PubMed] [Google Scholar]
- 18.Patel V, Saxena S, Lund C, Thornicroft G, Baingana F, Bolton P, Chisholm D, Collins PY, Cooper JL, Eaton J, Herrman H, Herzallah MM, Huang Y, Jordans MJD, Kleinman A, Medina-Mora ME, Morgan E, Niaz U, Omigbodun O, Prince M, Rahman A, Saraceno B, Sarkar BK, De Silva M, Singh I, Stein DJ, Sunkel C, Unützer J. The lancet commission on global mental health and sustainable development. Lancet. 2018;392(10157):1553–1598. doi: 10.1016/S0140-6736(18)31612-X. [DOI] [PubMed] [Google Scholar]
- 19.Global Burden of Disease Study 2017 Results (2017) http://vizhub.healthdata.org/gbd-compare/. Accessed 13 July 2021
- 20.Kieling C, Baker-Henningham H, Belfer M, Conti G, Ertem I, Omigbodun O, Rohde LA, Srinath S, Ulkuer N, Rahman A. Child and adolescent mental health worldwide: evidence for action. Lancet. 2011;378(9801):1515–1525. doi: 10.1016/S0140-6736(11)60827-1. [DOI] [PubMed] [Google Scholar]
- 21.Reiss F. Socioeconomic inequalities and mental health problems in children and adolescents: a systematic review. Soc Sci Med. 2013;90:24–31. doi: 10.1016/j.socscimed.2013.04.026. [DOI] [PubMed] [Google Scholar]
- 22.Costello EJ, Erkanli A, Copeland W, Angold A. Association of family income supplements in adolescence with development of psychiatric and substance use disorders in adulthood among an American Indian population. JAMA. 2010;303(19):1954–1960. doi: 10.1001/jama.2010.621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Palmer GN, Jenny, Carr, Jane, Kenway, Peter . Monitoring poverty and social exclusion 2003. York, United Kingdom: Joseph Rowntree foundation; 2003. [Google Scholar]
- 24.Beardslee WR, Chien PL, Bell CC. Prevention of mental disorders, substance abuse, and problem behaviors: a developmental perspective. Psychiatric Serv (Wash DC) 2011;62(3):247–254. doi: 10.1176/ps.62.3.pss6203_0247. [DOI] [PubMed] [Google Scholar]
- 25.Knapp M, Evans-Lacko S. Health economics. Rutter's Child Adolesc Psychiatry. 2015 doi: 10.1002/9781118381953.ch18. [DOI] [Google Scholar]
- 26.Angeles G, de Hoop J, Handa S, Kilburn K, Milazzo A, Peterman A. Government of Malawi's unconditional cash transfer improves youth mental health. Soc Sci Med. 2019;225:108–119. doi: 10.1016/j.socscimed.2019.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lund C, De Silva M, Plagerson S, Cooper S, Chisholm D, Das J, Knapp M, Patel V. Poverty and mental disorders: breaking the cycle in low-income and middle-income countries. Lancet. 2011;378(9801):1502–1514. doi: 10.1016/S0140-6736(11)60754-X. [DOI] [PubMed] [Google Scholar]
- 28.Barry MM, Clarke AM, Jenkins R, Patel V. A systematic review of the effectiveness of mental health promotion interventions for young people in low and middle income countries. BMC Public Health. 2013;13(1):835. doi: 10.1186/1471-2458-13-835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Patel V, Kleinman A. Poverty and common mental disorders in developing countries. Bull World Health Organ. 2003;81(8):609–615. [PMC free article] [PubMed] [Google Scholar]
- 30.Thirthalli J, Venkatesh BK, Kishorekumar KV, Arunachala U, Venkatasubramanian G, Subbakrishna DK, Gangadhar BN. Prospective comparison of course of disability in antipsychotic-treated and untreated schizophrenia patients. Acta Psychiatr Scand. 2009;119(3):209–217. doi: 10.1111/j.1600-0447.2008.01299.x. [DOI] [PubMed] [Google Scholar]
- 31.Lawal RA, Adelekan ML, Ohaeri JU, Orija OB. Rehabilitation of heroin and cocaine abusers managed in a Nigerian psychiatric hospital. East Afr Med J. 1998;75(2):107–112. [PubMed] [Google Scholar]
- 32.Skeen S, Laurenzi CA, Gordon SL, du Toit S, Tomlinson M, Dua T, Fleischmann A, Kohl K, Ross D, Servili C, Brand AS, Dowdall N, Lund C, van der Westhuizen C, Carvajal-Aguirre L, Eriksson de Carvalho C, Melendez-Torres GJ. Adolescent mental health program components and behavior risk reduction: a meta-analysis. Pediatrics. 2019;144:2. doi: 10.1542/peds.2018-3488. [DOI] [PubMed] [Google Scholar]
- 33.Burgess RA, Jain S, Petersen I, Lund C. Social interventions: a new era for global mental health? Lancet Psychiatry. 2019 doi: 10.1016/s2215-0366(19)30397-9. [DOI] [PubMed] [Google Scholar]
- 34.Lund C, Brooke-Sumner C, Baingana F, Baron EC, Breuer E, Chandra P, Haushofer J, Herrman H, Jordans M, Kieling C, Medina-Mora ME, Morgan E, Omigbodun O, Tol W, Patel V, Saxena S. Social determinants of mental disorders and the sustainable development goals: a systematic review of reviews. Lancet Psychiatry. 2018;5(4):357–369. doi: 10.1016/s2215-0366(18)30060-9. [DOI] [PubMed] [Google Scholar]
- 35.Bauer A, Garman E, McDaid D, Pabon MA, Hessel P, Díaz Y, Baltra RA, Lund C, Malvasi P, Matijasevich A, Park A-L, Paula CS, Ziebold C, Zimmerman A, Evans-Lacko S (2021) Integrating Youth Mental Health into Cash Transfer Programmes in response to the COVID-19 Crisis in Low- and Middle-income Countries. Lancet Psychiatry 8(4):340–346. 10.1016/s2215-0366(20)30382-5 [DOI] [PMC free article] [PubMed]
- 36.Alves FJO, Machado DB, Barreto ML. Effect of the Brazilian cash transfer programme on suicide rates: a longitudinal analysis of the Brazilian municipalities. Soc Psychiatry Psychiatr Epidemiol. 2019;54(5):599–606. doi: 10.1007/s00127-018-1627-6. [DOI] [PubMed] [Google Scholar]
- 37.Christian C, Roth, C (2016) Can Cash Transfers Prevent Suicides? Experimental Evidence From Indonesia. https://www.aeaweb.org/conference/2017/preliminary/paper/5Dt2Kkft. Accessed 13 July 2021
- 38.Christian C, Hensel L, Roth C. Income shocks and suicides: causal evidence from Indonesia. Rev Econ Statis. 2019;101(5):905–920. doi: 10.1162/rest_a_00777. [DOI] [Google Scholar]
- 39.Kilburn K, Thirumurthy H, Halpern CT, Pettifor A, Handa S. Effects of a large-scale unconditional cash transfer program on mental health outcomes of young people in Kenya. J Adolesc Health Off Publ Soc Adolesc Med. 2016;58(2):223–229. doi: 10.1016/j.jadohealth.2015.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Baird S, Ferreira FHG, Özler B, Woolcock M. Conditional, unconditional and everything in between: a systematic review of the effects of cash transfer programmes on schooling outcomes. J Develop Effective. 2014;6(1):1–43. doi: 10.1080/19439342.2014.890362. [DOI] [Google Scholar]
- 41.Samuels F, Stavropoulou M. ‘Being able to breathe again’: the effects of cash transfer programmes on psychosocial wellbeing. J Develop Stud. 2016;52(8):1099–1114. doi: 10.1080/00220388.2015.1134773. [DOI] [Google Scholar]
- 42.Eyal K. Follow the child: the effect of an unconditional cash transfer on adolescent human capital and mental health. Cape Town, South Africa: University of Cape Town; 2016. [Google Scholar]
- 43.Attah R, Barca V, Kardan A, MacAuslan I, Merttens F, Pellerano L. Can social protection affect psychosocial wellbeing and why does this matter? Lessons from cash transfers in Sub-Saharan Africa. J Develop Stud. 2016;52(8):1115–1131. doi: 10.1080/00220388.2015.1134777. [DOI] [Google Scholar]
- 44.Beegle K, Coudouel A, Monsalve Montiel E (2018) Realizing the Full Potential of Social Safety Nets in Africa. Africa Development Forum. Washington, DC: World Bank. https://openknowledge.worldbank.org/handle/10986/29789. Accessed 13 July 2021
- 45.Baird S, McIntosh C, Özler B. Cash or condition? Evidence from a cash transfer experiment *. Q J Econ. 2011;126(4):1709–1753. doi: 10.1093/qje/qjr032. [DOI] [Google Scholar]
- 46.Prosperidad Social DPS (2017) Informe de la Evaluación de Impacto del Programa Jóvenes en Acción. http://centrodedocumentacion.prosperidadsocial.gov.co/Documentos%202019/JeA/Evaluaciones/Evaluacio%CC%81n%20de%20Impacto%20del%20Programa%20Jo%CC%81venes%20en%20Accio%CC%81n-Resumen%20ejecutivo%20-%20Dic%202017.pdf. Accessed 13 July 2021
- 47.García S, Saavedra JE. Educational impacts and cost-effectiveness of conditional cash transfer programs in developing countries: a meta-analysis. Rev Edu Res. 2017;87(5):921–965. doi: 10.3102/0034654317723008. [DOI] [Google Scholar]
- 48.Creswell JW. Research design: qualitative, quantitative, and mixed methods approaches. 4. California: SAGE Publications; 2014. [Google Scholar]
- 49.Dunning T. Natural experiments in the social sciences: a design-based approach. Strategies for Social Inquiry: Cambridge University Press, Cambridge; 2012. [Google Scholar]
- 50.VanderWeele TJ. Explanation in causal inference: methods for mediation and interaction. New York: Oxford University Press; 2015. [Google Scholar]
- 51.Chisholm D, Heslin M, Docrat S, Nanda S, Shidhaye R, Upadhaya N, Jordans M, Abdulmalik J, Olayiwola S, Gureje O, Kizza D, Mugisha J, Kigozi F, Hanlon C, Adugna M, Sanders R, Pretorius C, Thornicroft G, Lund C. Scaling-up services for psychosis, depression and epilepsy in sub-Saharan Africa and South Asia: development and application of a mental health systems planning tool (OneHealth) Epidemiol Psychiatric Sci. 2017;26(3):234–244. doi: 10.1017/S2045796016000408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Glaser BG, Strauss AL. The discovery of grounded theory: Strategies for qualitative research. Hawthorne, New York: Aldine; 1967. [Google Scholar]
- 53.COREQ (Consolidated Criteria for Reporting Qualitative Studies) In Guidelines for reporting health research. User's Manual. 2014 doi: 10.1002/9781118715598.ch21. [DOI] [Google Scholar]
- 54.World Bank (2015) Mind, Society and Behavior: World Development Report World Bank Group Washington DC. World Development Report 2015: Mind, Society, and Behavior (worldbank.org). Accessed 13 July 2021
- 55.Fiszbein A, Schady N. Conditional cash transfers. World Bank Policy Research Report: World Bank Group, Washington D.C; 2009. [Google Scholar]
- 56.Soares S (2012) Bolsa família, its design, its impacts and possibilities for the future. Working papers 89. International policy centre for inclusive growth. print capa wp 89.pmd (ipcig.org). Accessed 13 July 2021
- 57.Ministério da Cidadania . O que é o bolsa família. Secretaria Especial do Desenvolvimento Social: Ministério da Cidadania; 2019. [Google Scholar]
- 58.Seekings J. Deserving individuals and groups: justifying the shape of South Africa's welfare state. Centre for Social Science Research: University of Cape Town, Cape Town; 2007. [Google Scholar]
- 59.NIDS (2019) National Income Dynamics Study (2008–2019). University of Cape Town. http://www.nids.uct.ac.za/. Accessed 13 July 2021
- 60.Blattman CJ, Julian C.; Sheridan, Margaret (2016) Reducing crime and violence: experimental evidence on adult noncognitive investments in Liberia. Policy research working paper. world bank group, development economics vice presidency, development policy department, Washington D.C. World Bank Document. Accessed 13 July 2021
- 61.World Bank Open Data (2019) World Bank. https://data.worldbank.org/. Accessed 06 April 2020
- 62.WHO (2017) Mental Health ATLAS 2017. World Health Organization. https://www.who.int/mental_health/evidence/atlas/mental_health_atlas_2017/en/. Accessed 13 July 2021
- 63.Docrat S, Besada D, Cleary S, Daviaud E, Lund C. Mental health system costs, resources and constraints in South Africa: a national survey. Health Policy Plan. 2019;34(9):706–719. doi: 10.1093/heapol/czz085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Azzopardi PS, Hearps SJC, Francis KL, Kennedy EC, Mokdad AH, Kassebaum NJ, Lim S, Irvine CMS, Vos T, Brown AD, Dogra S, Kinner SA, Kaoma NS, Naguib M, Reavley NJ, Requejo J, Santelli JS, Sawyer SM, Skirbekk V, Temmerman M, Tewhaiti-Smith J, Ward JL, Viner RM, Patton GC. Progress in adolescent health and wellbeing: tracking 12 headline indicators for 195 countries and territories, 1990–2016. Lancet. 2019;393(10176):1101–1118. doi: 10.1016/S0140-6736(18)32427-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data sources for the quantitative analysis are secondary sources, which are already publicly available. For the qualitative data analysis, data are not fully shareable as some of the will contain identifiable information. However, findings from the analysis will be published together with details on the research methods and tools.
Not applicable.