Abstract
Objective
To examine the trajectory of psychosomatic symptoms and to explore the impact of psychosomatic symptoms on setup error in patients undergoing breast cancer radiotherapy.
Methods
A total of 102 patients with early breast cancer who received initial radiotherapy were consecutively recruited. The M.D. Anderson Symptom Inventory (MDASI) and three different anxiety scales, i.e., the Self-Rating Anxiety Scale (SAS), State-Trait Anxiety Inventory (STAI), and Anxiety Sensitivity Index (ASI), were used in this study. The radiotherapy setup errors were measured in millimetres by comparing the real-time isocratic verification film during radiotherapy with the digitally reconstructed radiograph (DRR). Patients completed the assessment at three time points: before the initial radiotherapy (T1), before the middle radiotherapy (T2), and before the last radiotherapy (T3).
Results
The SAS and STAI-State scores of breast cancer patients at T1 were significantly higher than those at T2 and T3 (F=24.44, P<0.001; F=30.25, P<0.001). The core symptoms of MDASI were positively correlated with anxiety severity. The setup errors of patients with high SAS scores were greater than those of patients with low anxiety levels at T1 (Z=−2.01, P=0.044). We also found that higher SAS scores were associated with a higher risk of radiotherapy setup errors at T1 (B=0.458, P<0.05).
Conclusions
This study seeks to identify treatment-related psychosomatic symptoms and mitigate their impact on patients and treatment. Patients with early breast cancer experienced the highest level of anxiety before the initial radiotherapy, and then, anxiety levels declined. Patients with high somatic symptoms of anxiety may have a higher risk of radiotherapy setup errors.
Keywords: Psychosomatic symptom, anxiety, setup error, radiotherapy, breast cancer
Introduction
The quality of radiotherapy is a key element in the treatment of breast cancer (1). Breast cancer radiotherapy has entered the era of precision treatment, and setup errors are one of the important indicators to measure the accuracy of radiotherapy.
Radiotherapy setup errors include errors caused by the treatment system that cannot be reduced or eliminated and errors caused by changes in setup and anatomical position (respiratory motion, tumour size, etc.) during treatment (2). Research on breast cancer radiotherapy mainly focuses on radiotherapy technology, curative effects, and dosimetry, while research on the psychological aspects of patients undergoing radiotherapy is limited.
Anxiety is a common psychiatric symptom in cancer patients (3-6). Lewis et al. (7) repeatedly assessed the state anxiety levels of patients with breast cancer undergoing radiotherapy. The results showed that 5%−16% of breast cancer patients experienced clinically relevant anxiety during the entire treatment process. However, in their study, state anxiety was only measured with a single-item visual analogue scale instead of a validated questionnaire. In patients scheduled to receive chemotherapy for breast cancer and colorectal cancer, patients with high trait anxiety are particularly likely to require additional support, as they tend to continuously feel more anxious throughout treatment (8). While not a commonly observed barrier to successful delivery of radiation for breast cancer, anxiety is an important study endpoint in and of itself.
Considering that the dimensionality of anxiety complaints may have important implications, different types of anxiety scales were developed (9). Somatic symptoms found in anxiety disorders are manifested in many systems, including musculoskeletal (e.g., muscle tension, trembling), cardiovascular (e.g., palpitations, tachycardia), respiratory (e.g., constriction in chest, dyspnoea), gastrointestinal (e.g., nausea, diarrhoea), genitourinary (e.g., frequency of micturition, urgency), and skin (e.g., flushing, sweating) systems. The Self-Rating Anxiety Scale (SAS) was developed primarily as a measure of somatic symptoms associated with anxiety response (9).
The State-Trait Anxiety Inventory (STAI) (10) was developed based on Spielberger’s anxiety model, which differentiates between state and trait anxiety. State anxiety represents a transitory emotional state as a reaction to a particular stressor, e.g., being diagnosed with cancer, fluctuating over time. Trait anxiety, on the other hand, is a stable susceptibility or proneness to experience anxiety and is regarded as a vulnerability factor for adverse reactions to stress.
Anxiety sensitivity is the fear of anxiety-related sensations. According to Reiss’s theory, anxiety sensitivity amplifies fear and anxiety reactions and plays an important role in the aetiology and maintenance of anxiety disorders. The Anxiety Sensitivity Index (ASI) appears to tap 2 primary aspects of anxiety sensitivity: fears of somatic sensations of anxiety and fears of loss of mental control (11).
The goal of the current study was to evaluate the anxiety levels and trajectories of patients with early breast cancer undergoing radiotherapy and to examine the relationship between anxiety levels and radiotherapy setup errors. We hypothesized that the time point before the initial radiotherapy was the most anxiety-provoking situation and that the high somatic symptoms of anxiety would affect the radiotherapy setup errors.
Materials and methods
Study design
The study was a longitudinal cohort study. Patient’s anxiety level and radiotherapy setup errors were assessed separately just before the initial radiotherapy (T1) (SAS, STAI, ASI), before the middle radiotherapy (T2) (SAS, STAI-State) and before the last radiotherapy (T3) (SAS, STAI-State) in the waiting room of radiotherapy. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Institutional Review Board of the Peking University Cancer Hospital (No. 2014KT54). All patients provided written informed consent.
Participant recruitment
The study recruited breast cancer patients who were admitted to the Department of Radiation Oncology in Peking University Cancer Hospital from June to November 2018. The inclusion criteria were as follows: 1) age ≥18 years old; 2) diagnosed with early breast cancer patients (stage I or II); 3) prepared to have initial radiotherapy; and 4) could understand the questionnaire. The exclusion criteria were as follows: 1) history of major severe mental disorders, unable to cooperate with the investigator; or 2) poor physical condition as judged by the attending physician and not suitable for participation in the study.
Study measures
Demographic information and disease characteristics data were assessed at baseline, including age, gender, marital status, educational level, occupational status, economic status and medical condition.
The M.D. Anderson Symptom Inventory (MDASI) is a widely used symptom inventory with 19 items (13 items for symptom severity, 6 items for interference), and scores range from 0 (“Nothing”) to 10 (“Most severe”). A psychometric study has shown that the Chinese version of the MDASI has good reliability and validity, so the Chinese MDASI can be used to measure the severity of multiple symptoms and their impact on function in Chinese cancer patients.
SAS (12) was used to assess the frequency of anxiety symptoms based on diagnostic conceptualizations. It consists primarily of somatic symptoms. This scale contains 20 items ranging from 1 (“no or very little time”) to 4 (“most or all of the time”). The SAS yields a total score that ranges from 20 to 80, and higher scores indicate a greater anxiety level. According to the Chinese norm, scores exceeding a cut-off of 50 are considered to indicate an anxiety state.
A 40-item STAI (13) widely used measurement of state and trait anxiety. Each subscale consists of 20 items that are rated on a 4-point scale. The first 20 items were used to assess the state of anxiety level, and the last 20 items were used to assess the patients’ trait anxiety level. The total score range for each subscale is 20−80, with higher scores indicating higher anxiety. According to the Chinese norm, a STAI-State score ≥48 indicates the presence of anxiety, and a STAI-Trait score ≥49 indicates the presence of anxiety traits.
ASI (14) contains 18 items and is divided into three subscales: physical concerns, cognitive concerns and social concerns. Items are rated on a 5-point Likert-type response scale ranging from 0 to 4. For further analyses, we used the combined sum score (range, 0−72), with a higher score having an increased risk for the development of anxiety disorder.
For the radiotherapy setup errors, patient localization computerized tomography (CT) was used to delineate the treatment target area and digitally reconstruct the digitally reconstructed radiograph (DRR) image. After the simulator is reset, intensity-modulated radiotherapy is performed on the linear accelerator. The treatment is aligned with the body surface marking line, which is based on the end of inhalation, using portal vision technology. The body position verification image is taken in the direction of the illumination field, and the verification image is compared with the DRR image to obtain radiotherapy setup errors. Because the mammary gland is soft tissue and there is edema, the chest wall is the main contrast, and the breast contour is supplemented. The setup accuracy of patients in the radiotherapy is evaluated in millimetres (mm) using the ventral direction errors (Vrt), the head and foot direction errors (Lng), and the left and right direction errors (Lat). According to expert consensus, it is generally believed that radiotherapy is accurate when the patients’ setup errors are <5 mm. We used a mean of 3 mm as the cut-off point. In the study, the maximum of three directions of errors during each radiotherapy was selected to reflect the maximum positional change between the patients’ actual position and the simulated positioning DRR image.
Statistical analysis
Descriptive analysis of each scale score and radiotherapy setup error data and repeated measure analysis of variance (ANOVA) to explore the trend of anxiety level were performed. Least significant difference (LSD) was used for those variables with statistically significant differences. The Wilcoxon rank sum test was used to compare the setup errors of patients with high anxiety levels and low anxiety levels. The correlation between anxiety and setup errors was analyzed using the Chi-square test. SAS, STAI-State, STAI-Trait and ASI scores were ranked, with the top 27% being in the high anxiety group and the last 27% of patients being defined as the low anxiety group. The Wilcoxon rank sum-test was used to analyze the setup errors of patients in high anxiety group and low anxiety group. Finally, multiple linear regression analysis was used to examine the association of setup errors and variables adjusted by sample demographics and some key covariates. Linear regression requires that residuals conform to normal analysis and are independent of each other, so PP chart and histogram are used to explore whether the residuals conform to normal distribution. Durbin-Watson is used to test whether the residuals in linear regression model are independent of each other. The variance inflation factor (VIF) is used to judge whether there is collinearity among variables. All statistical analyses were performed using IBM SPSS Statistics (Version 20.0; IBM Corp., New York, USA). All the statistical tests used were two-tailed, and a P<0.05 was considered statistically significant.
Results
Patients’ baseline characteristics
A total of 106 patients were enrolled in the study. The data from 102 participants were analyzed, as four participants refused to complete the follow-up study. The patients were all females with an average age of 51±8.7 years. The baseline characteristics of all participants are summarized in Table 1. Most patients were married and completed the surgical operation.
Table 1. Baseline characteristics of study participants (N=102).
| Characteristics | n (%) |
| ER, estrogen receptor; PR, progesterone receptor; HER2, human epidermal growth factor receptor 2. | |
Age (year) (
 ) )
|
50.5±8.7 |
| Marital status | |
| Married | 93 (91.2) |
| Divorced | 4 (3.9) |
| Widowed | 5 (4.9) |
| Educational level (year) | |
| ≤9 | 18 (17.6) |
| >9 | 84 (82.4) |
| Occupational status | |
| Farmer | 9 (8.8) |
| Worker | 21 (20.6) |
| Office worker | 27 (26.5) |
| Professional skill worker | 20 (19.6) |
| Individual business | 2 (2.0) |
| Unemployed | 2 (2.0) |
| Other | 21 (20.6) |
| Type of adjuvant therapy received | |
| Surgery | 102 (100) |
| Chemotherapy | 59 (57.8) |
| Endocrine therapy | 62 (60.8) |
| ER and PR status | |
| ER+ | 78 (76.5) |
| ER− | 23 (22.5) |
| PR+ | 77 (75.5) |
| PR− | 24 (23.5) |
| HER2 status | |
| HER2+ | 79 (77.5) |
| HER2++ | 8 (7.8) |
| HER2+++ | 14 (13.7) |
Anxiety levels and symptoms
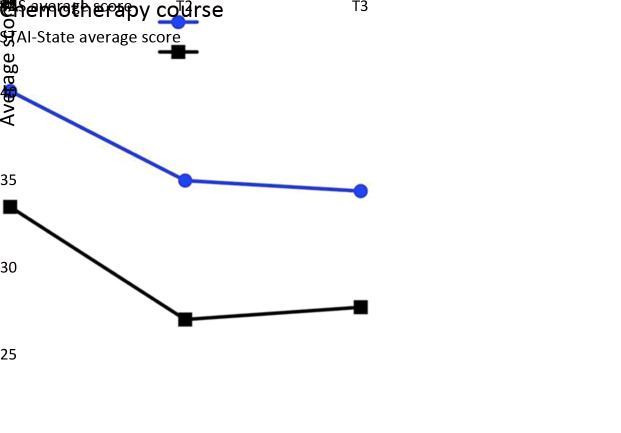
The distribution of SAS and STAI-State score was analyzed using normality test. Both of the SAS and STAI-State scores were following the normal distribution. The differences in SAS and STAI-State scores of T1, T2 and T3 were statistically significant (F=24.44, 30.25, both P<0.001) (Table 2, Figure 1). The results of LSD pair comparison showed that SAS score and STAI-State score at T1 were significantly higher than those at T2 (both P<0.001) and T3 (both P<0.001), and there was no significant difference in SAS and STAI-State scores between T2 and T3 (P=0.618; P=0.592). Almost all the symptoms of MDASI were correlated with anxiety (P<0.05).
Table 2. SAS, STAI, ASI scores and setup errors.
| Variables | T1 | T2 | T3 | F | P |
| SAS, Self-Rating Anxiety Scale; STAI, The State-Trait Anxiety Inventory; ASI, Anxiety Sensitivity Index; T1, before the initial radiotherapy; T2, before the middle radiotherapy; T3, before the last radiotherapy. | |||||
| SAS scores | |||||
|
40.8±9.1 | 35.6±8.7 | 35.0±9.5 | 24.44 | <0.001 |
| Range | 25−71 | 25−61 | 25−62 | − | − |
| STAI-State scores | |||||
|
34.1±10.8 | 27.7±9.1 | 28.4±9.8 | 30.25 | <0.001 |
| Range | 20−71 | 20−60 | 20−58 | − | − |
| STAI-Trait scores | |||||
|
36.5±10.7 | − | − | − | − |
| Range | 21−70 | − | − | − | − |
| ASI scores | − | ||||
|
22.8±14.9 | − | − | − | − |
| Range | 0−67 | − | − | − | − |
Setup errors (mm) (
 ) )
|
2.7±0.1 | 2.7±0.1 | 2.7±0.1 | ||
| Errors ≤3 (n) | 68 | 73 | 69 | − | − |
| Errors >3 (n) | 32 | 27 | 31 | − | − |
Figure 1.
Course of SAS and STAI-State over the course (from T1−T3) of radiotherapy. SAS, Self-Rating Anxiety Scale; STAI, the State-Trait Anxiety Inventory; T1, before the initial radiotherapy; T2, before the middle radiotherapy; T3, before the last radiotherapy.
Radiotherapy setup errors
The average setup errors of radiotherapy at all three time points were the same (2.7±0.1 mm), and the numbers of patients with >3 mm errors at the three time points were 32, 27 and 31 ( Table 2). In addition, the results showed that the patients’ age, marital status, education level, occupation, and treatments were not associated with radiotherapy setup errors.
Anxiety and radiotherapy setup errors
The results showed that according to the SAS score grouping, the setup errors of patients with a high anxiety level at T1 (3.2±0.1) were higher than those of patients with a low anxiety level (2.6±0.1) (Z=−2.01, P=0.044). There was no significant difference between the setup errors of patients with high anxiety levels (2.5±0.1, 2.6±0.1) and patients with low anxiety levels (2.8±0.1, 3.0±0.1) at T2 and T3 (Z=−0.68, P=0.494; Z=−1.01, P=0.314) (Table 3).
Table 3. Setup errors between high and low anxiety level*.
| Course of radiotherapy
|
SAS | STAI-State | STAI-Trait | ASI | |||||||||||
| High | Low | P | High | Low | P | High | Low | P | High | Low | P | ||||
| T1, before the initial radiotherapy; T2, before the middle radiotherapy; T3, before the last radiotherapy; SAS, Self-Rating Anxiety Scale; STAI, The State-Trait Anxiety Inventory; ASI, Anxiety Sensitivity Index; *, SAS, STAI-State, STAI-Trait and ASI scores were ranked, with the top 27% being in the high anxiety group and the last 27% of patients were defined as low anxiety group. | |||||||||||||||
T1 (
 ) )
|
3.2±0.1 | 2.6±0.1 | 0.044 | 2.6±0.1 | 3.0±0.1 | 0.326 | 2.8±0.1 | 2.8±0.1 | 0.788 | 2.6±0.1 | 2.6±0.1 | 0.880 | |||
T2 (
 ) )
|
2.5±0.1 | 2.8±0.1 | 0.494 | 2.7±0.1 | 2.7±0.1 | 0.800 | − | − | − | − | − | − | |||
T3 (
 ) )
|
2.6±0.1 | 3.0±0.1 | 0.314 | 2.6±0.1 | 2.7±0.1 | 0.860 | − | − | − | − | − | − | |||
For the STAI-State grouping, we did not find any significant difference between the setup errors at all three time points; the results were similar for the STAI-Trait and ASI scores (Table 4).
Table 4. Association between SAS and high-risk setup errors at initial radiotherapy.
| SAS scores | n | High-risk errors people (>3 mm) | High-risk errors percentage (%) | χ2 | P |
| SAS, Self-Rating Anxiety Scale. | |||||
| ≥50 | 18 | 10 | 55.56 | 5.597 | 0.018 |
| <50 | 82 | 22 | 26.83 | − | − |
Of the 100 patients (two missing data points), 32 patients had high-risk setup errors (>3 mm) at the initial radiotherapy, and 10 patients were considered to have an anxiety state (SAS score ≥50). A total of 68 patients had low-risk setup errors (≤3 mm), and 8 patients had an anxiety state (SAS score ≥50). Using the Chi-square test of the fourfold table, we found that there was a significant difference in the risk of radiotherapy setup errors between breast cancer patients with and without anxiety before the initial radiotherapy (χ2=5.597, P<0.05) (Table 4). A multiple linear regression model was performed to assess the predictors of radiotherapy setup errors at T1. The Durbin-Watson (DW) value is about 1.82, which shows that the independence of the residuals is acceptable. PP chart and histogram show that the residuals are normally distributed, and linear regression analysis is feasible. The range of VIF is 1.04−1.62, which indicates that there is no multicollinearity problem in this regression analysis. The SAS was positively associated with setup errors, with those reporting higher SAS (B=0.458, P<0.05) experiencing greater setup errors. ASI-cognitive concerns were negatively associated with setup errors (B=−0.376, P<0.05) (Table 5).
Table 5. Multiple linear regression analysis for radiotherapy setup error.
| Dependent variable: setup error | Β* | SE | Β** | t | P | R2 |
| SAS, Self-Rating Anxiety Scale; STAI, The State-Trait Anxiety Inventory; ASI, Anxiety Sensitivity Index; SE, standard error, *, unstandardized coefficients; **, standardized coefficients. | ||||||
| Independent variables | 0.55 | |||||
| SAS | 0.006 | 0.002 | 0.458 | 2.750 | 0.007 | |
| STAI-State | 0.003 | 0.002 | 0.178 | 1.330 | 0.187 | |
| STAI-Trait | 0.004 | 0.002 | 0.338 | 1.840 | 0.069 | |
| ASI-Total | −0.002 | 0.002 | −0.154 | −1.505 | 0.136 | |
| ASI-Physical concerns | 0.003 | 0.003 | 0.136 | 0.881 | 0.381 | |
| ASI-Social concerns | 0.002 | 0.003 | 0.103 | 0.752 | 0.454 | |
| ASI-Cognitive concerns | −0.009 | 0.005 | −0.376 | −2.048 | 0.043 | |
Discussion
This study shows data at different time points to track how the anxiety level changes as treatment progresses, especially when trying to correlate it with setup accuracy. We used multiple anxiety scales to enrich the work, as they may show which scales are more relevant as a potential marker for increased setup difficulty.
There were many somatic symptoms during radiotherapy. Some symptoms tend to be aggravated with the progress of radiotherapy, such as pain, which affects the quality of life of patients. The results of our study show that the core symptoms are positively correlated with the anxiety level of patients. Some studies have shown that there is a great correlation between the symptom burden and anxiety of patients with breast cancer. Therefore, it is suggested that the control of symptoms in radiotherapy should also be considered.
The anxiety level of breast cancer patients was the highest before the initial radiotherapy and decreased significantly with the progress of radiotherapy. This trajectory applied to both somatic anxiety and state anxiety, which is consistent with a previous study (7). Studies have shown that many patients do not understand radiotherapy itself and possible side effects (e.g., visceral damage, skin damage, pain, fatigue) before radiotherapy or lack contact with radiotherapy professionals, which may cause fear of the unknown (15). Anxiety during the initial radiotherapy may also be related to certain characteristics of the radiotherapy environment (e.g., waiting room, linear accelerator room) (16). Thus, as radiotherapy progresses, a significant drop in anxiety levels reflects the patient’s adaptation to treatment and may be related to the support provided by the radiation therapy team after the start of treatment.
Similar processes involving a decline in anxiety levels have been reported in patients treated with surgery and chemotherapy. Lien et al. (17) highlighted social support as an important driver for adjustment and anxiety attenuation. Schneider et al. (8) provided an explanation that could be due to the high overall performance status of the patient sample. These factors might also play a role in radiotherapy treatment and may have contributed to the observed downtrend in anxiety ratings.
For radiotherapy setup errors, we found that in patients with different levels of SAS, there were significant differences in radiotherapy setup errors. A similar analysis was performed between the STAI/ASI and radiotherapy setup errors, but we did not find any significant difference. In recognition of the importance of somatic complaints in anxiety disorders, many self-report measures of anxiety incorporating items assessing somatic concerns have been developed. The SAS may be a better instrument than existing anxiety measures for assessing the somatic symptoms of anxiety given its broader content sampling of such symptoms (9). Somatic symptoms involved in many systems, including musculoskeletal symptoms (e.g., muscle tension, trembling), may affect the patient’s setup position, which may affect the patient’s radiotherapy setup errors.
Our study also supports that in the first day treatment setup, which could detect underlying anxiety, such as a warning sign, providers might be better equipped to point patients experiencing elevated anxiety towards interventions to address psychosocial concerns for improving patients’ quality of life.
This study suggests that the anxiety of patients with early breast cancer radiotherapy needs our attention, and alleviating anxiety before radiotherapy can make them better receive radiotherapy. Patients with higher somatic symptoms of anxiety may have a higher risk of radiotherapy setup errors. Concerns regarding somatic anxiety before the initial radiotherapy may be warranted.
The results of this study can improve our understanding of the anxiety of breast cancer patients during radiotherapy and provide data support for the development of precision radiotherapy. Compared with previous studies on the trend of anxiety levels during radiotherapy (7), our study selected standardized and widely used scales and explored the relationship between anxiety and setup errors.
However, the sample size is limited, so a large sample study is needed for further verification. Because of the lack of a control group in the study, it was not possible to determine whether patients’ anxiety was associated with radiation therapy or was related to the initial treatment and therefore was nonspecific anxiety. Additionally, in the actual radiotherapy implementation process, due to the strict requirements for the fixation of body position, the analysis of setup errors in the study was limited. Only setup errors were used as the observation index, which failed to fully reflect the influences of anxiety for the whole process of radiotherapy setup. Additionally, some information that may affect the setup errors has not been collected, such as axillary dissection. In future studies, we should add objective observation indexes, such as the time course and times of posture adjustments of patients on the radiotherapy bed.
Conclusions
Our study explored the trend of anxiety levels in patients with early breast cancer during radiotherapy. Patients experienced the highest level of anxiety before the initial radiotherapy, and then, anxiety levels declined. Patients with high somatic symptoms of anxiety may have a higher risk of radiotherapy setup errors. Our findings provide a better understanding of psychosocial factors that affect radiotherapy precision.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Acknowledgements
None.
Contributor Information
Yi He, Email: tanglili_cpos@126.com.
Chang Gao, Email: tanglili_cpos@126.com.
Lili Tang, Email: tanglili_cpos@126.com.
References
- 1.Begg AC, Stewart FA, Vens C Strategies to improve radiotherapy with targeted drugs. Nat Rev Cancer. 2011;11:239–53. doi: 10.1038/nrc3007. [DOI] [PubMed] [Google Scholar]
- 2.Cuijpers JP, Dahele M, Jonker M, et al Analysis of components of variance determining probability of setup errors in CBCT-guided stereotactic radiotherapy of lung tumors. Med Phys. 2017;44:382–8. doi: 10.1002/mp.12074. [DOI] [PubMed] [Google Scholar]
- 3.Fritzsche K, Liptai C, Henke M Psychosocial distress and need for psychotherapeutic treatment in cancer patients undergoing radiotherapy. Radiother Oncol. 2004;72:183–9. doi: 10.1016/j.radonc.2004.03.015. [DOI] [PubMed] [Google Scholar]
- 4.Hopwood P, Sumo G, Mills J, et al START Trials Management Group. The course of anxiety and depression over 5 years of follow-up and risk factors in women with early breast cancer: results from the UK Standardisation of Radiotherapy Trials (START) Breast. 2010;19:84–91. doi: 10.1016/j.breast.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 5.Kawase E, Karasawa K, Shimotsu S, et al Estimation of anxiety and depression in patients with early stage breast cancer before and after radiation therapy. Breast Cancer. 2012;19:147–52. doi: 10.1007/s12282-010-0220-y. [DOI] [PubMed] [Google Scholar]
- 6.Stiegelis HE, Ranchor AV, Sanderman R Psychological functioning in cancer patients treated with radiotherapy. Patient Educ Couns. 2004;52:131–41. doi: 10.1016/s0738-3991(03)00021-1. [DOI] [PubMed] [Google Scholar]
- 7.Lewis F, Merckaert I, Liénard A, et al Anxiety and its time courses during radiotherapy for non-metastatic breast cancer: a longitudinal study. Radiother Oncol. 2014;111:276–80. doi: 10.1016/j.radonc.2014.03.016. [DOI] [PubMed] [Google Scholar]
- 8.Schneider A, Kotronoulas G, Papadopoulou C, et al Trajectories and predictors of state and trait anxiety in patients receiving chemotherapy for breast and colorectal cancer: Results from a longitudinal study. Eur J Oncol Nurs. 2016;24:1–7. doi: 10.1016/j.ejon.2016.07.001. [DOI] [PubMed] [Google Scholar]
- 9.Olatunji BO, Deacon BJ, Abramowitz JS, et al Dimensionality of somatic complaints: factor structure and psychometric properties of the Self-Rating Anxiety Scale. J Anxiety Disord. 2006;20:543–61. doi: 10.1016/j.janxdis.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 10.Spielberger, C. State-trait Anxiety Inventory: A Comprehensive Bibliography. The second edition. Palo Alto: Consulting Psychologists Press, 1989.
- 11.Taylor S, Cox BJ An expanded anxiety sensitivity index: evidence for a hierarchic structure in a clinical sample. J Anxiety Disord. 1998;12:463–83. doi: 10.1016/s0887-6185(98)00028-0. [DOI] [PubMed] [Google Scholar]
- 12.Zung WW A rating instrument for anxiety disorders. Psychosomatics. 1971;12:371–9. doi: 10.1016/S0033-3182(71)71479-0. [DOI] [PubMed] [Google Scholar]
- 13.Shek DT The Chinese version of the State-Trait Anxiety Inventory: its relationship to different measures of psychological well-being. J Clin Psychol. 1993;49:349–58. doi: 10.1002/1097-4679(199305)49:3<349::aid-jclp2270490308>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 14.Cai W, Dong W, Pan Y, et al Reliability, validation and norms of the Chinese version of Anxiety Sensitivity Index 3 in a sample of military personnel. PLoS One. 2018;13:e0201778. doi: 10.1371/journal.pone.0201778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Halkett GK, Kristjanson LJ, Lobb E, et al Information needs and preferences of women as they proceed through radiotherapy for breast cancer. Patient Educ Couns. 2012;86:396–404. doi: 10.1016/j.pec.2011.05.010. [DOI] [PubMed] [Google Scholar]
- 16.Mose S, Budischewski KM, Rahn AN, et al Influence of irradiation on therapy-associated psychological distress in breast carcinoma patients. Int J Radiat Oncol Biol Phys. 2001;51:1328–35. doi: 10.1016/s0360-3016(01)01711-4. [DOI] [PubMed] [Google Scholar]
- 17.Lien CY, Lin HR, Kuo IT, et al Perceived uncertainty, social support and psychological adjustment in older patients with cancer being treated with surgery. J Clin Nurs. 2009;18:2311–9. doi: 10.1111/j.1365-2702.2008.02549.x. [DOI] [PubMed] [Google Scholar]