Abstract
Objective
Before the COVID-19 pandemic, elder abuse affected one in 10 American older adults annually. It has been assumed that the pandemic has brought with it a surge in elder abuse due to individuals ordered to stay at home combined with increased interpersonal stressors. However, empirical evidence is lacking. This study aims to estimate the prevalence of, and risk and resilience factors of elder abuse during the pandemic.
Methods
The survey was conducted via two online platforms during April 23 and May 5, 2020, when all states had stay-at-home orders. The final cohort consisted of a sociodemographically diverse sample of 897 older persons in the United States. The prevalence of elder abuse was evaluated by a validated measure previously used in a population-based study of elder abuse. Pandemic-related factors were examined at the community, relational, and individual contexts. We conducted multivariate logistic regression analyses to examine determinants of elder abuse.
Results
One in five older persons in the study sample (n = 191; 21.3%) reported elder abuse, an increase of 83.6% from prevalence estimates before the pandemic. In the final models, sense of community emerged as a persistent protective factor for elder abuse (odds ratio [OR]: 0.89, 95% confidence interval [CI]: 0.85–0.93). At the relational level, physical distancing was associated with reduced risk of elder abuse (OR: 0.94, 95% CI: 0.90–0.98). At the individual level, financial strain was associated with increased risk of abuse (OR: 1.08, 95% CI: 1.02–1.14).
Conclusion
Health care professionals and policy makers must be prepared to address the increase in elder abuse associated with the evolving pandemic.
Key Words: Elder abuse, COVID-19, older adults, social determinants of health
INTRODUCTION
Elder abuse represents a highly prevalent public health problem with serious social, economic, and health consequences. Before the pandemic, elder abuse affected one in ten American older adults annually.1 The World Health Organization defines elder abuse as “a single, or repeated act, or lack of appropriate action, occurring within any relationship where there is an expectation of trust which causes harm or distress to an older person.”2
Even though elder abuse data collected during the pandemic is lacking, experts at the World Health Organization and United Nations have warned about the possible increase in elder abuse during the ongoing public health crisis based on previous crises.3 , 4 Existing studies have shown that interpersonal violence tends to increase and intensify during times of unrest, including during economic downfalls and natural catastrophes.5 , 6
The ecological model of elder abuse7 , 8 is particularly well-suited to identify risk factors for abuse that are likely exacerbated during the pandemic. The framework systematically characterizes the interaction between older persons and their surrounding relational, community, and social dynamics. Its capacity to capture contextual factors across various levels of influence also holds direct implications for prevention programming.9 According to this framework, we examined three pandemic-related factors that may be associated with older persons’ vulnerability and resilience against abuse.
At the community-level, positive attachment to one's community has been shown to reduce elder abuse, because individuals who view themselves as part of a larger network are likely to derive a stronger sense of resilience and self-mastery in face of adversity.10 However, to what extent the positive community-level cohesion, in the form of a stronger sense of community, could buffer against the proliferation of pandemic stressors for elder abuse remain unknown. Examining the association between abuse and sense of community would also contribute to designing community-based elder abuse prevention programs that extend beyond conventional individual or relationship prevention initiatives.
At the relational level, having strong and diverse social relationships tends to protect older persons from abuse.11 , 12 Existing relationships and interactional patterns may be disrupted during the evolving pandemic due to public health prevention measures, such as practicing physical-distancing from people outside one's own household.13 The extended periods of close contacts with potential abusers in the same household may also put relationships under strain and exacerbate conflict.14 On the other hand, maintaining physical distancing is recommended for reducing the spread of the virus.15 Understanding the link between physical distancing and risk of elder abuse is necessary for ensuring the safety of older persons.
At the individual level, financial strain due to wide-spread economic downturn may affect negative interpersonal interactions, a link that is well-documented in interpersonal violence scholarship.16 Unlike objective markers of financial resources, such as income levels, financial strain captures one's own psychological perception of economic pressure.17 Financial strain could jeopardize family well-being directly by triggering hostile and disruptive interactions, or indirectly via collective concerns about future economic outlook.18 , 19 Both mechanisms have been shown to precipitate family violence.20 Whether or not the adverse effects of financial strain extend to risk of elder abuse during a crisis has not been investigated.
The present investigation will be the first to provide estimates of self-reported elder abuse victimization in a relatively large (n = 897), socioeconomically, and racial/ethnically diverse older person sample. We hypothesize that 1) prevalence of elder abuse will be higher during the pandemic than previous nonpandemic studies; 2) at the community level, greater sense of community during the pandemic will be associated with reduced risk of abuse; 3) at the relational level, adherence of physical distancing will be associated with increased risk of abuse; and 4) at the individual level, older persons who experience greater pandemic-related financial strain will be at increased risk of abuse.
METHODS
Population
Sample during the COVID-19 pandemic
Our sample consisted of 897 older persons aged 60 years and older recruited through two online crowd-sourcing platforms, Amazon MTurk and Lucid. Two platforms were utilized in order to expedite recruitment and increase participants' diversity.21 Eligibility criteria for our study included 60 years and older, ability to read and write English, and U.S. residence. Participants were recruited through a double opt-in process. They first opted in as a platform panel member, and then opted-in again to take part in the online survey on Qualtrics, if they were eligible. All 50 U.S. states implemented stay-at-home orders during the data collection period between April 23 and May 5, 2020. Participants missing birth year were excluded (n = 2). In the final study sample, mean age was 68.9 (SD = 5.3), 64.3% women, and 30.7% of racial/ethnic minority membership. The majority of the participants had at least some college education (84.0%), were married (52.6%), and self-identified in good health (40.0%). All participants provided online informed consent. This study was approved by the institutional review board at Yale University.
Comparison samples before the COVID-19 pandemic
The comparison samples were from the National Elder Mistreatment Study (NEMS), and prevalence survey study conducted by the National Social Life, Health, and Aging Project (NSHAP) investigators.1 , 22 These two population-based studies are the few investigations to date with available nationally representative elder abuse prevalence estimates. Conducted prior to the pandemic, both studies utilized area probability sampling frame with NEMS sampled 5,777 older persons aged between 60 and 97 years and NSHAP sampled 3,005 participants between 57 and 85 years old.
Predictors
Sense of community was a three-item scale included in the longitudinal Midlife in the United States Study (MIDUS).23 Participants were asked to indicate the extent to which they agree with the following statements from 1 (strongly disagree) to 7 (strongly agree): 1) “I feel close to other people in my community,” 2) “My community is a source of comfort,” and 3) “I don't feel I belong to anything I'd call a community.” Responses to item three were reverse coded. Higher scores indicate higher levels of sense of community. Cronbach's α was 0.86 in the study.
Adherence to physical distancing behavior was a four-item measure that represented pandemic preventive action recommendations from the Centers for Disease Control and Prevention.15 Older persons indicated whether or not they have carried out physical distancing practice since the pandemic from 1 (not a priority) to 6 (essential), including “practiced physical distancing (staying six feet apart from each other),” “only leaving home for essential reasons,” “avoid group gathering,” and “avoid going to stores often.” Higher scores indicated greater physical-distancing. Cronbach's α was 0.89 in the study.
Pandemic-related financial strain was a three-item measure adapted from the Pew Center Survey24 on a scale ranging from 1 (not at all) to 5 (a great deal): 1) how much has the pandemic affected you financially, 2) how much has stock market downturn affected you financially? 3) how much stress has economic changes due to pandemic caused you? Total score ranged from 5 to 15 with higher scores indicated greater strain. Cronbach's α was 0.72 in the study.
Outcome Measure
To assess elder abuse, we adapted a 10-item elder abuse assessment25 , 26 by asking participants if they experienced any of the 10 incidents since the beginning of the pandemic. Items in this assessment were originally derived from the Hwalek-Sengstok Elder Abuse Screening Test (H-S/EAST) and the Vulnerability to Abuse Screening Scale (Hwalek & Sengstock, 1986; Schofield & Mishra, 2003 27 , 28). Both measures were among the first and most widely-used self-reported assessment tools for elder abuse, with items that determined older persons’ vulnerability to abuse, scenarios of coercion, dejection, direct abuse, and potentially abusive situations. In this study, participants were asked: “Since the beginning of the pandemic, has anyone close to you ever behaved in the following ways.” The incidents included whether “someone close tried to hurt or harm them;” “nobody wanted them around;” and they were “afraid of someone in the family.” These questions evaluated important indicators of abuse and mistreatment. Three questions in the assessment were identical as the outcome measures in NEMS and NSHAP that enabled us to compare results across studies. A response of “yes” to any one of the 10 questions would indicate abuse. This 10-item assessment has shown good reliability, content validity, and convergent validity.26 Participants who screened positive were subsequently asked to appraise the seriousness of the experience, and whether or not the incidents have happened more frequently during the pandemic, compared to before. Cronbach's α was 0.91 in the study.
Covariates
Covariates were chosen based on literature and selected a-priori,12 including age (continuous), sex (binary), race/ethnicity (White vs minority), education (continuous), marital status (married, separated or divorced, widowed, never married), household living arrangement (live alone, single-generation, two-family-generation, multigenerational), and self-rated health (continuous).
Analysis
Descriptive statistics were used to examine the overall proportion of older persons who screened positive to elder abuse. We calculated the absolute difference (%) and used chi-square tests (x 2) to compare prevalence during and before the pandemic.
To assess risk and resilience factors for elder abuse, data analyses were proceeded in two ways. First, the comparison between groups with and without experience of elder abuse was carried out using x 2 for categorical and independent samples t tests for continuous variables. Second, we conducted multivariate logistic regression analyses to determine the unique contribution of each risk and resilience factor for predicting elder abuse while controlling for covariates. We checked model fit of all regression models based on Hosmer and Lemeshow Goodness-of-Fit Test. Multicollinearity and heteroscedasticity were evaluated based on tolerance, variance inflation factor diagnostics values. We presented data as mean and standard deviation for numeric variables, and for categorical variables we presented their frequencies and percentages. The level of statistical significance was set at α = 0.05 (two-tailed). All statistical analyses were conducted using SAS, Version 9.2 (SAS Institute Inc., Cary, NC).
Results
In bivariate analyses, participants who screened positive to elder abuse were significantly younger (t = 2.23, df = 893, p = 0 .027), more likely to reside in larger households (x 2 = 7.83, def = 3, p = 0.049), and in poorer health (x 2 = 14.41, df = 3, p = 0.002). Participants with elder abuse also demonstrated significantly lower sense of community (t = −6.98, df = 893, p < 0.001), lower adherence to physical distance guidelines (t = −3.89, df = 893, p < 0.001), and higher levels of financial strain (t = 3.56, df = 892, p < 0.001). There were no differences with respect to sex, race, education, and marital status, between two groups of participants.
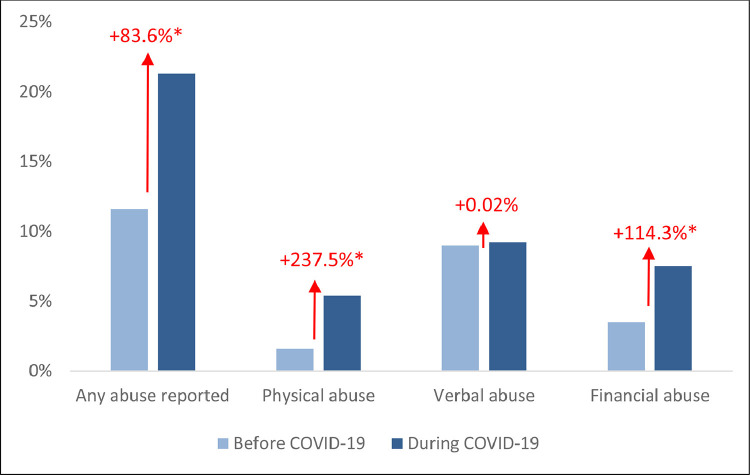
As predicted by hypothesis 1, our findings indicated prevalence of 21.3% elder abuse victimization since the beginning of the pandemic. This is an 83.6% increase from the NEMS cohort that showed a past-year prevalence of 11.6% (experience of at least one type of abuse over the year) (Fig. 1 ).1 The rise in prevalence estimates was statistically significant (x 2 = 93.24, df = 1, p < 0.001). As our estimates only captured prevalence since the pandemic, or approximately 6 weeks prior to data collection, a 1-year prevalence would likely be greater, potentially resulting in a sharper increase than before the pandemic.
FIGURE 1.
Increase of elder abuse prevalence during the COVID-19 pandemica. aElder abuse prevalence before the COVID-19 pandemic was based on two U.S. population-based, nationally-representative studies: The National Elder Mistreatment Study (NEMS), and The National Social Life, Health, and Aging Project (NSHAP). Prevalence of elder abuse during the COVID-19 was based on results in this study, with data collected from April 23 and May 5, 2020. *Two-tailed χ2 analysis conducted for significant testing, with significant level defined as p-value < 0.001.
Subtypes of elder abuse also appeared to be higher during the pandemic (Fig. 1).1 , 22 By using the same item to access financial mistreatment (“someone has taken your money or belongings without your OK”), our findings indicated a prevalence of 7.5%, which is a 114.3% increase from 3.5% detected in the NSHAP cohort (x 2 = 26.07, df = 1, p < 0.001).22 Verbal abuse, assessed by “someone close called you name or put you down,” was similar to that observed in the NSHAP cohort measured by the same item (9.2% versus 9.0%, x 2 = 0.02, df = 1, p = 0.87).22 The NEMS cohort reported an overall physical abuse prevalence of 1.6%, whereas our study found that 5.4% older persons reported that someone close tried to hurt or harm them during the pandemic (x 2 = 767.49, df = 1, p < 0.001). This is an increase of 237.5%.
Of the subset of participants who experienced elder abuse, more than one in three (38.4%) reported these incidents as serious. One in four (24.9%) reported that the incidents have happened more frequently during the pandemic, compared to before.
In the final adjusted models (Table 1 ), as predicted by hypothesis 2, greater sense of community was associated with reduced risk of abuse (OR: 0.89, 95% CI: 0.86–0.93, Wald x 2 = 24.25, df = 1, p < 0.001). Contrary to prediction by hypothesis 3, greater physical distancing was associated with reduced risk of abuse (OR: 0.94, 95% CI: 0.89–0.98, Wald x 2 = 7.29, df = 1, p = 0.007). Last, supporting hypothesis 4, we found that higher pandemic-related financial strain was associated with increased risk of abuse (OR: 1.08, 95% CI: 1.02–1.14, Wald x 2 = 6.54, df = 1, p = 0.01). Independent variables in the final adjusted model had tolerance of 0.95 or above and variance inflation factor of 1.19 or below, which suggests no multicollinearity.
TABLE 1.
Factors that Predict Elder Abuse
| Bivariate Models | Multivariate Models | |
|---|---|---|
| OR (95% CI) | ||
| Sense of community | 0.88 (0.84–0.91)⁎⁎⁎ | 0.89 (0.86–0.93)⁎⁎⁎ |
| Physical distancing | 0.93 (0.89–0.96)⁎⁎⁎ | 0.94 (0.89–0.98)⁎⁎ |
| Financial strain | 1.10 (1.04–1.16)⁎⁎⁎ | 1.08 (1.02–1.14)* |
| Age (reference 60–69) | ||
| 70–79 | 0.59 (0.41–0.84)* | 0.67 (0.45–0.99)* |
| 80+ | 0.92 (0.41–2.08) | 1.35 (0.54–3.34) |
| Female (reference: male) | 0.85 (0.61–1.18) | 0.91 (0.63–1.32) |
| Minority race/ethnicity (reference: White) | 0.98 (0.69–1.39) | 0.97 (0.66–1.42) |
| Education (reference: postgraduate) | ||
| High school or less | 0.61 (0.34–1.10) | 0.66 (0.35–1.26) |
| Some college | 0.94 (0.60–1.48) | 1.00 (0.61–1.66) |
| College | 1.01 (0.63–1.62) | 1.11(0.67–1.84) |
| Marital status (reference: married) | ||
| Separated or divorced | 0.98 (0.65–1.46) | 0.75(0.42–1.34) |
| Widowed | 0.71 (0.41–1.23) | 0.53(0.25–1.12) |
| Never married | 1.23 (0.75–2.00) | 1.03 (0.54–1.97) |
| Living arrangement (reference: living alone) | ||
| One-generation family | 0.94 (0.64–1.36) | 0.72 (0.39–1.32) |
| Two-generation family | 1.58 (1.00–2.48)* | 1.43 (0.82–2.49) |
| Three-generation family | 1.77 (0.80–3.95) | 1.74 (0.70–4.32) |
| Self-rated health (reference: poor health) | ||
| Excellent or very good | 0.25 (0.10–0.60) ⁎⁎ | 0.38 (0.14–1.04) |
| Good | 0.41 (0.17–0.96)* | 0.56 (0.21–1.51) |
| Fair | 0.41 (0.16–1.00) | 0.51 (0.19–1.40) |
p < 0.05.
p < 0.01.
p < 0.001.
DISCUSSION
To the best of our knowledge, this is the first study of elder abuse prevalence, risk and protective factors during the ongoing COVID-19 pandemic. Central among the findings is the surge in elder abuse prevalence compared to existent population-based prevalence estimates in the United States.1 , 22 Our findings further lend support to the evolving evidence of increased vulnerability in older persons during the pandemic.29 , 30 Medical professionals and policy makers must be prepared to address the increase in elder abuse associated with the evolving pandemic.
Even though our pandemic elder abuse estimates are substantially higher than nationally representative prevalence of elder abuse estimates from before the pandemic, there are a number of reasons to assume that our pandemic prevalence levels are conservative. In light of digital inequalities in older population and that lower socioeconomic resources and poorer health remain strong risk factors for elder abuse,12 our study sample collected during the pandemic, which consisted of relatively healthy older persons who had access to internet, may not capture those subgroups at most risks of abuse. Considering that we found financial strain was a predictor of elder abuse, it may be that our estimates would have been higher if we included older persons who were not digitally connected. Additionally, we followed the focused definition of elder abuse guided by the World Health Organization.2 This typology excludes other forms of elder safety violation, such as elder self-neglect and stranger-perpetrated financial fraud and scam. Thus, our prevalence only focused on abuse and mistreatment perpetrated by someone in a position of trust. Nonetheless, the high prevalence of elder abuse found in our study coincides with burgeoning commentaries and editorials that speculated increasing elder abuse during the pandemic.30 , 31
A key contribution of the current study includes the exploration of community-level protective factors for abuse during the pandemic, an important area for designing elder abuse prevention that remains understudied.12 Building and expanding on the well-established protective role of social engagement against elder abuse,1 we found that older persons with a stronger sense of community were less likely to experience abuse during the pandemic. Additionally, the protective effects of community remained above and beyond the negative impact of existing risk factors including financial strain. Identifying and creating supportive environmental mechanism that foster older persons’ sense of community should continue to be a policy priority.
At the relational level, we found that individuals who adhered to physical distancing practicing behaviors were less likely to experience abuse. This is contrary to the widely held hypothesis that physical distancing may uniformly exacerbate sense of isolation and therefore predispose older persons to greater risk of abuse.5 The mechanism between physical distancing and elder abuse remains unclear. Preliminary evidence suggests that adherence to physical distancing was associated with the uptake of conventional health promoting behaviors.32 Thus, it could be that older persons who adhere to physical distancing guidelines may hold active problem-solving strategies and positive coping appraisals that mitigate against risk of abuse.33 Another postulation may be that older persons who engage in physical distancing would be doing so for the greater good of the community,34 in which case the enhanced social connection buffers against risk for elder abuse. It is also plausible that older persons’ adherence to physical distancing helps keep perpetrators at bay.
Another contribution of our study was to examine a previously unexplored link between pandemic-related financial strain and risks for elder abuse victimization. It could be that the perceived economic uncertainty reported by older persons reflected the adverse financial impact on the family as a whole, rendering older persons vulnerable to abuse. Perceived financial strain could also constrain victims’ willingness and access to help-seeking resources during and after traumatic events.35 The extent to which financial strain impinges differentially across subgroups of at-risk older persons to affect abuse victimization merits further attention.
A limitation of our study was that we based our analysis of change in elder abuse prevalence estimates on different cross-sectional studies rather than on the same cohort of older persons over time. However, as NEMS and NSHAP are nationally representative cohort studies that used the same items we used to assess elder abuse, they are the most ideal prepandemic baseline proxy for elder abuse prevalence for our study. Also, considering that our pandemic sample was less likely to capture those in poorer health, those with less resources, and at higher risk of abuse victimization, it is likely that our study provides a conservative estimate of the prevalence of elder abuse during the pandemic. Further, even though the magnitude of effects were small to moderate in this study, small effect sizes can yield meaningful health outcomes on a population level. To illustrate, the association between sense of community and reduced risk for elder abuse (OR: 0.89, 95% CI: 0.86–0.63) indicated that 0.89 people could experience elder abuse for everyone who does not, which may translate to 890,000 people who could experience abuse for every 1 million who does not. This could make a difference of 110,000 less older persons at risk of abuse. Future intervention programming that strengthens older persons’ sense of community could potentially yield population-level changes in preventing elder abuse.
Our findings carry a few important implications for health care providers in helping to increase the safety and health of their older patients. First, as more than one in three elder abuse cases in this study identified these incidents as serious, collaborative efforts to enhance victims’ help-seeking knowledge and behavior is vital.36 Medical professionals, including health care providers and first responders, all play a critical role to screen at-risk patients at this time. Continuing training for health care professionals’ awareness of increased risk and knowledge of local support options and services can help streamline medical community's preparedness and responses for elder abuse cases.
It is necessary that the medical community review their existing protocols for identifying and supporting victims of elder abuse at this time. Considering telemedicine has become an emerging norm of care in the COVID-19 era, it could present novel screening opportunities to uncover cases that would otherwise go undetected during regular in-clinic visits. For instance, medical professionals could closely observe older persons’ physical living environments as well as social interactions with family members; both of which may provide valuable information to detect signs of abuse or neglect. As potential abusers may also be present during telehealth, implementing measures to protect the safety and privacy of the victims are needed. Setting up discrete signals for help during telehealth, such as having “a safe word,” is one channel to facilitate conversation.37 Providers could also be trained to pay close attention to subtle body language as well as comments made by patients and their caregivers.
There is also a need to increase medical training in the detection and management of elder abuse. More than half of the U.S. primary care physicians do not receive any formal training regarding the identification and assessment of elder abuse during their residency.38 This training could be especially valuable if it included information about the how to address elder abuse detected both during a pandemic and through telemedicine.
Another major health care policy implication of this study would be to ensure funding for all families and at-risk older persons to gain access to high-speed internet, hotlines, and shelters. Enhancing the accessibility and availability of help resources and service infrastructure would be particularly critical for families in higher financial distress and those with older persons at home, both during and beyond the COVID-19 crisis.
Furthermore, for health care practitioners developing primary prevention to safeguard older persons from abuse, this study provides insights into how acute economic distress could influence violence against older persons. This aligns with key findings in disaster preparedness scholarship that policy efforts to build individual and family financial resilience could likely mitigate the severity of adverse impact.39
Last, initiatives to augment community connectedness may be more critical now than ever. Potential measures may include building volunteering programs and providing families with access to community outreach initiatives. Collective efforts to encourage the availability and accessibility of community help may be a pragmatic way to promote social support when one adheres to physical distancing guidelines.11 , 12 Strengthening community cohesion as a key structural-level preventive measure for elder abuse may further enhance the public health benefits of physical distancing for all.
The COVID-19 pandemic has exacerbated many social, economic, and health problems to millions of families worldwide. As indicated by our study, it also intensifies another type of persistent, yet preventable, public health burden: increasing cases of elder abuse. The clear needs of safety for older persons must be taken into account in public health action planning during the ongoing pandemic.
Author Contributions
Study concept and design: EC, BL. Acquisition of data: EC, BL. Analysis and interpretation of data: EC, BL. Preparation of manuscript: EC, BL. Resources: BL.
Sponsor's Role: None.
Disclosure
The authors report no conflicts with any product mentioned or concept discussed in this article.
Reference
- 1.Acierno R, Hernandez MA, Amstadter AB. Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: the National Elder Mistreatment Study. Am J Public Health. 2010;100:292–297. doi: 10.2105/AJPH.2009.163089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . World Health Organization; Geneva: 2017. Elder Abuse Fact Sheet. [Google Scholar]
- 3.United Nations . United Nations; Geneva, Switzerland: 2020. “Unacceptable” – UN Expert Urges Better Protection of Older Persons Facing the Highest Risk of the COVID-19 Pandemic. [Google Scholar]
- 4.United Nations . 2020. 2020 World elder abuse awareness day: the impact of COVID-19 on violence, abuse and neglect of older persons. [Google Scholar]
- 5.Boserup B, McKenney M, Elkbuli A. Alarming trends in US domestic violence during the COVID-19 pandemic. Am J Emerg Med. 2020;38:2753–2755. doi: 10.1016/j.ajem.2020.04.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schneider D, Harknett K, McLanahan S. Intimate partner violence in the great recession. Demography. 2016;53:471–505. doi: 10.1007/s13524-016-0462-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Research Council . National Academies Press; Washington, DC.: 2003. Elder Mistreatment: Abuse, Neglect, and Exploitation in An Aging America. [PubMed] [Google Scholar]
- 8.Schiamberg LB, Gans D. Elder abuse by adult children: an applied ecological framework for understanding contextual risk factors and the intergenerational character of quality of life. Int J Aging Hum Dev. 2000;50:329–359. doi: 10.2190/DXAX-8TJ9-RG5K-MPU5. [DOI] [PubMed] [Google Scholar]
- 9.Teresi JA, Burnes D, Skowron EA. State of the science on prevention of elder abuse and lessons learned from child abuse and domestic violence prevention: Toward a conceptual framework for research. J Elder Abuse Negl. 2016;28:263–300. doi: 10.1080/08946566.2016.1240053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Greenfield EA, Marks NF. Sense of community as a protective factor against long-term psychological effects of childhood violence. Soc Serv Rev. 2010;84:129–147. doi: 10.1086/652786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johannesen M, LoGiudice D. Elder abuse: a systematic review of risk factors in community-dwelling elders. Age Ageing. 2013;42:292–298. doi: 10.1093/ageing/afs195. [DOI] [PubMed] [Google Scholar]
- 12.Pillemer K, Burnes D, Riffin C. Elder abuse: Global situation, risk factors, and prevention strategies. Gerontologist. 2016;56(Suppl 2):S194–S205. doi: 10.1093/geront/gnw004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Usher K, Bhullar N, Durkin J. Family violence and COVID-19: Increased vulnerability and reduced options for support. Int J Ment Health Nurs. 2020;29:549–552. doi: 10.1111/inm.12735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Campbell AM. An increasing risk of family violence during the Covid-19 pandemic: Strengthening community collaborations to save lives. Forensic Sci Int Rep. 2020;2 doi: 10.1016/j.fsir.2020.100089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Social distancing: Keeping a safe distance to slow the spread. 2020.
- 16.Capaldi DM, Knoble NB, Shortt JW. A systematic review of risk factors for intimate partner violence. Partner Abuse. 2012;3:231–280. doi: 10.1891/1946-6560.3.2.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gutman LM, McLoyd VC, Tokoyawa T. Financial strain, neighborhood stress, parenting behaviors, and adolescent adjustment in urban African American families. J Res Adolesc. 2005;15:425–449. [Google Scholar]
- 18.Prime H, Wade M, Browne DT. Risk and resilience in family well-being during the COVID-19 pandemic. Am Psychol. 2020;75:631–643. doi: 10.1037/amp0000660. [DOI] [PubMed] [Google Scholar]
- 19.Vinokur AD, Price RH, Caplan RD. Hard times and hurtful partners: how financial strain affects depression and relationship satisfaction of unemployed persons and their spouses. J Personality Soc Psychol. 1996;71:166–179. doi: 10.1037//0022-3514.71.1.166. [DOI] [PubMed] [Google Scholar]
- 20.Schneider W, Waldfogel J, Brooks-Gunn J. The Great Recession and risk for child abuse and neglect. Children Youth Serv Rev. 2017;72:71–81. doi: 10.1016/j.childyouth.2016.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Coppock A, McClellan OA. Validating the demographic, political, psychological, and experimental results obtained from a new source of online survey respondents. Res. Pol. 2019;6 2053168018822174. [Google Scholar]
- 22.Laumann EO, Leitsch SA, Waite LJ. Elder mistreatment in the United States: prevalence estimates from a nationally representative study. J Gerontol B Psychol Sci Soc Sci. 2008;63:S248–S254. doi: 10.1093/geronb/63.4.s248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Keyes C. Social well-being. Social Psychol Quart. 1998;61:121–140. [Google Scholar]
- 24.Pew Research Center. Most Americans say coronavirus outbreak has impacted their lives.2020.
- 25.Dong X, Wang B. Associations of child maltreatment and intimate partner violence with elder abuse in a US Chinese population. JAMA Int Med. 2019;179:889–896. doi: 10.1001/jamainternmed.2019.0313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dong X, Chen R, Fulmer T. Prevalence and correlates of elder mistreatment in a community-dwelling population of U.S. Chinese older adults. J Aging Health. 2014;26:1209–1224. doi: 10.1177/0898264314531617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hwalek MA, Sengstock MC. Assessing the probability of abuse of the elderly: toward development of a clinical screening instrument. J Appl Gerontol. 1986;5:153–173. [Google Scholar]
- 28.Schofield MJ, Mishra GD. Validity of self-report screening scale for elder abuse: Women's Health Australia Study. Gerontologist. 2003;43:110–120. doi: 10.1093/geront/43.1.110. [DOI] [PubMed] [Google Scholar]
- 29.Ayalon L, Chasteen A, Diehl M. Aging in Times of the COVID-19 pandemic: avoiding ageism and fostering intergenerational solidarity. J Gerontol B Psychol Sci Soc Sci. 2020;76:e49–e52. doi: 10.1093/geronb/gbaa051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Han SD, Mosqueda L. Elder abuse in the COVID-19 era. J Am Geriatr Soc. 2020;68:1386–1387. doi: 10.1111/jgs.16496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Elman A, Breckman R, Clark S. Effects of the COVID-19 outbreak on elder mistreatment and response in New York City: initial lessons. J Appl Gerontol. 2020 doi: 10.1177/0733464820924853. 733464820924853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bourassa KJ, Sbarra DA, Caspi A. Social distancing as a health behavior: county-level movement in the United States during the COVID-19 pandemic is associated with conventional health behaviors. Ann Behav Med. 2020;54:548–556. doi: 10.1093/abm/kaaa049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Storey JE. Risk factors for elder abuse and neglect: A review of the literature. Aggress Violent Behav. 2020;50 [Google Scholar]
- 34.Webster R, Brooks S, Smith L. How to improve adherence with quarantine: rapid review of the evidence. medRxiv. 2020 doi: 10.1016/j.puhe.2020.03.007. 2020.2003.2017.20037408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kahn JR, Pearlin LI. Financial strain over the life course and health among older adults. J Health Soc Behav. 2006;47:17–31. doi: 10.1177/002214650604700102. [DOI] [PubMed] [Google Scholar]
- 36.Burnes D, Lachs MS, Burnette D. Varying Appraisals of elder mistreatment among victims: findings from a population-based study. J Gerontol B Psychol Sci Soc Sci. 2019;74:881–890. doi: 10.1093/geronb/gbx005. [DOI] [PubMed] [Google Scholar]
- 37.Bradley NL, DiPasquale AM, Dillabough K. Health care practitioners’ responsibility to address intimate partner violence related to the COVID-19 pandemic. Can Med Assoc J. 2020;192:E609. doi: 10.1503/cmaj.200634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wagenaar D, Rosenbaum R, Herman S, Page C. Elder abuse education in primary care residency programs: a cluster group analysis. Family Med. 2009;41:481–486. [PubMed] [Google Scholar]
- 39.Mathbor G. Enhancement of community preparedness for natural disasters. Int SocWork. 2007;50:357–369. [Google Scholar]