Abstract
Background:
Lateral extra-articular tenodesis in the context of anterior cruciate ligament (ACL) reconstruction (ACLR) is performed to better control anterolateral knee instability in patients with high-grade preoperative pivot shift. However, some authors believe these procedures may cause lateral compartment overconstraint, affecting knee motion in daily life.
Purpose/Hypothesis:
The primary aim of the present study was to identify kinematic differences during the execution of an activity under weightbearing conditions between knees having undergone ACLR using anatomic single-bundle (SB) versus single-bundle plus lateral plasty (SBLP) techniques. The secondary aim was to compare the postoperative kinematic data with those from the same knees before ACLR and from the healthy contralateral knees in order to investigate if ACLR was able to restore physiologic knee biomechanics during squat execution. The hypotheses were that (1) the SBLP technique would allow a better restoration of internal-external (IE) knee rotation than would SB and (2) regardless of the technique, ACLR would not fully restore physiologic knee biomechanics.
Study Design:
Randomized controlled trial; Level of evidence, 2.
Methods:
In total, 32 patients (42 knees) were included in the study. Patients were asked to perform a single-leg squat before surgery (ACL-injured group, n = 32; healthy contralateral group, n = 10) and at minimum 18-month follow-up after ACLR (SB group, n = 9; SBLP group, n = 18). Knee motion was determined using a validated model-based tracking process that matched patient-specific magnetic resonance imaging bone models to dynamic biplane radiographic images under the principles of roentgen stereophotogrammetric analysis. Data processing was performed using specific software. The authors compared IE and varus-valgus rotations and anterior-posterior and medial-lateral translations among the groups.
Results:
The mean follow-up period was 21.7 ± 4.5 months. No kinematic differences were found between the SB and SBLP groups (P > .05). A more medial tibial position (P < .05) of the ACL-injured group was reported during the entire motor task and persisted after ACLR in both the SB and the SBLP groups. Differences in IE and varus-valgus rotations were found between the ACL-injured and healthy groups.
Conclusion:
There were no relevant kinematic differences between SBLP and anatomic SB ACLR during the execution of a single-leg squat. Regardless of the surgical technique, ACLR failed in restoring knee biomechanics.
Registration:
NCT02323386 (ClinicalTrials.gov identifier).
Keywords: anterior cruciate ligament, lateral extra-articular tenodesis, biplane radiography, in vivo knee kinematics, single-leg squat
The role of lateral extra-articular tenodesis (LET) in anterior cruciate ligament (ACL) reconstruction has been increasingly debated during recent years. The recourse to such a technique has been claimed to overcome the limits of the standard single-bundle (SB) ACL reconstruction in terms of residual laxity and rotatory instability. 7,9,21,24,46,55 Indeed, it is mainly recommended for patients with high-grade preoperative pivot shift or generalized ligamentous laxity and athletes performing cutting maneuvers. 21,22,38,45 Recent studies have shown that the addition of LET to SB reconstruction in these patients guarantees better control of rotatory laxity and reduces ACL reconstruction failures. 22,45
Nonetheless, the effectiveness of LET addition remains controversial; some authors believe it can result in lateral compartment overconstraint, thus being harmful to knee cartilage. 4,12,39,44 In a prospective randomized study, Anderson et al 4 found that patients who underwent an ACL reconstruction plus LET had a higher incidence of motion loss and compartment crepitation. Furthermore, a cadaveric study by Schon et al 44 demonstrated that anatomic anterolateral ligament reconstruction resulted in significant rotational overconstraint of the knee joint for most flexion angles in the setting of a concomitant ACL reconstruction.
For this reason, in North America, LET procedures have been mainly abandoned in the past 20 years for patients not at risk for increased rotatory instability. 21 Recent clinical studies with long-term follow-up have shown that patients who undergo ACL reconstruction with the addition of LET do not have an increased risk of degenerative changes in knee cartilage, 18,22,40,53 but the risk of osteoarthritis is higher after ACL surgery than in healthy knees. 13,14,25 This latter aspect might imply that ACL surgery still has a limited positive long-term effect on surrounding tissues in the knee regardless of the surgical technique adopted.
In such a scenario, biomechanical analyses could be crucial to understand the possible presence of overconstraint and to what extent the physiologic knee motion is restored after ACL surgery. Nevertheless, most of the published biomechanical studies have been conducted in a cadaveric setting or, when in vivo, under nonweightbearing conditions. New technologies, including video analysis, stereometry, and the most accurate radiograph-based tools, allow investigation of knee motion during the active execution of motor tasks. 1,2,5,17,20,25,26,48
The primary aim of the present study was to identify, through a system of dynamic biplane radiographs, kinematic differences during the execution of a single-leg squat in knees having undergone ACL reconstruction with anatomic SB versus SB plus lateral plasty (SBLP). The secondary aim was to compare these postoperative kinematic data with those of the same knees before ACL reconstruction and with those of healthy contralateral knees in order to investigate if ACL surgery was able to restore physiologic knee biomechanics during squat execution. The hypotheses were that (1) the SBLP technique would allow a better restoration of internal-external (IE) knee rotation than would SB and that (2) ACL reconstruction would not fully restore physiologic knee biomechanics regardless of the technique.
Methods
The study protocol was approved by an institutional review board, and all the patients involved signed informed consent forms. This study represents the secondary analysis of data collected from a prospective study aimed at evaluating the outcome of ACL reconstruction. Based on the original study protocol, 62 patients were included and assessed preoperatively using 1.5-T magnetic resonance imaging (MRI) analysis and dynamic roentgen stereophotogrammetric analysis (RSA) of the injured and contralateral knees. The study patients were randomly assigned to undergo ACL reconstruction using the SB, SBLP, or double-bundle (DB) surgical techniques. Simple randomization was performed using a sealed opaque envelope. An orthopaedic resident, who was not a member of the study group, took care of the randomization process. Dynamic RSA evaluation of the 3 groups was performed at a minimum of 18 months postoperatively.
The inclusion criteria for the original study were age 16 to 50 years; complete, traumatic, and unilateral ACL injury; no previous knee ligament reconstruction or repair; no concomitant posterior cruciate ligament, posterolateral corner, lateral collateral ligament, or medial collateral ligament lesion; and absence of mild or advanced knee osteoarthritis (Kellgren-Lawrence grade 3 or 4).
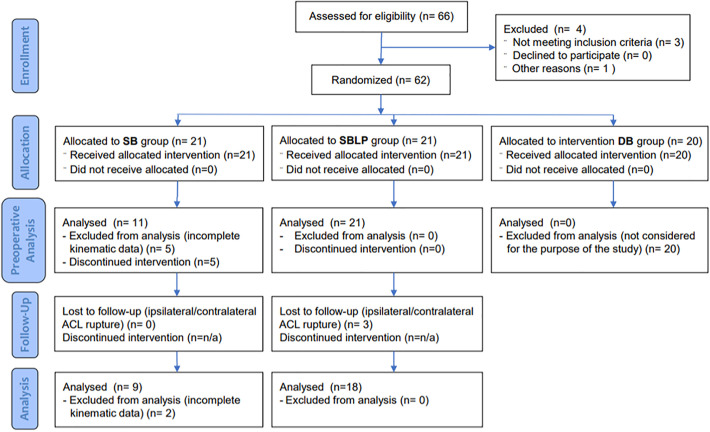
For the purpose of the present study, the inclusion criteria were ACL reconstruction with anatomic SB or SBLP surgical techniques, noncontact ACL injury, and no injury to the contralateral knee. Exclusion criteria were concomitant ligamentous injuries, incomplete kinematic data, and unwillingness to take part in the study (Figure 1). The patients who underwent DB reconstruction were excluded to clarify the focus on the addition of lateral plasty in SB ACL reconstruction.
Figure 1.
CONSORT (Consolidated Standards of Reporting Trials) flow diagram describing the design of the study. ACL, anterior cruciate ligament; DB, double-bundle; SB, single bundle; SBLP, single-bundle plus lateral plasty.
Surgical Techniques
The anatomic SB ACL reconstruction (Figure 2A) was performed as reported by Prodromos and Joyce 42 ; the SBLP ACL reconstruction (Figure 2B) was performed using the over-the-top SB technique with the additional extra-articular tenodesis in the lateral compartment, as reported by Marcacci et al. 36 With regard to SB reconstruction, the starting point of the tibial tunnel was on the medial tibial metaphysis, inclined laterally approximately 65° with respect to the horizontal line and directed to the center of the native ACL tibial insertion. The harvested tendons (semitendinosus and gracilis tendon autografts) were detached from the tibial insertion and quadrupled. A femoral half-tunnel of at least 2.5 cm was drilled from the native ACL footprint. The graft was passed in both tunnels and intra-articularly and then fixed using an Endobutton (Smith & Nephew) against the rigid anterolateral femoral cortex and a bioabsorbable interference screw in the tibial tunnel, the knee at the fixation moment was flexed to 30°, and the posterior tibial drawer was applied.
Figure 2.
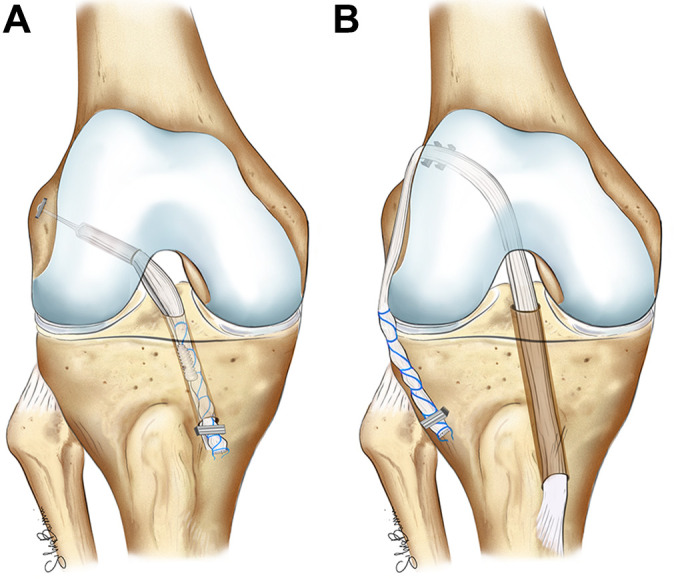
Anterior cruciate ligament reconstructive surgery using (A) single-bundle and (B) single-bundle plus lateral plasty.
In the SBLP reconstruction, the semitendinosus and gracilis tendons were harvested, leaving the tibial insertion intact. The tibial tunnel was drilled with the knee flexed to 35°, aiming at the posteromedial part of the ACL footprint. After a lateral incision proximal to the lateral epicondyle and dissection of the iliotibial band and intermuscular septum, the over-the-top position was reached. The graft was then introduced into the tibial tunnel, into the joint, and outside from the lateral incision. The graft was fixed in the over-the-top position using 2 barbed metal staples (Citieffe) with the knee flexed to 70° and the tibial posterior drawer applied. Finally, the distal part of the graft was passed underneath the fascial layer and fixed below the Gerdy tubercle using a metal staple.
All of the surgeries were performed by a single experienced surgeon (S.Z.), who was not aware of the purposes of the study at the time of the surgery. Patients were blinded to the surgical technique.
Rehabilitation
All patients underwent the same rehabilitation protocol. A knee brace was not used postoperatively. Range of motion, quadriceps muscle active exercises, straight-leg raises, and prone hamstring muscle-stretching exercises were all begun the day after surgery. Patients were allowed partial weightbearing during the first 2 weeks. From the third postoperative day, patients could begin passive and active flexion-extension, starting from 30° and increasing 5° every day until reaching complete range of motion. Three weeks after surgery, full weightbearing was allowed. Cyclette, active knee extension using weights, and one-quarter squats were introduced 4 weeks after surgery. Running was introduced at 2 months, and sports activities were introduced after 4 months. Patients were allowed to return to full sports activities when there was no muscle atrophy of the operated leg, usually after the sixth month.
Data Acquisition
The patients were asked to perform a single-leg squat, according to their abilities. The investigators carefully checked the initial position of the foot in order to limit the bias caused by IE alignment: the foot had to be aligned with the ideal anterior-posterior (AP) axis of the knee, thus pointing forward. The acquisition was performed in a specialized radiographic room. The tasks were performed 3 times, the first 2 to gain comfort with the experimental setup (no radiographic exposure) and the third one for data acquisition (radiographic exposure).
The data were collected using a radiographic setup for dynamic RSA developed in our institute. The specifics of the RSA radiographic setup were analogous to the ones already published in previous articles from the same study group. 1,3,11 In brief, the 2 radiographic tubes and 2 digital flat panels were used. The beamlines were perpendicular to each other and synchronized to acquire contemporary radiographs at 8 frames per second. Three-dimensional bone models of the femur and tibia (obtained from 1.5-T MRI) were positioned according to the radiographs acquired per each frame.
The 6 degrees of freedom kinematic quantitative data were calculated using the Grood and Suntay decomposition in dedicated software in MATLAB (R2016a; MathWorks Inc) using a validated workflow with submillimetric accuracy (0.22 ± 0.46 mm and 0.26° ± 0.2° for the model position and orientation, respectively). 1,10 The test-retest reliability was assessed using a set of repeated tests under different image noise conditions, 27,41 and the average error 8 was <0.48 mm (95% CI, 0.15-0.80 mm). The RSA operator was blinded to the surgical technique.
Because it was impossible to standardize the time elapsed to perform the motor task by each patient, data were normalized to the peak knee flexion angle and divided in a descendant phase, from the initial standing position to the peak knee flexion, and an ascendant phase, from the peak knee flexion to the final standing position.
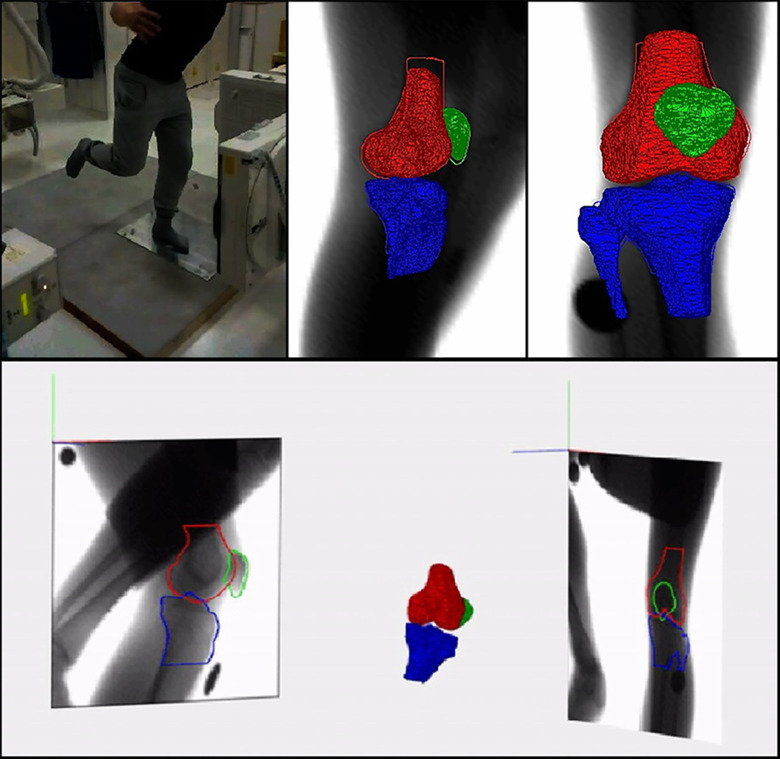
IE and varus-valgus (VV) rotation and AP and medial-lateral (ML) translation were computed and further analyzed (Figure 3).
Figure 3.
Roentgen stereophotogrammetric analysis data elaboration: 3-dimensional models of bones were obtained from magnetic resonance imaging and used in specific software to reproduce the joint movement through a validated tracking system that matched models and dynamic radiographs. Also see Supplemental Figure S1 (available online).
Statistical Analysis
The kinematic data were processed using MATLAB and presented as mean ± SE over the knee flexion angles separately for the descendant and ascendant phases of the single-leg squat. For conciseness in data presentation, kinematic data were grouped every 15° of knee flexion (eg, 0°-15°, 15°-30°, 30°-45°, and 45°-60° for the descendant phase). The maximum peak flexion that patients could comfortably obtain during the single-leg squat was 60°.
The general linear model (unbalanced analysis of variance) was used to assess the statistical differences among the groups along with each frame of the entire motor task for all the parameters. The 2-tailed Student t test was used to compare the single groups with Dunn-Sidak adjustment for post hoc comparisons. Differences were considered statistically significant at P < .05.
An a priori power analysis was conducted to calculate the adequate sample size. Given that no previous studies have been performed comparing 2 surgical ACL reconstructions using similar radiographic/fluoroscopic techniques, the power analysis was based on a previous study comparing IE rotation between ACL-reconstructed and unaffected limbs. 47 In that study, a fluoroscopic technique was used to evaluate knee kinematics on 6 patients. Given an IE rotation difference between the groups of 3.8° ± 2.3° (mean ± standard deviation [SD]), to achieve a power of 0.8 and an α level of .05, the minimum number of patients required was set at 7.
Results
Of the 42 patients who met the inclusion criteria and were enrolled in the study, 32 (30 men, 2 women; mean ± SD age, 26.4 ± 8.7 years) successfully completed the preoperative kinematic assessment. Based on the ACL status, 4 groups were created: ACL-injured group, healthy group, SB group, and SBLP group. Preoperatively, all 32 patients underwent dynamic RSA of the injured knee and were included in the ACL-injured group. From this cohort, 10 patients also underwent dynamic RSA of the healthy contralateral knee and were included in the healthy group. At follow-up, 5 patients did not complete kinematic assessment. Based on the ACL reconstruction technique, postoperative kinematic assessment was performed on 9 patients in the SB group and 18 patients in the SBLP group. The mean ± SD follow-up time for the kinematic assessment was 21.7 ± 4.5 months. The distribution of meniscal lesions was similar in the 2 groups: 1 irreparable and 1 repaired medial meniscal lesion in the SB group (22%) and 2 irreparable and 3 repaired medial meniscal lesions in the SBLP group (28%) (P > .05).
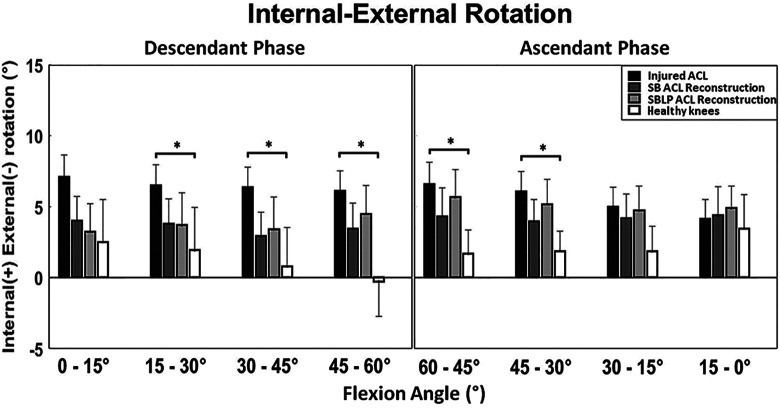
IE Rotation
The ACL-injured group showed statistically significantly higher internal rotation compared with the healthy knee group between 15° and 30° of knee flexion in the descendant phase (P = .0217) and between 30° and 60° in both the descendant and the ascendant phases (P < .05) (Tables 1 and 2, Figure 4).
Table 1.
Kinematic Assessment of the Descendant Phase of the Single-Leg Squat Through Dynamic RSA a
| Rotation, deg | Translation, mm | |||
|---|---|---|---|---|
| Internal-External | Varus-Valgus | Anterior-Posterior | Medial-Lateral | |
| 0°-15° | ||||
| ACL-injured | 7.1 ± 1.6 | –0.4 ± 0.7 b | 4.2 ± 1.1 | 0.2 ± 0.5 b |
| SB | 4.0 ± 1.7 | –0.5 ± 1.0 | 0.2 ± 2.0 | 0.5 ± 1.0 b |
| SBLP | 3.2 ± 2.0 | –1.9 ± 1.0 | 0.7 ± 1.3 c | 0.3 ± 0.7 b |
| Healthy | 2.5 ± 3.0 | –3.0 ± 1.2 | 4.4 ± 2.2 | –1.9 ± 0.9 |
| 15°-30° | ||||
| ACL-injured | 6.5 ± 1.4 b | –1.9 ± 0.8 | 10.1 ± 1.1 | 0.5 ± 0.5 b |
| SB | 3.8 ± 1.7 | –1.8 ± 1.1 | 7.6 ± 2.3 | 0.0 ± 0.8 b |
| SBLP | 3.7 ± 2.3 | –3.0 ± 1.2 | 6.5 ± 1.6 c | –0.2 ± 0.7 b |
| Healthy | 1.9 ± 3.0 | –3.6 ± 1.5 | 9.6 ± 2.4 | –1.7 ± 0.7 |
| 30°-45° | ||||
| ACL-injured | 6.3 ± 1.4 b | –3.3 ± 1.0 | 15.6 ± 0.9 | 0.8 ± 0.5 b |
| SB | 2.9 ± 1.7 | –2.9 ± 1.3 | 14.5 ± 1.5 | 0.4 ± 0.5 |
| SBLP | 3.4 ± 2.3 | –3.5 ± 1.4 | 13.5 ± 1.7 | –0.1 ± 0.8 |
| Healthy | 0.8 ± 2.8 | –5.0 ± 1.9 | 15.5 ± 2.5 | –1.2 ± 0.6 |
| 45°-60° | ||||
| ACL-injured | 6.1 ± 1.4 b | –4.2 ± 1.2 | 20.1 ± 0.9 | 1.3 ± 0.5 b |
| SB | 3.4 ± 1.8 | –3.5 ± 1.6 | 19.1 ± 1.3 | 0.4 ± 0.5 |
| SBLP | 4.5 ± 2.0 | –3.6 ± 1.5 | 20.0 ± 1.4 | 0.6 ± 0.8 b |
| Healthy | –0.3 ± 2.4 | –6.0 ± 1.6 | 20.5 ± 2.4 | –1.4 ± 0.6 |
a All values are reported as mean ± SE. ACL, anterior cruciate ligament; RSA, roentgen stereophotogrammetric analysis; SB, single-bundle; SBLP, single-bundle plus lateral plasty.
b Statistically significant difference compared with the healthy group (P < .05).
c Statistically significant difference compared with the ACL-injured group (P < .05).
Table 2.
Kinematic Assessment of the Ascendant Phase of the Single-Leg Squat Through Dynamic RSA a
| Rotation, deg | Translation, mm | |||
|---|---|---|---|---|
| Internal-External | Varus-Valgus | Anterior-Posterior | Medial-Lateral | |
| 60°-45° | ||||
| ACL-injured | 6.6 ± 1.5 b | –4.2 ± 1.3 | 19.0 ± 0.9 | 0.3 ± 0.5 b |
| SB | 4.3 ± 2.0 | –3.5 ± 1.7 | 18.0 ± 1.4 | 0.1 ± 0.5 |
| SBLP | 5.7 ± 1.9 | –3.9 ± 1.5 | 19.2 ± 1.1 | 0.3 ± 0.8 b |
| Healthy | 1.7 ± 1.7 | –6.9 ± 1.6 | 20.0 ± 2.1 | –2.0 ± 0.6 |
| 45°-30° | ||||
| ACL-injured | 6.1 ± 1.4 b | –3.1 ± 1.0 | 15.3 ± 0.9 | 0.1 ± 0.5 b |
| SB | 3.9 ± 1.6 | –3.0 ± 1.5 | 12.6 ± 1.4 b | –0.1 ± 0.6 b |
| SBLP | 5.2 ± 1.7 | –3.8 ± 1.2 | 13.5 ± 1.3 b | 0.2 ± 0.7 b |
| Healthy | 1.9 ± 1.4 | –5.6 ± 1.7 | 16.4 ± 2.3 | –2.2 ± 0.7 |
| 30°-15° | ||||
| ACL-injured | 5.0 ± 1.3 | –2.1 ± 0.8 b | 9.8 ± 1.0 | 0.0 ± 0.5 b |
| SB | 4.2 ± 1.7 | –1.6 ± 1.1 b | 6.8 ± 2.0 | 0.0 ± 0.7 b |
| SBLP | 4.7 ± 1.7 | –2.5 ± 1.0 | 5.7 ± 1.3 c | –0.1 ± 0.7 b |
| Healthy | 1.8 ± 1.8 | –4.5 ± 1.4 | 9.1 ± 2.8 | –1.8 ± 0.8 |
| 15°-0° | ||||
| ACL-injured | 4.1 ± 1.4 | –0.7 ± 0.8 | 4.0 ± 1.0 | –0.4 ± 0.5 |
| SB | 4.4 ± 2.0 | –0.6 ± 1.0 | 1.0 ± 2.2 | 0.1 ± 0.7 |
| SBLP | 4.9 ± 1.5 | –1.4 ± 1.0 | –1.6 ± 1.4 c | –0.5 ± 0.8 |
| Healthy | 3.5 ± 2.4 | –3.0 ± 1.3 | 2.2 ± 2.2 | –1.1 ± 0.9 |
a All values are reported as mean ± SE. ACL, anterior cruciate ligament; RSA, roentgen stereophotogrammetric analysis; SB, single-bundle; SBLP, single-bundle plus lateral plasty.
b Statistically significant difference compared with the healthy group (P < .05).
c Statistically significant difference compared with the ACL-injured group (P < .05).
Figure 4.
Comparison of knee internal-external rotation among the 4 groups. The asterisk indicates a statistically significant difference (P < .05). ACL, anterior cruciate ligament; SB, single-bundle; SBLP, single-bundle plus lateral plasty.
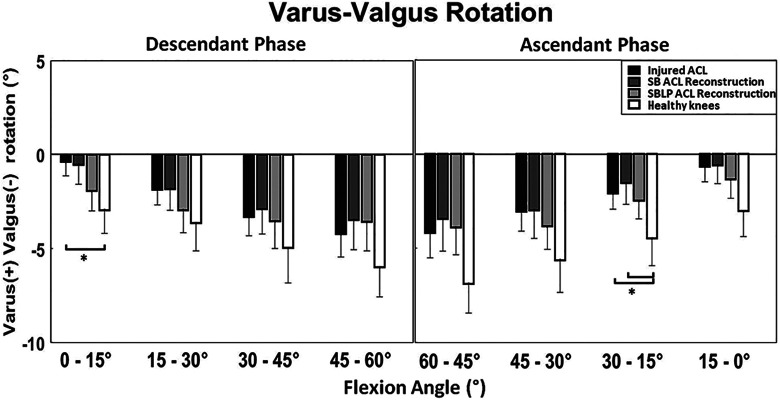
VV Rotation
Statistically significant differences were found between the ACL-injured and healthy knee groups between 0° and 15° of knee flexion in the descendant phase (P = .0144) and between 30° and 15° in the ascendant phase (P = .0227) (Tables 1 and 2, Figure 5). Furthermore, the SB group significantly differed from the healthy group between 30° and 15° in the ascendant phase (P = .0303).
Figure 5.
Comparison of knee varus-valgus rotation among the 4 groups. The asterisk indicates a statistically significant difference (P < .05). ACL, anterior cruciate ligament; SB, single-bundle; SBLP, single-bundle plus lateral plasty.
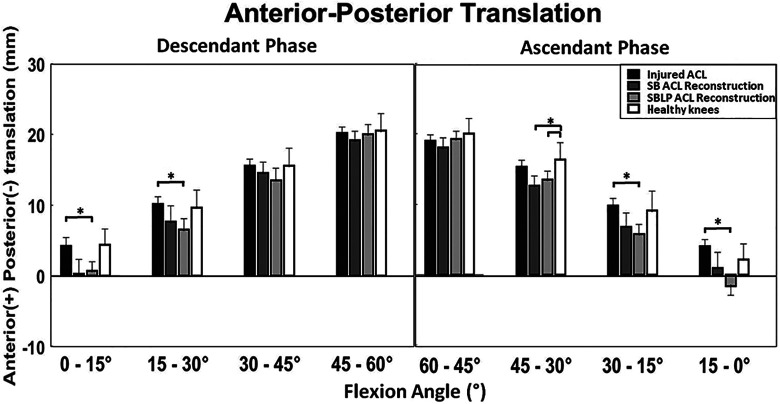
AP Translation
In the ACL-injured group, anterior translation between 0° and 30° of knee flexion was higher compared with the SBLP group in both the descendant and ascendant phases (P < .05) (Tables 1 and 2, Figure 6). Furthermore, anterior translation was higher in both the SB and the SBLP groups (P = .0230 and P = .0466, respectively) compared with the healthy group between 45° and 30° in the ascendant phase.
Figure 6.
Comparison of tibial anterior-posterior translation among the 4 groups. The asterisk indicates a statistically significant difference (P < .05). ACL, anterior cruciate ligament; SB, single-bundle; SBLP, single-bundle plus lateral plasty.
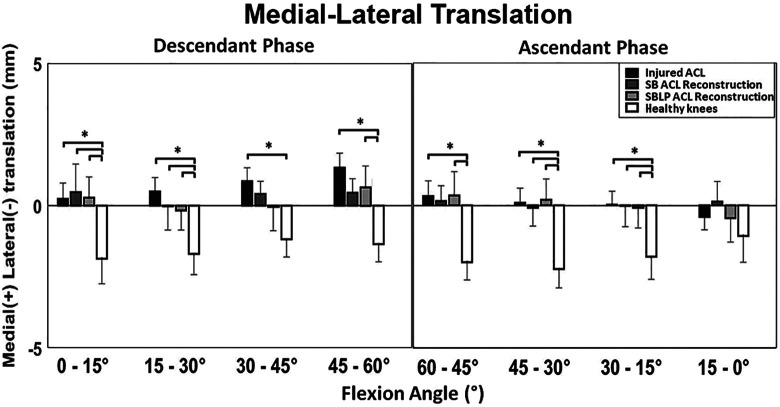
ML Translation
The healthy group showed a lateral tibial alignment during the entire movement that significantly differed from that of the other 3 groups between 0° and 30° in the descendant phase and between 45° and 15° in the ascendant phase (P < .05) (Tables 1 and 2, Figure 7). Furthermore, significant differences were found between 45° and 60° in both the descendant and the ascendant phases between the healthy group and both the ACL-injured and the SBLP groups.
Figure 7.
Comparison of tibial medial-lateral translation among the 4 groups. The asterisk indicates a statistically significant difference (P < .05). ACL, anterior cruciate ligament; SB, single-bundle; SBLP, single-bundle plus lateral plasty.
Discussion
The most important findings of the present study were as follows: (1) no statistically significant differences in knee kinematics were found between anatomic SB and SBLP techniques during a single-leg squat; (2) both techniques improved knee kinematics in terms of IE rotation and VV, making the kinematics comparable with that of the healthy contralateral knee; (3) for both techniques, a more posterior tibial position was found between 45° and 30° of knee flexion in the ascendant phase when compared with the healthy contralateral group; and (4) the tibial position of injured knees was more medial than that of the healthy ones. A significant tibial medialization also remained in the ACL-reconstructed knees.
Based on these findings, our first hypothesis was not confirmed because the SBLP technique group did not differ from either the SB or the healthy knee groups in terms of IE rotation. Moreover, our second hypothesis was confirmed because physiologic knee motion was not fully restored, regardless of the surgical technique, and significant differences remained postoperatively when compared with the healthy knee group.
The present study was the first to investigate kinematic differences between 2 different ACL surgical techniques, in vivo and under weightbearing conditions, through a highly accurate evaluation method based on dynamic biplane radiographs. Previously published studies conducted using analogous technologies (radiostereometry or biplanar fluoroscopy) often had even smaller cohorts and included patients with different reconstruction techniques in the same postoperative group. ¶ Furthermore, because we included ACL-injured and healthy knee groups, it was possible to assess the postoperative kinematics in light of 2 boundary knee conditions.
Regarding the kinematic comparison between the SB and the SBLP groups, LET procedures have regained attention in recent years for their possible implication in the unsolved problem of rotatory laxity persistence after ACL reconstruction. 15,21,22
The previous literature, either in favor of or against the use of LET, was mainly based on cadaveric or intraoperative settings, thus not accounting for real-life knee motion. In contrast, the present study was aimed at evaluating knee kinematics during activities of daily living—thus, in vivo and under weightbearing conditions. Furthermore, the adopted radiographic setup has submillimetric accuracy, has been validated, and has already been used for knee motion analysis in the same context. 1,3,11 In such a scenario, no differences were found between the 2 ACL-reconstructed groups or between both groups and the healthy contralateral knees for IE rotation during a simple and safe motor task like a single-leg squat. In our opinion, this is a robust biomechanical demonstration that the addition of lateral plasty does not cause overconstraint in the context of ACL reconstruction when performing safe motor tasks under weightbearing conditions. The results of the present study, alongside previous evidence asserting that LET reduces pivot-shift laxity and tension on the hamstring graft, 22,45,50 could reinforce the concept of lateral plasty as a safe procedure in the context of ACL reconstruction.
Regarding our second finding, we observed that specific kinematic patterns of the ACL-injured knees that differed from those of the healthy contralateral knees persisted even after surgery. In particular, this was true for VV rotation and AP and ML translation but not for IE rotation. Indeed, ACL-injured knees were more internally rotated than were healthy ones, but ACL reconstruction reduced such discrepancy for both techniques. The results of the present study are in line with those obtained using less accurate methodologies in a large part of the current literature: a wider internal rotation in ACL-deficient knees compared with healthy or ACL-reconstructed ones has been observed in cadaveric studies through rotational tests, 29,34 in gait through video analysis, 5,20 and in squat through monoplanar fluoroscopy. 28 Nonetheless, some contrasting findings are present in the literature. One study by Isberg et al 26 through radiostereometry did not find differences in IE among ACL-injured, ACL-reconstructed, and healthy knees during a weightbearing knee extension. Two more studies using biplanar fluoroscopy found a more externally rotated tibia in ACL-reconstructed knees compared with the contralateral ones during the execution of a single-leg hop. 17,23
The contribution of ACL on restraining VV rotation is a controversial topic. Previous works have demonstrated that ACL deficiency influences knee VV when performing weightbearing activities. 1,47,51 In our study, significant differences were found between ACL-deficient and healthy contralateral knees at low knee flexion angles (<30°) (Figure 3). Moreover, only SB reconstruction was found to be less sound in restoring physiologic VV because statistically significantly more varus persisted between 30° and 15° of knee flexion in the ascendant phase when compared with healthy knees. Such a difference was not present for the SBLP group; this could have happened because the traction practiced in lateral plasty before the fixation on the Gerdy tubercle permits a better restoration of lateral condyle distance from the tibial plateau.
Differences in AP translation between ACL-reconstructed and healthy contralateral knee groups were found at 45° to 30° of knee flexion in the ascendant phase. A similar trend was also found in the rest of the motor task. Hoshino et al, 25 through the same methodology and task, reported a similar finding: the tibia was more posterior in ACL-reconstructed knees than contralateral knees. This aspect could derive from an excessive force applied in the posterior drawer during graft fixation. 28 Previous studies have demonstrated that a posterior tibial load at the moment of graft fixation is useful to reduce anterior tibial subluxation. 24,55 Nonetheless, further studies are needed to understand the maximum entity of the force that should be applied to reproduce the correct sagittal tibiofemoral alignment. The absence of significant differences in AP translation between ACL-injured and healthy knees might appear contradictory. However, co-contraction of knee flexors and extensors has a stabilizing effect on the knee AP translation, while it has a limited effect on the rotational parameters. In this respect, several previous studies have reported that the squat does not highlight knee AP laxity. 1,31,35,49
The ML translation clearly differed between healthy contralateral knees and all the other groups. Indeed, a more medial position of the tibia in the ACL-injured group was found during the entire motor task and also persisted after ACL reconstruction (in the SBLP group for about the entire motor task and in the SB group between 0° and 30° of knee flexion in the descendant phase and between 45° and 30° of knee flexion in the ascendant phase). The concept of tibial medialization under weightbearing has already been observed in previous studies in both ACL-deficient and ACL-reconstructed conditions and in different motor tasks. 1,16,23,32,33 The combination of pathological tibial medialization and varus thrust could explain the higher risk of medial knee osteoarthritis in ACL deficiency and reconstruction. Indeed, the altered force distribution on the medial tibial plateau and tibial spine could contribute to cartilage degeneration of the medial compartment. 19,32,37 Moreover, an interesting paper by Zaid et al 54 correlated kinematic differences in knee flexion-extension and cartilage degeneration between pre- and postoperative injured knees and contralateral knees through weightbearing MRI. Although they observed a restoration of tibial AP translation after reconstruction, a persistent anomaly of cartilage signal in T1ρ was registered. Therefore, degenerative cartilage changes might not necessarily be correlated with AP anomalies but with ML alignment.
The present study has several limitations. First, the overall small sample size, the different number of patients per group, and the high loss of follow-up kinematic data in the SB group were limiting factors. However, the single groups respected the minimum number of patients required for the statistical effectiveness computed through the power analysis. The complexity and high accuracy of the methodology should also be kept in mind. Therefore, in our opinion, the present study can be considered one of the largest in terms of sample size among the ones with such a complex kinematic analysis.
A second limitation regards the motor task evaluated: the squat is a safe exercise for ACL-deficient knees because the co-contraction of knee flexors and extensors compensates for the absence of the ligament in stabilizing the joint in the AP direction. 31,51 More demanding motor tasks, including countermovements or jumps, could have highlighted differences in knee rotation between SB and SBLP techniques or in anterior tibial translation between pre- and postsurgery data. 17,52 To the date, high-dynamics tasks are impossible to analyze using such radiographic setups because of the limited spaces and the obstacles represented by the medical devices available. Furthermore, from an ethical point of view, such movements could have been unsafe for an ACL-injured population. The analysis of a safe task allowed appreciation of biomechanical alterations of knee motion in daily life and investigation of the presence or absence of an overconstraint caused by the addition of the lateral plasty.
Another limitation was the absence of patients selection based on the time from injury. The time from injury could be a confounder for ACL-deficient knee biomechanics because patients might progressively develop muscular asymmetries to stabilize the joint before the surgery. 52 Nevertheless, the present study was mainly focused on the comparison between the 2 surgical techniques. Further studies should be conducted to investigate the influence of injury-to-surgery time and rehabilitation on presurgical knee movement.
The average peak flexion was 60°. Therefore, the results of the present study cannot be extended to higher degrees of knee flexion. The patients were asked to perform a comfortable movement and reach a peak flexion that they could handle stably. Notably, the cohort investigated was not limited to high-level athletic patients, who could probably have achieved higher knee flexion degrees.
Moreover, the surgical techniques adopted were both based on hamstring graft, and the lateral plasty was not one of the “popular LET procedures.” In particular, the lateral plasty was passed above—instead of deep to—the lateral collateral ligament. However, no consensus has been reached yet on which anterolateral reconstruction technique is optimal, 21 and the hamstrings represent one of the most common graft choices for ACL reconstruction. 6,43 Therefore, the present study’s findings should be confirmed using other ACL reconstruction techniques and LET procedures such as anterolateral ligament reconstruction. 46
The last limitation regards the contralateral knees: no kinematic data were available for all the contralateral knees, thus not allowing for a direct longitudinal comparison. Contralateral knees were used as healthy controls, although kinematic differences have been claimed in previous studies. 30,31 However, the recourse to the contralateral knee as a control is predominant in the literature. Moreover, because of radiographic exposure, collecting data from healthy patients would have been highly unethical.
Conclusion
The knee biomechanics of patients undergoing SBLP ACL reconstruction (over-the-top plus lateral plasty) was comparable with that of an anatomic SB ACL reconstruction during the execution of a single-leg squat. Both techniques improved kinematics in terms of VV and IE rotation compared with the ACL-deficient conditions. Moreover, ACL reconstruction did not fully restore physiologic knee behavior.
Supplemental material for this article is available at http://journals.sagepub.com/doi/suppl/10.1177/23259671211011940.
Supplemental Material
Supplemental Material, sj-gif-1-ojs-10.1177_23259671211011940 for Dynamic Radiostereometry Evaluation of 2 Different Anterior Cruciate Ligament Reconstruction Techniques During a Single-Leg Squat by Stefano Di Paolo, Piero Agostinone, Alberto Grassi, Gian Andrea Lucidi, Erika Pinelli, Marco Bontempi, Gregorio Marchiori, Laura Bragonzoni and Stefano Zaffagnini in Orthopaedic Journal of Sports Medicine
Acknowledgment
The authors thank Silvia Bassini for the graphics support.
Footnotes
Final revision submitted February 27, 2021; accepted March 19, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: The authors received funding for this study from the Italian National Health Service. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Rizzoli Orthopaedic Institute (ID No. 40/CE/US/ml).
References
- 1. Agostinone P, Di Paolo S, Grassi A, et al. ACL deficiency influences medio-lateral tibial alignment and knee varus-valgus during in vivo activities. Knee Surg Sports Traumatol Arthrosc. 2021;29(2):389–397. [DOI] [PubMed] [Google Scholar]
- 2. Akpinar B, Thorhauer E, Irrgang JJ, Tashman S, Fu FH, Anderst WJ. Alteration of knee kinematics after anatomic anterior cruciate ligament reconstruction is dependent on associated meniscal injury. Am J Sports Med. 2018;46(5):1158–1165. [DOI] [PubMed] [Google Scholar]
- 3. Alesi D, Marcheggiani Muccioli GM, Roberti di Sarsina T, et al. In vivo femorotibial kinematics of medial-stabilized total knee arthroplasty correlates to post-operative clinical outcomes. Knee Surg Sports Traumatol Arthrosc. 2021;29(2):491–497. [DOI] [PubMed] [Google Scholar]
- 4. Anderson AF, Snyder RB, Lipscomb AB. Anterior cruciate ligament reconstruction: a prospective randomized study of three surgical methods. Am J Sports Med. 2001;29(3):272–279. [DOI] [PubMed] [Google Scholar]
- 5. Andriacchi TP, Dyrby CO. Interactions between kinematics and loading during walking for the normal and ACL deficient knee. J Biomech. 2005;38(2):293–298. [DOI] [PubMed] [Google Scholar]
- 6. Arnold MP, Calcei JG, Vogel N, et al. ACL Study Group survey reveals the evolution of anterior cruciate ligament reconstruction graft choice over the past three decades. Knee Surg Sports Traumatol Arthrosc. Published online January 24, 2021. doi:10.1007/s00167-021-06443-9 [DOI] [PubMed] [Google Scholar]
- 7. Björnsson H, Desai N, Musahl V, et al. Is double-bundle anterior cruciate ligament reconstruction superior to single-bundle? A comprehensive systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23(3):696–739. [DOI] [PubMed] [Google Scholar]
- 8. Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8(2):135–160. [DOI] [PubMed] [Google Scholar]
- 9. Bonanzinga T, Signorelli C, Grassi A, et al. Kinematics of ACL and anterolateral ligament, part II: anterolateral and anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25(4):1062–1067. [DOI] [PubMed] [Google Scholar]
- 10. Bontempi M, Cardinale U, Bragonzoni L, et al. A computer simulation protocol to assess the accuracy of a Radio Stereometric Analysis (RSA) image processor according to the ISO-5725. Preprint. Posted online June 6, 2020. arXiv 2006.03913v1. https://arxiv.org/abs/2006.03913
- 11. Bontempi M, Roberti di Sarsina T, Marcheggiani Muccioli GM, et al. J-curve design total knee arthroplasty: the posterior stabilized shows wider medial pivot compared to the cruciate retaining during chair raising. Knee Surg Sports Traumatol Arthrosc. 2020;28(9):2883–2892. [DOI] [PubMed] [Google Scholar]
- 12. Branch T, Lavoie F, Guier C, et al. Single-bundle ACL reconstruction with and without extra-articular reconstruction: evaluation with robotic lower leg rotation testing and patient satisfaction scores. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):2882–2891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Castoldi M, Magnussen RA, Gunst S, et al. A randomized controlled trial of bone--patellar tendon--bone anterior cruciate ligament reconstruction with and without lateral extra-articular tenodesis: 19-year clinical and radiological follow-up. Am J Sports Med. 2020;48(7):1665–1672. [DOI] [PubMed] [Google Scholar]
- 14. Chalmers PN, Mall NA, Moric M, et al. Does ACL reconstruction alter natural history? A systematic literature review of long-term outcomes. J Bone Joint Surg Am. 2014;96(4):292–300. [DOI] [PubMed] [Google Scholar]
- 15. Claes S, Vereecke E, Maes M, Victor J, Verdonk P, Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat. 2013;223(4):321–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Defrate LE, Papannagari R, Gill TJ, Moses JM, Pathare NP, Li G. The 6 degrees of freedom kinematics of the knee after anterior cruciate ligament deficiency: an in vivo imaging analysis. Am J Sports Med. 2006;34(8):1240–1246. [DOI] [PubMed] [Google Scholar]
- 17. Deneweth JM, Bey MJ, McLean SG, Lock TR, Kolowich PA, Tashman S. Tibiofemoral joint kinematics of the anterior cruciate ligament-reconstructed knee during a single-legged hop landing. Am J Sports Med. 2010;38(9):1820–1828. [DOI] [PubMed] [Google Scholar]
- 18. Devitt BM, Bouguennec N, Barfod KW, Porter T, Webster KE, Feller JA. Combined anterior cruciate ligament reconstruction and lateral extra-articular tenodesis does not result in an increased rate of osteoarthritis: a systematic review and best evidence synthesis. Knee Surg Sports Traumatol Arthrosc. 2017;25(4):1149–1160. [DOI] [PubMed] [Google Scholar]
- 19. Fairclough JA, Graham GP, Dent CM. Radiological sign of chronic anterior cruciate ligament deficiency. Injury. 1990;21(6):401–402. [DOI] [PubMed] [Google Scholar]
- 20. Georgoulis AD, Papadonikolakis A, Papageorgiou CD, Mitsou A, Stergiou N. Three-dimensional tibiofemoral kinematics of the anterior cruciate ligament-deficient and reconstructed knee during walking. Am J Sports Med. 2003;31(1):75–79. [DOI] [PubMed] [Google Scholar]
- 21. Getgood A, Brown C, Lording T, et al. The anterolateral complex of the knee: results from the International ALC Consensus Group Meeting. Knee Surg Sports Traumatol Arthrosc. 2019;27(1):166–176. [DOI] [PubMed] [Google Scholar]
- 22. Getgood AMJ, Bryant DM, Litchfield R, et al. Lateral extra-articular tenodesis reduces failure of hamstring tendon autograft anterior cruciate ligament reconstruction: 2-year outcomes from the STABILITY Study randomized clinical trial. Am J Sports Med. 2020;48(2):285–297. [DOI] [PubMed] [Google Scholar]
- 23. Hofbauer M, Thorhauer ED, Abebe E, Bey M, Tashman S. Altered tibiofemoral kinematics in the affected knee and compensatory changes in the contralateral knee after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42(11):2715–2721. [DOI] [PubMed] [Google Scholar]
- 24. Höher J, Kanamori A, Zeminski J, Fu FH, Woo SL. The position of the tibia during graft fixation affects knee kinematics and graft forces for anterior cruciate ligament reconstruction. Am J Sports Med. 2001;29(6):771–776. [DOI] [PubMed] [Google Scholar]
- 25. Hoshino Y, Fu FH, Irrgang JJ, Tashman S. Can joint contact dynamics be restored by anterior cruciate ligament reconstruction? Clin Orthop Relat Res. 2013;471(9):2924–2931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Isberg J, Faxén E, Laxdal G, Eriksson BI, Kärrholm J, Karlsson J. Will early reconstruction prevent abnormal kinematics after ACL injury? Two-year follow-up using dynamic radiostereometry in 14 patients operated with hamstring autografts. Knee Surg Sports Traumatol Arthrosc. 2011;19(10):1634–1642. [DOI] [PubMed] [Google Scholar]
- 27. ISO 5725-1:1994(en). Accuracy (trueness and precision) of measurement methods and results—part 1: general principles and definitions. Published November 22, 2019. Accessed May 9, 2021. https://www.iso.org/obp/ui/#iso:std:iso:5725:-1:ed-1:v1:en
- 28. Kidera K, Yonekura A, Miyaji T, et al. Double-bundle anterior cruciate ligament reconstruction improves tibial rotational instability: analysis of squatting motion using a 2D/3D registration technique. J Orthop Surg Res. 2018;13(1):111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kondo E, Merican AM, Yasuda K, Amis AA. Biomechanical analysis of knee laxity with isolated anteromedial or posterolateral bundle-deficient anterior cruciate ligament. Arthroscopy. 2014;30(3):335–343. [DOI] [PubMed] [Google Scholar]
- 30. Kozanek M, Van de Velde SK, Gill TJ, Li G. The contralateral knee joint in cruciate ligament deficiency. Am J Sports Med. 2008;36(11):2151–2157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kvist J, Gillquist J. Sagittal plane knee translation and electromyographic activity during closed and open kinetic chain exercises in anterior cruciate ligament-deficient patients and control subjects. Am J Sports Med. 2001;29(1):72–82. [DOI] [PubMed] [Google Scholar]
- 32. Li G, Moses JM, Papannagari R, Pathare NP, DeFrate LE, Gill TJ. Anterior cruciate ligament deficiency alters the in vivo motion of the tibiofemoral cartilage contact points in both the anteroposterior and mediolateral directions. J Bone Joint Surg Am. 2006;88(8):1826–1834. [DOI] [PubMed] [Google Scholar]
- 33. Li G, Papannagari R, DeFrate LE, Yoo JD, Park SE, Gill TJ. The effects of ACL deficiency on mediolateral translation and varus-valgus rotation. Acta Orthop. 2007;78(3):355–360. [DOI] [PubMed] [Google Scholar]
- 34. Lord BR, El-Daou H, Sabnis BM, Gupte CM, Wilson AM, Amis AA. Biomechanical comparison of graft structures in anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):559–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Luque-Seron JA, Medina-Porqueres I. Anterior cruciate ligament strain in vivo: a systematic review. Sports Health. 2016;8(5):451–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Marcacci M, Zaffagnini S, Iacono F, Neri MP, Loreti I, Petitto A. Arthroscopic intra- and extra-articular anterior cruciate ligament reconstruction with gracilis and semitendinosus tendons. Knee Surg Sports Traumatol Arthrosc. 1998;6(2):68–75. [DOI] [PubMed] [Google Scholar]
- 37. Murrell GA, Maddali S, Horovitz L, Oakley SP, Warren RF. The effects of time course after anterior cruciate ligament injury in correlation with meniscal and cartilage loss. Am J Sports Med. 2001;29(1):9–14. [DOI] [PubMed] [Google Scholar]
- 38. Noyes FR, Barber SD. The effect of an extra-articular procedure on allograft reconstructions for chronic ruptures of the anterior cruciate ligament. J Bone Joint Surg Am. 1991;73(6):882–892. [PubMed] [Google Scholar]
- 39. O’Brien SJ, Warren RF, Wickiewicz TL, et al. The iliotibial band lateral sling procedure and its effect on the results of anterior cruciate ligament reconstruction. Am J Sports Med. 1991;19(1):21–25. [DOI] [PubMed] [Google Scholar]
- 40. Pernin J, Verdonk P, Si Selmi TA, Massin P, Neyret P. Long-term follow-up of 24.5 years after intra-articular anterior cruciate ligament reconstruction with lateral extra-articular augmentation. Am J Sports Med. 2010;38(6):1094–1102. [DOI] [PubMed] [Google Scholar]
- 41. Pizza N, Di Paolo S, Zinno R, et al. Over-constrained kinematic of the medial compartment leads to lower clinical outcomes after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. Published online January 2, 2021. doi:10.1007/s00167-020-06398-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Prodromos C, Joyce B. Endobutton femoral fixation for hamstring anterior cruciate ligament reconstruction: surgical technique and results. Tech Orthop. 2005;20(3):233–237. [Google Scholar]
- 43. Samuelsen BT, Webster KE, Johnson NR, Hewett TE, Krych AJ. Hamstring autograft versus patellar tendon autograft for ACL reconstruction: is there a difference in graft failure rate? A meta-analysis of 47,613 patients. Clin Orthop Relat Res. 2017;475(10):2459–2468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Schon JM, Moatshe G, Brady AW, et al. Anatomic anterolateral ligament reconstruction of the knee leads to overconstraint at any fixation angle. Am J Sports Med. 2016;44(10):2546–2556. [DOI] [PubMed] [Google Scholar]
- 45. Sonnery-Cottet B, Saithna A, Cavalier M, et al. Anterolateral ligament reconstruction is associated with significantly reduced ACL graft rupture rates at a minimum follow-up of 2 years: a prospective comparative study of 502 patients from the SANTI Study Group. Am J Sports Med. 2017;45(7):1547–1557. [DOI] [PubMed] [Google Scholar]
- 46. Sonnery-Cottet B, Thaunat M, Freychet B, Pupim BHB, Murphy CG, Claes S. Outcome of a combined anterior cruciate ligament and anterolateral ligament reconstruction technique with a minimum 2-year follow-up. Am J Sports Med. 2015;43(7):1598–1605. [DOI] [PubMed] [Google Scholar]
- 47. Tashman S, Collon D, Anderson K, Kolowich P, Anderst W. Abnormal rotational knee motion during running after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32(4):975–983. [DOI] [PubMed] [Google Scholar]
- 48. Tashman S, Kolowich P, Collon D, Anderson K, Anderst W. Dynamic function of the ACL-reconstructed knee during running. Clin Orthop Relat Res. 2007;454:66–73. [DOI] [PubMed] [Google Scholar]
- 49. Wilk KE, Escamilla RF, Fleisig GS, Barrentine SW, Andrews JR, Boyd ML. A comparison of tibiofemoral joint forces and electromyographic activity during open and closed kinetic chain exercises. Am J Sports Med. 1996;24(4):518–527. [DOI] [PubMed] [Google Scholar]
- 50. Williams A, Ball S, Stephen J, White N, Jones M, Amis A. The scientific rationale for lateral tenodesis augmentation of intra-articular ACL reconstruction using a modified “Lemaire” procedure. Knee Surg Sports Traumatol Arthrosc. 2017;25(4):1339–1344. [DOI] [PubMed] [Google Scholar]
- 51. Yamazaki J, Muneta T, Ju YJ, Sekiya I. Differences in kinematics of single leg squatting between anterior cruciate ligament-injured patients and healthy controls. Knee Surg Sports Traumatol Arthrosc. 2010;18(1):56–63. [DOI] [PubMed] [Google Scholar]
- 52. Yang C, Tashiro Y, Lynch A, Fu F, Anderst W. Kinematics and arthrokinematics in the chronic ACL-deficient knee are altered even in the absence of instability symptoms. Knee Surg Sports Traumatol Arthrosc. 2018;26(5):1406–1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Zaffagnini S, Marcheggiani Muccioli GM, Grassi A, et al. Over-the-top ACL reconstruction plus extra-articular lateral tenodesis with hamstring tendon grafts: prospective evaluation with 20-year minimum follow-up. Am J Sports Med. 2017;45(14):3233–3242. [DOI] [PubMed] [Google Scholar]
- 54. Zaid M, Lansdown D, Su F, et al. Abnormal tibial position is correlated to early degenerative changes one year following ACL reconstruction. J Orthop Res. 2015;33(7):1079–1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Zampeli F, Terzidis I, Espregueira-Mendes J, et al. Restoring tibiofemoral alignment during ACL reconstruction results in better knee biomechanics. Knee Surg Sports Traumatol Arthrosc. 2018;26(5):1367–1374. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-gif-1-ojs-10.1177_23259671211011940 for Dynamic Radiostereometry Evaluation of 2 Different Anterior Cruciate Ligament Reconstruction Techniques During a Single-Leg Squat by Stefano Di Paolo, Piero Agostinone, Alberto Grassi, Gian Andrea Lucidi, Erika Pinelli, Marco Bontempi, Gregorio Marchiori, Laura Bragonzoni and Stefano Zaffagnini in Orthopaedic Journal of Sports Medicine