Abstract
Background:
Humeral avulsion of the glenohumeral ligament (HAGL) is an uncommon condition but a major contributor to shoulder instability and functional decline.
Purpose:
To describe the pre- and postoperative HAGL lesion presentations of instability, pain, and functionality and the return-to-sports activities in patients managed arthroscopically for anterior and posterior HAGL lesions.
Study Design:
Case series; Level of evidence, 4.
Methods:
Data on patients with HAGL lesions treated with arthroscopic repair between 2009 and 2018 were retrospectively retrieved from medical charts, and the patients were interviewed to assess their level of postoperative functionality. The Rowe; Constant; University of California, Los Angeles; Oxford; and pain visual analog scale (VAS) scores were obtained for both pre- and postoperative status. Return-to-sports activities and level of activities after surgery were compared with the preinjury state, and complications, reoperations, and recurrent instability were recorded and evaluated.
Results:
There were 23 study patients (12 females and 11 males; mean age, 24 years). The mean follow-up duration was 24.4 months (range, 7-99 months; median, 17 months). In 7 (30.4%) of the patients, HAGL lesions were diagnosed only intraoperatively. A significant improvement was seen in all examined postoperative functional scores and VAS. At the last follow-up visit, 2 patients (8.7%) reported residual instability with no improvement in pain levels and declined any further treatment, and 3 others (13.0%) required revision surgeries for additional shoulder pathologies (reoperations were performed 18-36 months after the index procedure). The remaining 18 patients (78.3%) were free of pain and symptoms. There was a mean of 0.65 coexisting pathologies per patient, mostly superior labral anterior-posterior, Bankart, and rotator cuff lesions.
Conclusion:
HAGL lesions are often missed during routine workup in patients with symptoms of instability, and a high level of suspicion is essential during history acquisition, clinical examination, magnetic resonance imaging arthrogram interpretation, and arthroscopic evaluation. Arthroscopic repair yields good pain and stability results; however, some high-level athletes may not return to their preinjury level of activity.
Keywords: HAGL, labral tears, outcome analysis, shoulder instability, concomitant pathologies
Disruption of the capsule-labral complex, particularly the labrum and inferior glenohumeral ligaments (IGHLs) from the glenoid side, is a major pathology in anterior shoulder instability and one that has been well-studied and documented in the literature. 24 Humeral avulsion of the glenohumeral ligaments (HAGL) 17 is less common and has been poorly described, 8 possibly due to being underdiagnosed. The reported prevalence is between 2.8% and 9.3% of shoulders diagnosed with anterior instability. 2,10,21,24 As described by the West Point nomenclature, a HAGL lesion may affect the anterior IGHL, the posterior IGHL (reverse HAGL), or both and with or without the avulsion of a bone fragment. 4 In addition, the floating anterior band, as described by Bokor et al, 2 refers to a bipolar detachment of the IGHL 22 where HAGL and Bankart lesions coexist. 6 Hyperabduction and external rotation of the arm have both been suggested as mechanisms of injury that could result in a HAGL lesion, as demonstrated by Nicola 17 in a cadaveric model.
The clinical appearance of patients with HAGL lesions is not uniform, and it consists mainly of pain, instability, and functional decline of the involved shoulder. 6,20 A HAGL lesion may be isolated, but it is frequently associated with additional injuries such as rotator cuff tears, Bankart lesions, Hill-Sachs lesions, and glenoid bone loss. 3,4 Because a HAGL lesion is not common and often combined with other pathologies, a high level of suspicion is required to detect it. Magnetic resonance imaging (MRI) arthrograms have been recommended as the imaging method of choice, 8 although false-positive and false-negative findings have been reported. 13,15 Intraoperatively, a HAGL lesion may be seen as a detachment of the capsule from the humeral neck and the presence of an exposed subscapularis muscle, 24 or, as Bokor et al 2 described it, it could be a disruption of the wave formed by the reflection of the capsule onto the humeral neck.
Indications for surgery include failed nonoperative management of shoulder instability or pain and revision surgery for ongoing instability after primary Bankart repair. 3 Both open and arthroscopic repairs have been described in the literature as appropriate methods for HAGL lesion repair, 8,9 having shown promising results. 12 The Latarjet procedure was also described as an optional treatment for this kind of lesion. 14
The primary objective of the present study was to describe the pre- and postoperative presentations of HAGL lesions in terms of instability, pain, functionality, and return-to-sports activities in patients managed arthroscopically for anterior and posterior HAGL lesions. The investigators’ hypothesis was that arthroscopic repair yields good results in terms of improvement in the variable symptoms. The secondary objective was to describe the pathologies coexisting with HAGL lesions in those patients.
Methods
Study Population
Institutional review board approval was obtained for this retrospective case series. Patients or their legal guardians gave their informed consent before data collection. The data were retrieved from the database of a shoulder surgery unit in a tertiary center. Patients characteristics are presented in Table 1. Inclusion criteria were a HAGL lesion confirmed during diagnostic arthroscopy (anterior, posterior, or both) and repaired arthroscopically. A humeral avulsion of the capsule that did not involve any of the ligaments was not considered as being a HAGL lesion, even if it had been diagnosed as such on the preoperative MRI. Patients were excluded if treatment of the HAGL lesion was performed nonarthroscopically (eg, open repair or a coracoid transfer [Bristow-Latarjet procedure]) and if the follow-up was <6 months.
Table 1.
Patient Characteristics a
| Variable | Value |
|---|---|
| Female sex | 12 (52.2) |
| Age, y, mean (range) | 24 (15-41) |
| Right shoulder dominant | 20 (86.9) |
| Working preoperative diagnosis | |
| HAGL only | 7 (30.4) |
| HAGL and others | 8 (34.8) |
| Others | 8 (34.8) |
| Hyperflexibility | 60% |
a Values are expressed as n (%) unless otherwise noted. HAGL, humeral avulsion of the glenohumeral ligament.
The collected data included patients’ demographic characteristics, presenting symptoms, initial assessment (clinical examination, level and type of sport before and after surgery, imaging modality, and findings), working diagnosis, and intraoperative findings (including technical notes on the HAGL repair and any additional interventions). Hypermobility was assessed using the Beighton score. 1 Shoulder scores including Rowe; Constant; University of California, Los Angeles (UCLA); Oxford; and visual analog scale (VAS) results were obtained for both pre- and postoperative status. 18 Complications and additional surgeries were documented.
Surgical Technique
The operations were performed by 3 fellowship-trained shoulder specialists (E.M., O.C., E.R.). All procedures were carried out arthroscopically with the patient in a sitting beach-chair position as described by Fritz et al. 8 A double-loaded, 2.8-mm metallic anchor was used (Piton-Tornier).
Postoperative Rehabilitation
The operated shoulder was placed in a sling for 6 weeks. Active and passive movements of only the elbow and wrist were allowed, as was pendular movement of the shoulder, unless motion was restricted due to combined procedures. Active range-of-motion exercises of the operated shoulder were begun at postoperative week 6 with strengthening exercises initiated at 3 months after surgery. Full return to unrestricted sports activities was permitted by 6 months after surgery.
Statistical Analysis
Comparisons of the demographic and clinical variables were conducted by Student t test, Mann-Whitney nonparametric test for continuous parameters, and chi-square or Fisher exact test for categorical parameters. Statistical analysis was carried out using SPSS for Windows (Version 22.0), and significance was set at P ≤ .05.
Results
Between February 2009 and August 2018, a total of 28 patients were arthroscopically diagnosed with a HAGL lesion. Excluded were 3 patients who underwent open procedures and 1 patient who declined to participate. Further, 1 of the 24 remaining patients was lost to follow-up (Figure 1).
Figure 1.

Study flowchart of inclusion and exclusion criteria and numbers of patients. HAGL, humeral avulsion of the glenohumeral ligament.
The 23 remaining patients included 12 female patients and 11 male patients whose ages ranged from 15 to 41 years (mean, 24 years) (Table 1). The mean follow-up duration was 24.4 months (range, 7-99 months).
The presenting symptoms were distributed as follows: 17 of 23 (73.9%) patients reported a sensation of instability (feeling of shoulder out of its place) as their main complaint, and 6 of 23 (26.1%) presented with frank dislocations. Pain was the second most common presenting symptom, being present in 13 of 23 (56.5%) patients. The mean time from initial symptoms to surgery was 24.3 months (range, 1-72 months). In total, 2 patients had previously undergone shoulder surgeries: 1 was a capsular shift for instability and 1 was a repair for a superior labral tear from anterior to posterior (SLAP) with no mention of a HAGL lesion. Neither patient reported significant improvement after the previous surgeries, which indicates that a HAGL lesion may have been missed.
Imaging
Details on the preoperative imaging notes were available for all patients. In total, 22 patients (95.6%) underwent an MRI, and 19 (82.6%) had a concurrent arthrogram. The preoperative diagnosis included HAGL lesions in only 16 (69.6%) patients. Of the remaining 7 patients, 4 patients had an MRI with arthrography and the lesion had been overlooked, 2 patients had an MRI without arthrography, and 1 patient had a computed tomography scan on which the lesion could not be identified.
Intraoperative Findings
An anterior HAGL lesion was present in 17 patients (73.9%), a posterior HAGL lesion in 3 patients (13.0%), a combined anterior + posterior HAGL lesion in 2 patients (8.7%), and a central lesion in 1 patient (4.3%). Further, 11 patients (47.8%) had additional shoulder pathologies that required further intervention (Table 2). A type 2 SLAP lesion was the most frequently encountered (n = 5; 21.7%), followed by anterior Bankart lesion (n = 4; 17.4%) and rotator cuff tear (n = 3; 13.0%). We noted 1 case of each (4.3%) of the following lesions: glenolabral articular disruption lesion, Hill-Sachs lesion, and dislocated long head of biceps (LHB). Overall, 15 additional interventions were performed: 5 arthroscopic Bankart repairs, 3 SLAP repairs, 2 subpectoral LHB tenodeses, 2 rotator cuff repairs (subscapularis, supraspinatus, and infraspinatus), and 1 each of an intra-articular LHB tenodesis, remplissage, and debridement of a minor supraspinatus tear (Table 2).
Table 2.
Intraoperative Findings, Procedures, Pitfalls, and Postoperative Complications a
| Patient | HAGL | Intraoperative Remarks | Additional Interventions | Surgical Complications |
|---|---|---|---|---|
| 1 | Anterior | — | — | — |
| 2 | Anterior | Subscapularis tear | Subscapularis repair | — |
| 3 | Anterior | — | — | — |
| 4 | Anterior | — | — | — |
| 5 | Anterior | — | — | — |
| 6 | Anterior | Anterior Bankart lesion | ABR | — |
| 7 | Anterior | — | — | Musculocutaneous transient hypoesthesia |
| 8 | Posterior | Anterior Bankart lesion | ABR | |
| 9 | Anterior | Supraspinatus tear, intraoperative failure of anchor due to incorrect anchor angle—replaced | Debridement | Significant venous bleeding |
| 10 | Anterior | — | — | — |
| 11 | Anterior | Dislocated LHB, intraoperative failure of anterior anchor due to incorrect anchor application angle | Subpectoral LHB tenodesis | — |
| 12 | Anterior | Anterior Bankart lesion, SLAP type 2, GLAD | ABR + SLAP repair | — |
| 13 | Anterior | SLAP type 2 | SLAP repair | — |
| 14 | Posterior | — | — | — |
| 15 | Anterior | — | — | — |
| 16 | Anterior | SLAP type 2 | LHB subpectoral tenodesis | — |
| 17 | Posterior | — | — | — |
| 18 | Anterior | — | — | — |
| 19 | Anterior | RC (supraspinatus +infraspinatus tear), anterior Bankart, SLAP type 2 + LHB tendinitis | RC repair, LHB intra-articular tenodesis, ABR | — |
| 20 | Anterior | SLAP type 2, repeat anchor insertion required | SLAP repair | — |
| 21 | Anterior + posterior | — | — | — |
| 22 | Anterior + posterior | Intraoperative failure of anterior anchor due to incorrect anchor application angle | — | — |
| 23 | Central | ALPSA, HSL | ABR, remplissage | — |
a ABR, arthroscopic Bankart repair; ALPSA, anterior labroligamentous periosteal sleeve avulsion; GLAD, glenolabral articular disruption; HAGL, humeral avulsion of the glenohumeral ligament; HSL, Hill-Sachs lesion; LHB, long head of biceps; RC, rotator cuff; SLAP, superior labral anterior to posterior. Dashes indicate “none.”
Functional Outcomes
A total of 18 patients (78.2%) reported resolution of their symptoms after a mean follow-up of 20.2 months (median, 16.5 months; range, 7-57 months). No patient experienced frank shoulder dislocation after surgery; however, 2 patients (patients 9 and 11; 8.7%) remained symptomatic and described recurrent feelings of instability as their main complaint. One patient underwent concurrent subpectoral tenodesis and a small rotator cuff tear debridement.
A further 3 patients (patients 1, 2, and 14; 13.0%) who continued with noninstability shoulder symptoms underwent additional surgeries with satisfactory results. These included 1 LHB tenodesis, 1 revision of subscapularis repair, and 1 adhesiolysis with anchor removal due to significant range of motion limitation postoperatively. One other patient with asymptomatic, significantly limited range of motion (possibly due to ligament overtightening) declined adhesiolysis.
The HAGL repair was intact in the patients who underwent postoperative MRI arthrography and in the ones who had revision surgery.
Functional Scores
Statistically significant improvement (P < .05) that exceeded the minimal clinically important difference was achieved postoperatively in the mean Rowe score (increased by mean of 35.5 points), Constant score (increased by mean of 20.1 points), Oxford score (increased by mean of 18 points), UCLA score (increased by mean of 14.7 points) and VAS score (decreased by mean of 6.6 points) (Figure 2). 11,19,23,25
Figure 2.
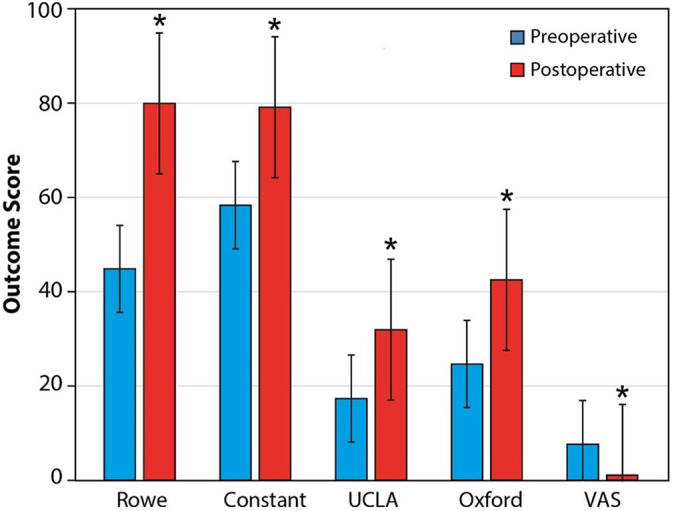
Pre- and postoperative functional scores. UCLA, University of California, Los Angeles; VAS, visual analog scale. *Statistically significant difference between pre- and postoperative (P < .05).
Return to Sports
Only 12 (52.2%) patients were involved in sports activities (professional level judo, extreme sports, volleyball, basketball, handball, water skiing, parachuting) before the shoulder injury. Of these patients, 6 (50%) were able to return to the same level of sport activity, 4 (33.3%) experienced a decrease in their level of activity, and 2 (16.7%) were unable to return to their previous sport.
Complications
Intraoperative anchor failure due to poor insertion technique occurred in 4 patients (17.4%) and required the replacement of these failed anchors. There was 1 incident of a transient musculocutaneous sensory deficit that recovered spontaneously, and 1 patient had major venous bleeding around the low anterior portal, which required admission to a pediatric intensive care unit and transfusion of 1 unit of packed blood cells. Revision surgeries were performed on 3 patients (13.0%) and consisted of LHB tenodesis for the treatment of LHB pain appearing postoperatively, removal of a loose anchor screw, and repair of subscapularis retear. Notably, at the primary surgery, introduction of the anchor was uneventful in the case of the second patient; in the third patient, a subscapularis tear was diagnosed and repaired. Essentially, 2 of these patients presented with an initial anterior HAGL lesion and 1 with a posterior HAGL lesion.
Discussion
The main purpose of this study was to contribute to the sparse data on the pre- and postoperative presentations of HAGL lesions in terms of instability, pain, functionality, and return to sports in patients managed arthroscopically for anterior and posterior HAGL lesions. We also described the pathologies coexisting with HAGL lesions in our patient cohort. The principal findings of this study demonstrated that arthroscopic repair of anterior and posterior HAGL lesions resulted in a significant improvement in all functional and instability scores.
As described in the literature, we also observed that the clinical presentation of a HAGL lesion is nonspecific. 12 The degree of instability in this study varied, with frank dislocation in 26% of the patients, feeling of shoulder not being in place or any shoulder instability in 74%, and pain in 56.5%. Provencher et al 20 reported pain as being the main complaint of patients with HAGL lesions, present in 85% of their patients, whereas shoulder dislocations and subluxations were reported in 11% and 32%, respectively, of their patients. Schmiddem et al 22 reported shoulder dislocations in 67% of their cohort of 18 patients treated surgically for HAGL lesions. One possible explanation for the sensation of instability is the disruption of proprioceptive feedback in the case of a HAGL lesion, as described by Myers et al 16 for additional shoulder instability pathologies. It was those authors’ assumption that this vague clinical presentation likely led to the relatively extended time period of 24.3 months to surgical treatment.
In the current study, the HAGL lesion was diagnosed intraoperatively rather than before surgery in 7 patients (30.4%). Of these 7 patients, 4 patients had been misdiagnosed (the HAGL lesion was evident in preoperative imaging but was overlooked), and 3 patients had no preoperative arthrographic imaging study. Preoperative misdiagnosis of HAGL lesions is well-described in the literature. Castagna et al 5 identified a posterior HAGL lesion on only retrospective examination and never before the procedure in all 9 of their reported patients. Huberty and Burkhart 10 reported that 3 of their 6 patients with HAGL lesions were identified only intraoperatively and that the diagnosis was missed on an MRI examination. Longo et al 12 stated that the difficulty in diagnosing a HAGL lesion probably contributes to its low reporting rate. This difficulty only emphasizes the significance of maintaining a high index of suspicion while taking the medical history, 4,5 performing the physical examination, 12 analyzing the MRI arthrogram, and executing a systematic diagnostic arthroscopy that involves assessment for a potential HAGL lesion, even if other pathologies have already been identified in the presenting patient. 20
The location of the HAGL lesion in our study patients was predominantly anterior (n = 17; 73.9%), followed by posterior (n = 3; 13.0%) and combined (n = 3; 13.0%). These results are in line with those reported in the literature, demonstrating dominancy of an anterior HAGL injury. 4,20 Bui-Mansfield et al 4 reported an anterior HAGL lesion in 93% of their 66 patients. Provencher et al, 20 however, described a distribution of 52% anterior, 37% posterior, and 11% combined HAGL lesions among their 27 patients.
Coexisting pathologies are often found with HAGL lesions. 12 In a recently published study, Schmiddem et al 22 reported an 89% rate of additional shoulder pathologies among patients treated for HAGL lesions. The frequently encountered pathologies are Bankart or anterior labroligamentous periosteal sleeve avulsion lesions, Hill-Sachs lesions, and rotator cuff tears, particularly subscapularis. 2,3,7,12 These findings are in line with those of the present study, in which 47.8% of the patients sustained concomitant pathologies. A mean of 0.65 additional pathologies per patient was documented, mostly SLAP, Bankart, and rotator cuff lesions. Although that finding may add a possible confounder to the clinical results, there is no available published information to distinguish between treatment of the concomitant pathologies with and without treatment for the HAGL lesion.
On the final follow-up visit, 2 patients (8.7%) reported a residual sensation of instability with no improvement in pain levels, and they declined any further treatment, whereas the remaining 21 patients (91.3%) were pain- and symptom-free. We noted significant improvement in all examined postoperative functional scores and VAS scores in this study. Oxford, UCLA, and Constant scores displayed excellent to good results. Similar results are reported in the literature for open or arthroscopic repair of HAGL lesions. Castagna et al 5 demonstrated significant improvement in UCLA and Constant scores after arthroscopic repair of a posterior HAGL in 9 patients. Huberty and Burkhart 10 reported an improvement in UCLA score (from 18.3 to 33) in 6 patients treated arthroscopically for HAGL lesions. The Rowe score, which tests for instability, showed a significant improvement and reached a good final result in the current study (from 45.33 to 80.83; SD, 19.45). The results reported in the literature were similar. Schmiddem et al 22 reported a significant improvement in the median Rowe score (from 33 to 86) for patients who had been treated arthroscopically for HAGL lesions. Rhee and Cho 21 reported an improvement in the Rowe score (from 24 to 92) and an improvement in VAS scores during motion (from 4.5 to 0.3) in 5 patients treated with open HAGL repair. Finally, 2 systematic reviews by Bozzo et al 3 and Longo et al 12 concluded that both arthroscopic and open repair demonstrated promising results whereas nonoperative treatment resulted in poor outcomes.
Revision surgeries were performed on 3 patients in this study cohort (13.0%). One revision was directly related to the HAGL repair and required the removal of an anchor screw. The other 2 revision surgeries addressed other pathologies (LHB tenodesis and a subscapularis tear) that were found and treated during the index procedure.
Reports in the literature on patients’ return to sports activities after HAGL repair are inconclusive. In this study, of the 12 patients who participated in sports presurgically, 6 (50%) patients returned to their preinjury level of sports activity, 4 (33.3%) experienced a decrease in their level, and 2 (16.7%) were unable to return to sport. We found no correlation between concomitant pathologies and return-to-sports activity. In their systematic review, Bozzo et al 3 reported that only 2 of the 79 patients who underwent HAGL repair were unable to return their previous levels of sports performance. Schmiddem et al 22 reported that 5 of their 9 patients failed to reach their preinjury level of sport; 3 of those 5 patients had an additional rotator cuff tear, whereas the 4 patients who did recover had associated labral tears and Hill-Sachs lesions. This information led the authors to suggest that there was a relationship between a coexisting rotator cuff tear and the inability to fully return to the preinjury level of sport activity. Analysis of these data indicates that the return of a top-level athlete to his or her preinjury performance level is not certain and may be affected by failed healing of the HAGL lesion and/or concomitant lesions. We suggest that alternative means of repairing HAGL lesions should be considered, possibly a Latarjet-Bristow procedure, when treating a top athlete for a HAGL lesion.
Limitations
This was a small-sized, underpowered, retrospective cohort study. The study included a heterogeneous population, with different symptoms, physical and imaging findings, concomitant pathologies, and surgical indications. The follow-up period was short and did not allow full recovery in some patients. These limitations cause difficulty in drawing conclusions or calculating statistical tests regarding the functional outcomes and return to sports after arthroscopic repair of HAGL lesions. Furthermore, MRI examinations were not performed on the same machine or using a standard protocol. Surgeries were performed by different surgeons with slight technical variations. Functional outcomes and return to sports were recorded only at the final follow-up visit and not sequentially. Nevertheless, because HAGL lesion is a rare entity, it is important to report even these limited results.
Conclusion
HAGL lesions are often missed during routine workup in patients with symptoms of instability, and a high degree of suspicion is essential during history taking, clinical examinations, MRI arthrogram interpretation, and arthroscopic evaluation. The study findings indicated that arthroscopic repair yields good results in pain relief and stability; however, some top-level athletes may not return to their preinjury level of sports activity.
Footnotes
Final revision submitted January 24, 2021; accepted February 24, 2021.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Tel Aviv Sourasky Medical Center (protocol No. 0525-15-TLV).
References
- 1. Beighton P, Horan F. Orthopaedic aspects of the Ehlers-Danlos syndrome. J Bone Joint Surg Br. 1969;51(3):444–453. [PubMed] [Google Scholar]
- 2. Bokor DJ, Conboy VB, Olson C. Anterior instability of the glenohumeral joint with humeral avulsion of the glenohumeral ligament. J Bone Joint Surg Br. 1999;81(1):93–96. [DOI] [PubMed] [Google Scholar]
- 3. Bozzo A, Oitment C, Thornley P, et al. Humeral avulsion of the glenohumeral ligament: indications for surgical treatment and outcomes—a systematic review. Orthop J Sports Med. 2017;5(8):2325967117723329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bui-Mansfield LT, Banks KP, Taylor DC. Humeral avulsion of the glenohumeral ligaments: the HAGL lesion. Am J Sports Med. 2007;35(11):1960–1966. [DOI] [PubMed] [Google Scholar]
- 5. Castagna A, Snyder SJ, Conti M, Borroni M, Massazza G, Garofalo R. Posterior humeral avulsion of the glenohumeral ligament: a clinical review of 9 cases. Arthroscopy. 2007;23(8):809–815. [DOI] [PubMed] [Google Scholar]
- 6. Field LD, Bokor DJ, Savoie FH III. Humeral and glenoid detachment of the anterior inferior glenohumeral ligament: a cause of anterior shoulder instability. J Shoulder Elbow Surg. 1997;6(1):6–10. [DOI] [PubMed] [Google Scholar]
- 7. Forsythe B, Frank RM, Ahmed M, et al. Identification and treatment of existing copathology in anterior shoulder instability repair. Arthroscopy. 2015;31(1):154–166. [DOI] [PubMed] [Google Scholar]
- 8. Fritz EM, Pogorzelski J, Hussain ZB, Godin JA, Millett PJ. Arthroscopic repair of humeral avulsion of the glenohumeral ligament lesion. Arthrosc Tech. 2017;6(4):e1195–e1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Godin JA, Sanchez G, Kennedy NI, Ferrari MB, Provencher MT. Open repair of an anterior humeral avulsion of the glenohumeral ligament. Arthrosc Tech. 2017;6(4):e1367–e1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Huberty DP, Burkhart SS. Arthroscopic repair of anterior humeral avulsion of the glenohumeral ligaments. Techn Shoulder Elbow Surg. 2006;7(4):186–190. [Google Scholar]
- 11. Jones IA, Togashi R, Heckmann N, Vangsness CT, Jr. Minimal clinically important difference (MCID) for patient-reported shoulder outcomes. J Shoulder Elbow Surg. 2020;29(7):1484–1492. [DOI] [PubMed] [Google Scholar]
- 12. Longo UG, Rizzello G, Ciuffreda M, et al. Humeral avulsion of the glenohumeral ligaments: a systematic review. Arthroscopy. 2016;32(9):1868–1876. [DOI] [PubMed] [Google Scholar]
- 13. Magee T. Prevalence of HAGL lesions and associated abnormalities on shoulder MR examination. Skeletal Radiol. 2014;43(3):307–313. [DOI] [PubMed] [Google Scholar]
- 14. McHale KJ, Sanchez G, Lavery KP, et al. Latarjet technique for treatment of anterior shoulder instability with glenoid bone loss. Arthrosc Tech. 2017;6(3):e791–e799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Melvin JS, Mackenzie JD, Nacke E, Sennett BJ, Wells L. MRI of HAGL lesions: four arthroscopically confirmed cases of false-positive diagnosis. AJR Am J Roentgenol. 2008;191(3):730–734. [DOI] [PubMed] [Google Scholar]
- 16. Myers JB, Wassinger CA, Lephart SM. Sensorimotor contribution to shoulder stability: effect of injury and rehabilitation. Man Ther. 2006;11(3):197–201. [DOI] [PubMed] [Google Scholar]
- 17. Nicola T. Acute anterior dislocation of the shoulder. J Bone Joint Surg Am. 1949;31(1):153–159. [PubMed] [Google Scholar]
- 18. Oh JH, Jo KH, Kim WS, Gong HS, Han SG, Kim YH. Comparative evaluation of the measurement properties of various shoulder outcome instruments. Am J Sports Med. 2009;37(6):1161–1168. [DOI] [PubMed] [Google Scholar]
- 19. Park I, Lee JH, Hyun HS, Lee TK, Shin SJ. Minimal clinically important differences in Rowe and Western Ontario Shoulder Instability Index scores after arthroscopic repair of anterior shoulder instability. J Shoulder Elbow Surg. 2018;27(4):579–584. [DOI] [PubMed] [Google Scholar]
- 20. Provencher MT, McCormick F, LeClere L, et al. Prospective evaluation of surgical treatment of humeral avulsions of the glenohumeral ligament. Am J Sports Med. 2017;45(5):1134–1140. [DOI] [PubMed] [Google Scholar]
- 21. Rhee YG, Cho NS. Anterior shoulder instability with humeral avulsion of the glenohumeral ligament lesion. J Shoulder Elbow Surg. 2007;16(2):188–192. [DOI] [PubMed] [Google Scholar]
- 22. Schmiddem U, Watson A, Perriman D, Liodakis E, Page R. Arthroscopic repair of HAGL lesions yields good clinical results, but may not allow return to former level of sport. Knee Surg Sports Traumatol Arthrosc. 2019;27(10):3246–3253. [DOI] [PubMed] [Google Scholar]
- 23. Tashjian RZ, Shin J, Broschinsky K, et al. Minimal clinically important differences in the American Shoulder and Elbow Surgeons, Simple Shoulder Test, and visual analog scale pain scores after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2020;29(7):1406–1411. [DOI] [PubMed] [Google Scholar]
- 24. Wolf EM, Cheng JC, Dickson K. Humeral avulsion of glenohumeral ligaments as a cause of anterior shoulder instability. Arthroscopy. 1995;11(5):600–607. [DOI] [PubMed] [Google Scholar]
- 25. Xu S, Chen JY, Lie HME, Hao Y, Lie DTT. Minimal clinically important difference of Oxford, Constant, and UCLA shoulder score for arthroscopic rotator cuff repair. J Orthop. 2020;19:21–27. [DOI] [PMC free article] [PubMed] [Google Scholar]


