The COVID-19 pandemic has forced various national and international bodies to modify or generate new treatment protocols and algorithms to manage it.1 In general, individuals with mental illness living in the community face unique challenges that make them vulnerable to adverse health outcomes during the pandemic. These include limited access to health care resources, high residence rates in population-dense dwellings such as shelters or supportive housing, and difficulty accessing and implementing the public health recommendations designed to reduce transmission rates.2,3,4
Further, several individuals, particularly those with severe mental illness, require long-term inpatient (IP) care. Institutional settings make enforcement of pandemic control measures difficult, because IPs often share bedrooms, bathrooms, and dining facilities, and are required to participate in group therapeutic activities.2,5,6 Additionally, the presence of active or persistent psychiatric symptoms is often a barrier to individuals’ abilities to adhere to or accept interventions designed to reduce transmission, such as isolation, social distancing, use of masks, or nasopharyngeal swabs for COVID-19 testing.6,7 Consequently, outbreaks of COVID-19 in IP psychiatric units have been reported from different parts of the world.8,9,10 This has led to implementing strategies to prevent the spread of COVID-19 in IP units.9,11 However, no such operational algorithm of a dedicated psychiatric setting has been reported from India.
With this background, we present a working framework that we hope will help mental health professionals and hospital administrators deliver an adequate standard of psychiatric care in a dedicated psychiatric setting while containing the spread of infection. Specifically, we describe the setting up of a psychiatric-COVID-19 unit (PCU) to address the challenges and record learning from the same. This dedicated unit was made operational at the RM Varma Subspecialty Block at the National Institute of Mental Health and Neuro Sciences (NIMHANS), Bengaluru, Karnataka. The framework presented below was designed by an expert committee of the institute, consisting of a panel of infectious disease experts, microbiologists, pulmonologists (external), anesthetists/intensivists, and psychiatrists, and is being implemented since the COVID-19 lockdown. Along with this framework, we have added recommendations for special populations, like children and adolescents and the elderly, as well.
Modifications in Admission Procedures During COVID-19 Pandemic
Under normal circumstances, IP admission occurs through two main pathways: (a) outpatient services and (b) emergency psychiatry and acute care (EPAC) services. In all cases, this takes place after a detailed evaluation by a qualified psychiatrist who decides upon the need for IP psychiatric care.
During the pandemic, some modifications were made to this pathway to curtail outbreaks in IP services. This was in keeping with the mandate of infection control as per national and local guidelines for managing the pandemic. First, the EPAC block was made the single-entry point for all patients requiring IP psychiatric care. Second, all patients presenting to the EPAC block underwent mandatory temperature checks and were screened for influenza-like illness (ILI) symptoms, history of travel, and known contact with an individual with COVID-19. Third, all patients requiring IP psychiatric care underwent a nasopharyngeal and oropharyngeal swab for reverse transcription polymerase chain reaction (RT-PCR) or a rapid antigen test for COVID-19 before admission. Patients presenting with ILI symptoms or coming for testing had a separate entry and exit. This was a modification made in the current infrastructure, to minimize contact. Further, all mental health professionals in the EPAC block were provided personal protective equipment, N95 masks, and face shields to prevent the spread of infection. The patients managed in the EPAC services during this time fell into the following three groups:
Group A: Registered patients of the institute referred from the outpatient services for admission and new patients presenting directly to the EPAC services and without symptoms of COVID-19.
Group B: Patients who developed symptoms of COVID-19 after admission to the institute’s IP psychiatric facility.
Group C: COVID-19 patients referred from COVID centers to control psychiatric symptomatology.
Out of the three groups, group A constituted the most numbers of patients, while group C had the least number.
As per the usual protocol, all patients were assessed for the requirement of admission by a qualified psychiatrist in the EPAC. Patients who were planned for admission and their caregivers underwent RT-PCR testing, which occurred in a separate swabbing area at the EPAC facility.
Subsequently, patients and caregivers were placed in a holding area at the EPAC facility while waiting for the RT-PCR results. The holding area was well-defined, with adequate bed spacing and separate bath and restroom areas for both sexes. The holding area also had separate rooms that could be utilized if patients or caregivers developed ILI symptoms. Patients who tested positive for COVID-19 were shifted safely to the PCU for further management. If a caregiver tested positive for COVID-19, he/she was transferred to COVID care centers or a designated COVID-19 hospital, or were recommended home isolation depending on the severity of symptoms. The remaining admitted patients who tested negative were managed in the usual way, taking utmost precautions (wearing a mask, having a face-shield, and following social distancing) to minimize contacts and infections. IPs who developed ILI symptoms were categorized under group B.
Contact Tracing
In all cases, contact tracing was carried out by a team of psychiatrists and psychiatric social workers (PSWs) in liaison with the hospital infection committee. The steps involved gathering information on travel and other movements of the patients and their close contacts. Information was gathered by phone calls and interviews with family members. Those identified to be at high risk were advised home quarantine and were requested to inform the nearest COVID-19 facility if they developed ILI symptoms.
Psychiatric–COVID Unit
This unit consisted of a dedicated ten-bedded ward allocated to care for those with psychiatric illness and COVID-19. The unit was managed by a multidisciplinary team that consisted of psychiatrists, PSWs, and staff nurses. There was also a facility for liaison with neuro-anesthesiologists if patients admitted to the unit required critical care intervention.
Criteria for Admission/Transfer of Patients to the PCU
The patients admitted/transferred to the PCU were diagnosed with COVID-19 based on a positive RT-PCR report in most cases. In a few cases, patients were also admitted based on a positive result of a rapid antigen test in conjunction with a clinical suspicion of COVID-19. Adult patients were admitted to the unit without caregivers. However, caregivers could communicate with the multidisciplinary team outside the facility in a designated counseling room.
The patients admitted/transferred to the unit included those requiring IP psychiatric care due to the severity of their psychiatric illness and the wandering mentally ill with asymptomatic, mild, or moderate COVID-19. In some instances, patients with progressing ILI symptoms or those with severe infection who were awaiting transfer to a designated COVID hospital were also managed.
Procedures Followed After Admission to the PCU
Following admission to the unit, all patients were reassessed and categorized into asymptomatic, mild, moderate, and severe, based on clinical management protocol for COVID-19 provided by the Government of India. All patients also underwent recommended laboratory investigations such as C-reactive protein (CRP) Ferritin, Lactate dehydrogenase (LDH) and D-Dimer levels to aid with staging and management. Patients in the asymptomatic, mild, and moderate groups were monitored and provided care for both COVID and mental health concerns. Patients in the severe group were transferred to a dedicated COVID-19 hospital at the earliest. However, frequent delays occurred in the transfer of such patients, due to the nonavailability of beds in COVID-19-designated hospitals. While awaiting transfer, these patients were jointly managed by the psychiatrists and the anesthetist/intensivist on duty.
Logistics of Management While Admitted to PCU
Each team member had assigned roles and responsibilities to ensure the unit’s smooth functioning and to reduce the risk of infection. The nursing staff, who were posted to the unit in shifts, oversaw patient monitoring, drawing blood for investigations, and administering medications. Dedicated psychiatry residents were posted to the unit for two weeks on rotation and were responsible for daily assessment and treatment of all patients admitted there. All treatment/management changes were discussed with the consultant in charge of the patient and the in-charge consultant of the PCU. Administrative tasks, including auditing patient admissions, discharges, and their current treatment; the functioning of equipment; availability of medications; and facilitating liaison in case of need for referral, were carried out by the in-charge consultant of the PCU. Emergency liaison consultations were done with the neuro-anesthesia/neurology/neurosurgery team on duty whenever required. A PSW was also assigned to the unit to assist the psychiatrists in liaising with family and providing psychosocial support.
Transfer/Discharge of Patients from PCU
Following treatment at the PCU, discharge or transfer out of the unit occurred in one of the following ways:
The patient’s discharge to home quarantine, which happened if the patient’s psychiatric symptoms were apt to be managed at home.
The transfer of the patient to the IP psychiatric facility, which was done if the patient had persistent psychiatric symptoms that warranted continued IP psychiatric care. However, retransfer/readmission to an earlier adult IP psychiatric facility of the institute mandated a negative RT-PCR report after a period of 10 to 14 days.
The transfer of the patient to a designated COVID-19 hospital, which was undertaken in the event of worsening of COVID-19 symptoms. The psychiatric resident carried out the transfer in coordination with the hospital administration. The PSW did the coordination with family members and the designated COVID-19 hospitals, for psychosocial issues. Post-transfer, daily updates about the patients were obtained by the residents, and the progress was documented in our records.
Following discharge from the COVID-19-designated hospitals, two scenarios were commonly encountered: The first was where the patient remained symptom-free both for COVID-19 and the mental illness, in which case home isolation was advised for a further two weeks as per government guidelines.12 The second was where the patient was asymptomatic for COVID-19 but remained with psychiatric symptoms and was brought back to NIMHANS directly for further management. In the latter case, the treating team decided upon further management, with readmission to the PCU as needed.
Readmission of Patients to PCU
The most common reason for readmission to the PCU was continued behavioral issues not manageable at a COVID-19-designated hospitals, with persistence of ILI symptoms and illness duration of COVID-19 being less than ten days after the last positive RT-PCR test.
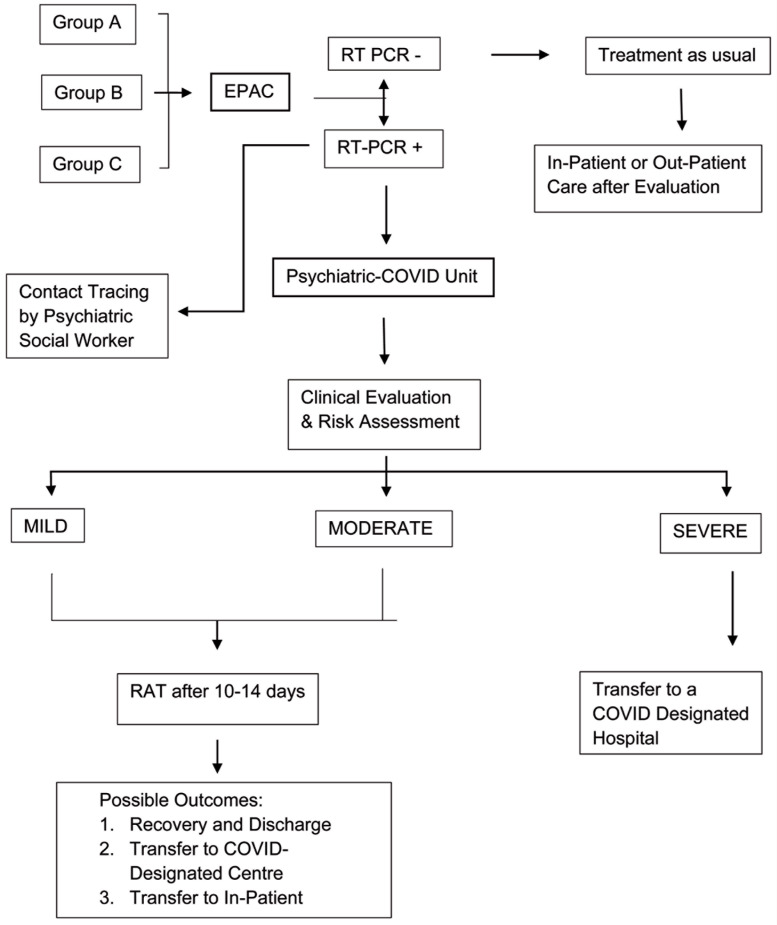
Patients with no ILI symptoms and illness duration of more than ten days after the last positive RT-PCR test were typically not readmitted in the PCU and were managed in IP psychiatric facility if they required continued care. The entire framework has been depicted in Figure 1.
Figure 1. Algorithm for COVID Testing and Triaging.
EPAC: Emergency psychiatry and acute care; RT-PCR: Reverse transcription polymerase chain reaction; RAT: Rapid antigen test.
Recommendations for Special Populations
Children and Adolescents
Across the globe, children have a lower rate of transmission and carriage than adults, a milder illness than adults, and a better prognosis, but can spread the infection to the older adults in a space-limited setup.13,14,15 Children with mental illness present a challenge, particularly when they have externalizing disorders such as attention deficit hyperkinetic disorder and conduct disorder or developmental disorders such as intellectual and developmental disabilities and autism, where following the COVID-19 restrictions is difficult.16
Children can have diverse manifestations of the disease, from asymptomatic to critically ill. The symptoms can mimic several common infections, with respiratory, gastrointestinal, and CNS symptoms. Although cough and fever are the most common symptoms, even in children, many remain asymptomatic.17 Hence, in the current scenario, all children presenting to the hospital may need to be tested for COVID-19.
Children who have an asymptomatic infection without any comorbid illness can be home quarantine, like adults, with monitoring of symptoms and a hospital visit, as necessary. Children who have significant comorbidity or moderate-to-severe illness would require admission to an isolation facility. A caretaker will be required to stay with them in the COVID-19 ward. That caretaker should be familiar to them, and preferably a parent or a close relative. Hence, baseline and follow-up contact testing are required for the person who is accompanying the child. That caretaker should preferably have no comorbidities that may put him or her at a greater risk for the development of adverse events.
Geriatric
The older adults have their own set of limitations, which are compounded by the COVID-19 pandemic. Preexisting diabetes, hypertension, chronic respiratory disease, and chronic kidney disease prevalent in the older adults are known risk factors for poor COVID-19 outcomes. Besides, elderly patients with cognitive impairment are likely to have problems understanding, remembering, and following self-protection procedures, quarantine rules, and isolation.18,19 The presence of comorbid delirium or any preexisting mental illness magnifies the intensity of the problem while increasing their morbidity and mortality.20 Therefore, the emergency setting’s priority should be on rapid diagnosis and management of acute presentations, to reduce the overall risk of exposure. This may be integrated with telepsychiatry follow-ups, which have been found in many cases to be acceptable and to provide the benefit of care access to elderly patients.21
Substance Use Disorders
Individuals with substance use disorders (SUD) form a large proportion of patients seen in most specialized psychiatric settings in India. From a service delivery standpoint, emergency IP admissions for SUD are mostly related to substance intoxication, substance withdrawal or co-occurring SUD and severe mental illness. It is well established that individuals with SUD are at greater risk for developing COVID-19.22 Therefore, a framework for the management of individuals with SUD and COVID-19 in a psychiatric setting is imperative.
The general principles that were followed to reduce the risk of transmission included an emphasis on outpatient-based medical management, proactive and aggressive management of substance use emergencies, particularly alcohol withdrawal seizures and delirium, and upscaling of the existent after-care system to ensure continuity of care. Long-term psychosocial interventions were conducted, wherever feasible, using telephone calls or video consultations. Group therapy interventions were temporarily halted, although online groups have been used in other centers and by twelve-step programs.
In general, most patients with substance use emergencies were successfully managed in the EPAC facility for 48 to 72 hours, with IP management in indicated cases only. The decision to perform a nasopharyngeal swab and RT-PCR for COVID-19 was guided by clinical suspicion and for individuals for whom admission to the IP wards was required as per institutional guidelines. Individuals with SUD whose RT-PCR for COVID-19 was positive were managed based on the assessment of the clinical condition and in keeping with the general guidelines for management issued by the Ministry of Health and Family Welfare.
In cases where the substance use emergency was managed and COVID-19 was asymptomatic or mild, patients were advised home isolation or were referred to COVID care centers with a prescription for acute withdrawal management if applicable. Cases continuing to require acute specialized withdrawal management and nutritional support were managed in the psychiatric COVID block, provided that COVID-19 was asymptomatic, mild, or moderate. In all cases with severe COVID-19, prescriptions for withdrawal management and a referral and transfer to a COVID-designated hospital were provided.
Conclusion
Patients with psychiatric illness face several challenges in managing infectious diseases because impaired judgment may contribute to difficulties in understanding and adhering to infection control protocols during pandemic situations. This is compounded by the fact that health professionals in other specialties often find it challenging to understand their problems and to manage them. Hence, we aver that hospitals providing exclusive psychiatric care should equip themselves to provide care for patients with mental illness and COVID-19, at least in cases where the infection is asymptomatic, mild, or moderate. This would greatly reduce the burden on general medical hospitals and ensure that patients with mental illness receive optimal care as mental health professionals might be better positioned to manage coexisting behavioral and psychological issues. We expect that sharing this overall design and workflow would help other psychiatric facilities emulate this model and provide mental health care amidst the COVID-19 pandemic and any future infectious disease outbreak or epidemic of a similar nature.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Ministry of Health and Family Welfare Directorate General of Health Services (EMR Division) Government of India. Clinical Management Protocol for COVID 19, https://www.mohfw.gov.in/pdf/UpdatedClinicalManagementProtocolforCOVID19dated03072020.pdf (accessed July3, 2020).
- 2.Li L. Challenges and priorities in responding to COVID-19 in inpatient psychiatry. Psychiatr Serv 2020; 71: 624–626. [DOI] [PubMed] [Google Scholar]
- 3.Shinn AK, Viron M. Perspectives on the COVID-19 Pandemic and individuals with serious mental illness. J Clin Psychiatry. 2020. April 28; 81(3): 20com13412. doi: https://doi.org/10.4088/JCP.20com13412. PMID: 32369691 [DOI] [PubMed] [Google Scholar]
- 4.Yao H, Chen J-H, and Xu Y-F. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry 2020; 7: e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barnett B, Esper F, and Foster CB. Keeping the wolf at bay: Infection prevention and control measures for inpatient psychiatric facilities in the time of COVID-19. Gen Hosp Psychiatry 2020; 66: 51–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Russ MJ, Sisti D, and Wilner PJ. When patients refuse COVID-19 testing, quarantine, and social distancing in inpatient psychiatry: Clinical and ethical challenges. J Med Ethics 2020; 46: 579–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Benson NM, Öngür D, and Hsu J. COVID-19 testing and patients in mental health facilities. Lancet Psychiatry 2020; 7: 476–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xiang Y-T, Zhao Y-J, Liu Z-H, et al. The COVID-19 outbreak and psychiatric hospitals in China: Managing challenges through mental health service reform. Int J Biol Sci 2020; 16: 1741–1744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spitzer Sverd S, Gardner LE, Cabassa JA, et al. A Bronx tale: Exposure, containment and care on inpatient psychiatry units during COVID-19. Gen Hosp Psychiatry 2021; 69: 121–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Skelton L, Pugh R, Harries B, Blake L, Butler M, Sethi F. The COVID-19 pandemic from an acute psychiatric perspective: A London psychiatric intensive care unit experience. BJ Psych Bull 2021; 45(2): 76–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brody BD, Parish SJ, Kanellopoulos D, and Russ MJ. A COVID-19 testing and triage algorithm for psychiatric units: One hospital’s response to the New York region’s pandemic. Psychiatry Res 2020; 291: 113244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Government of Karnataka. Revised discharge. 2020. https://covid19.karnataka.gov.in/storage/pdffiles/revised%20discharge%2023.06.2020.pdf (accessed 7February2021).
- 13.Badal S, Thapa Bajgain K, Badal S, Thapa R, Bajgain BB, and Santana MJ. Prevalence, clinical characteristics, and outcomes of pediatric COVID-19: A systematic review and meta-analysis. J Clin Virol 2021; 135: 104715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zar HJ, Dawa J, Fischer GB, and Castro-Rodriguez JA. Challenges of COVID-19 in children in low- and middle-income countries. Paediatr Respir Rev 2020; 35: 70–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Somekh E, Gleyzer A, Heller E, et al. The Role of Children in the Dynamics of Intra Family Coronavirus 2019 Spread in Densely Populated Area. Pediatr Infect Dis J 2020; 39: e202–e204. [DOI] [PubMed] [Google Scholar]
- 16.Amorim R, Catarino S, Miragaia P, Ferreras C, Viana V, and Guardiano M. The impact of COVID-19 on children with autism spectrum disorder. Rev Neurol 2020; 71: 285–291. [DOI] [PubMed] [Google Scholar]
- 17.Li B, Zhang S, Zhang R, Chen X, Wang Y, Zhu C. Epidemiological and clinical characteristics of COVID-19 in children: A systematic review and meta-analysis. Front Pediatr 2020; 8: 591132. doi: https://doi.org/10.3389/fped.2020.591132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shahid Z, Kalayanamitra R, McClafferty B, et al. COVID-19 and older adults: What we know. J Am Geriatr Soc 2020; 68: 926–929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fahed M, Barron GC, and Steffens DC. Ethical and logistical considerations of caring for older adults on inpatient psychiatry during the COVID-19 pandemic. Am J Geriatr Psychiatry 2020; 28: 829–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kotfis K, Williams Roberson S, Wilson JE, Dabrowski W, Pun BT, and Ely EW. COVID-19: ICU delirium management during SARS-CoV-2 pandemic. Crit Care 2020; 24: 176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Murphy RP, Dennehy KA, Costello MM, et al. Virtual geriatric clinics and the COVID-19 catalyst: A rapid review. Age Ageing 2020; 49: 907–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spagnolo PA, Montemitro C, and Leggio L. New challenges in addiction medicine: COVID-19 infection in patients with alcohol and substance use disorders--The perfect storm. Am J Psychiatry 2020; appiajp202020040417. [DOI] [PMC free article] [PubMed]