In low- and middle-income countries (LMICs) such as India, the treatment gap for common mental disorders (CMDs) is 76% to 85%.1 Factors such as the insufficient coverage of mental health services, stigma, the lack of trained human resources, and the unavailability of a replicable and scalable model of care are some of the major reasons for this large treatment gap.2,3 The situation could be worse in the rural and remote regions of the country and among the marginalized people.4 Access to mental health care in a rural region is often limited because of issues such as stigma, sociocultural beliefs, poor coverage of national mental health programs (NMHP), non-availability of tertiary care hospitals/medical colleges, and lack of psychiatrists.5 Moreover, Asian countries, including India, are also more prone to infectious disease outbreaks and natural and human-made disasters.6 These conditions have an analogous impact on mental health in terms of an increase in the burden of mental health disorders and interruption of routine health care services, which often leads to further widening of the treatment gap for CMDs during and after such conditions.7,8
To reduce the treatment gap for CMDs, the government of India has taken initiatives such as an increase in the number of training institutes for psychiatry and allied courses and also postgraduate seats.5,9 Besides, the stepped care models may be used to improve the delivery of mental health services in the rural and inaccessible regions, with a primary focus on cost-effectiveness, accessibility, and sustainability.10
Globally, COVID-19 affected almost every aspect of health care because of the implementation of public health measures to control the spread of infection, the COVID-19-specific mortalities and morbidities, and the fear of infection.11 Published literature has focused on the impact of the COVID-19 pandemic on health care systems,12 but not on alternative models (e.g., stepped care models or matched care models). However, exploring these issues is important as these models are one of the potential strategies to address the mental health needs of the population living in the rural regions under NMHP.
Stepped Care Model of Care
Stepped care models involve collaboration among primary health care workers (HCWs, e.g., nurses) and specialized providers (e.g., psychiatrists) to improve the delivery of services.13–15 These models aim to reduce the treatment gap, increase the efficiency of service provision through the adoption of brief interventions, and enhance cost-effectiveness and are sustainable across different settings.14,16 Although the evidence for the effectiveness of stepped care models is mainly from the western countries,17 a few studies have also been attempted in LMICs, including India.18–20 These models are often considered for implementation under the NMHP of LMICs.10 Ideally, during any public health emergency, the mitigation and preparedness measures must go hand in hand for an effective, sustainable, and accessible delivery of health services. Understanding the effects of a pandemic and intersecting factors/barriers could help improve these models in terms of sustainability and accessibility during disaster or pandemic settings. In this article, we attempted to share our experiences and observations about the effect of the COVID-19 pandemic on our stepped care model for perinatal depression (brief psychological intervention for perinatal depression: BIND-P model).
Case Study
BIND-P Model
Considering the poor availability and accessibility of perinatal mental health services (PMHS) in India, we had developed and implemented a stepped care model (BIND-P model) in the rural region of Maharashtra, India.13,21 The model involves collaboration among auxiliary nurse midwives (ANMs) and psychiatric services to improve access to PMHS. It also attempts to address some barriers of implementation (e.g., stigma, inadequate or lack of training) through training of nurses and conducting awareness sessions among the general population. ANMs provide screening, brief psychological intervention for mild to moderate depression [patient health questionnaire (PHQ-2 ≥ 3, PHQ-9: 5–19)], and referral services to the perinatal women.21,22 More details about the model of care, steps, and interventions that formed the basis for the BIND-P model are published elsewhere.21,22
How has the COVID-19 Pandemic Affect the BIND-P Model?
Like other health care systems, the COVID-19 pandemic and mitigation efforts have affected the various components of the BIND-P model, namely screening, intervention, referrals, and training. Many intersecting barriers emerged during the different phases of the pandemic (we categorized them into four phases: Table 1).23 The effect of these factors on the ANM-based stepped care model (BIND-P model) was assessed using the WHO toolkit24 and described under subheadings, namely “effect on existing services” and “addressing COVID-19 mental health issues.”
Table 1.
ANM-Based Stepped Care Model (BIND-P Model): Screening Component
| Phase | Phase I Prelockdown Period |
Phase II Lockdown Period |
Phase III Unlock Period: 1 |
Phase IV Unlock Period: 2 |
|
| Period | January 17, 2020 to March 24, 2020 | March 25, 2020 to May 31, 2020#23 | June 1, 2020 to August 7, 2020 | August 8, 2020 to October 14, 2020 | |
| Screening* | Total perinatal women enrolled | 240 | 292 | 285 | 218 |
| New screening | 46 (19.16%) | 65 (22.26%) | 74 (25.96%) | 21 (9.63%) | |
| Follow-up screening | 143 (59.58%) | 184 (63.01%) | 183 (64.21%) | 165 (75.68%) | |
| Total screened | 189 (78.75%) | 249 (85.27%) | 257 (90.17%) | 186 (85.32%) | |
| Not screened | 51 (21.25%) | 43 (14.72%) | 28 (9.82%) | 32 (14.67%) | |
| Reasons for nonscreening$ | No mobile/telephone /network | NA | 20 (46.51%) | 10 (35.71%) | 12 (37.50%) |
| Mobile phone mainly with husband | NA | 4 (9.30%) | 5 (17.85%) | 6 (18.75%) | |
| Travel-related issues | 2 (3.92%) | 9 (20.93%) | 6 (21.42%) | 3 (9.37%) | |
| Fear of COVID-19 infection | NA | 5 (11.62%) | 4 (14.28%) | 3 (9.37%) | |
| Follow-up consultations in other hospitals | 26 (50.98%) (only in-person screening) |
1 (2.32%) (mixed ) |
1 (3.57%) | 2 (6.25%) | |
| Failed to contact with perinatal women | 23 (45.09%) (only in-person screening) |
4 (9.30%) | 4 (14.28%) | 6 (18.75%) | |
Note: *, ANMs screened the perinatal women using PHQ-2; $, JRF assessed the reasons for nonscreening; #, Duration of each phase: 68 days (lockdown period was considered as a reference value).
Abbreviations: NA, not assessed.
Impact on Existing Services Screening
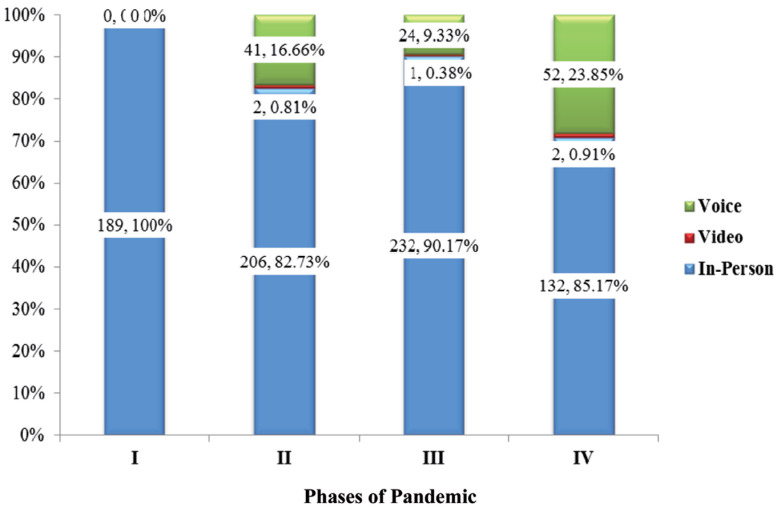
During the lockdown period (phase II), there was an abrupt increase in the number of women who screened for perinatal depression (n = 292) compared to the pre-lockdown period (n = 240; Table 1). The increase in the number of new and follow-up screenings persisted during phase III (n = 285) of the pandemic. In phase IV, there was a decline in the total number of women (n = 218) screened for depression. Also, there was a substantial increase in telephonic consultations and a reduction in the number of perinatal women who did not avail the facility for screening during phase II and phase III (Figure 1). The reasons for non-screening were assessed during subsequent follow-ups, telephonic consultations, and home visits by a project staff (junior research fellow, JRF). The most common reasons for non-screening during phases II, III, and IV were fear of COVID-19 infection and travel difficulties among those perinatal women who were screened during their in-person visits (Table 1). For others, limited access to mobile phones (for being women) and poor telephonic network were the common reasons (Table 1).
Figure 1. Perinatal Women (n, %) Screened for Depression and Screening Approaches During the Pandemic.
Note: Denominator, number of perinatal women completed screening for depression.
Interventions and Referral Services
The proportion of perinatal women who screened positive for depression decreased in phase II, i.e., lockdown period (9.63%), compared to phase I, i.e., prelockdown period (12.16%; Table 2). Subsequently, there was an increase in the proportion of women who screened positive, in phases III (11.57%) and IV (18.80%). Similarly, there was an increase in the number of women receiving the ANM-based brief psychological intervention (BIND-P intervention) and referral services (n = 4; Table 2). The BIND-P intervention components include exercise, sleep hygiene, dietary recommendations, and monitoring sheets (published elsewhere).21,22 These dietary recommendations are directed towards preventing common nutritional deficiencies (e.g., iron deficiency anemia, vitamin B12 deficiency). During the follow-up visits, the women were expected to submit the self-recorded dietary intake in the chart provided. In the COVID-19 pandemic, the women faced difficulties in following the recommended diet because of movement restrictions (e.g., closure of the weekly market and food transportation services) and unemployment.
Table 2.
ANM-Based Stepped Care Model (BIND-P Model): Intervention and Referral Component
| Phase | Phase I | Phase II | Phase III | Phase IV | |
| Screened positive (PHQ-2 ≥ 3) and considered for intervention | 23 (12.16%) | 24 (9.63%) | 33 (11.57%) | 41 (18.80%) | |
| Delivery of intervention* | In-person | 20 (86.95%) | 16 (66.66%) | 23 (69.69%) | 16 (39.02%) |
| Video | NA | NA | NA | NA | |
| Voice (telephonic) | NA | 3 (12.5%) | 1 (3.30%) | 11 (26.82%)$ | |
| Mixed (in-person + voice ) | NA | 1 (4.16%) | 5 (15.15%) | 7 (17.07%)$ | |
| Drop out# | 3 (1.30%) | 4 (16.66%) | 4 (12.12%) | 7 (17.07%) | |
| Reasons for dropout# | No telephone or mobile network | 2 (66.66%) | 1 (25.00%) | 1 (25.00%) | 3 (42.85%) |
| Mobile phone accessible to husband | 1 (33.33%) | 1 (25.00%) | 2 (50.00%) | 2 (28.57%) | |
| Travel-related issues or fear of COVID-19 infection | NA | 1 (25.00%) | 1 (25.00%) | 2 (28.57%) | |
Note: *, ANMs delivered the intervention; #, JRFs conducted the assessments; $, migration during the unlock period.
Abbreviations: NA, not assessed.
Those who failed to attend the in-person consultation for screening and intervention were approached via phone by the ANMs.The video consultation for both screening and intervention failed because of the lack of access to the internet, the lack of telephonic network, the low quality of phones, and the mobile phone being with the husband (Tables 1 and 2). Therefore, the voice call was attempted to screen or deliver the intervention. Most women were not comfortable discussing their mental health issues on the telephone at home, in the presence of their in-laws or husbands. These issues were reported to the ANMs during face-to-face or phone consultations.
Service Providers
Before the lockdown period (phase I), a total of five ANMs were providing services for screening and intervention through the BIND-P model. At the beginning of the lockdown period, two were redeployed in COVID-19 care settings and one for community-based surveys. Further, although we approached to train new ANMs (n = 17) for perinatal depression screening and intervention, only one was trained from March 25, 2020 to October 14, 2020. The COVID-19-related responsibilities (e.g., screening, household survey), the lack of prior experience with video conferencing, and the non-availability of the internet were the reasons cited by the ANMs.
Addressing COVID-19 Mental Health Issues
During regular screening and intervention, the ANMs noticed that some women were not aware of precautionary measures and specific care related to COVID-19. Myths and misinformation (e.g., skepticism about breastfeeding and considering the option of formula milk) were also circulating among them. Illiterate women and those who did not have a mobile phone or access to the internet were protected from such infodemic.
But, issues such as the scarcity of perinatal mental health experts in India, lack of time, rapidly changing COVID-19-specific policies, unavailability of ANMs for training, and human resource constraints at the rural level (redeployment of existing ANMs for COVID-19 purposes) prevented us from preparing and addressing the COVID-19-specific mental health issues through appropriate and specific interventions.
However, considering this complex, unpredictable pandemic that has affected people living in the rural and remote regions and the vulnerable population, we have made a few efforts to address some COVID-19-related mental health issues. The ANMs, under the supervision of project staff (e.g., JRFs), made several attempts to reach the perinatal women registered with us. A WhatsApp group was formed to disseminate COVID-19-related information. The group had 176, 184, and 210 members at the end of phases II, III, and IV, respectively. The ANMs disseminated COVID-19-related information and education material (e.g., etiology, transmission, and safety measures) published daily by the Ministry of Health and Family Welfare, India, on their Twitter handle. We were not able to assess whether this information reached the participants and whether or not they benefited from this. But, creating awareness among perinatal women about COVID-19 through the available resources was considered a priority. Besides, ANMs also provided virtual and telephone support consisting of reassurance, evaluation of mood symptoms, and education of breastfeeding practices to all the women as and when required.
Discussion
Although the COVID-19 pandemic and mitigation efforts have affected our BIND-P model, perinatal women’s periodic screening with brief standardized screening tools (e.g., PHQ-2, PHQ-9) was found to be useful to identify and monitor depression and to provide first-level interventions along with referral services. In the presence of many hurdles such as the paucity of organizations, lack of preparation, increase in the number of service users, and human resource constraints, we attempted to overcome some barriers and provided sustainable and efficient services. The abrupt rise in the number of service users was mainly because of the migration of perinatal women from metropolitan cities (Mumbai and Pune) to their hometowns (Konkan), i.e., rural regions, and an increase in the pregnancy rate during the lockdown period.25 The migration of perinatal women was mainly because of fear of getting COVID-19, unemployment, and food insecurity (because of the closure of markets and food transportation services).25
The in-person consultations were not much affected, maybe because of the relatively low number of COVID-19 cases, a few alternative options for perinatal care, and a decreased impact of infodemic (because of digital illiteracy, poor telephonic network) in the rural regions. But, the safety precautions or measures (e.g., masks) compromised communication, the establishment of rapport, enabling environment for breastfeeding, and delivery of the psychological intervention, as in other reports.26 Also, video consultation was not feasible and acceptable in rural regions, for both service providers and service users. This was because of the poor quality of internet connectivity (variable from village to village), low technological literacy, disrupted telephonic network, sex-based access to a phone (mainly husband has access to a mobile phone), illiteracy or lower education, poverty, high internet costs, and confidentiality and privacy concerns. Further, telephonic (voice) screening and intervention were preferred to video consultations, and there was a gradual increase in the number of users (voice) across the different phases.
The decline in the proportion of women with perinatal depression during the lockdown period (phase II) could be because of increased family time and support during the early lockdown period and the heroic, honeymoon phase of a pandemic.27 In contrast, the subsequent increase in women found to have perinatal depression (phases III and IV) is indicative of the catastrophic impact of the COVID-19 pandemic and mitigation efforts. But these findings should be interpreted cautiously because of the relatively small sample size. Despite the availability of newly developed screening tools (e.g., fear of COVID-19, coronavirus anxiety scales),28 the lack of availability of ANMs for in-person or virtual training affected the screening of these women for COVID-19-specific mental health issues. Some women canceled their visits because of fear of infection in the hospital settings either from other patients or HCWs, public health advisory for pregnant women, and lack of transport facilities, particularly during the lockdown period. Misconceptions, such as being skeptical about breastfeeding and considering the option of formula milk, were circulating among perinatal women, as reported previously.29,30
During the pandemic, policymakers, psychiatrists, and researchers focused more on telepsychiatry services or virtual training.31,32 No doubt, these services are valuable to reduce the treatment gap for people with mental illness. But our experience suggests that direct service-user-based telepsychiatry may not be a feasible choice in rural settings because of the reasons listed above. Also, the Government of India tried to assist the people by developing helplines and telepsychiatry care during the pandemic.33 However, such an initiative was not accessible to women living in rural or remote areas. On the contrary, the ANMs, being the grass-roots health workers, played a vital role in delivering services during the pandemic. For these women, the ANMs were one of the few accessible health care providers during the pandemic. This model has provided an opportunity for rural perinatal women to interact with either the nurse or mental health professionals as and when required and obtain authentic information.
In the future, the primary health care worker (e.g., ANM) based stepped care model could be beneficial for communication, coordination, and collaboration among different stakeholders and mental health professionals for CMDs in complex settings of pandemics or disasters.10,34 In the presence of constraints like interruption of services, loss of support, and virtual connectivity, stepped care models could sustain the mental health services in the rural and remote regions.21 Also, these models could be more helpful if HCWs receive regular training. To the best of our knowledge, this is the first report to discuss the challenges with stepped care models adopted for mental health. Unfortunately, barriers like complexities involved in a pandemic and rapidly changing situations, being the most vulnerable population (perinatal women and infants), and limited research capacity for mental health in the rural regions prevented us from conducting well-organized research.
Way Forward
To a certain extent, the ANM-based stepped care model was sustainable, effective, acceptable, and feasible in the remote and rural regions of India during the pandemic. However, the following measures should be considered to improve these models.
Infrastructure: Provision of internet, mobile network, electricity, and mobile phones at concessional rates to marginalized populations could be an ideal option. But for the time being, services can be provided through ANMs and a network of HCWs. India has the advantage of a well-established network of HCWs like accredited social health activists, anganwadi workers, and ANMs, which would help to facilitate cost-effective and sustainable delivery of mental health services.10,35
Primary Mental Health Interventions Protocol Under the Stepped Care Model: The inclusion of primary mental health interventions in public health emergencies or disaster protocol may improve the screening and provision of psychological first aid under these models. Researchers and policymakers should empower these HCWs through appropriate training and networking them with specialists, as in the BIND-P model.
Specific Arrangement for Mental Health: Maternal and child health services are a priority area for the government of India.36 Therefore, it is important to consider the stepped care model for the delivery of perinatal mental health care under the National Health Mission in the future.
Capacity Building and Research: Research on stepped care models in routine care, disaster, or public emergency settings is limited. Therefore, further research should focus on developing, implementing, and evaluating promising and effective interventions through these models to provide high-quality, first-level, and periodic screening for CMDs. Also, efforts should be directed toward increasing the health care capacity through training, coordination, support, and adequate funding.
Conclusion
Despite many challenges, the stepped care model was found to be sustainable, effective, and feasible for providing mental health services in the remote and rural regions of India. Some efforts with limited success were also made to address the COVID-19-specific mental health issues. Addressing challenges and barriers experienced during a pandemic can improve mental health services during public health emergencies and disasters in the future.
Acknowledgments
This work is part of the BIND-P project (CTRI/2018/07/014836). The work was supported by the Indian Council Medical Research (ICMR) under capacity building projects for national mental health program, ICMR-NMHP. We would like to thank Dr Soumya Swaminathan (then Secretary, Dept. of Health Research, DHR), Dr Balram Bhargav, current Secretary DHR, Prof. V.L. Nimgaonkar, Dr Ravinder Singh, Dr Harpreet Singh, and Dr Krushnaji Kulkarni. We also thank the faculty of “Cross-Fertilized Research Training for New Investigators in India and Egypt” (D43 TW009114, HMSC File No. Indo-Foreign/35/M/2012-NCD-1, funded by Fogarty International Centre, NIH). We acknowledge the constant support and guidance of the National Coordinating Unit of ICMR for NMHP Projects. We are thankful to the Data Management Unit of ICMR for designing the database. We would like to thank the ANM staff (Sadhana Mohite, Shital Jadhav, Akashta Lingayat, Harshada Katkar, Sakshi Kodare) who coordinated data collection, training, and awareness sessions. The content of this manuscript is solely our responsibility and does not necessarily represent the official views of NIH or ICMR. NIH and ICMR had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Ethical Statement: Ethical approvals were obtained from the BKL Walawalkar Rural Medical College, Maharashtra; Lady Hardinge Medical College, New Delhi; and Yenepoya Medical College, Karnataka and Dharwad Institute of Mental Health and Neurosciences (DIMHANS), Karnataka.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Gururaj G, Varghese M, Benegal V, et al. National Mental Health Survey of India, 2015-16: Summary. Bengaluru: National Institute of Mental Health and Neuro, Sciences; (NIMHANS Publication No. 128) 2016. [Google Scholar]
- 2.Singh OP. Closing treatment gap of mental disorders in India: Opportunity in new competency-based Medical Council of India curriculum. Indian J Psychiatry, 2018; 60 375–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gupta S and Sagar R. National mental health program-optimism and caution: A narrative review. Indian J Psychol Med, 2018; 40 509–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kumar A. Mental health services in rural India: Challenges and prospects. Health (N Y), 2011; 03 757–761. [Google Scholar]
- 5.Ransing RS, Agrawal G, Bagul K, et al. Inequity in distribution of psychiatry trainee seats and institutes across Indian states: A critical analysis. J Neurosci Rural Pract, 2020; 11 299–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kokai M, Fujii S, Shinfuku N, et al. Natural disaster and mental health in Asia. Psychiatry Clin Neurosci, 2004; 58 110–116. [DOI] [PubMed] [Google Scholar]
- 7.Esterwood E and Saeed SA. Past epidemics, natural disasters, COVID-19, and mental health: Learning from history as we deal with the present and prepare for the future. Psychiatr Q, 2020; 91 1121–1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moreno C, Wykes T, Galderisi S, et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry, 2020; 7 813–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kakunje A, Punnoose VP, Ponnusamy KP, et al. Revisiting postgraduate (PG) psychiatry training in India. Indian J Psychol Med, 2019; 41 380–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Behera P, Amudhan RS, Gupta R, et al. Adapting the stepped care approach for providing comprehensive mental health services in rural India: Tapping the untapped potential. Indian J Community Fam Med, 2018; 4: 5. [Google Scholar]
- 11.Pelizza L and Pupo S. The COVID-19 pandemic and Italian public mental health services: Experience and future directions. J Patient Exp, 2020; 7 642–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.WHO COVID-19 disrupting mental health services in most countries, WHO survey, https://www.who.int/news/item/05-10-2020-covid-19-disrupting-mental-health-services-in-most-countries-who-survey (2020, accessed 2February2021).
- 13.Olin S-CS, McCord M, Stein REK, et al. Beyond screening: A stepped care pathway for managing postpartum depression in pediatric settings. J Womens Health, 2017; 26 966–975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reeves P, Szewczyk Z, Proudfoot J, et al. Economic evaluations of stepped models of care for depression and anxiety and associated implementation strategies: A review of empiric studies. Int J Integr Care, 2019; 19: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maehder K, Löwe B, Härter M, et al. Management of comorbid mental and somatic disorders in stepped care approaches in primary care: A systematic review. Fam Pract, 2019; 36 38–52. [DOI] [PubMed] [Google Scholar]
- 16.Meuldijk D and Wuthrich VM. Stepped care treatment of anxiety and depression in older adults: A narrative review. Aust J Rural Health, 2019; 27 275–280. [DOI] [PubMed] [Google Scholar]
- 17.Ho FY-Y, Yeung W-F, Ng TH-Y, et al. The efficacy and cost-effectiveness of stepped care prevention and treatment for depressive and/or anxiety disorders: A systematic review and meta-analysis. Sci Rep, 2016; 6: 29281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pereira B, Andrew G, Pednekar S, et al. The integration of the treatment for common mental disorders in primary care: Experiences of health care providers in the MANAS trial in Goa, India. Int J Ment Health Syst, 2011; 5: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Michelson D, Malik K, Krishna M, et al. Development of a transdiagnostic, low-intensity, psychological intervention for common adolescent mental health problems in Indian secondary schools. Behav Res Ther, 2020; 130: 103439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mendenhall E, De Silva MJ, Hanlon C, et al. Acceptability and feasibility of using nonspecialist health workers to deliver mental health care: Stakeholder perceptions from the PRIME district sites in Ethiopia, India, Nepal, South Africa, and Uganda. Soc Sci Med, 2014; 118 33–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ransing R, Kukreti P, Raghuveer P, et al. Development of a brief psychological intervention for perinatal depression (BIND-P). Asia-Pac Psychiatry, 2021; 13: e12436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Raghuveer P, Ransing R, Kukreti P, et al. Effectiveness of a brief psychological intervention delivered by nurse for depression in pregnancy: Study protocol for a multicentric randomized controlled trial from India. Indian J Psychol Med, 2020; 42: S23–S30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Saha J and Chouhan P. Lockdown and unlock for the COVID-19 pandemic and associated residential mobility in India. Int J Infect Dis, 2021; 104 382–389. [DOI] [PubMed] [Google Scholar]
- 24.TDR | Implementation research toolkit. WHO, http://www.who.int/tdr/publications/topics/ir-toolkit/en/ (accessed 5January2021). [Google Scholar]
- 25.Jungari S. Maternal mental health in India during COVID-19. Public Health, 2020; 185 97–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Veluri N. Are masks impacting psychiatric inpatients’ treatment? Psychiatry Res, 2020; 293: 113459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Math SB, Nirmala MC, Moirangthem S, et al. Disaster management: Mental health perspective. Indian J Psychol Med, 2015; 37 261–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ransing R, Ramalho R, Orsolini L, et al. Can COVID-19 related mental health issues be measured? Brain Behav Immun, 2020; 88 32–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brown A and Shenker N. Experiences of breastfeeding during COVID-19: Lessons for future practical and emotional support. Matern Child Nutr. Epub ahead of print 23 September 2020. DOI: 10.1111/mcn.13088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.van Tulleken C, Wright C, Brown A, et al. Marketing of breastmilk substitutes during the COVID-19 pandemic. Lancet Lond Engl. Epub ahead of print 8 October 2020. DOI: 10.1016/S0140-6736(20)32119-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ibrahim FA, Pahuja E, Dinakaran D, et al. The future of telepsychiatry in India. Indian J Psychol Med, 2020; 42: 112S-117S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dhawan S. Online learning: A panacea in the time of COVID-19 crisis. J Educ Technol Syst, 2020; 49 5–22. [Google Scholar]
- 33.Ransing R, Kar SK, and Menon V. National helpline for mental health during COVID-19 pandemic in India: New opportunity and challenges ahead. Asian J Psychiatry, 2020; 54: 102447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Adiukwu F, Orsolini L, Gashi Bytyçi D, El Hayek S, Gonzalez-Diaz J, Larnaout A. et al. COVID-19 mental health care toolkit: An international collaborative effort by Early Career Psychiatrists section. Gen Psychiatry, 2020; 33(5): e100270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Prinja S, Jeet G, Verma R, et al. Economic analysis of delivering primary health care services through community health workers in 3 North Indian states. PLoS ONE, 2014; 9: e91781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Maternal health: National health mission, https://www.nhm.gov.in/index1.php?lang=1&level=2&sublinkid=822&lid=218 (2021, accessed 14February2021).