Abstract
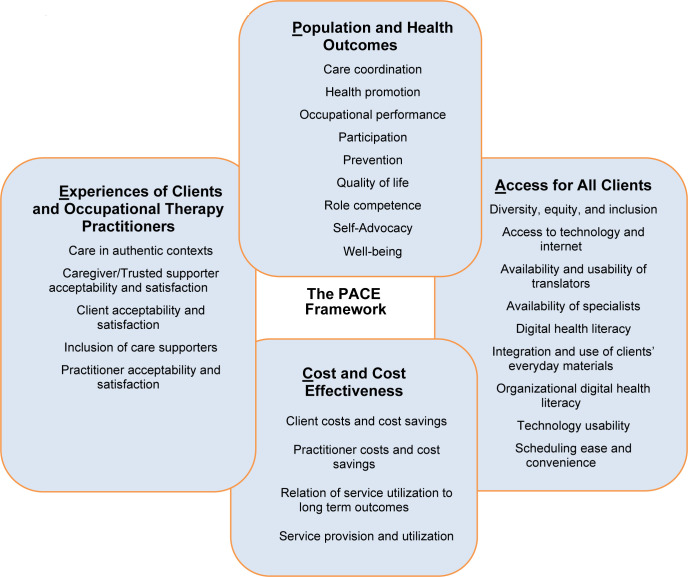
The use of telehealth to deliver occupational therapy services rapidly expanded during the COVID-19 pandemic. There are frameworks to evaluate services delivered through telehealth; however, none are specific to occupational therapy. Therefore, occupational therapy would benefit from a framework to systematically evaluate components of telehealth service delivery and build evidence to demonstrate the distinct value of occupational therapy. The PACE Framework outlines four priority domains to address areas of need: (1) Population and Health Outcomes; (2) Access for All Clients; (3) Costs and Cost Effectiveness; and (4) Experiences of Clients and Occupational Therapy Practitioners. This article describes the development and expert reviewer evaluation of the PACE Framework. In addition, the PACE Framework's domains, subdomains, and outcome measure examples are described along with future directions for implementation in occupational therapy research, practice, and program evaluation.
Keywords: Occupational therapy, PACE Framework, Program evaluation, Research, Telehealth
The use of telehealth to deliver occupational therapy services rapidly expanded due to the COVID-19 pandemic as practitioners in community-based settings, early intervention, hospitals, nursing homes, outpatient clinics, and schools pivoted to using telehealth to serve clients. The American Occupational Therapy Association (AOTA, 2018) defined telehealth as the “application of evaluative, consultative, preventative, and therapeutic services delivered through information and communication technology (p. 1).” Before and during the pandemic, AOTA was active in educating occupational therapy practitioners (occupational therapists and occupational therapy assistants) about telehealth through practice guidance and position papers (AOTA, 2005, 2010, 2013, 2018, 2021). Additionally, research had demonstrated the efficacy, client satisfaction, and potential cost savings of occupational therapy services delivered through telehealth (for reviews see Nissen & Serwe, 2018; Nobakht et al., 2017). However, lack of payment structures and associated decreased system and clinician utilization of telehealth limited its use in occupational therapy practice until the pandemic. The pandemic emphasized the need for quality, evidence-based approaches to telehealth delivery, and offered significant opportunities to collect and analyze data related to the implementation and outcomes of telehealth. Occupational therapy could benefit from a framework from which to draw and organize the data and guide future research and program evaluation.
There are existing frameworks for the evaluation and measurement of healthcare services delivered through telehealth. The National Quality Forum (2017) outlined four domains of measurement in telehealth: access to care, financial impact and/or cost, experience, and effectiveness. The Institute of Health (Berwick et al., 2008; Bodenheimer & Sinsky, 2014) described four pillars of telehealth, including the patient care experience, population health, affordability, and improved work-life for the practitioner. Recently, the American Academy of Pediatrics (Chuo et al., 2020) outlined four domains of measurement for pediatric focused care delivered through telehealth: health outcomes; health delivery (e.g., quality and cost); experience; and program implementation and key performance indicators. These frameworks share similarities; however, no existing framework captures the distinct measurement and evaluation needs of occupational therapy services and programs delivered through telehealth. Telehealth offers only a tool through which occupational therapy services are delivered, such a framework would encompass many concepts and ideas that are profession specific but not necessarily different when approached through telehealth versus in-person service delivery.
The occupational therapy profession would benefit from a framework that serves as a resource to support evaluation of evidence-based telehealth practices. The purpose of this article is to describe the PACE Framework for measurement and evaluation of occupational therapy services delivered through telehealth. We draw from existing frameworks of telehealth measurement to propose four domains that are priorities for occupational therapy: (1) Population and Health Outcomes; (2) Access for All Clients; (3) Costs and Cost Effectiveness; and (4) Experiences of Clients and Occupational Therapy Practitioners.
METHOD
TELEHEALTH PLANNING GRANT COLLECTIVE
In October 2020, the American Occupational Therapy Foundation (AOTF) convened a Planning Grant Collective titled “Stimulating Research to Advance Evidence-Based Applications of Telehealth in Occupational Therapy.” This event led to the identification of several areas of telehealth research and practice. These areas were described in a publication with outcomes from that meeting (Proffitt et al., 2021). Existing telehealth frameworks were consulted in an attempt to: (a) examine the need for a new framework to collect and analyze data related to telehealth implementation, (b) capture the distinct value of occupational therapy, and (c) identify outcomes of telehealth across occupational therapy settings and populations. This process resulted in the development of the PACE Framework. Following the AOTF 2020 Planning Grant Collective, members of the AOTF Planning Grant Collective Organizing Committee continued to meet to conceptualize the PACE Framework, outline a process and agenda for expert stakeholder review, and analyze and integrate stakeholder feedback.
OCCUPATIONAL THERAPY STAKEHOLDER EVALUATION
Prior to inviting stakeholder review of the PACE framework, the Institutional Review Board granted exempt status to the review process. We invited nine stakeholders with various backgrounds in occupational therapy practice and research and representation across practice settings (e.g., outpatient rehabilitation, early intervention), to review the PACE Framework and provide feedback. Specifically, we asked the stakeholders to use a sliding scale of 1–100 to rate the (1) clarity of the PACE Framework (0=not clear at all to 100=exceptionally clear), (2) utility of the PACE Framework (0=not useful at all to 100=exceptionally useful), (3) content of the PACE Framework (0=critical components are missing to 100=all critical components are well addressed), (4) distinctness of each construct (0=not distinct at all to 100=constructs are completely distinct), (5) alignment of outcomes within each construct (0=not aligned to 100=exceptionally aligned), and (6) possibility of implementation of the PACE Framework (0=I would not recommend PACE Framework to a colleague to 100=I would highly recommend the PACE Framework to a colleague). We also asked stakeholders four open-ended questions focused on general feedback, inclusion of additional constructs, outcomes or measures, and the ways in which the PACE Framework may be implemented in their respective practice and/or research settings.
DATA ANALYSIS AND FRAMEWORK REFINEMENT
We used descriptive statistics to examine quantitative stakeholder responses (n=8; one stakeholder did not respond) and compiled qualitative responses for each question to refine the framework. We used content analysis (Elo & Kyngäs, 2008) to examine qualitative responses. Continuous discussion among the authors, along with integration of quantitative and qualitative stakeholder feedback, led to revisions that assured that the PACE Framework presented in this article captured domains, outcomes, and outcome measures related to occupational therapy. Quantitative ratings from the expert review panel are shown in Table 1.
Table 1.
Quantitative Ratings from the Expert Review Panel
| Item | Mean (SD) | Range |
|---|---|---|
| Clarity | 82.88 (10.76) | 71–100 |
| Utility | 81.13 (16.58) | 50–100 |
| Content | 87.25 (6.43) | 75–93 |
| Distinctness | 83.75 (22.51) | 30–100 |
| Alignment | 84.14 (10.64) | 68–95 |
| Possibility of Implementation | 83.88 (11.76) | 66–100 |
Based on content analysis of qualitative responses, we discussed how to integrate stakeholder feedback within the PACE Framework. Qualitative comments that resulted in edits to the PACE Framework are shown in Table 2. First, in response to qualitative comments on general impressions and feedback, we added and removed numerous measurement tools to have a balance of adult and pediatric populations. Second, in response to suggestions about missing constructs, we emphasized the link between the primary domain of Access for All Clients s as it may be related to social determinants of health (see Results). We also emphasized that outcomes may include reported measures (e.g., occupational therapy practitioner, client, caregiver) and/or evidence from documentation or medical records. Third, we responded to reviewer suggestions about missing outcome measures by adding suggested assessments. We removed any condition specific outcome measures because researchers and/or practitioners are equipped with such knowledge of assessments specific to their contexts (e.g., stroke versus autism spectrum disorder specific measures). Fourth, with regard to envisioned use, we emphasized that the PACE Framework may be used to support evidence-based occupational therapy services, and includes both outcome and process measures.
Table 2.
Qualitative Comments that Resulted in Edits to the PACE Framework
| Survey Question | Expert Reviewer Comments | Resulting Edits |
|---|---|---|
| What are your overall impressions and general feedback? |
“More adult outcome tools and examples are needed” “Very comprehensive” “The PACE Framework is an excellent tool to use to guide telehealth research and program evaluation” “Having a reminder will foster better quality” |
More balanced outcome measures that represented pediatrics and adult populations were included. |
| Is the PACE Framework missing any constructs? |
“Perhaps need to look at how SDOH [social determinants of health] affect implementation” “Consider separating client reported outcomes and practitioner reported outcomes” |
In the Results section, we included increased supporting text to ensure that social determinants of health (SDOH) are considered within the Access construct. We also specified why client and practitioner reported outcomes were included, and added suggested outcome measures. |
| Is the PACE Framework missing specific outcome measures? |
“Days absent from school/truancy/attendance at community support activities” “Numerous specific assessments were recommended for +/− (i.e. “cancer or lymphedema QOL [quality of life] scales)” “Well-being could be expanded to include a few common caregiver burden scales” |
We included an explanation for not including diagnosis-specific assessments in the text and added suggested scales. |
| How do you envision implementing the PACE Framework? | “…I think being clear about what is measuring telehealth as a delivery method (such as access and cost, satisfaction) versus outcomes of the intervention (participation, occupational performance) versus processes that are enhanced by telehealth (e.g., collaboration, coordination) would be helpful.” | In response to the comment, we emphasized that the PACE Framework includes both process measures and outcome measures throughout the text. |
OVERVIEW OF THE PACE FRAMEWORK
The PACE Framework is comprised of four domains: (1) Population and Health Outcomes; (2) Access for All Clients; (3) Costs and Cost Effectiveness; and (4) Experiences of Clients and Occupational Therapy Practitioners. Within each domain, we included a number of possible outcomes and associated operational definitions that aligned with AOTA's Occupational Therapy Practice Framework – 4th Edition (2020d) and/or the World Health Organization (2001) when possible. The PACE Framework also includes measurable subdomains within outcomes, as many outcomes are broad in nature and may be broken into measurable components. We propose that the four domains of the PACE Framework and associated areas of specific measurement (see Table 3) can be used to capture the distinct value of occupational therapy delivered across settings and populations. The PACE Framework is unique from other telehealth measurement and evaluation guidelines, as we aligned telehealth measurement and evaluation domains with the specific needs of occupational therapy.
Table 3.
The PACE Framework
| Population and Health Outcomes | ||
|---|---|---|
| Outcome | Operational Definition and Measurable Sub-Domains | Examples of Outcome Measures |
| Care coordination |
Policies and practices that create coherent and timely client-centered care both within and across care settings and over time. Examples include:
|
|
| Health promotion |
“Process of enabling people to increase control over, and to improve, their health. To reach a state of complete physical, mental, and social well-being, an individual or group must be able to identify and realize aspirations, to satisfy needs, and to change or cope with the environment” (World Health Organization, 1986). Examples include:
|
Groups & Populations
Individuals
|
| Occupational performance |
“Accomplishment of the selected occupation resulting from the dynamic transaction among the client, their contexts, and the occupation” (AOTA, 2020d, p. 8). Examples include:
|
|
| Participation |
“Involvement in a life situation” (World Health Organization, 2001, p. 10). Examples include:
|
|
| Prevention |
“Education or health promotion efforts designed to identify, reduce, or prevent the onset and decrease the incidence of unhealthy conditions, risk factors, diseases, or injuries” (American Occupational Therapy Association, 2020d, p. 81). Examples include:
|
Analysis of data related to:
|
| Quality of life |
“Dynamic appraisal of the client's life satisfaction (perceptions of progress toward goals), hope (real or perceived belief that one can move toward a goal through selected pathways), self-concept (composite of beliefs and feelings about oneself), health and functioning (e.g., health status, self-care capabilities), and socioeconomic factors (e.g., vocation, education, income; adapted from Radomski, 1995)” (AOTA, 2020d, p. 66). Examples include:
|
|
| Role competence |
“Ability to effectively meet the demands of the roles in which one engages” (AOTA, 2020d, p. 67). Examples include:
|
|
| Self-Advocacy |
“Advocacy for oneself, including making one's own decisions about life, learning how to obtain information to gain an understanding about issues of personal interest or importance, developing a network of support, knowing one's rights and responsibilities, reaching out to others when in need of assistance, and learning about self-determination” (AOTA, 2020d, p.83). Examples include:
|
|
| Well-being |
“Contentment with one's health, self-esteem, sense of belonging, security, and opportunities for self-determination, meaning, roles, and helping others” (AOTA, 2020d, p. 67). “A general term encompassing the total universe of human life domains, including physical, mental, and social aspects, that make up what can be called a ‘good life’” (World Health Organization, 2006, p. 211). Examples include:
|
Caregiver
Client
|
| Access for All Clients | ||
| Diversity, equity and inclusion [This topic merits extensive content, which is beyond the scope of this article and must be fully addressed in future work.] | In accord with AOTA's commitment to diversity, equity, and inclusion (AOTA, 2020b) and the AOTA Vision 2025 (AOTA, n.d.-a), telehealth research, practice, and policy should reflect diversity in race, ethnicity, gender, age, socio-economic status, geography, and other demographics; promote occupational justice; and be client-centered. |
Outcome measures can be extracted from the following guides:
|
| Access to technology and internet |
The extent to which technology and available internet data is sufficiently available and affordable to individuals and communities. Examples include:
|
|
| Availability and usability of translators |
The ways in which an organization supports the availability and quality of translation services for clients to access services. Examples include:
|
|
| Availability of specialists |
The extent to which telehealth extends the availability of providers with specializations and/or certifications. Examples include:
|
|
| Digital health literacy |
The degree to which individuals have the ability to find, understand, and use information and services to inform health-related decisions and actions for themselves and others. Examples include:
|
|
| Integration and use of clients’ everyday materials |
The ways in which assessment and intervention sessions use clients’ readily available materials in their natural contexts. Examples include:
|
|
| Organizational digital health literacy |
The degree to which organizations equitably enable individuals to find, understand, and use information and services to inform health-related decisions and actions for themselves and others (CDC, 2021). Examples include:
|
|
| Technology usability |
The extent to which available technology is appropriate for telehealth access, including evaluation and intervention sessions. Examples include:
|
|
| Scheduling ease and convenience |
Client reports of scheduling ease as convenient and fitting into daily life. Examples include:
|
|
| Cost and Cost Effectiveness | ||
| Client costs and cost savings |
The costs and cost savings associated with accessing and attending telehealth sessions; clients may save expenses due to convenience of telehealth and/or incur costs if any additional technology or data is necessary to access telehealth sessions. Examples include:
|
Costs
Savings
|
| Practitioner costs and cost savings |
The costs and cost savings among practitioners that result from telehealth. Examples include:
|
|
| Relation of service utilization to long term outcomes |
The degree to which costs of occupational therapy delivered through telehealth are associated with long term health and/or developmental outcomes across clients and settings. Examples include:
|
|
| Service provision and utilization | The extent to which occupational therapy services are offered, available, and attended by clients across settings and communities. |
|
| Experiences of Clients and Occupational Therapy Practitioners | ||
| Authentic contexts | The extent to which telehealth sessions occur within clients’ authentic contexts and address clients’ everyday activities. |
|
| Caregiver/care partner acceptability and satisfaction | The acceptability and perceived quality of the service delivery mechanism from the perspective of the caregiver for younger clients and/or trusted supporter for older clients. |
|
| Client acceptability and satisfaction | The perceived acceptability, value, and client attributed outcomes of telehealth delivered occupational therapy services. |
|
| Inclusion of care partners (caregiver/family/other) | The extent to which clients’ care supporters actively participate in and are included in the occupational therapy process (i.e., assessment, intervention, re-evaluation). |
|
| Practitioner acceptability and satisfaction | The extent to which occupational therapy practitioners perceive that telehealth promotes wellness, reduces burnout, and is an effective mechanism to deliver assessments and interventions that meet clients’ needs and achieve evidence-based practice standards. |
|
The PACE Framework was designed for outcome and process evaluation of evidence-based interventions delivered through telehealth. Although specific elements of the PACE Framework are applicable to in-person occupational therapy services, the entirety of the Framework was created with the intention of informing telehealth and hybrid service delivery. Therefore, the example outcome measures provided are easily administered through telehealth. Example outcome measures reflect observation, process evaluation, and self-, caregiver-, and practitioner-report, as well as evidence that may be gathered through chart and/or documentation review. There is a lack of evidence supporting administration of behavioral/performance-based assessments, and we chose not to include many of these in the PACE Framework (AOTA, 2018). The PACE Framework is shown in Table 3.
In accord with AOTA's commitment to diversity, equity, and inclusion (AOTA, 2020b) and the AOTA Vision 2025 (AOTA, n.d.-a), telehealth research, practice, and policy should reflect diversity in race, ethnicity, gender, age, socio-economic status, geography, and other demographics; promote occupational justice; and be client-centered. All programs and research projects that use telehealth must consider how to integrate measures that capture the complexities associated with uncovering inequities that may be associated with the use of telehealth and/or how telehealth may be used to overcome inequities in access. Occupational therapy researchers, practitioners, and policy-makers must consider how measurement across all domains within the PACE Framework will contribute to ongoing discourse and subsequent actions to address inequity. While a full discussion of how telehealth intersects with diversity, equity, and inclusion is beyond the scope of this article, we do suggest the following resources as examples that may guide telehealth programming and measurement across domains: (1) Diversity, Equity and Inclusion in Occupational Therapy, Resources and the DEI Tool Kit (AOTA's, n.d.-b); (2) Equity & Inclusion Lens Guide (Non-Profit Association of Oregon, 2018); (3) Disability Inclusion Toolkit (Ford Foundation, n.d.) and (4) Guide to Acknowledging the Impact of Discrimination, Stigma, and Implicit Bias on Provision of Services (AOTA, 2020a). While diversity, equity, and inclusion are relevant to all domains of the PACE Framework, potential measures are represented in the Access for All Clients domain. To underscore the importance of measurement and consideration of diversity, equity, and inclusion as well as to avoid a circumstance wherein consumers of the PACE Framework might overlook this critical area, it is visually represented in the Access for All Clients domain.
POPULATION AND HEALTH OUTCOMES
Occupational therapy delivered through telehealth is ultimately aimed at increasing individuals’ participation in everyday activities within authentic contexts to improve health. The PACE Framework captures approaches to telehealth intervention that occur at the person, group, and population levels. Given occupational therapy's focus on participation, our measurement approaches should encompass methods of understanding the influence of telehealth on population health as well as individual client outcomes. Occupational therapy outcomes within the Population and Health Outcomes domain include care coordination, occupational performance, participation, prevention, promotion of health and wellness, quality of life, role competence, self-determination/self-management, and caregiver and client well-being (AOTA, 2020d). The outcomes of occupational therapy services are numerous; the purpose of the PACE Framework is to outline outcomes appropriate for telehealth service delivery. Therefore, the outcomes and associated measures in this section are limited to ones that lend themselves to telehealth (e.g., objective measures from documentation or medical records; observation; self-, practitioner-, and caregiver-report) and span age ranges, practice settings, and populations.
ACCESS FOR ALL CLIENTS
We conceptualize the measurement and evaluation of access broadly. Access to telehealth is not limited to technology and internet, although both are vital to telehealth use. We structured the PACE Framework domain of Access for All Clients to align with occupational therapy's commitment to diversity, equity, and inclusion (AOTA, 2020b). Telehealth research, practice, and policy should reflect diversity across person and environmental factors, including race, ethnicity, gender, age, socio-economic status, geography, and other demographics. Programs and research projects must collect and report such data to inform approaches that promote occupational justice. Factors that directly influence access include technology usability, digital literacy, health literacy, availability and usability of translators, scheduling when convenient for clients and caregivers, availability of specialists, and intervention approaches that use everyday materials. Occupational therapy practitioners have expertise in evaluating and resolving access barriers to support clients’ participation in services delivered through telehealth.
COSTS AND COST EFFECTIVENESS
A changing policy and payment landscape necessitate the demonstration of efficacy and value (both financial and non-financial) of occupational therapy services provided through telehealth. Components of cost and cost effectiveness associated with telehealth may include a decrease in cancelled appointments and “no shows,” and indirect cost savings for clients such as less time off work and elimination of travel to therapy appointments. In addition, occupational therapy practitioners working in settings that require travel to clients’ homes or between facilities (e.g., schools, nursing homes) also experience cost avoidance associated with decreased travel. Prevention of hospitalization/re-hospitalization, pressure ulcers, and other health-related complications are examples of cost-avoidance that may occur and factor into the value of occupational services provided through telehealth.
EXPERIENCES OF CLIENTS AND OCCUPATIONAL THERAPY PRACTITIONERS
Telehealth is a natural fit for occupational therapy interventions aimed at increasing participation in authentic contexts through the use of occupation. Telehealth creates opportunities for providing and measuring occupational therapy services in authentic contexts, and the inclusion of caregivers during telehealth sessions changes the overall experience for the client and the occupational therapy practitioner. Measuring client, caregiver/care partner, and provider satisfaction are all essential to understanding the overall experience of telehealth. Preferences for and acceptability of all components of telehealth, such as the videoconference platform and session frequency or intensity, should be considered. Assessing the client, caregiver, and practitioner experience early and at frequent intervals will facilitate adoption and long-term use.
DISCUSSION
The goal of occupational therapy is to facilitate participation in authentic contexts through the use of occupation. With a focus on participation and performance in everyday life, the profession of occupational therapy is well-positioned to serve as a leader in demonstrating the benefits of services delivered through telehealth. The occupational therapy profession must leverage expertise in participation, occupational performance, and authentic contexts to show the value of services delivered through telehealth regardless of population or setting.
The intention of the PACE Framework is to provide a menu of domains, outcomes, and associated outcome measures that are possible within the context of telehealth. The PACE Framework is not meant to serve as a checklist of requirements for telehealth-based interventions; instead, we offer areas for outcome measurement, subdomains, and measurement tools to consider during the design, implementation, adoption, and dissemination of occupational therapy services delivered through telehealth. The four domains of the framework function as a Venn or logic diagram in that each domain is definable, independent from the whole, but all domains are also related to the whole and overlap in numerous areas (Figure 1).
Figure 1.
Conceptual Model of the PACE Framework
The PACE Framework can be used to support researchers, practitioners, and policy-makers who are determining how to best capture the value of occupational therapy services delivered through telehealth. The PACE framework provides a set of telehealth measurement and evaluation domains that are priorities in occupational therapy research and practice. Researchers and occupational therapy practitioners can begin to collaborate across settings to collect data specific to outcomes and/or sub-domains that demonstrate the distinct value of services delivered through telehealth. To this end, how the framework is utilized by an end-user(s) will likely vary widely. Some may choose to focus their work on a single aspect of one component of one domain, while others may address all four domains in their design. Similarly, the PACE Framework is meant to be useful in both a prospective and retrospective manner. Prospectively, the PACE Framework is designed to help guide study or intervention design by facilitating discussion of all aspects of the occupational therapy telehealth implementation process. Retrospectively, the PACE Framework can be used to organize and analyze data from research and program evaluation. Using the PACE Framework, occupational therapy can continue to build evidence that can be shared with various stakeholders (e.g., clients, policy makers, administrators, payors, and other healthcare practitioners).
The PACE Framework shares similarities with other professions’ and organizations’ telehealth measurement frameworks (Bodenheimer & Sinsky, 2014; Chuo et al., 2020). Across practice settings and professions, frameworks outline the importance of client and provider experiences, and measure effectiveness, cost, and access. The PACE Framework, however, has three important differences that are relevant to occupational therapy delivered through telehealth. First, population health was included in the PACE Framework due to occupational therapy practitioners’ emergent role in health promotion and prevention (AOTA, 2020c). Systematic approaches to document process and outcome measures are needed for evidence-based occupational therapy programs delivered through telehealth to promote prevention, self-advocacy, and well-being for individuals and groups. Second, the PACE Framework explicitly included outcomes and example measures related to caregivers, or care partners. For many settings and populations, occupational therapy practitioners and researchers must establish partnerships with clients’ caregivers to facilitate successful access and utilization of telehealth. Instead of considering caregivers as secondary to the intervention process, the PACE Framework offers specific ways that caregivers may be recognized as essential participants in many occupational therapy interventions and measured as such.
Finally, Access for All Clients is considered a construct with multiple sub-domains; services must be purposefully designed and implemented to ensure access for all clients. The PACE Framework outlines sub-domains of access that must be considered, which include but are not limited to the consideration of authentic contexts, use of clients’ and families’ everyday items during telehealth sessions, and scheduling issues that have been shown to disproportionately impact clients from lower socio-economic status and minority backgrounds. Aligned with diversity, inclusion, and equity initiatives, the PACE Framework's Access for All Clients domain and associated sub-domains are meant to call attention to the explicit and implicit biases that create barriers to telehealth across individuals and groups. We invite researchers, practitioners, and policy makers to think broadly about access and ways to create opportunities for clients across settings and populations to use telehealth.
CONCLUSION
The COVID-19 pandemic necessitated a shift in service delivery to telehealth across practice settings and occupational therapy practitioners adapted in response. The PACE Framework provides a means for occupational therapy practitioners and researchers to continue to build the telehealth evidence base in occupational therapy. The changing practice, policy, and payment landscape necessitates researchers and occupational therapy practitioners support best practices and demonstrate the efficacy of occupational therapy services. The PACE Framework facilitates a systematic approach to evaluating components of occupational therapy service delivery through telehealth. It is vital that occupational therapy demonstrates a concerted effort in the measurement and evaluation of services delivered though telehealth to keep PACE with 21st century healthcare, meet the demands of payors moving towards value-based payments for services, and demonstrate the distinct value of occupational therapy services delivered through telehealth.
ACKNOWLEDGEMENTS
This paper was made possible by the efforts of the 2020 American Occupational Therapy Foundation Planning Grant Collective. Additionally, the authors sincerely thank the following expert reviewers of the PACE Framework (see Methods section): Susan Cahill, PhD, OTR/L, FAOTA; Evan E. Dean, PhD, OTR/L, FAAIDD; Winnie Dunn, PhD, OTR/L, FAOTA; Katie Jordan, OTD, OTR/L, FAOTA; Brenda Koverman, PhD, MBA, MS, OTR/L; and Grace Wilske, MS, OTR/L.
Footnotes
DECLARATION OF CONFLICTING INTERESTS: The authors declare no real or perceived conflicting interests with the presented work.
FUNDING: The Planning Grant Collective was sponsored by the American Occupational Therapy Foundation. KAP was supported by the National Institutes of Health [UL1TR002373, KL2TR002374].
REFERENCES
- American Occupational Therapy Association [AOTA]. (n.d.-a). AOTA unveils Vision 2025. https://www.aota.org/AboutAOTA/vision-2025.aspx
- American Occupational Therapy Association [AOTA]. (n.d.-b). Diversity, equity, and inclusion in occupational therapy. https://www.aota.org/About-Occupational-Therapy/diversity.aspx
- American Occupational Therapy Association [AOTA]. (n.d.-c). Safe at Home Checklist. https://www.aota.org/~/media/Corporate/Files/Practice/Aging/rebuilding-together/RT-Aging-in-Place-Safe-at-Home-Checklist.pdf
- American Occupational Therapy Association [AOTA]. (2005). Telerehabilitation position paper. American Journal of Occupational Therapy, 59, 656–660. 10.5014/ajot.59.6.656 [DOI] [PubMed] [Google Scholar]
- American Occupational Therapy Association [AOTA]. (2010). Telerehabilitation [Position Paper]. American Journal of Occupational Therapy, 64, S92–S102. 10.5014/ajot.2010.64S92 [DOI] [PubMed] [Google Scholar]
- American Occupational Therapy Association [AOTA]. (2013). Telehealth [Position Paper]. American Journal of Occupational Therapy, 67, S69–S90. 10.5014/ajot.2013.67S69 [DOI] [Google Scholar]
- American Occupational Therapy Association [AOTA]. (2018). Telehealth in occupational therapy [Position Paper]. American Journal of Occupational Therapy, 72(Suppl. 2), 7212410059. 10.5014/ajot.2018.72S219 [DOI] [Google Scholar]
- American Occupational Therapy Association [AOTA]. (2020a). AOTA's Guide to Acknowledging the Impact of Discrimination, Stigma, and Implicit Bias on Provision of Services. https://www.aota.org/-/media/Corporate/Files/Practice/Guide-Acknowledging-Impact-Discrimination-Stigma-Implicit-Bias.pdf
- American Occupational Therapy Association [AOTA]. (2020b). Occupational therapy's commitment to diversity, equity, and inclusion. American Journal of Occupational Therapy, 74(Suppl. 3), 7413410030. 10.5014/ajot.2020.74S3002 [DOI] [PubMed] [Google Scholar]
- American Occupational Therapy Association [AOTA]. (2020c). Occupational therapy in the promotion of health and well-being. American Journal of Occupational Therapy, 74, 7403420010. 10.5014/ajot.2020.743003 [DOI] [Google Scholar]
- American Occupational Therapy Association [AOTA]. (2020d). Occupational therapy practice framework: Domain and process (4th ed.). American Journal of Occupational Therapy, 74(Suppl. 2), 7412410010. 10.5014/ajot.2020.74S2001 [DOI] [Google Scholar]
- American Occupational Therapy Association [AOTA]. (2021, February 19). COVID-19 state updates: Summary of telehealth, insurance, and licensure developments; and comprehensive state-by-state chart. https://www.aota.org/Advocacy-Policy/State-Policy/StateNews/2020/COVID-19-Summary-Telehealth-Insurance-Licensure.aspx
- Barnes, C. R., & Adamson-Macedo, E. N. (2007). Perceived Maternal Parenting Self-efficacy (PMP S-E) tool: Development and validation with mothers of hospitalized preterm neonates. Journal of Advanced Nursing, 60(5) 550–560. 10.1111/j.1365-2648.2007.04445.x [DOI] [PubMed] [Google Scholar]
- Baron, K., Kielhofner, G., Iyenger, A., Goldhammer, V., & Wolenski, J. (2002). The Occupational Self Assessment: OSA: Version 2.0: a User's Manual. University of Illinois, College of Applied Health Sciences. [Google Scholar]
- Bedell, G. (2011). The Child and Adolescent Scale of Participation (CASP) © administration and scoring guidelines. http://sites.tufts.edu/garybedell/files/2012/07/CASP-Administration-Scoring-Guidelines-8-19-11.pdf
- Berwick, D. M., Nolan, T. W., & Whittington, J. (2008). The triple aim: Care, health, and cost. Health Affairs, 27(3), 759–769. 10.1377/hlthaff.27.3.759 [DOI] [PubMed] [Google Scholar]
- Bodenheimer, T., & Sinsky, C. (2014). From triple to quadruple aim: Care of the patient requires care of the provider. Annals of Family Medicine, 12(6), 573–576. 10.1370/afm.1713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boot, W. R., Charness, N., Czaja, S. J., Sharit, J., Rogers, W. A., Fisk, A. D., Mitzner, T., Lee, C. C., & Nair, S. (2015). Computer proficiency questionnaire: Assessing low and high computer proficient seniors. Gerontologist, 55(3), 404–411. 10.1093/geront/gnt117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuo, J., Macy, M. L., & Lorch, S. A. (2020). Strategies for evaluating telehealth. Pediatrics, 146(5), e20201781. 10.1542/peds.2020-1781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, S. R., Russell, L. B., Leis, A., Shahidi, J., Porterfield, P., Kuhl, D. R., Gadermann, A. M., & Sawatzky, R. (2019). More comprehensively measuring quality of life in life-threatening illness: The McGill Quality of Life Questionnaire - Expanded. BMC Palliat Care, 18(1), 92. 10.1186/s12904-019-0473-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coster, W. Deeney, T., Haltiwanger, J., & Haley, S. (1998). School Function Assessment Psychological Corporation/Therapy Skill Builders.
- Demerouti, E., Bakker, A. B., Nachreiner, F., & Schaufeli, W. B. (2001). The job demands-resources model of burnout. Journal of Applied Psychology, 86(3), 499–512. 10.1037/0021-9010.86.3.499 [DOI] [PubMed] [Google Scholar]
- Dumas, H. M., Fragala-Pinkham, M. A., Rosen, E. L., Lombard, K. A., & Farrell, C. (2015). Pediatric Evaluation of Disability Inventory Computer Adaptive Test (PEDI-CAT) and Alberta Infant Motor Scale (AIMS): Validity and responsiveness. Physical Therapy, 95(11), 1559–1568. 10.2522/ptj.20140339 [DOI] [PubMed] [Google Scholar]
- Dunn, W. (2014). Sensory Profile-2. https://www.pearsonassessments.com/store/usassessments/en/Store/Professional-Assessments/Motor-Sensory/Sensory-Profile-2/p/100000822.html
- Elo, S., & Kyngäs, H. (2008). The qualitative content analysis process. Journal of Advanced Nursing, 62(1), 107–115. 10.1111/j.1365-2648.2007.04569.x [DOI] [PubMed] [Google Scholar]
- Ford Foundation. (n.d.). Disability Inclusion Toolkit. https://www.fordfoundation.org/work/learning/research-reports/disability-inclusion-toolkit/
- Forsyth, K., Deshpande, S., Kielhofner, G., Henriksson, C., Haglund, L., Olson, L., Skinner, S., & Kulkarni, S. (2005). The Occupational Circumstances Assessment Interview and Rating Scale Version 4.0. https://www.moho.uic.edu/productDetails.aspx?aid=35
- Frost, J. S., Hammer, D. P., Nunez, L. M., Adams, J. L., Chesluk, B., Grus, C., Harvison, N., McGuinn, K., Mortensen, L., Nishimoto, J. H., Palatta, A., Richmond, M., Ross, E. J., Tegzes, J., Ruffin, A. L., & Bentley, J. P. (2019). The intersection of professionalism and interprofessional care: Development and initial testing of the interprofessional professionalism assessment (IPA). Journal of Interprofessional Care, 33(1), 102–115. 10.1080/13561820.2018.1515733 [DOI] [PubMed] [Google Scholar]
- Heinemann, A. W. (2010). Measurement of participation in rehabilitation research. Archives of Physical Medicine and Rehabilitation, 91(9), S1–S4. 10.1016/j.apmr.2009.08.155 [DOI] [PubMed] [Google Scholar]
- Hibbard, J. H., Stockard, J., Mahoney, E. R., & Tusler, M. (2004). Development of the Patient Activation Measure (PAM): Conceptualizing and measuring activation in patients and consumers. Health Services Research, 39(4p1), 1005–1026. 10.1111/j.1475-6773.2004.00269.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huebner, E. S. (1991). Initial development of the student's life satisfaction scale. School Psychology International, 12(3), 231–240. 10.1177/0143034391123010 [DOI] [Google Scholar]
- Hyland, M. E., & Sodergren, S. C. (1996). Development of a new type of global quality of life scale, and comparison of performance and preference for 12 global scales. Quality of Life Research, 5(5), 469–480. 10.1007/bf00540019 [DOI] [PubMed] [Google Scholar]
- Karnoe, A., Furstrand, D., Christensen, K. B., Norgaard, O., & Kayser, L. (2018). Assessing competencies needed to engage with digital health services: Development of the eHealth Literacy Assessment Toolkit. Journal of Medical Internet Research, 20(5), e178. 10.2196/jmir.8347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kayser, L., Karnoe, A., Furstrand, D., Batterham, R., Christensen, K. B., Elsworth, G., & Osborne, R. H. (2018). A multidimensional tool based on the eHealth literacy framework: Development and initial validity testing of the eHealth Literacy Questionnaire (eHLQ). Journal of Medical Internet Research, 20(2), e36. 10.2196/jmir.8371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kielhofner, G., Mallinson, T., Forsyth, K., & Lai, J.-S. (2001). Psychometric properties of the second version of the Occupational Performance History Interview (OPHI-II). American Journal of Occupational Therapy, 55(3), 260–267. 10.5014/ajot.55.3.260 [DOI] [PubMed] [Google Scholar]
- Kiresuk, T. J., & Sherman, R. E. (1968). Goal attainment scaling: A general method for evaluating comprehensive community mental health programs. Community Mental Health Journal, 4(6), 443–453. 10.1007/BF01530764 [DOI] [PubMed] [Google Scholar]
- Law, M., Baptiste, S., McColl, M., Opzoomer, A., Polatajko, H., & Pollock, N. (1990). The Canadian Occupational Performance Measure: An outcome measure for occupational therapy. Canadian Journal of Occupational Therapy, 57(2), 82–87. 10.1177/000841749005700207 [DOI] [PubMed] [Google Scholar]
- Law, M., King, G., Petrenchik, T., Kertoy, M., & Anaby, D. (2012). The assessment of preschool children's participation: Internal consistency and construct validity. Physical & Occupational Therapy in Pediatrics, 32(3), 272–287. 10.3109/01942638.2012.662584 [DOI] [PubMed] [Google Scholar]
- Little, L. M., Wallisch, A., Pope, E., & Dunn, W. (2018). Acceptability and cost comparison of a telehealth intervention for families of children with autism. Infants & Young Children, 31(4), 275–286. 10.1097/iyc.0000000000000126 [DOI] [Google Scholar]
- Maslach, C., & Jackson, S. E. (1981). The measurement of experienced burnout. Journal of Organizational Behavior, 2(2), 99–113. 10.1002/job.4030020205 [DOI] [Google Scholar]
- Matuska, K. (2012). Description and development of the Life Balance Inventory. Occupational Therapy Journal of Research, 32(1), 220–228. 10.3928/15394492-20110610-01 [DOI] [Google Scholar]
- Maujean, A., Davis, P., Kendall, E., Casey, L., & Loxton, N. (2014). The Daily Living Self-Efficacy Scale: A new measure for assessing self-efficacy in stroke survivors. Disability and Rehabilitation, 36(6), 504–511. 10.3109/09638288.2013.804592 [DOI] [PubMed] [Google Scholar]
- Nasreddine, Z. S., Phillips, N. A., Bédirian, V., Charbonneau, S., Whitehead, V., Collin, I., Cummings, J. L., & Chertkow, H. (2005). The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. Journal of the American Geriatrics Society, 53(4), 695–699. 10.1111/j.1532-5415.2005.53221.x [DOI] [PubMed] [Google Scholar]
- National Quality Forum. (2017). Creating a framework to support measure development for telehealth. https://www.qualityforum.org/Publications/2017/08/Creating_a_Framework_to_Support_Measure_Development_for_Telehealth.aspx
- Nissen, R. M., & Serwe, K. M. (2018). Occupational therapy telehealth applications for the dementia-caregiver dyad: A scoping review. Physical & Occupational Therapy in Geriatrics, 36(4), 366–379. 10.1080/02703181.2018.1536095 [DOI] [Google Scholar]
- Nobakht, Z., Rassafiani, M., Hosseini, S. A., & Ahmadi, M. (2017). Telehealth in occupational therapy: A scoping review. International Journal of Therapy and Rehabilitation, 24(12), 534–538. 10.12968/IJTR.2017.24.12.534 [DOI] [Google Scholar]
- Nonprofit Association of Oregon. (2018). Equity and Inclusion Lens Guide. https://nonprofitoregon.org/sites/default/files/NAO-Equity-Lens-Guide-2019.pdf
- Norman, C. D., & Skinner, H. A. (2006). eHEALS: The eHealth Literacy Scale. Journal of Medical Internet Research, 8(4), e27. 10.2196/jmir.8.4.e27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Northwestern University. (2021a). PROMIS® (Patient-Reported Outcomes Measurement Information System). https://www.healthmeasures.net/explore-measurement-systems/promis
- Northwestern University. (2021b). NIH Toolbox®. https://www.healthmeasures.net/explore-measurement-systems/nih-toolbox
- Ohan, J. L., Leung, D. W., & Johnston, C. (2000). The Parenting Sense of Competence Scale: Evidence of a stable factor structure and validity. Canadian Journal of Behavioural Science/Revue Canadienne des Sciences du Comportement, 32(4), 251–261. 10.1037/h0087122 [DOI] [Google Scholar]
- Orchard, C. A., King, G. A., Khalili, H., & Bezzina, M. B. (2012). Assessment of Interprofessional Team Collaboration Scale (AITCS): Development and testing of the instrument. Journal of Continuing Education in the Health Professions, 32(1), 58–67. 10.1002/chp.21123 [DOI] [PubMed] [Google Scholar]
- Parham, L. D., Ecker, C., Miller-Kuhaneck, H., Henry, D. A., & Glennon, T. J. (2007). SPM Sensory Processing Measure. Western Psychological Services. [Google Scholar]
- Proffitt, R., Cason, J., Little, L., & Pickett, K. A. (2021). Stimulating research to advance evidence-based applications of telehealth in occupational therapy. Occupational Therapy Journal of Research, 10.1177/15394492211011433. [DOI] [PMC free article] [PubMed]
- Radomski, M. V. (1995). There is more to life than putting on your pants. American Journal of Occupational Therapy, 49, 487–490. 10.5014/ajot.49.6.487 [DOI] [PubMed] [Google Scholar]
- Regenstein, M. (2007). Measuring and improving the quality of hospital language services: insights from the Speaking Together collaborative. Journal of General Internal Medicine, 22(2), 356–359. 10.1007/s11606-007-0358-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roque, N. A., & Boot, W. R. (2018). A new tool for assessing mobile device proficiency in older adults: The Mobile Device Proficiency Questionnaire. Journal of Applied Gerontology, 37(2), 131–156. 10.1177/0733464816642582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarzer, R., & Jerusalem, M. (1995). Generalized Self-Efficacy Scale. In Weinman J., Wright S., & Johnston M., Measures in health psychology: A user's portfolio. Causal and control beliefs (pp. 35–37). Windsor, UK: NFER-NELSON. [Google Scholar]
- Scott, J. P. (2019). Role Checklist Version 3: Participation and Satisfaction (RCv3). https://www.moho.uic.edu/productDetails.aspx?iid=6
- Stamm, B. (2009). Professional quality of life measure: Compassion, satisfaction, and fatigue version 5 (ProQOL). https://proqol.org/ProQol_Test.html
- Temkin-Greener, H., Gross, D., Kunitz, S. J., & Mukamel, D. (2004). Measuring interdisciplinary team performance in a long-term care setting. Medical Care, 42(5), 472–481. 10.1097/01.mlr.0000124306.28397.e2 [DOI] [PubMed] [Google Scholar]
- Tinetti, M. E., Richman, D., & Powell, L. (1990). Falls efficacy as a measure of fear of falling. Journal of Gerontology, 45(6), P239–243. 10.1093/geronj/45.6.p239 [DOI] [PubMed] [Google Scholar]
- Trockel, M., Bohman, B., Lesure, E., Hamidi, M. S., Welle, D., Roberts, L., & Shanafelt, T. (2018). A brief instrument to assess both burnout and professional fulfillment in physicians: Reliability and validity, including correlation with self-reported medical errors, in a sample of resident and practicing physicians. Academic Psychiatry, 42(1), 11–24. 10.1007/s40596-017-0849-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. (n.d.). Health People 2030: Leading health indicators. https://health.gov/healthypeople/objectives-and-data/leading-health-indicators
- van der Vaart, R., & Drossaert, C. (2017). Development of the Digital Health Literacy Instrument: Measuring a broad spectrum of health 1.0 and health 2.0 skills. Journal of Medical Internet Research, 19(1), e27. 10.2196/jmir.6709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varni, J. W., Seid, M., & Rode, C. A. (1999). The PedsQL: Measurement model for the pediatric quality of life inventory. Medical Care, 37(2), 126–139. 10.1097/00005650-199902000-00003 [DOI] [PubMed] [Google Scholar]
- Vismara, L. A., Young, G. S., & Rogers, S. J. (2012). Telehealth for expanding the reach of early autism training to parents. Autism Research and Treatment, 2012, 121878. 10.1155/2012/121878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washington Co. Family Caregiver Support Program. (n.d.). Washington Co. Family Caregiver Satisfaction Survey. https://www.oregon.gov/dhs/SENIORS-DISABILITIES/SUA/Documents/WA%20Co%20%20FCG%20Satisfaction%20Survey.pdf
- Wehmeyer, M. L. (1999). A functional model of self-determination: Describing development and implementing instruction. Focus on autism and other developmental disabilities, 14(1), 53–61. 10.1177/108835769901400107 [DOI] [Google Scholar]
- Wehmeyer, M. L., & Kelchner, K. (1995). The Arc's Self-Determination Scale (Adolescent Version). Arc of the United States.
- Wehmeier P. M., Fox, T., Doerr, J.M., Schnierer, N., Bender, M., Nater, U.M. (2019). Development and validation of a brief measure of self-management competence: The Self-Management Self-Test (SMST). Therapeutic Innovation & Regulatory Science, 2168479019849879. 10.1177/2168479019849879 [DOI] [PubMed]
- World Health Organization [WHO]. (1986). The 1st International Conference on Health Promotion, Ottawa 1986. https://www.who.int/teams/health-promotion/enhanced-wellbeing/first-global-conference
- World Health Organization [WHO] (1998). Well-being Measures in Primary Health Care/The Depcare Project. WHO Regional Office for Europe: Copenhagen. [Google Scholar]
- World Health Organization [WHO]. (2001). International classification of functioning, disability and health. Geneva: Author. [Google Scholar]
- World Health Organization [WHO]. (2004). The World Health Organization Quality of Life (WHOQOL) - BREF, 2012 revision. https://apps.who.int/iris/handle/10665/77773
- World Health Organization [WHO]. (2006). Constitution of the World Health Organization (45th ed.). https://www.who.int/governance/eb/who_constitution_en.pdf
- Zarit, S. H., Reever, K. E., & Bach-Peterson, J. (1980). Relatives of the impaired elderly: Correlates of feelings of burden. Gerontologist, 20(6), 649–655. 10.1093/geront/20.6.649 [DOI] [PubMed] [Google Scholar]