Abstract
Background
Normative data are necessary for validation of new outcome measures. Recently, the 95th centile of stride speed was qualified by the European Medicines Agency as a valid secondary outcome for clinical trials in subjects with Duchenne muscular dystrophy. This study aims to obtain normative data on spontaneous stride velocity and length in a non-controlled environment and their evolution after 12 months.
Method
Ninety-one healthy volunteers (50 females, 41 males), with a mean age of 16 years and 2 months, were recruited and assessed at baseline and 12 months later. The 4-stair climb, 6-min walk test, 10-m walk test and rise from floor assessments were performed. Stride length, stride velocity, and the distance walked per hour were studied in an everyday setting for one month after each evaluation.
Results
Of the 91 subjects assessed, 82 provided more than 50 h of recordings at baseline; and 73 subjects provided the same at the end of the year. We observed significant positive correlations of the stride length with age and height of participants, and a significant increase of the median stride length in children after the period. In this group, the 95th centile stride velocity was not correlated with age and was stable after one year. All measures but the 10MWT were stable in adults after a one-year period.
Conclusion
This study provides with data on the influence of age, height, and gender on stride velocity and length as well as accounting for natural changes after one year in controls.
Keywords: Accelerometer, Home monitoring, Healthy volunteers, Stride length, Stride velocity
Background
Duchenne muscular dystrophy (DMD) is a severe, rapidly progressive neuromuscular disorder characterized by muscle weakening. It has an estimated incidence of 1 in 5000 males [1]. DMD is caused by out-of-frame mutations in the dystrophin gene, which leads to an absence or deficiency of the protein dystrophin and the degeneration of muscles fibres [2]. Therefore, loss of ambulation occurs generally around the age of 12.
The 6-min walk distance test (6MWT) has been used as a primary outcome in most published pivotal phase 2 and 3 trials in ambulant patients with DMD [3–6]. Other outcomes used include the 4-stair climb (4SC) and functional scales such as the North Star Ambulatory Assessments (NSAA) in which participants are rated on their ability to perform standardized motor function tasks [3, 5–10]. In DMD, the low Standardized Response Mean of these different outcome measures, which illustrates the power of these measures to demonstrate a change over a certain period of time, meant that pivotal trials required over 100 patients per group and trial durations of 18 months and 2 years (NCT02851797 and NCT02500381, respectively). To accelerate clinical development and investigate in parallel several approaches without being limited by the number of patients available, it is crucial to validate more powerful outcome measures. This is the case for DMD and for numerous other rare diseases, within or outside the neuromuscular field.
The last decade has seen an increase in the availability of wearable technology for continuous monitoring of health and wellbeing [11]; for example, wearable devices that can be used to assess ambulation range from crude step counters to sophisticated multisensory systems [12]. Unlike consumer devices, medical devices must demonstrate validated measurement accuracy, sensitivity, and specificity [13]. Wearable devices have the potential to provide a complete view of a patient’s condition over a long time period by band-pass filtering day-to-day variation. Therefore, wearable devices provide a complementary approach with a major advantage over hospital-based assessments, which only provide ‘snapshots’ of a patient’s condition that can be affected by fatigue, illness, or lack of motivation.
In this context, Sysnav, a medium size private company, along with academic partners specifically developed a CE-marked class 1 wearable medical device, called Actimyo®, that records passively, in a precise and sensitive way, upper and lower limb movements in everyday life [14, 15]. From the capture of any single movement, several outcomes may be extracted. In ambulant patients, the identification and quantification of every individual stride allows for the calculation of the distribution of stride length and stride speed as well as for the analyses of different centiles such as the 95th centile stride velocity (SV95C). These variables are measured in a home-based environment over a 180-h period and are reliable and highly sensitive to changes in ambulant patients with DMD [16].
Recently, the EMA qualified SV95C as a valid secondary endpoint in clinical trials on ambulant patients with DMD [17]. Additional data are needed to qualify the measure as a primary endpoint [16]. Wearable technology is or has been used in clinical trials of therapies for spinal muscular atrophy [18, 19], facioscapulohumeral muscular dystrophy (NCT02579239, NCT04004000), limb girdle muscular dystrophy type 2E (NCT02579239), centronuclear myopathy (NCT02057705), and Angelman syndrome (NCT04259281).
To properly interpret the longitudinal evolution of the SV95C over time in patient populations, it is necessary to understand the longitudinal evolution in subjects without muscle conditions within the same age range, in particular between 5 and 18 years old, which is the age range mostly targeted in clinical trials of ambulant DMD patients and during which growth or maturational factors may significantly interfere with measures [20, 21]. Therefore, we conducted a longitudinal study in ambulant healthy subjects between 5 and 85 years of age to evaluate the changes in SV95C, as measured with the Actimyo® device, after a 12-months follow-up.
Method
Study design
We designed a monocentric academic study that was conducted in the Reference Centre for Neuromuscular Disease in Liège, Belgium between July 2017 and September 2019 with grant funding from Action Duchenne. The protocol was approved by the local ethics committee in Liège (N/Ref:1646). Before inclusion, all participants or parents or legal guardians provided written informed consent for participation and publication.
Participants
The initial protocols planned to include a maximum of 130 healthy subjects to gather a distribution of about 5–10 subjects par age year in children and a group of 30 adults. However, due to difficulties in recruiting controls—mainly in the adult age group—91 healthy subjects above the age of 5 years were assessed at baseline and 84 were assessed after 12 months. The exclusion criteria were occurrence of surgery or recent trauma in the upper or lower limbs within six months prior to the first visit; participating in sport at a high (national) level; pregnant or breastfeeding women; occurrence of muscular, neurological, infectious, acute, or chronic inflammatory disease within three weeks of inclusion date; and occurrence of orthopaedic, neuromuscular, or neurological disease with an impact on the quality of the walk.
Demographic data as well as medical and surgical histories were obtained during the baseline visit. A full physical examination, including weight, height, and vital signs, was performed at the first visit and at the 12-month visit. The subjects performed the 6MWT while wearing the sensors at baseline and at 12 months. They also performed the 4SC, rise from floor (RFF), and 10-m walk test (10MW). Assessment of dynamometric grip and pinch strength were evaluated with the Myogrio and Myopinch, as previously described [22]. All tests were conducted by trained and certified physiotherapists from the neuromuscular centre.
Timed tests
The subjects performed the 6MWT according to the modified ATS guidelines [23]. For RFF, trained examiners recorded using a stopwatch the time taken by the patient to complete the task of rising from supine to standing as fast as possible. For the 4SC, the subject had to climb a four-step flight of stairs as fast as possible. For the 10MW, the subject had to walk or run for ten meters in a straight line. We recorded the time taken to complete the task as fast as possible. In order to ascertain that the patient’s best performance is captured, each of these tests were performed three times with a 1-min rest between each trial and we kept the test performed at the highest speed.
Movement monitoring
The ActiMyo® device (Sysnav, Vernon, France) was worn for 1 month at baseline and at 12 months. The two sensors, each containing a magneto-inertial sensor that records the linear acceleration, the angular velocity and the magnetic field of the movement in all directions, were fixed to the dominant wrist and ankle. According to the EMA, for the purposes of qualification, a recording is considered as valid if it includes at least 50 h of recording; optimally it should include 180 h of recording [16]. We studied three different variables: stride length, stride velocity, and the number of meters walked per hour. Stride length and stride velocity were studied as the medians (SL50C and SV50C) or the 95th centiles (SL95C or SV95C).
Upper limb measurement is still a work in progress and will be presented elsewhere.
Statistical analysis
For analysis, data were excluded from subjects who recorded less than 50 h; 9 subjects at baseline and 18 subjects at follow-up, respectively. Analysis was first performed on the whole sample and then we analysed children (5 to 17 years) and adults (18 years and older) separately. Then within these groups, we analysed male and female subgroups. We used a series of Mann–Whitney U tests to compare subgroups. We then performed correlation analyses using Spearman’s rank correlation coefficient based on accelerometer measures, time test performances, age, and height. Finally, we use the Wilcoxon test to assess the evolution of each measure after 12 months. For compliance analysis, we used the 50-h and 180-h thresholds as these two thresholds were defined in the EMA qualification document as acceptable and optimal, respectively (16). All analyses were performed using IBM’s SPSS Statistics software. The limit of statistical significance was set to 0.05.
Results
Population
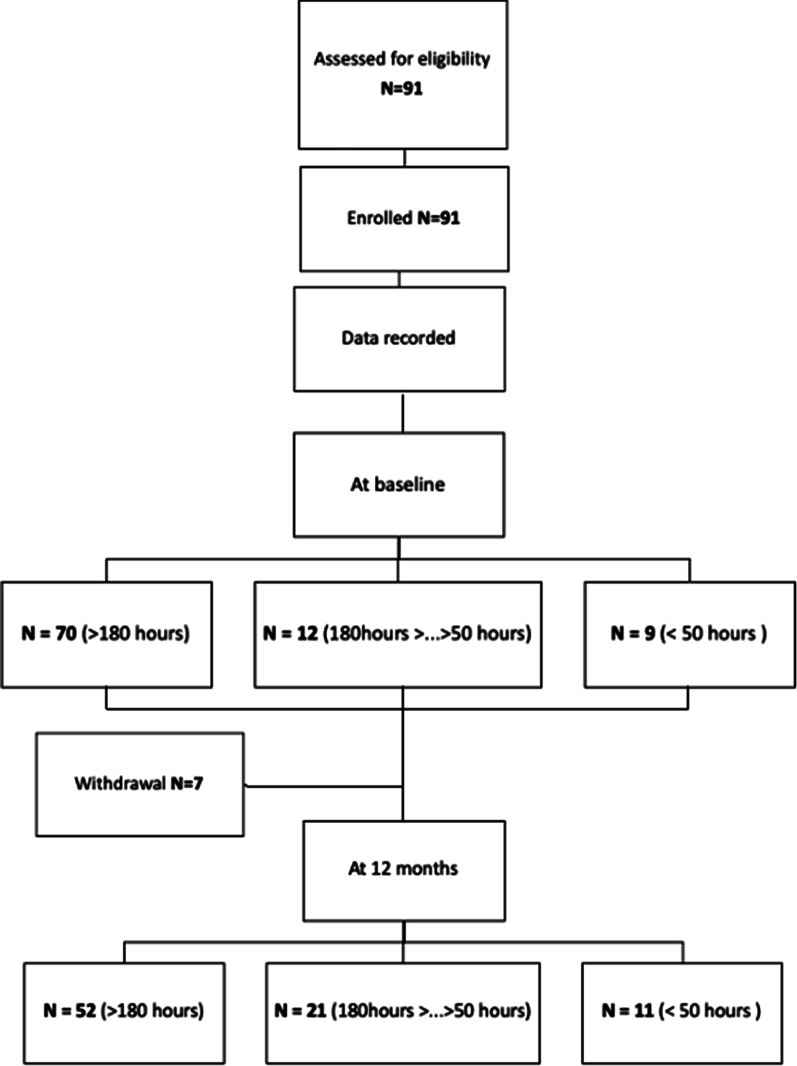
We included 91 healthy individuals (41 males (45.1%) and 50 females (54.9%) aged between 6 and 85 years, with a mean age of 16 years 2 months. Seven participants withdrew between the baseline and the follow-up visit for personal reasons. A flow chart of subject participation is shown in Fig. 1. The demographic and clinical characteristics of participants whose baseline data were analysed, as well as ActiMyo® variables, are provided in Table 1.
Fig. 1.
Flow-chart displaying the compliance and inclusion of subjects. Withdrawals resulted from loss of follow up (5 subjects) and withdrawal by the subject (2 subjects)
Table 1.
Demographic and clinical characteristics of participants who recorded more than 50 h
| Characteristics | ||||
|---|---|---|---|---|
| All | Adult | Children | ||
| All | Male | |||
| Sample size | 82 | 17 | 65 | 31 |
| Age (years) | 16.9 (16.0) | 43 (18.9) | 10.1 (2.8) | 10.6 (2.9) |
| [6.0–84.3] | [18.0–84.3] | [6.0–17.6] | [6.1–17.6] | |
| Sex: number of female (%) | 46 (56.0%) | 12 (70,6%) | 34 (52.3%) | 0 (0%) |
| Height (cm) | 144.0 (18.3) | 167.5 (10.6) | 137.8 (14.6) | 142.5 (15.1) |
| [114.0–195.0] | [153.2–195.0] | [114.0–173.3] | [118.0–174.3] | |
| BMI (kg/m2) | 18.8 (4.5) | 25.7 (3.6) | 17.0 (2.5) | 17.2 (2.4) |
| [13.2–32.8] | [20.1–32.8] | [13.2–26.1] | [13.9–23.7] | |
| 6MWT (m) | 594.7 (71.2) | 551.5 (82.0) | 606.0 (64.1) | 618.2 (61.6) |
| [436.0–761.0] | [436.0–716.0] | [464.0–761.0] | [496.0–761.0] | |
| 4SC (s) | 1.4 (0.3) | 1.6 (0.4) | 1.3 (0.3) | 1.3 (0.3) |
| [0.9–2.3] | [1.1–2.3] | [0.9–2.3] | [1–2.3] | |
| RFF (s) | 1.8 (0.6) | 2.7 (0.9) | 1.6 (0.2) | 1.57 (0.3) |
| [1.0–4.9] | [1.2–4.9] | [1.0–2.2] | [1.0–2.2] | |
| 10WT (m) | 4.8 (0.8) | 5.1 (0.8) | 4.7 (0.7) | 4.5 (3.5) |
| [3.1–7.3] | [4.1–7.3] | [3.1–7.2] | [3.5–5.7] | |
| Distance/hour (m/h) | 265.2 (87.2) | 246.4 (89.5) | 270.2 (86.5) | 294.8 (88.9) |
| [39.9–484.4] | [119.6–433.0] | [39.9–484.4] | [39.9–484.4] | |
| SV50C (m/s) | 1.0 (0.1) | 1.1 (0.1) | 1.0 (0.1) | 1.0 (0.1) |
| [0.7–1.3] | [0.7–1.3] | [0.9–1.3] | [0.9–1.3] | |
| SV95C (m/s) | 2.4 (0.6) | 1.6 (0.3) | 2.6 (0.4) | 2.6 (0.4) |
| [1.1–3.6] | [1.1–2.3] | [1.6–3.6] | [1.7–3.2] | |
| SL50C (m) | 1.1 (0.1) | 1.2 (0.1) | 1.0 (0.1) | 1.1 (0.1) |
| [0.8–1.5] | [0.8–1.5] | [0.8–1.4] | [0.8–1.4] | |
| SL95C (m) | 1.7 (0.2) | 1.5 (0.2) | 1.7 (0.2) | 1.7 (0.2) |
| [1.1–2.3] | [1.1–1.8] | [1.4–2.3] | [1.4–2.1] | |
Data are expressed in mean (SD) [Min–Max]. BMI body mass index, 6MWT 6-min walk distance, 4SC 4-stair climb; RFF rise from floor; 10MW 10-m walk test; SV50C 50th centile stride velocity; SV95C 95th centile stride velocity; SL50C 50th centile stride length; SL95C 95th centile stride length
Statistical analysis was performed on data from the 82 participants who achieved more than 50 h of recording at baseline. For further analysis, healthy subjects were distributed into two age subgroups: those 5 to 17 years of age and those aged 18 years and older. The first subgroup was composed of 65 participants, 34 of whom were females (52.3%). The second group was composed of 17 participants, of whom 12 were females (70.6%).
The two age groups differed from each other in most measures including height, 6MWD, 4SC, RFF, and stride characteristics (SV50C, SV95C, SL50C and SL95C). Younger subjects were shorter (p < 0.001) but had a higher 6MWD (p = 0.011) than adults. The younger group also performed better at 4SC (p = 0.001) and RFF (p < 0.001). The groups did not differ significantly in 10MW performance (p = 0.079). Regarding measurements obtained with the magneto-inertial device, the groups did not differ significantly in the distance walked per hour (p = 0.215). SV50C tended to be higher in the adult group (p = 0.047), whereas SV95C was higher in children (p = 0.001). We found a similar pattern in stride length measures: the median (SL50C) was higher in adults (p = 0.001) but the 95th centile (SL95C) was higher in children (p = 0.001). The ratio between the SV95C and the SV50C was three times higher in younger subjects than in adults, and the ratio between SL95C and SL50C was twice higher in younger subjects, which seems to indicate a more stereotyped walking patterns in adults.
Compliance in wearing the device
Among the 91 healthy controls who wore the wearable device for one month, 90% recorded more than 50 h, and 77% recorded more than 180 h at baseline. During the second period, 86% recorded more than 50 h, and 73% recorded more than 180 h. The main reason reported by subjects who recorded less than 50 h was ‘technical issues’. There was no age or gender effect evident on the recording duration (data not shown).
Correlations between timed tests, stride parameters and walking activity
Table 2 presents correlation coefficients between stride parameters obtained using the wearable device and clinical measures at baseline in both subgroups. We also present data from the 82 subjects who achieved more than 50 h of recording at baseline. 6MWD was significantly correlated with SV50C, SV95C, and SL95C in the younger group. In the adult group, 6MWD was only correlated with ‘maximum performance’ measures SV95C and SL95C. In the younger population, the impact of age and height was more obvious than in the adult population (Table 2). Among the group aged 5 to 17 years, height was highly correlated with age, 6MWD, 10MW, SV50C, SL50C, and weakly correlated with SV95C and SL95C. In adults, height was only correlated with stride length measures SL50C and SL95C. We found no correlation between recording duration and stride length, stride velocity, or walking activity (distance/h, p = 0.323; SV50C, p = 0.466; SV95C, p = 0.664; SL50C, p = 0.723 and SL95C, p = 0.798).
Table 2.
Correlation between accelerometer measures and clinical measures (Spearmen coefficient)
| Age | Height | BMI | 6MWT | 4SC | RRF | 10MW | Distance | SV50C | SV95C | SL50C | SL95C | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | 5–17 y | 0.927** | 0.667** | 0.122 | 0.184 | 0.418** | − 0.143 | − 0.083* | 0.513** | − 0.609** | 0.829** | − 0.099* | |
| ≥ 18 y | |||||||||||||
| Height | 5–17 y | 0.909** | 0.620** | 0.157 | 0.137 | 0.389** | − 0.149 | − 0.135 | 0.499** | − 0.598** | 0.883** | − 0.037 | |
| ≥ 18 y | − 0.134 | ||||||||||||
| BMI | 5–17 y | 0.363** | 0.356** | − 0.204 | 0.057 | 0.390** | 0.065 | − 0.091 | 0.321** | − 0.575** | 0.510** | − 0.363** | |
| ≥ 18 y | 0.627** | 0.189 | |||||||||||
| 6MWD | 5–17 y | 0.6** | 0.538** | − 0.015 | − 0.135 | − 0.334** | − 0.565** | 0.101 | 0.336** | 0.271* | 0.212 | 0.465** | |
| ≥ 18 y | − 0.703** | 0.061 | − 0.559* | ||||||||||
| 4SC | 5–17 y | − 0.142 | − 0.163 | − 0.303* | − 0.033 | 0.607** | 0.256* | − 0.285** | − 0.077 | − 0.3** | 0.057 | − 0.224* | |
| ≥ 18 y | 0.14 | − 0.288 | 0.181 | 0.054 | |||||||||
| RFF | 5–17 y | − 0.011 | 0.028 | − 0.008 | − 0.183 | 0.515** | 0.181 | − 0.298** | − 0.01 | − 0.631** | 0.289** | − 0.494** | |
| ≥ 18 y | 0.447 | 0.01 | 0.432 | − 0.409 | 0.63** | ||||||||
| 10MW | 5–17 y | − 0.479** | − 0.407** | − 0.113 | − 0.595** | 0.155 | 0.089 | − 0.362** | − 0.377** | − 0.203 | − 0.276* | − 0.328** | |
| ≥ 18 y | 0.434 | − 0.326 | 0.225 | − 0.373 | 0.415 | 0.362 | |||||||
| Distance | 5–17 y | 0.03 | − 0.036 | 0.013 | 0.11 | − 0.232 | − 0.263* | − 0.426** | 0.455** | 0.389** | 0.081 | 0.289** | |
| ≥ 18 y | 0.115 | 0.108 | 0.174 | − 0.078 | − 0.43 | − 0.241 | − 0.201 | ||||||
| SV50C | 5–17 y | 0.621** | 0.552** | 0.292* | 0.454** | − 0.219 | − 0.222 | − 0.477** | 0.451** | − 0.053 | 0.74** | 0.293** | |
| ≥ 18 y | − 0.206 | 0.116 | − 0.113 | 0.444 | − 0.087 | − 0.018 | − 0.331 | 0.691** | |||||
| SV95C | 5–17 y | − 0.231 | − 0.269* | − 0.207 | 0.034 | − 0.117 | − 0.418** | − 0.09 | 0.437** | 0.114 | − 0.414** | 0.734** | |
| ≥ 18 y | − 0.738* | 0.254 | − 0.397 | 0.858** | 0.05 | − 0.385 | − 0.306 | 0.157 | 0.542* | ||||
| SL50C | 5–17 y | 0.869** | 0.876** | 0.285 | 0.518** | − 0.163 | − 0.1 | − 0.493** | 0.148 | 0.786** | − 0.098 | 0.16 | |
| ≥ 18 y | − 0.091 | 0.678** | − 0.145 | 0.103 | − 0.27 | 0 | − 0.331 | 0.659** | 0.684** | 0.417 | |||
| SL95C | 5–17 y | 0.312* | 0.274* | − 0.142 | 0.374** | − 0.144 | − 0.405** | − 0.298* | 0.281* | 0.418** | 0.728** | 0.455** | |
| ≥ 18 y | − 0.561* | 0.668** | − 0.093 | 0.485* | − 0.187 | − 0.256 | − 0.319 | 0.252 | 0.449 | 0.748** | 0.721** |
Significance level p ≤ 0.01**, p ≤ 0.05*. Upper part: correlation on the whole sample. Lower part: correlation on the two age groups. BMI body mass index, 6MWT 6-min walk distance, 4SC 4-stair climb; RFF rise from floor; 10MW 10-m walk test; SV50C 50th centile stride velocity; SV95C 95th centile stride velocity; SL50C 50th centile stride length; SL95C 95th centile stride length
Gender effect
In the adult population, males showed statistically significantly higher SL50C (p = 0.009) and SL95C (p = 0.001), probably because they are on average taller than women in the cohort (p = 0.048). There was no other difference between males and females in the adult group. In contrast, in the younger population, male subjects were taller than female subjects, but we did not detect significant differences in any qualitative real-life walking parameter between the two subgroups.
Longitudinal data
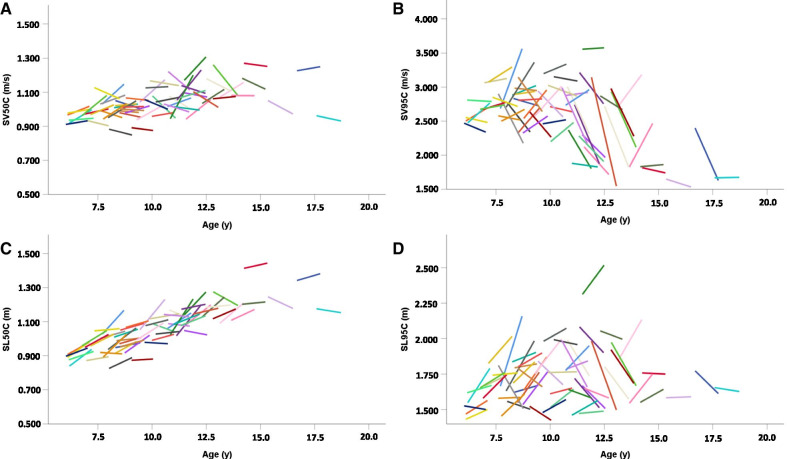
Changes after 12 months are presented in Table 3 and evolution of the measures obtained with the magneto-inertial device in children are displayed in Fig. 2. We present data on the 73 subjects who achieved more than 50 h of recording both at baseline and on follow-up visits. Given the effects of growth, we investigated two subgroups separately. In the younger group, we observed a significant increase in functional measures (6MWD, 4SC, 10MW) after one year. Of the measures obtained with the magneto-inertial device, only SL50C increased after one year. We did not observe a significant change after a year in adults in stride length, stride velocity, distance walked, 6MWD, or RFF with the exception of a slight improvement in the 10MW performance.
Table 3.
Evolution of measures after one year
| Subgroup | 5–17 years old | Over 18 years old | ||
|---|---|---|---|---|
| Characteristics | Mean (SD) | Sig | Mean (SD) | Sig |
| Δ6MWD (m) | 33.6 (50.302) | p = 0.000** | 14.87 (46.649) | p = 0.191 |
| Δ4SC (s) | − 0.11 (0.288) | p = 0.004** | − 0.02 (0.463) | p = 0.875 |
| ΔRFF (s) | − 0.07 (0.336) | p = 0.293 | − 0.24 (0.736) | p = 0.239 |
| Δ10MW (s) | − 0.76 (0.77) | p = 0.000** | − 0.52 (0.632) | p = 0.011* |
| ΔDistance (m/h) | − 17.23 (76.17) | p = 0.059 | 9.38 (67.15) | p = 0.609 |
| ΔSV50C (m/s) | 0.01 (0.078) | p = 0.359 | 0.01 (0.154) | p = 0.691 |
| ΔSV95C (m/s) | − 0.12 (0.447) | p = 0.112 | 0.12 (0.389) | p = 0.955 |
| ΔSL50C (m) | 0.05 (0.06) | p = 0.000** | 0.01 (0.095) | p = 0.427 |
| ΔSL95C (m) | 0,02 (0.184) | p = 0.241 | 0,04 (0.133) | p = 0.691 |
Time effect was assessed by a rank Wilcoxon test for single sample (null hypothesis: median = 0). Significance level p ≤ 0.01**, p ≤ 0.05*. 6MWT: 6-min walk distance, 4SC: 4-stair climb; RFF: rise from floor; 10MW: 10-m walk test; SV50C: 50th centile stride velocity; SV95C: 95th centile stride velocity; SL50C: 50th centile stride length; SL95C: 95th centile stride length
Fig. 2.
One year evolution of SV50C (A), SV95C (B), SL50C (C) and SL95C (D) in subjects aged 5 to 17 years. SV50C 50th centile stride velocity; SV95C 95th centile stride velocity; SL50C 50th centile stride length; SL95C 95th centile stride length
Discussion
As a result of this study, we provide normative data for spontaneous stride velocity, stride length and walking distance per hour obtained passively with a wearable device during a one-month recording period in a non-controlled setting and the one-year evolution thereafter. Most previous studies using wearable devices provide us with quantitative parameters [24]. Qualitative gait analysis as stride length and velocity were mostly obtained based on evaluations inside clinical facilities [25, 26]. Recently, several efforts were made to collect, in a home-based setting, qualitative data from subjects with various diseases and control populations [18, 19, 22, 27]. However, to the best of our knowledge, we found no other published data regarding normative longitudinal evaluations of spontaneous stride velocity, stride length, and walking activity in an everyday setting.
As suggested in previous findings [28], acquiring normative data was feasible. The overall compliance with device use was good. More than 90% of subjects wore the device more than the minimum requirement of 50 h, which indicates that wearing devices at the ankle and at the wrist for one month was acceptable for most participants. The main reason given for data collection below the 50-h threshold was ‘technical issues’, and compliance was not influenced by gender or age. In addition, the recording duration did not influence the variables that were studied.
As expected, results of timed tests were growth dependent [22]. We also observed the influence of height (in adults) and height and growth (in children) on stride length. These results support previous findings [29, 30]. Height did not influence SV95C, for which only a very weak inverse correlation was found with height in the adult subgroup only. In children, all correlations between age, height and stride length or speed were much weaker with maximum performance as measured by the 95th centile than with median values. Independence of growth is an advantage in clinical trials that are conducted in children over 1 or 2 years, especially in DMD where growth is altered by steroid use.
In comparison to ambulant DMD patients of the same age, healthy children present a 67.3% higher SV95C [17]. The difference for other variables was not as extreme, and there is some overlap between DMD and control participants (SL50C 31.39%, SL95C 52.41%, SV50C 25.72%, distance walked/hour 63.13%) [16]. SV95C was stable after one year in controls but significantly and constantly decreases in subjects with DMD. In DMD patients, there is a significant correlation between SV95C and all timed tests [17]. We did not find such correlations in controls, which is probably related to the fact that weakness constitutes a common limiting factor on 6MWD and SV95C in patients with DMD, strengthening the correlation in this group.
Gathering normative data is crucial in the validation process of an outcome measure, as it allows identification of potentially confounding variables such as age, height, or gender. For a specific outcome, the normative data can either show a strong ceiling effect, as is the case for most of normative scales such as CHOP Intend, NSAA, and Motor Function Measure [31–34], or increases with age, as is the case for strength [21, 35] and the 6MWD [20].
The limitations of this study reside in the small number of controls per subgroup (age and gender), principally related to the limited availability of recording devices. Given the number of subjects, we did not study the seasonal influence on the parameters. It is likely that a seasonal analysis would need to take weather conditions into account, as they are more likely to influence walking behaviour than does the time of year, and would require continuous recording over one year, which could be burdensome in controls. Another limitation is that the BMI evolution of participants tends toward a more gradual increase than those of age-matched DMD, mainly after 8 years of age [36]. However, this is not a major issue since there is no correlation between BMI and SV95C in both the adult and children subgroups. During the study, participants wore devices on both wrist and ankle. The analysis of upper limb movement in control patients is complex, since there is an interference with movement produced during the ambulation. The results will therefore be presented elsewhere, with comparison to the upper limb measures in ambulant and non-ambulant DMD patients.
Conclusion
This study provides evidence that normative data regarding stride length and velocity in a home-based environment with wearable sensors is feasible. These normative data will allow us to express a patient’s data as a percentage of predicted value for age or height and to identify those variables that have important confounding factors. There is still a large amount of work to be done to enable analysis of ambulation and upper limb function in various diseases using medical device for real-life mobility measurement. Future research should focus on exploring new fields of neurological disease and the creation of algorithms to study upper limb function, falls, or ataxia.
Acknowledgements
We would like to thank all of the participants, including parents and guardians, for the time they have provided to this study. We would also like to thank the team at the Citadelle Regional Hospital Centre in Liège, as well as Sysnav in Vernon. We are extremely grateful to the Foundation for Action Duchenne for financial support. The authors are thankful to Dominic Tromans for English correction
Abbreviations
- 4SC
4-Stair climb
- 6MWT
6-Minute walk test
- 6MWD
6-Minute walk distance
- 10MW
10-Meter walk test
- BMI
Body mass index
- DMD
Duchenne muscular dystrophy
- EMA
European Medicines Agency
- NSAA
North Star Ambulatory Assessments
- RFF
Rise from floor
- SV95C
95Th centile stride velocity
- SV50C
50Th centile stride velocity
- SL95C
95Th centile stride length
- SL50C
50Th centile stride length
Authors' contributions
MP: helped with data analysis and writing the article. AU: experimenter, data collection, data analysis, and writing the article. AD: helped with patient selection, clinical supervision, and data collection. OS, FD, MD: data collection. MA, DE, DV: technical support, data analysis. AD: helped with patient selection, clinical supervision, and data collection. LS: clinical supervision, protocol preparation, and article writing. All authors read and approved the final manuscript.
Funding
This work was supported by a grant from Action Duchenne.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study was approved by the ethics committees of the Citadelle Regional Hospital Centre in Liège (Belgian N°: B412201731844), and the experiment was conducted in accordance with the good clinical practice and with the Declaration of Helsinki (2013). Prior to their inclusion in the study, all participants (and/or their legal guardians) gave their full written informed consent.
Consent for publication
Not applicable.
Competing interests
Academic authors declare no competing interests. Melanie Annoussamy and Damien Eggenspieler are employed by Synsav, the medium-sized enterprise responsible for ActiMyo® development. David Vissière is the CEO, founder and main shareholder of Sysnav.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ryder S, Leadley RM, Armstrong N, Westwood M, de Kock S, Butt T, et al. The burden, epidemiology, costs and treatment for Duchenne muscular dystrophy: an evidence review. Orphanet J Rare Dis. 2017;12(1):79. doi: 10.1186/s13023-017-0631-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mah JK, Korngut L, Dykeman J, Day L, Pringsheim T, Jette N. A systematic review and meta-analysis on the epidemiology of Duchenne and Becker muscular dystrophy. Neuromuscul Disord. 2014;24(6):482–491. doi: 10.1016/j.nmd.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 3.Clemens PR, Rao VK, Connolly AM, Harper AD, Mah JK, Smith EC, et al. Safety, tolerability, and efficacy of viltolarsen in boys with duchenne muscular dystrophy amenable to exon 53 skipping: a phase 2 randomized clinical trial. JAMA Neurol. 2020;77(8):982–991. doi: 10.1001/jamaneurol.2020.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Frank DE, Schnell FJ, Akana C, El-Husayni SH, Desjardins CA, Morgan J, et al. Increased dystrophin production with golodirsen in patients with Duchenne muscular dystrophy. Neurology. 2020;94(21):e2270–e2282. doi: 10.1212/wnl.0000000000009233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McDonald CM, Campbell C, Torricelli RE, Finkel RS, Flanigan KM, Goemans N, et al. Ataluren in patients with nonsense mutation Duchenne muscular dystrophy (ACT DMD): a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;390(10101):1489–1498. doi: 10.1016/s0140-6736(17)31611-2. [DOI] [PubMed] [Google Scholar]
- 6.Mendell JR, Rodino-Klapac LR, Sahenk Z, Roush K, Bird L, Lowes LP, et al. Eteplirsen for the treatment of Duchenne muscular dystrophy. Ann Neurol. 2013;74(5):637–647. doi: 10.1002/ana.23982. [DOI] [PubMed] [Google Scholar]
- 7.Bushby K, Finkel R, Wong B, Barohn R, Campbell C, Comi GP, et al. Ataluren treatment of patients with nonsense mutation dystrophinopathy. Muscle Nerve. 2014;50(4):477–487. doi: 10.1002/mus.24332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goemans N, Mercuri E, Belousova E, Komaki H, Dubrovsky A, McDonald CM, et al. A randomized placebo-controlled phase 3 trial of an antisense oligonucleotide, drisapersen Duchenne muscular dystrophy. Neuromuscul Disord. 2018;28(1):4–15. doi: 10.1016/j.nmd.2017.10.004. [DOI] [PubMed] [Google Scholar]
- 9.Voit T, Topaloglu H, Straub V, Muntoni F, Deconinck N, Campion G, et al. Safety and efficacy of drisapersen for the treatment of Duchenne muscular dystrophy (DEMAND II): an exploratory, randomised, placebo-controlled phase 2 study. Lancet Neurol. 2014;13(10):987–996. doi: 10.1016/s1474-4422(14)70195-4. [DOI] [PubMed] [Google Scholar]
- 10.Assessment report for Kyndrisa. European Medicines Agency. https://www.ema.europa.eu/en/documents/withdrawal-report/withdrawal-assessment-report-kyndrisa_en.pdf. Accessed 1 Dec 2020.
- 11.Piwek L, Ellis DA, Andrews S, Joinson A. The Rise of Consumer Health Wearables: Promises and Barriers. PLoS Med. 2016;13(2):e1001953. doi: 10.1371/journal.pmed.1001953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dobkin BH. Wearable motion sensors to continuously measure real-world physical activities. Curr Opin Neurol. 2013;26(6):602–608. doi: 10.1097/wco.0000000000000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Caulfield B, Reginatto B, Slevin P. Not all sensors are created equal: a framework for evaluating human performance measurement technologies. NPJ Digit Med. 2019;2:7. doi: 10.1038/s41746-019-0082-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Le Moing AG, Seferian AM, Moraux A, Annoussamy M, Dorveaux E, Gasnier E, et al. A movement monitor based on magneto-inertial sensors for non-ambulant patients with duchenne muscular dystrophy: a pilot study in controlled environment. PLoS ONE. 2016;11(6):e0156696. doi: 10.1371/journal.pone.0156696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lilien C, Gasnier E, Gidaro T, Seferian A, Grelet M, Vissière D, et al. Home-based monitor for gait and activity analysis. J Vis Exp. 2019 doi: 10.3791/59668. [DOI] [PubMed] [Google Scholar]
- 16.Qualification opinion on stride velocity 95th centile as a secondary endpoint in Duchenne muscular dystrophy measured by a valid and suitable wearable device*European Medicines Agency. https://www.ema.europa.eu/en/documents/scientific-guideline/qualification-opinion-stride-velocity-95th-centile-secondary-endpoint-duchenne-muscular-dystrophy_en.pdf. Accessed 15 July 2021.
- 17.Haberkamp M, Moseley J, Athanasiou D, de Andres-Trelles F, Elferink A, Rosa MM, et al. European regulators' views on a wearable-derived performance measurement of ambulation for Duchenne muscular dystrophy regulatory trials. Neuromuscul Disord. 2019;29(7):514–516. doi: 10.1016/j.nmd.2019.06.003. [DOI] [PubMed] [Google Scholar]
- 18.Chabanon A, Seferian AM, Daron A, Péréon Y, Cances C, Vuillerot C, et al. Prospective and longitudinal natural history study of patients with Type 2 and 3 spinal muscular atrophy: baseline data NatHis-SMA study. PLoS ONE. 2018;13(7):e0201004. doi: 10.1371/journal.pone.0201004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Annoussamy M, Seferian AM, Daron A, Péréon Y, Cances C, Vuillerot C, et al. Natural history of Type 2 and 3 spinal muscular atrophy: 2-year NatHis-SMA study. Ann Clin Transl Neurol. 2020 doi: 10.1002/acn3.51281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goemans N, Klingels K, van den Hauwe M, Boons S, Verstraete L, Peeters C, et al. Six-minute walk test: reference values and prediction equation in healthy boys aged 5 to 12 years. PLoS ONE. 2013;8(12):e84120. doi: 10.1371/journal.pone.0084120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hogrel JY, Decostre V, Ledoux I, de Antonio M, Niks EH, de Groot I, et al. Normalized grip strength is a sensitive outcome measure through all stages of Duchenne muscular dystrophy. J Neurol. 2020;267(7):2022–2028. doi: 10.1007/s00415-020-09800-9. [DOI] [PubMed] [Google Scholar]
- 22.Seferian AM, Moraux A, Canal A, Decostre V, Diebate O, Le Moing AG, et al. Upper limb evaluation and one-year follow up of non-ambulant patients with spinal muscular atrophy: an observational multicenter trial. PLoS ONE. 2015;10(4):e0121799. doi: 10.1371/journal.pone.0121799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McDonald CM, Henricson EK, Han JJ, Abresch RT, Nicorici A, Elfring GL, et al. The 6-minute walk test as a new outcome measure in Duchenne muscular dystrophy. Muscle Nerve. 2010;41(4):500–510. doi: 10.1002/mus.21544. [DOI] [PubMed] [Google Scholar]
- 24.Perry B, Herrington W, Goldsack JC, Grandinetti CA, Vasisht KP, Landray MJ, et al. Use of mobile devices to measure outcomes in clinical research, 2010–2016: a systematic literature review. Digit Biomark. 2018;2(1):11–30. doi: 10.1159/000486347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fang X, Liu C, Jiang Z. Reference values of gait using APDM movement monitoring inertial sensor system. R Soc Open Sci. 2018;5(1):170818. doi: 10.1098/rsos.170818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Voss S, Joyce J, Biskis A, Parulekar M, Armijo N, Zampieri C, et al. Normative database of spatiotemporal gait parameters using inertial sensors in typically developing children and young adults. Gait Posture. 2020;80:206–213. doi: 10.1016/j.gaitpost.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shah VV, McNames J, Mancini M, Carlson-Kuhta P, Spain RI, Nutt JG, et al. Quantity and quality of gait and turning in people with multiple sclerosis, Parkinson's disease and matched controls during daily living. J Neurol. 2020;267(4):1188–1196. doi: 10.1007/s00415-020-09696-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wiedmann I, Grassi M, Duran I, Lavrador R, Alberg E, Daumer M, et al. Accelerometric Gait analysis devices in children-will they accept them? results from the AVAPed study. Front Pediatr. 2020;8:574443. doi: 10.3389/fped.2020.574443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dusing SC, Thorpe DE. A normative sample of temporal and spatial gait parameters in children using the GAITRite electronic walkway. Gait Posture. 2007;25(1):135–139. doi: 10.1016/j.gaitpost.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 30.Pierrynowski MR, Galea V. Enhancing the ability of gait analyses to differentiate between groups: scaling gait data to body size. Gait Posture. 2001;13(3):193–201. doi: 10.1016/s0966-6362(01)00097-2. [DOI] [PubMed] [Google Scholar]
- 31.Clinical Review Report: Nusinersen (Spinraza): (Biogen Canada Inc.): Indication: Treatment of patients with 5q SMA [Internet]. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; 2018 Jan. https://www.ncbi.nlm.nih.gov/books/NBK533989/. Accessed 14 July 2021. [PubMed]
- 32.de Lattre C, Payan C, Vuillerot C, Rippert P, de Castro D, Bérard C, et al. Motor function measure: validation of a short form for young children with neuromuscular diseases. Arch Phys Med Rehabil. 2013;94(11):2218–2226. doi: 10.1016/j.apmr.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 33.Klingels K, Van Verdegem L, van den Hauwe M, Buyse G, Goemans N, et al. Reference values for the three-minute walk test, North Star ambulatory assessment and timed tests in typically developing boys aged 2.5–5 years. Neuromuscul Disord. 2015;25:S228. doi: 10.1016/j.nmd.2015.06.159. [DOI] [Google Scholar]
- 34.Kolb SJ, Coffey CS, Yankey JW, Krosschell K, Arnold WD, Rutkove SB, et al. Baseline results of the NeuroNEXT spinal muscular atrophy infant biomarker study. Ann Clin Transl Neurol. 2016;3(2):132–145. doi: 10.1002/acn3.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Servais L, Deconinck N, Moraux A, Benali M, Canal A, Van Parys F, et al. Innovative methods to assess upper limb strength and function in non-ambulant Duchenne patients. Neuromuscul Disord. 2013;23(2):139–148. doi: 10.1016/j.nmd.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 36.Lamb MM, West NA, Ouyang L, Yang M, Weitzenkamp D, James K, et al. Corticosteroid treatment and growth patterns in ambulatory males with Duchenne muscular dystrophy. J Pediatr. 2016;173:207–13.e3. doi: 10.1016/j.jpeds.2016.02.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.