Abstract
Objectives
This study aimed to compare the isokinetic peak torque and, secondarily, other parameters of the rotator cuff in the shoulders of paraplegic wheelchair basketball athletes and non-athletes controls.
Design
Cross-sectional study.
Methods
Thirty-six complete spinal cord injured individuals aged between 18 and 45 years performed an isokinetic evaluation of peak torque, power, and work exerted by the rotator cuff muscle group, in a Biodex System. All Concentric isokinetic tests were performed in the seated position with the shoulder at a 45° abduction from the scapular plane and flexed at 30° to the frontal plane. Subjects completed five repetitions at 60°/s and 180°/s, and ten repetitions at 300°/s, bilaterally, with an interval of one minute between each series. Statistical analysis (t-test, P < 0.05) compared athletes and non-athletes, dominant and non-dominant upper limbs according to all isokinetic parameters and angular velocities.
Results
Peak torque/weight, work, and muscle power of wheelchair basketball athletes were significantly greater than those of the control group (P < 0.05), but there were no statistical differences between dominant and non-dominant upper limb. Internal rotators were stronger than the external rotators both for athletes and for non-athletes. There is a positive correlation between peak torque and time since injury.
Conclusions
Wheelchair basketball athletes showed greater peak torque and other muscle performance parameters, which suggest that wheelchair basketball influences the shoulder musculature of those with traumatic spinal cord injury.
Keywords: Isokinetic evaluation, Shoulder, strength, Spinal cord injury
Introduction
Wheelchair basketball (WB) progressively grows in the sports environment with the participation of open and elite athletes. WB improves physical and cardio-pulmonary fitness, while it promotes social integration and improved self-confidence in people with disabilities. Basketball in wheelchairs consists of activities that require explosive strength and speed.1–4 Typically WB overloads the upper limbs, during locomotion on the court and movements such as passing, rebounding, dribbling, and shooting.5 Overload to the upper limbs may lead to the development of injuries like tendinopathies in WB players.4
Regular practice in WB is associated with a high rate of shoulder injury, due to a muscle imbalance,6,7 which is also observed when the wheelchair athletes are compared to sedentary individuals.8–10 The study by Burnham et al.9 investigated the role of imbalance in shoulder strength as a factor in the development of rotator cuff problems. The evaluation of the peak torque of abductors and adductors, and internal and external rotators of 19 paraplegic athletes and 20 healthy male individuals indicated that the weakness of rotators and adductors is associated with the rotator cuff impact syndrome in wheelchair athletes, but, as a cross-over study, it does not clarify the causal relationship. Magnetic resonance imaging in 296 individuals with spinal cord injury evidenced torn rotator cuffs in as much as 75.7% of the individuals in the overhead sports group (at least 1–2 times per week) and 36.3% in the non-sports group.8
Fullerton and colleagues11 directly reported wheelchair athletes to be less likely to have shoulder pain than non-athletes. Also, those who participate in wheelchair sports players enjoyed more years without shoulder pain since injury than non-athletes. Thus, the study suggests that athletic activity has a protective effect on shoulder pain. Mulroy12 showed that individuals who had decreased muscle strength and lower levels of physical activity before the onset of shoulder pain were more likely to develop it. Finally, Finley and Rodgers13 have shown that wheelchair sports alone did not affect the risk of developing shoulder pain. Therefore, results are conflicting regarding influence of sport and physical activity. Regardless of the reference to pain and the possible pathologies due to the muscular overload of the wheelchair, it is necessary to consider the peak torque in these individuals without any lesions in the shoulder, once muscle balance is mandatory for the movement of this joint and is associated with musculoskeletal injuries and local pain. Isokinetic peak torque is the method of choice to assess muscle performance because of is reproducibility and association with clinical manifestations.
Inukaia and colleagues14 have determined the importance of muscle strength in sport, which may be of even greater importance in adapted sports, where players with spinal cord injury may experience a loss of active fibers and muscle mass due to their particular injury. In this regard, some researchers have stated that both the player's functional potential and their strength will influence physical performance in practice sports.15
Aspects such as muscle imbalance,2 on-court agility,16 incidence of musculoskeletal injuries,12 and pain in WB athletes,9,15,17,18 have already been addressed in the literature. However, there is a gap concerning the comparison of isokinetic shoulder evaluation between sedentary and athletic individuals with traumatic spinal cord injury at different angular velocities (60, 180, and 300°/s). The objective of the present study was to compare the peak torque, and, secondarily, other isokinetic parameters of internal and external shoulder rotators in individuals with traumatic spinal cord injury who practiced WB to those who did not.
Methods
Paricipants
The present study was approved by the Internal Review Board at Ribeirão Preto Medical School under the code No. 14185/2014. The participants signed a Free and Informed Consent form after previous explanations on the research and check for the inclusion / exclusion criteria. It was a cross-sectional study with data collected from only one study center.
The sample consisted of 36 male subjects with complete traumatic spinal cord injury below T1, aged between 18 and 45 years, divided into 18 WB athletes and 18 paraplegic non-athletic individuals. Inclusion criteria for the athletes were as follows: (1) paraplegic; (2) having spinal cord injury for at least two years; (3) using a wheelchair for locomotion in daily life; (4) training, at least, three times a week; and (5) having participated in competitions for at least two years. For the non-athletes: (1) paraplegic; (2) having a traumatic spinal cord injury for at least two years; (3) moving independently in a wheelchair in daily life; (4) not having practiced any other sport for at least two years. Excluded from both groups were: (1) individuals with joint deformities adjacent to the shoulders; (2) recent surgery in upper limbs; (3) active musculoskeletal injury of upper limbs. The athletes did not practice any resisted exercises to strengthen the shoulder girdle. Their pieces of training focused only on techniques for wheelchair mobility, throwing practice, particular basketball movements, and game tactics.
Sample size calculation considered data from a pilot study, in which mean peak torque for external rotation of the dominant upper limb at 60°/s, corrected by the body weight, was 59.08 ± 14.68 N.m/kg in athletes and 43.10 ± 16.42 N.m/kg in non-athletes. Considering the means difference to be 15.9 N.m /kg, significance level of P = 0.05 and 80% power, the total sample should include 36 subjects, being 18 athletes and 18 non-athletes.
Measures
Isokinetic evaluation was performed to quantify the peak torque corrected by weight (PTBW), muscle power and work exerted by internal and external shoulder rotators using a Biodex Isokinetic Dynamometer System 4 Pro® (Biodex Medical System Inc., Shirley, NY, USA). Subjects completed five minutes of active free upper limb exercises to warm up the joints and muscles and received orientations about the procedure and the effort required for the test as well as the testing sequence.
The subjects were positioned so that their shoulder was abducted 45 degrees in the scapular plane defined as 30 degrees anterior to abduction in the frontal plane. Range of motion was 70°, being 30° for internal rotation (IR) and 40° for external rotation (ER), from a reference position of the forearm horizontal at 0°. The humerus was aligned with the rotational axis of the dynamometer. The elbow was supported at 90° of flexion, and the forearm was in neutral pronation/supination. Self-adhesive straps were placed horizontally across the chest and pelvis to provide greater stabilization of the trunk to the seat and to minimize substitution during testing. This seated position was chosen in order to reduce stress and pain to the anterior capsule and rotator cuff, which could potentially alter the test results. Isokinetic assessments of IR and ER shoulder muscles in this seated position were shown to be valid and reliable.19 The position protocol used was in agreement with the systematic review of the positional reliability of the shoulder rotators isokinetic evaluation carried out by Edouard19 Subjects performed five submaximal repetitions for warm-up and familiarization with movements in the isokinetic dynamometer at angular speeds of 60°/s, 180°/s, and 300°/s. After this, maximal effort was made at these angular speeds to perform 5 repetitions for 60°/s and 180°/s, and 10 repetitions for 300°/s. One minute of rest separated each series of movements.
At each angular velocity, IR and ER dynamic strength was evaluated using measurements of the pPTBW (in N.m.kg − 1) to allow comparison between subjects with different morphological conditions.19
Statistical analysis
Data were analyzed with the help of the Prism Graphpad 5.0a software. Sample distribution was tested with the Shapiro–Wilk test and quantitative variables were summarized as means and standard-deviations, while the qualitative variables were grouped into categories and expressed in percentages. Student t-test was used to compare mean differences between the practice of sports and upper limb dominance in internal rotators (IR) and external rotators (ER). The angular velocity of 60°/s defined the balance between the ER and the IR musculature of the shoulder (ER/IR) and was compared with the literature.20,21 The significance level was set at (P = 0.05). Corrections for multiple tests were not performed.
Results
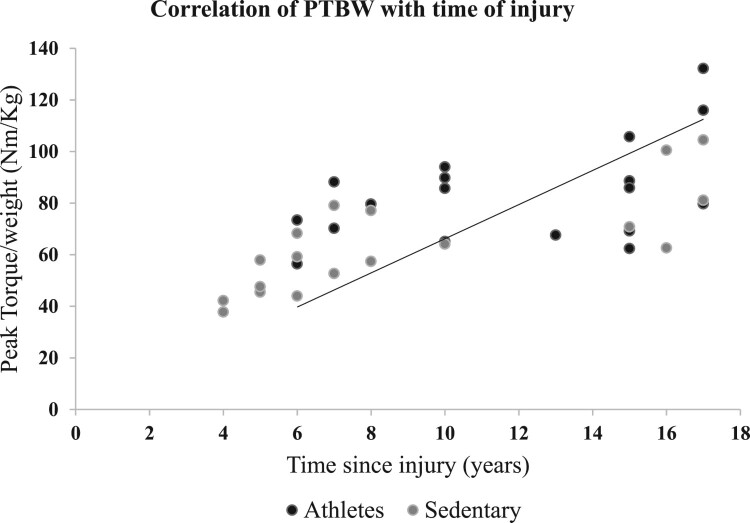
There was no statistical difference between the athletes and non-athletes regarding age, weight, height, and time since injury (Table 1). The spinal cord injury in both groups was from T12 to S4. WB athletes presented higher PTBW, work, and muscle power values of the rotator cuff when compared to the non-athletes at the velocities of 60°/s, 180°/s, and 300°/s (Table 2). There was no statistical difference for the internal rotators of the non-dominant limb at the velocities of 180°/s and 300°/s. There were no statistical differences between the dominant and non-dominant limb in all tested variables and at all speeds (Table 3). Muscle imbalances between IR and RE could not be detected (Table 3). PTBW was positively correlated with time since injury (Figure 1).
Table 1. Characteristics of the participants.
| Athletes | Non-athletes | P value* | |
|---|---|---|---|
| Variables | Mean ± SD | Mean ± SD | |
| Age (m ± dp) years | 35.6 ± 1.6 | 32.8 ± 1.8 | 0.25 |
| Weight (m ± dp) kg | 75.7 ± 3.1 | 73.4 ± 4.0 | 0.65 |
| Height (m ± dp) m | 1.74 ± 0.02 | 1.71 ± 0.01 | 0.19 |
| Time since injury (m ± dp) years | 11.7 ± 1.0 | 9.0 ± 1.1 | 0.07 |
| Time playing (m ± dp) years | 8.1 ± 3.6 |
*P = 0.05.
Table 2. Comparison of PTBW, work, and muscle power between the groups at 60°/s, 180°/s, and 300°/s.
| 60°/s | 180°/s | 300°/s | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Movements | Variables | Athletes | Non-athletes | P value* | Athletes | Non-athletes | P value* | Athletes | Non-athletes | P value* |
| Mean / SD | Mean / SD | Mean / SD | Mean / SD | Mean / SD | Mean / SD | |||||
| DER | PTBW | 58.93 ± 2.65 | 44.55 ± 3.33 | <0 . 01 | 52.87 ± 2.57 | 40.45 ± 3.20 | <0.01 | 59.47 ± 4.21 | 47.68 ± 4.02 | <0.05 |
| Work | 222.7 ± 7.8 | 175.9 ± 9.9 | <0.01 | 188.8 ± 5.8 | 140.4 ± 9.5 | <0.01 | 329.7 ± 9.3 | 247.2 ± 14.2 | <0.01 | |
| Power | 29.77 ± 1.04 | 21.53 ± 1.29 | <0.01 | 58.73 ± 2.00 | 41.03 ± 3.26 | <0.01 | 68.47 ± 2.82 | 44.93 ± 3.55 | <0.01 | |
| NDER | PTBW | 55.51 ± 4.07 | 40.33 ± 2.05 | <0.01 | 49.85 ± 3.37 | 38.82 ± 2.62 | <0.01 | 56.13 ± 3.98 | 45.79 ± 3.33 | <0.05 |
| Work | 195.1 ± 12.1 | 154.7 ± 8.3 | <0.01 | 172.1 ± 10.6 | 130.6 ± 7.1 | <0.01 | 294.8 ± 16.3 | 228.8 ± 11.9 | <0.01 | |
| Power | 26.48 ± 1.75 | 19.32 ± 1.03 | <0.01 | 54.32 ± 3.98 | 38.27 ± 2.14 | <0.01 | 60.76 ± 4.50 | 40.63 ± 2.79 | <0.01 | |
| RID | PTBW | 83.87 ± 4.57 | 64.02 ± 4.47 | <0.01 | 75.97 ± 3.36 | 58.91 ± 3.61 | <0.01 | 78.99 ± 3.39 | 65.86 ± 3.62 | <0.01 |
| Work | 325.4 ± 12.8 | 270.5 ± 11.4 | <0.01 | 290.5 ± 14.1 | 223.9 ± 12.8 | <0.01 | 530.5 ± 22.0 | 412.4 ± 18.4 | <0.01 | |
| Power | 42.77 ± 1.82 | 32.36 ± 1.56 | <0.01 | 90.07 ± 4.50 | 61.07 ± 4.13 | <0.01 | 108.20 ± 5.86 | 72.59 ± 4.18 | <0.01 | |
| NDIR | PTBW | 78.82 ± 4.79 | 62.57 ± 4.35 | <0.01 | 71.11 ± 4.68 | 60.18 ± 4.01 | <0.01 | 74.28 ± 4.83 | 64.82 ± 4.14 | 0.29 |
| Work | 301.0 ± 17.1 | 253.1 ± 12.9 | <0.05 | 266.4 ± 17.7 | 229.0 ± 11.6 | <0.08 | 443.9 ± 42.0 | 393.5 ± 21.6 | 0.14 | |
| Power | 39.14 ± 2.56 | 31.24 ± 1.78 | <0.01 | 81.50 ± 6.53 | 64.82 ± 4.06 | <0.05 | 96.09 ± 8.67 | 70.74 ± 4.78 | <0.01 | |
*P = 0.05.
Table 3. Ratio between agonist and antagonist (RI/RE) of the dominant and non-dominant limbs of athletes and non-athletes at 60°/s, 180°/s, and 300°/s.
| Velocities | Shoulder | Athletes | Non-athletes | P value* |
|---|---|---|---|---|
| 60°/s | D | 0.71 ± 0.02 | 0.70 ± 0.03 | 0.8 |
| ND | 0.71 ± 0.03 | 0.67 ± 0.03 | 0.5 | |
| 180°/s | D | 0.69 ± 0.02 | 0.68 ± 0.03 | 0.7 |
| ND | 0.71 ± 0.03 | 0.65 ± 0.02 | 0.1 | |
| 300°/s | D | 0.74 ± 0.02 | 0.72 ± 0.04 | 0.6 |
| ND | 0.82 ± 0.07 | 0.72 ± 0.05 | 0.2 |
*P = 0.05.
Figure 1.
Black dot: athlete, gray dot: non-athlete.
Discussion
Our results confirmed the hypothesis that isokinetic PTBW as well as other rotator cuff parameters from WB athletes were higher than the non-athletic group at all the tested angular velocities.
Loss of muscle mass in the acute phase after the spinal cord injury results in a catabolic state in which multiple intracellular signaling pathways stimulate the expression of specific genes. This results in protein degradation via proteasome and autophagy22 and is accompanied by increased adipose tissue in the abdominal circumference and upper limbs23 representing significant health risks after the spinal cord injury. Despite the similarity between groups concerning anthropometric parameters of height and weight, the difference of muscle performance variables may be caused by the differences in the proportion of body tissue distribution, with a higher percentage of muscle mass among those involved with regular sports activity.14
Spinal cord injuries are associated with the accumulation of visceral fat tissue.14 Spinal cord injured practitioners of sports activities develop greater muscle mass even when they have a body weight similar to sedentary individuals.24 Concerning WB, there is a component of aerobic predominance associated with the prolonged metabolic demand for the energy expenditure of dynamic acceleration, deceleration, and positional changes. Simultaneously, the anaerobic component is also present and is responsible for the short and intense bursts.25 As a result, the practice of WB stimulates the production of proteins that lead to muscle hypertrophy and increase in strength,6 which explains the greater muscle performance of WB athletes.
Daily activities regularly performed by wheelchair users demand frequent use of both upper limbs simultaneously, either to push the wheelchair on the flat and inclined surface, to overcome an obstacle, to perform transfers, or a weight-relief maneuver to prevent pressure ulcers.24 Bilateral strengthening of upper limbs is one of the bases of the rehabilitation process and seeks to prepare the body to perform those tasks by inducing symmetrical hypertrophy of the shoulder girdle. However, despite the end of inpatient rehabilitation programs, repeated practice continues to strengthen upper limbs even more.17,24 This may be the reason for the correlation between peak torque and time since injury occurred (Figure 1) and for the symmetry between the dominant and the non-dominant limbs in both groups (Table 3).
Internal rotators and ER relationship of shoulder rotators in both groups registered muscular balance, indicating the similarity between athletes and non-athletes and no influence of WB on ER/IR strength ratio. The muscular balance indicates that the internal rotators were stronger than external rotators, which may be explained by the absence of shoulder pain before the spinal cord injury.1,9,19 Surface electromyography and kinematic analysis showed high demands of muscular activities in the shoulder griddle due to the weight discharge of the individual in the wheelchair.15 To prevent displacement of the humeral head and to keep it centralized in the glenoid cavity, a muscle balance of the internal and external rotators is mandatory. Once shoulder joint is subject to a high load during the movement of the wheelchair,26,27 muscle overload can lead to imbalance.15,28,29 Future studies should assess individuals with a wider range of neurological function to clarify the role of injury level on shoulder strength.
One limitation of this study is that classification of the athletes’ functional capacity in court was not taken into account, and this may have interfered with the muscle strength. However, this would only apply to athletes and is very likely to be a consequence of muscle performance rather than a cause. Another limiting factor was the possibility of the basketball athlete having better functioning before deciding to play basketball. This problem could have been remedied with a longitudinal study. Finally, body composition of the sample was not evaluated and might interfere with muscle performance. To overcome this problem, peak torque was corrected by body weight. One may argue about the correction of significance level for multiple comparison tests, but sample size calculation for this study considered previous results of peak torque at 60°/s in a pilot study because this angular velocity has shown better reproducibility is the most used in the literature. Bonferroni correction for 40 comparisons would result in P = 0,00125, which is recognized as very severe and might require a much larger sample. Thus, we recommend the findings at lower velocities be considered definitive and suggest confirmatory studies, with properly calculated samples, for the other findings.
Conclusion
The practice of WB may have influenced the shoulder muscles of those with traumatic spinal cord injury, since the athletes presented, bilaterally, higher values of peak torque corrected by weigh, as much as other muscle performance variables, like work, and power. There was symmetry between the dominant and non-dominant, as much as we could not document agonist and antagonist (i.e. ER/IR) muscle imbalance in both groups. Time since spinal cord injury was correlated with the peak torque for internal rotators at 60°/s in both groups. These data contribute to future longitudinal studies of rotator cuff isokinetic parameters and their association with adapted sports practice.
Disclaimer statements
Contributors None.
Funding No funding was received for this study.
Conflicts of interest Authors have no conflicts of interest to declare.
References
- 1.Ambrosio F, Boninger ML. Souza AL, Fitzgerald SG, Koontz A, Cooper RA.. Biomechanics and strength of Manual wheelchair Uses. J Spinal Cord Med. 2005;28(5):407–14. doi: 10.1080/10790268.2005.11753840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cool AM, Witvrouw EE, Mahieu NN, Danneels LA.. Isokinetic scapular muscle performance in overhead Atheletes With and without Impingement Symptoms. J Athl Train. 2005;40(2):104–10. [PMC free article] [PubMed] [Google Scholar]
- 3.Johnson MP, McClure PW, Karduna AR.. New method to assess scapular upward rotation in subjects with shoulder pathology. J Orthop Sports Phys Ther. 2001;31(2):81–9. doi: 10.2519/jospt.2001.31.2.81 [DOI] [PubMed] [Google Scholar]
- 4.Kerr J, Borbas P, Meyer DC, Gerber C, Buitrago Téllez C, Wieser K.. Arthroscopic rotator cuff repair in the weight-bearing shoulder. J Shoulder Elbow Surg. 2015;24(12):1894–9. doi: 10.1016/j.jse.2015.05.051 [DOI] [PubMed] [Google Scholar]
- 5. International Wheelchair Basketball Federation IWBF classification for wheelchair basketball. 2010. (available online at: www.iwbf.org; accessed on 22.09.2015)
- 6.Lai KM, Gonzalez M, Poueymirou WT, Kline WO, Na E, Zlotchenko E, et al. Conditional activation of akt in adult skeletal muscle induces rapid hypertrophy. Mol Cell Biol. 2004;24(21):9295–304. doi: 10.1128/MCB.24.21.9295-9304.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lal S. Premature degenerative shoulder changes in spinal cord injured patients. Spinal Cord. 1998;36(3):186–9. doi: 10.1038/sj.sc.3100608 [DOI] [PubMed] [Google Scholar]
- 8.Akbar M, Brunner M, Ewerbeck V, Wiedenhöfer B, Grieser T, Bruckner T, et al. Do overhead sports increase risk for rotator cuff tears in wheelchair users? Arch Phys Med Rehabil. 2015;96(3):484–8. doi: 10.1016/j.apmr.2014.09.032 [DOI] [PubMed] [Google Scholar]
- 9.Burnham RS, May L, Nelson E, Steadward R, Reid DC.. Shoulder pain in wheelchair athletes. The role of muscle imbalance. Am J Sports Med. 1993;21(2):238–42. doi: 10.1177/036354659302100213 [DOI] [PubMed] [Google Scholar]
- 10.Mulroy SJ, Farrokhi S, Newsam CJ, Perry J.. Effects of spinal cord injury level on the activity of shoulder muscles during wheelchair propulsion: an electromyographic study. Arch Phys Med Rehabil. 2004;85(6):925–34. doi: 10.1016/j.apmr.2003.08.090 [DOI] [PubMed] [Google Scholar]
- 11.Fullerton HD, Borckardt JJ, Alfano AP.. Shoulder pain: a comparison of wheelchair athletes and nonathletic wheelchair users. Med Sci Sports Exerc. 2003;35(12):195–861. doi: 10.1249/01.MSS.0000099082.54522.55 [DOI] [PubMed] [Google Scholar]
- 12.Pellegrini A, Pegreffi F, Paladini P, Verdano MA, Ceccarelli F, Porcellini G.. Prevalence of shoulder discomfort in paraplegic subjects. Acta Biomed. 2012;83(3):177–82. [PubMed] [Google Scholar]
- 13.Finley MA, Rodgers MM.. Prevalence and identification of shoulder pathology in athletic and nonathletic wheelchair users with shoulder pain: A pilot study. J Rehabil Res Dev. 2004;41(3B):395–402. doi: 10.1682/JRRD.2003.02.0022 [DOI] [PubMed] [Google Scholar]
- 14.Inukaia Y, Takahashib K, Wanga D, Kira S.. Assessment of total and Segmental body composition in spinal cord-injured athletes in Okayama Prefecture of Japan. Acta Med Okayama. 2006;60(2):99–106. [DOI] [PubMed] [Google Scholar]
- 15.Mulroy SJ, Hatchett P, Eberly VJ, Haubert LL, Conners S, Requejo PS.. Shoulder strength and physical activity Predictors of shoulder pain in people With Paraplegia from spinal injury: Prospective Cohort study. Med Sci Sports Exerc. 2015;95(7):1027–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mason BS, Lemstra M, Van der Woude LH, Vegter R, Goosey-Tolfrey VL.. Influence of wheel configuration on wheelchair basketball performance: wheel stiffness, tyre type and tyre orientation. Med Eng Phys. 2015;37(4):392–9. doi: 10.1016/j.medengphy.2015.02.001 [DOI] [PubMed] [Google Scholar]
- 17.Gil-Agudo A, Mozos MSC, Ruiz B, Del-Ama AJ, Pérez-Rizo E, Segura-Fragoso A, et al. Shoulder kinetics and ultrasonography changes after performing a high-intensity task in spinal cord injury subjects and healthy controls. Spinal Cord. 2016;54(4):277–82. doi: 10.1038/sc.2015.140 [DOI] [PubMed] [Google Scholar]
- 18.Mccasland LD, Budiman-mak E, Weaver FM, Adams E, Miskevics S.. Shoulder pain in the traumatically injured spinal cord patient: evaluation of risk factors and function. J Clin Rheumatol. 2006;12(4):179–86. doi: 10.1097/01.rhu.0000230532.54403.25 [DOI] [PubMed] [Google Scholar]
- 19.Edouard P, Samozino P, Julia M, Gleizes CS, Vanbiervliet W, Calmels P, Gremeaux V, et al. Reliability of isokinetic assessment of shoulder-rotator strength: a systematic review of the effect of position. J Sport Rehabil. 2011;0(3):367–83. doi: 10.1123/jsr.20.3.367 [DOI] [PubMed] [Google Scholar]
- 20.Ellenbecker TS, Mattalino AJ.. Concentric isokinetic shoulder internal and external rotation strength in professional baseball pitchers. J Orthop Sports Phys Ther. 1997;25(5):323–8. doi: 10.2519/jospt.1997.25.5.323 [DOI] [PubMed] [Google Scholar]
- 21.Hughes RE, Johnson ME, O'Driscoll SW, An KN.. Normative values of agonist-antagonist shoulder strength ratios of adults aged 20 to 78 years. Arch Phys Med Rehabil. 1999;80(10):1324–6. doi: 10.1016/S0003-9993(99)90037-0 [DOI] [PubMed] [Google Scholar]
- 22.Cohen S, Nathan JA, Goldberg AL.. Muscle wasting in disease: molecular mechanisms and promising therapies. Nat Rev Drug Discov. 2015;14(1):58–74. doi: 10.1038/nrd4467 [DOI] [PubMed] [Google Scholar]
- 23.Gorgey AS, Wells KM, Austin TL.. Adiposity and spinal cord injury. World J Orthop. 2015;6(8):567–76. doi: 10.5312/wjo.v6.i8.567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gagnon D, Babineau AC, Champagne A, Desroches G, Aissaouiet R.. Trunk and shoulder kinematic and Kinetic and Electromyographic Adaptations to Slope increase during Motorized Treadmill Propulsion among Manual wheelchair users with a spinal cord injury. Biomed Res Int. 2015. doi: 10.1155/2015/636319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Coutts KD. Dynamics of wheelchair basketball. Med Sci Sports Exerc. 1992;24(2):231–4. doi: 10.1249/00005768-199202000-00012 [DOI] [PubMed] [Google Scholar]
- 26.Arnet U, Van Drongelen S, Scheel-Sailer A, van der Woude LH, Veeger DH.. Shoulder load during synchronous handcycling and handrim wheelchair propulsion in persons with paraplegia. J Rehabil Med. 2012;44(3):222–8. doi: 10.2340/16501977-0929 [DOI] [PubMed] [Google Scholar]
- 27.Fokter SK, Cicak N, Skorja J.. Functional and electromyographic results after open rotator cuff repair. Clin Orthop Relat Res. 2003;10(415):121–30. doi: 10.1097/01.000093903.12372.3f [DOI] [PubMed] [Google Scholar]
- 28.Perry J, Gronley JK, Newsam CJ, Reyes ML, Mulroy SJ.. Electromyographic analysis of the shoulder muscles during depression transfers in subjects with low-level paraplegia. Arch Phys Med Rehabil. 1996;77(4):350–5. doi: 10.1016/S0003-9993(96)90083-0 [DOI] [PubMed] [Google Scholar]
- 29.Reyes ML, Gronley JK, Newsam CJ, Mulroy SJ, Perry J.. Electromyographic analysis of shoulder muscles of men with low-level paraplegia during a weight relief raise. Arch Phys Med Rehabil. 1995;76(5):433–9. doi: 10.1016/S0003-9993(95)80572-9 [DOI] [PubMed] [Google Scholar]