Abstract
Objective: Evaluate the association between body mass index (BMI, kg/m2) and one-year mortality among people who survived the first 90 days after spinal cord injury (SCI).
Design: Cohort study.
Setting: Eighteen SCI Model Systems centers throughout the United States.
Participants: 6640 participants (men, 79.6%; mean age, 42.8 ± 17.7y; Whites, 62.3%) who had an SCI between October 2006 and March 2017.
Interventions: Not applicable.
Outcome Measures: All-cause mortality and causes of death. Life table method was used to estimate mortality rates, while Cox proportional hazard model was conducted to assess the impact of BMI on mortality after adjusting for demographic and injury-related factors.
Results: Based on BMI obtained during initial rehabilitation, participants were classified into underweight (4.2%), normal weight (41.2%), overweight (30.9%) and obese (23.8%) groups, and their corresponding one-year mortality rates were 2.6%, 1.8%, 3.1%, 3.5%, respectively (P = 0.002). After adjusting for potential confounding factors, people with obesity had a higher mortality risk than those with normal weight (hazard ratio, 1.51; 95% confidence interval, 1.00–2.28). The most frequent causes of death for people with obesity were infective and parasitic diseases and respiratory diseases, while respiratory diseases were the most frequent for people with other BMI statuses.
Conclusion: People with obesity who incur an SCI need special attention to prevent early mortality. Future studies should explore factors that contribute to such a higher mortality after SCI, such as preexisting conditions and comorbidities. The effects of BMI on long-term mortality also deserve further investigation.
Keywords: Spinal cord injury, Mortality, Body mass index
Introduction
In the spinal cord injury (SCI) population, the mortality rate within the first year after injury is significantly higher than the following years.1–5 The in-hospital acute mortality after SCI is about 5.7% to 8.0%.2–5 The first-year average mortality rate after the injury is 4.6%, which is almost two times greater than that of the second year to 20 years later (1.7–2.4%).1 The leading causes of death also vary by the duration of the injury. While respiratory diseases (28.0%) are the leading causes of death that occur within year 1 after injury; heart diseases (18.8%), external causes (including suicides, homicides, and accidents, 18.3%), and respiratory diseases (18.0%) are the primary causes of death beyond year 1 post-injury.6 In comparison, the leading causes of death in the general population are heart diseases (23.0%), cancers (21.3%) and accidents (6.0%).7
To improve the life expectancy of people with SCI, it is important to identify and then intervene to minimize the risk factors for mortality. Previous studies have linked mortality with a number of risk factors in the SCI population, including demographic information, injury characteristics, psychological and socio-environmental factors, health behaviors and health status.3,4,8–13 The early mortality rate is elevated among males, the elderly (≥ 65 years), and those who are injured by acts of violence and have high cervical injuries, concomitant injuries, multiple comorbidities, and multiple complications.3,4,6,13–15
In the general population, it is well accepted that obesity (body mass index (BMI) ≥30.0) is associated with an increased mortality risk by 30 to 70%, even after controlling for individual characteristics, such as age, sex, education, marital status, alcohol use, smoking, and physical activity.16–21 Underweight (BMI <18.5) is also associated with excess deaths.22,23 In addition, different BMI statuses are associated with certain causes of death in the general population. For example, among persons with BMI ≥25.0, there is a positive association between BMI and vascular and diabetic causes of death.20,24 However, a smaller BMI value (BMI < 22.5) implies a higher risk of respiratory disease-related deaths.20
Little is known about the association between BMI and mortality in the SCI population. By measuring a person’s weight in relation to height, BMI could be used to estimate the body fat and predict the risk of morbidity in the SCI population.25–27 Gater et al. found that people with BMI ≥22 had a higher risk of metabolic syndrome than those with BMI < 22, after adjusting individual characteristics, such as age, race, and neurological status.27 Furthermore, being obese (BMI ≥ 30) is associated with more frequent rehospitalization, reduced self-care capability, and decreased functional mobility among people with SCI.28–30 Despite the higher risk of dying during the first year compared to other years after the injury, there is no study that focused on the impact of BMI on one-year mortality.
Due to the neurological deficits of people with SCI, it is difficult to generalize findings of the BMI-mortality association in the general population to the SCI population. Because of neurological impairment and associated secondary complications,31,32 people with SCI have a shorter life expectancy than people without disability of same age, sex, and race, with standardized mortality ratios ranging from 1.55–52.31.1 Therefore, this study aimed to examine the association between BMI and mortality during year 1 after injury and identify the leading causes of death by BMI status, through analyzing data from the National SCI Model Systems (SCIMS) Database.
Methods
Data source
This project is a secondary analysis of data from the National SCIMS Database, the details of which have been described previously.33 Currently, the National SCIMS Database is estimated to capture data from approximately 6% of new SCI cases every year in the United States.33 The Institutional Review Board at National SCI Statistical Center (NSCISC) and each SCIMS center approved the data collection and utilization.
Study participants
To be eligible for this study, participants had to meet the following criteria: age at injury greater than 17 years and enrolled in the SCIMS Database on/after October 1, 2006, when weight and height data became available. Although SCIMS Database participants were admitted to the SCIMS within one year of injury, many received acute care at other facilities, thereby delaying enrollment until admission to the SCIMS rehabilitation setting. Therefore, to eliminate the bias caused by delayed admissions and incomplete reporting of deaths that occurred prior to SCIMS rehabilitation admission, we further limited the analysis to those who were admitted to the SCIMS centers within 90 days of injury and also survived the first 90 days after injury. As of March 16, 2017, 6735 people met the above eligibility criteria. Participants were later excluded if they had missing data on weight (n = 78) or height (n = 17). The final analytical sample included 6640 SCIMS Database participants from 18 SCIMS centers.
Vital status and causes of death
Deaths were identified by routine follow-up of study participants conducted in person, by phone or mail at each SCIMS center as well as online searches of databases and death notices conducted both at each SCIMS center and at the NSCISC. Web sites used to identify deaths include but are not limited to combinations of www.tlo.com, www.accurint.com, www.ancestry.com, www.findagrave.com, www.mylife.com, www.genealogybank.com, www.legacy.com, www.tributes.com, as well as Google searches for online newspaper and funeral home obituaries. Many of these sites include access to the Social Security Death Index which has been previously demonstrated to have 92.4% sensitivity and 99.5% specificity in identifying survival status for individuals in the National SCIMS Database.34 The NSCISC and some SCIMS centers also occasionally submit lists of cases to the National Death Index (NDI) when suspected deaths may have been missed by other means. The most recent systematic search for deaths conducted by NSCISC staff occurred in February and March of 2019.
Information on the cause of death was obtained from hospital discharge summaries, autopsy reports, death certificates, and NDI searches. The most recent NDI search was conducted in July 2018 for deaths that occurred up to December 2017. The causes of death were coded according to International Statistical Classification of Diseases and Related Health Problems, 10th revision (ICD-10). When multiple causes were reported, the underlying cause of death was determined by following the instructions of the National Center for Health Statistics35 with two exceptions. If either SCI without further detail or the original event that caused the SCI was the only listed cause of death, then the underlying cause of death was considered unknown because we were only interested in the nature of post-SCI fatal medical complications or events.
Measures
Body mass index (kg/m2) was estimated by measured body weight (kg) and self-reported height (m) obtained during initial rehabilitation. Bodyweight was measured with light clothing on a wheelchair-accessible scale or bed scale. According to the population standard,36 participants were grouped into: (1) underweight (BMI <18.5 kg/m2); (2) normal weight (BMI 18.5–24.9 kg/m2); (3) overweight (BMI 25.0–29.9 kg/m2); and (4) obesity (BMI ≥ 30.0 kg/m2).
Demographic (age at injury, sex, race/ethnicity, marital status, education, and employment) and injury-related factors (etiology, ventilator dependency, level of injury, completeness of injury, vertebral injury, associated injury and spinal surgery) were obtained during initial hospital care. To be consistent with the International Standards for Neurological Classification of SCI and the International SCI Core Data Set,37,38 neurological status was categorized into (1) ventilator dependent; (2) high tetraplegia (C1-C4) with motor functional complete injury (American Spinal Cord Injury Association Impairment Scale (AIS) A, B, or C); (3) low tetraplegia (C5-C8) with AIS A, B, or C; (4) paraplegia with AIS A, B, or C; and (5) motor functional incomplete injury at any level (AIS D). The associated injury was defined as the presence of one or more of the following injuries requiring surgery or intervention that occurred at the time of injury: traumatic brain injury, non-vertebral fractures, severe facial injuries affecting sensory organs, major chest injury, amputation, severe hemorrhaging, brachial plexus injury, and internal organ injury.37
Statistical analysis
Analysis of variance and Chi-square tests were used to compare the demographic and injury-related factors between the excluded and included participants as well as across the four BMI groups among 6640 study participants. Life table method was used to estimate one-year mortality rate for each BMI group, while log-rank test was performed to assess the significance of differences in mortality rate among the groups.39 For analytic purposes, the survival status of participants was determined on the first-anniversary date of injury or December 31, 2017, whichever came first. If participants were deceased, their survival time was counted from the date of injury to the date of death. For those classified as “alive,” the survival time was counted from the date of injury to the first-anniversary date of injury, December 31, 2017, or the date last known to be alive, whichever came first. Data on causes of death were analyzed and compared across BMI groups by using descriptive statistics, including frequencies and percentages.
After ascertaining that proportional hazards assumption was not violated using the supremum test, Cox proportional hazards model was performed to compare mortality risks across BMI groups adjusting for demographics and injury-related factors. Only participants with complete data for all covariates (n = 6405, 96.5%) were used for the development of the multivariate model.
SAS 9.4 statistical software was used to analyze data. Statistical significance was considered when P value was less than 0.05.
Results
There were no significant differences between 6640 study participants and 95 excluded individuals due to missing height or weight data in terms of demographic and injury-related factors, except for employment and etiology. Study participants were more likely to be employed (61.7% vs 51.1%, P = 0.02) and be injured by falls (30.4% vs 25.0%) and sports (8.3% vs 3.3%, P = 0.03), when compared with the excluded.
The mean BMI, weight, and height of 6640 participants were 26.7 ± 6.3 kg/m2, 82.4 ± 20.9 kg, and 1.76 ± 0.10 m during initial rehabilitation, respectively. The approximate timing of BMI measurements averaged 22–75 days after injury, based on the average time from injury to rehabilitation admission (22 days) and the average length of rehabilitation stay (53 days). As shown in Table 1, the prevalence of obesity, overweight, and underweight was 23.8%, 30.8%, and 4.2%, respectively. There were significant differences across BMI groups on demographic and injury-related factors, except spinal surgery. Regarding risk factors for mortality that were identified in previous studies, people with obesity tend to be older and have injuries as a result of medical/surgical complications and falls, while people with underweight were more likely to have more severe injuries and violent etiologies.
Table 1. Demographic and injury-related characteristics by BMI status.
| Characteristics | BMI status | P‡ | ||||
|---|---|---|---|---|---|---|
| Total | Underweight (<18.5) | Normal weight (18.5–24.9) | Overweight (25.0–29.9) | Obesity (≥30.0) | ||
| Sample size | 6640 | 280 (4.2) | 2734 (41.2) | 2049 (30.8) | 1577 (23.8) | |
| BMI | 26.7 ± 6.3 | 17.2 ± 1.2 | 22.2 ± 1.8 | 27.3 ± 1.4 | 35.4 ± 5.8 | <0.0001 |
| Weight (kg) | 82.4 ± 20.9 | 54.0 ± 6.6 | 68.8 ± 9.3 | 84.7 ± 9.9 | 107.8 ± 21.1 | <0.0001 |
| Height (m) | 1.76 ± 0.10 | 1.77 ± 0.09 | 1.76 ± 0.10 | 1.76 ± 0.09 | 1.74 ± 0.11 | <0.0001 |
| Age at injury | 42.8 ± 17.7 | 33.4 ± 17.1 | 39.1 ± 17.8 | 45.4 ± 17.1 | 47.5 ± 16.4 | <0.0001 |
| Sex | <0.0001 | |||||
| Male | 5288 (79.6) | 216 (77.1) | 2189 (80.1) | 1715 (83.7) | 1168 (74.1) | |
| Female | 1352 (20.4) | 64 (22.9) | 545 (19.9) | 334 (16.3) | 409 (25.9) | |
| Race | <0.0001 | |||||
| White | 4101 (62.3) | 145 (52.5) | 1640 (60.5) | 1355 (66.5) | 961 (61.6) | |
| Black | 1546 (23.5) | 107 (38.8) | 671 (24.8) | 394 (19.3) | 374 (23.9) | |
| Hispanic | 679 (10.3) | 19 (6.9) | 263 (9.7) | 221 (10.9) | 176 (11.3) | |
| Other | 259 (3.9) | 5 (1.8) | 136 (5.0) | 68 (3.3) | 50 (3.2) | |
| Unknown | 55 | 4 | 24 | 11 | 16 | |
| Marital status | <0.0001 | |||||
| Married | 2624 (39.8) | 51 (18.3) | 871 (32.1) | 926 (45.4) | 776 (49.7) | |
| Single | 2894 (43.9) | 199 (71.6) | 1441 (53.0) | 732 (35.9) | 522 (33.4) | |
| Other | 1075 (16.3) | 28 (10.1) | 404 (14.9) | 380 (18.7) | 263 (16.9) | |
| Unknown | 47 | 2 | 18 | 11 | 16 | |
| Education | <0.0001 | |||||
| <High school | 1005 (15.3) | 74 (26.5) | 457 (16.9) | 262 (13.0) | 212 (13.6) | |
| High school | 3550 (54.1) | 161 (57.7) | 1483 (55.0) | 1068 (52.8) | 838 (53.8) | |
| >High school | 1911 (29.2) | 41 (14.7) | 721 (26.7) | 666 (32.9) | 483 (31.0) | |
| Other | 92 (1.4) | 3 (1.1) | 38 (1.4) | 26 (1.3) | 25 (1.6) | |
| Unknown | 82 | 1 | 35 | 27 | 19 | |
| Occupation | <0.0001 | |||||
| Unemployed | 1020 (15.5) | 62 (22.3) | 462 (17.1) | 283 (13.9) | 213 (13.7) | |
| Employed | 4053 (61.7) | 152 (54.7) | 1603 (59.3) | 1318 (64.7) | 980 (63.0) | |
| Retired | 799 (12.1) | 19 (6.8) | 267 (9.9) | 269 (13.2) | 244 (15.7) | |
| Student or trainee | 459 (7.0) | 36 (13.0) | 285 (10.5) | 91 (4.5) | 47 (3.0) | |
| Other | 242 (3.7) | 9 (3.2) | 86 (3.2) | 75 (3.7) | 72 (4.6) | |
| Unknown | 67 | 2 | 31 | 13 | 21 | |
| Etiology | <0.0001 | |||||
| Vehicular | 2556 (38.5) | 119 (42.5) | 1074 (39.3) | 771 (37.7) | 592 (37.6) | |
| Violence | 930 (14.0) | 75 (26.8) | 462 (16.9) | 242 (11.8) | 151 (9.6) | |
| Falls | 2017 (30.4) | 55 (19.6) | 738 (27.0) | 671 (32.8) | 553 (35.1) | |
| Sports | 553 (8.3) | 18 (6.4) | 267 (9.8) | 178 (8.7) | 90 (5.7) | |
| Medical/surgical | 324 (4.9) | 8 (2.9) | 93 (3.4) | 93 (4.5) | 130 (8.2) | |
| Other | 255 (3.9) | 5 (1.8) | 97 (3.6) | 93 (4.5) | 60 (3.8) | |
| Unknown | 5 | 0 | 3 | 1 | 1 | |
| Neurological category | 0.0002 | |||||
| Vent dependent | 182 (2.8) | 8 (2.9) | 72 (2.7) | 57 (2.8) | 45 (2.9) | |
| C1-4, AIS ABC | 1058 (16.0) | 62 (22.2) | 424 (15.6) | 308 (15.2) | 264 (16.9) | |
| C5-8, AIS ABC | 874 (13.3) | 48 (17.2) | 394 (14.5) | 249 (12.3) | 183 (11.7) | |
| T1-S3, AIS ABC | 2069 (31.4) | 87 (31.2) | 887 (32.7) | 620 (30.5) | 475 (30.3) | |
| All AIS DE | 2405 (36.5) | 74 (26.5) | 937 (34.5) | 796 (39.2) | 598 (38.2) | |
| Unknown | 52 | 1 | 20 | 19 | 12 | |
| Vertebral injury | <0.0001 | |||||
| Yes | 5304 (80.1) | 234 (83.9) | 2273 (83.3) | 1610 (78.8) | 1187 (75.4) | |
| No | 1321 (19.9) | 45 (16.1) | 455 (16.7) | 434 (21.2) | 387 (24.6) | |
| Unknown | 15 | 1 | 6 | 5 | 3 | |
| Associated injury | <0.0001 | |||||
| Yes | 2581 (39.0) | 152 (54.5) | 1155 (42.4) | 740 (36.2) | 534 (34.0) | |
| No | 4040 (61.0) | 127 (45.5) | 1570 (57.6) | 1305 (63.8) | 1038 (66.0) | |
| Unknown | 19 | 1 | 9 | 4 | 5 | |
| Spinal surgery | 0.5976 | |||||
| Yes | 5289 (79.8) | 218 (77.9) | 2166 (79.3) | 1636 (80.0) | 1269 (80.7) | |
| No | 1339 (20.2) | 62 (22.1) | 564 (20.7) | 410 (20.0) | 303 (19.3) | |
| Unknown | 12 | 0 | 4 | 3 | 5 | |
Notes: Values are mean ± SD or n (%). Female includes two persons of transgender. Other race includes American Indian, Alaska Native, Asian, Pacific Islander, some other race and multiracial category. Other marital status includes divorced, separated, widowed, and unclassified. Other education includes 3-year nursing degree, special education and unclassified. Other occupation includes homemaker and unclassified.
‡Comparison across BMI status using the Chi-square test or analysis of variance.
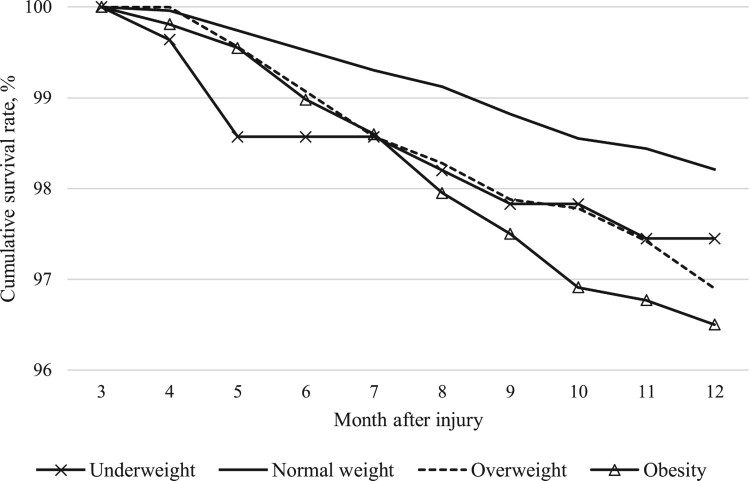
Of 6640 study participants, who survived the first 90 days of injury, 180 (2.7%) were reported deceased within the first year of injury. Figure 1 illustrates the estimated survival curve for each BMI status (P = 0.002) during 4–12 months after injury. The one-year mortality rate was highest for people with obesity (3.5%), followed by overweight (3.1%), underweight (2.6%), and normal weight (1.8%).
Figure 1.
Cumulative survival rate estimated by life table by BMI status.
The results of the Cox models are shown in Table 2. The hazard ratio (HR) of one-year mortality is 1.51 (95% CI, 1.00–2.28) for people with obesity relative to people with normal weight, after adjusting for variations in demographics and injury-related factors. However, there was no significant increased risk of death in the overweight group (HR, 1.28; 95% CI, 0.85–1.92) or underweight group (HR, 1.50; 95% CI, 0.59–3.82). Also, a higher risk of mortality was observed among people who were of old ages, male, single, injured by falls and medical/surgical complications, and having severe injuries, when compared with their respective counterparts.
Table 2. Cox proportional hazards model for predicting one-year mortality.
| Crude hazard ratio | 95% CI | Adjusted hazard ratio | 95% CI | |
|---|---|---|---|---|
| BMI status | ||||
| Underweight | 1.37 | 0.62, 3.01 | 1.50 | 0.59, 3.82 |
| Normal weight | Ref | Ref | Ref | Ref |
| Overweight | 1.72 | 1.19, 2.48 | 1.28 | 0.85, 1.92 |
| Obesity | 1.97 | 1.35, 2.87 | 1.51 | 1.00, 2.28 |
| Age at injury (5-year unit) | 1.37 | 1.31, 1.44 | 1.40 | 1.29, 1.52 |
| Sex | ||||
| Male | 1.19 | 0.81, 1.74 | 2.07 | 1.32, 3.25 |
| Female | Ref | Ref | Ref | Ref |
| Race | ||||
| White | Ref | Ref | Ref | Ref |
| Black | 0.83 | 0.58, 1.19 | 1.27 | 0.83, 1.95 |
| Hispanic/other | 0.56 | 0.33, 0.95 | 0.80 | 0.45, 1.44 |
| Marital status | ||||
| Married | Ref | Ref | Ref | Ref |
| Single | 0.47 | 0.32, 0.68 | 2.01 | 1.24, 3.24 |
| Other | 1.62 | 1.15, 2.30 | 1.75 | 1.17, 2.60 |
| Education | ||||
| <High school | Ref | Ref | Ref | Ref |
| High school | 0.73 | 0.48, 1.11 | 0.70 | 0.44, 1.11 |
| >High school/other | 0.91 | 0.58, 1.42 | 0.61 | 0.37, 1.02 |
| Employment | ||||
| Employed | Ref | Ref | Ref | Ref |
| Unemployed | 1.76 | 1.13, 2.75 | 1.52 | 0.91, 2.54 |
| Retired | 6.15 | 4.39, 8.62 | 1.38 | 0.88, 2.18 |
| Student or trainee | 0.14 | 0.02, 1.00 | 0.56 | 0.08, 4.23 |
| Other | 2.70 | 1.38, 5.25 | 1.11 | 0.47, 2.62 |
| Etiology | ||||
| Vehicular | Ref | Ref | Ref | Ref |
| Violence | 1.10 | 0.56, 2.14 | 1.55 | 0.66, 3.62 |
| Falls | 4.02 | 2.66, 6.06 | 2.11 | 1.31, 3.39 |
| Sports | 1.38 | 0.66, 2.91 | 2.18 | 0.96, 4.92 |
| Medical/surgical | 7.68 | 4.59, 12.86 | 6.02 | 3.09, 11.74 |
| Other | 2.37 | 1.04, 5.40 | 2.32 | 1.00, 5.36 |
| Neurological status | ||||
| Dependent | 5.96 | 3.49, 10.19 | 9.93 | 5.32, 18.55 |
| C1-4 ABC | 2.62 | 1.76, 3.92 | 3.94 | 2.55, 6.08 |
| C5-8 ABC | 1.55 | 0.95, 2.53 | 3.29 | 1.94, 5.57 |
| T1-S3 ABC | 0.90 | 0.58, 1.40 | 1.96 | 1.19, 3.23 |
| All AIS DE | Ref | Ref | Ref | Ref |
| Vertebral injury | ||||
| Yes | 0.50 | 0.37, 0.69 | 1.20 | 0.79, 1.82 |
| No | Ref | Ref | Ref | Ref |
| Associated injury | ||||
| Yes | 0.74 | 0.54, 1.01 | 1.34 | 0.92, 1.95 |
| No | Ref | Ref | Ref | Ref |
| Spinal surgery | ||||
| Yes | 0.72 | 0.51, 1.00 | 0.99 | 0.65, 1.50 |
| No | Ref | Ref | Ref | Ref |
Notes: Adjusted model includes all variables listed in the table. Female includes two persons of transgender. Other race includes American Indian, Alaska Native, Asian, Pacific Islander, some other race and multiracial category. Other marital status includes divorced, separated, widowed, and unclassified. Other education includes 3-year nursing degree, special education and unclassified. Other occupation includes homemaker and unclassified.
Of 180 deaths, 143 (79.4%) had causes of death identified. As shown in the Table 3, the top three causes of death overall were respiratory diseases [n = 37, 25.9%; of which 24 (64.9%) were cases of pneumonia], infective and parasitic diseases [n = 24, 16.8%; of which 22 (91.7%) were cases of septicemia], as well as hypertensive and ischemic heart diseases (n = 18, 12.6%). Among people with obesity, infective and parasitic diseases (n = 12, 27.3%) and respiratory diseases (n = 11, 25.0%) collectively accounted for more than half of the deaths with known causes, while pulmonary circulation diseases ranked third (n = 6, 13.6%). In contrast, among people who were overweight, respiratory diseases were the leading cause of death (n = 11, 21.2%), followed by hypertensive and ischemic heart diseases (n = 10, 19.2%), other heart diseases (n = 7, 13.5%), cancer (n = 6, 11.5%), and infective and parasitic diseases (n = 5, 9.6%).
Table 3. Cause of death during the first year after injury by BMI status.
| Cause of death, n (%) | BMI status | ||||
|---|---|---|---|---|---|
| Total | Underweight (<18.5) | Normal weight (18.5–24.9) | Overweight (25.0–29.9) | Obesity (≥30.0) | |
| Total deaths | 180 | 7 | 51 | 65 | 57 |
| Respiratory diseases (J00-J99) | 37 (25.9) | 2 (28.5) | 13 (32.5) | 11 (21.2) | 11 (25.0) |
| Infective and parasitic diseases (A00-B99) | 24 (16.8) | 1 (14.3) | 6 (15.0) | 5 (9.6) | 12 (27.3) |
| Hypertensive and ischemic heart diseases (C00-D48) | 18 (12.6) | 0 (0.0) | 4 (10.0) | 10 (19.2) | 4 (9.1) |
| Other heart diseases (I00-I09, I46) | 12 (8.4) | 1 (14.3) | 3 (7.5) | 7 (13.5) | 1 (2.3) |
| Cancers (I10-I25) | 9 (6.3) | 1 (14.3) | 1 (2.5) | 6 (11.5) | 1 (2.3) |
| Pulmonary circulation diseases 7 (I26-I28) | 8 (5.6) | 0 (0.0) | 2 (5.0) | 0 (0.0) | 6 (13.6) |
| Cerebrovascular diseases (I60-I69) | 5 (3.5) | 0 (0.0) | 2 (5.0) | 2 (3.9) | 1 (2.3) |
| Endocrine, nutritional, metabolic and immunity disorders (E00-E90) | 4 (2.8) | 0 (0.0) | 1 (2.5) | 0 (0.0) | 3 (6.8) |
| Mental disorders (F00-F99) | 4 (2.8) | 0 (0.0) | 2 (5.0) | 2 (3.9) | 0 (0.0) |
| Genitourinary diseases (N00-N99) | 3 (2.1) | 0 (0.0) | 0 (0.0) | 2 (3.9) | 1 (2.3) |
| Digestive diseases (K00-K93) | 3 (2.1) | 1 (14.3) | 0 (0.0) | 2 (3.9) | 0 (0.0) |
| Arteries, arterioles, and capillaries diseases (I70-I79) | 3 (2.1) | 0 (0.0) | 0 (0.0) | 2 (3.9) | 1 (2.3) |
| Othera | 13 (9.0) | 1 (14.3) | 6 (15.0) | 3 (5.5) | 3 (6.7) |
| Unknown causes | 37 | 0 | 11 | 13 | 13 |
aCauses of death that account for less than 2% of overall death, including musculoskeletal and connective tissue diseases, nervous and sense organs diseases, blood and blood-forming organs diseases, subsequent trauma of uncertain nature, symptoms and ill-defined conditions, unintentional injuries, homicides, and suicide.
Discussion
We assessed the impact of baseline BMI status on one-year mortality among 6640 people who survived the first 90 days after SCI. The findings suggest that people who are obese have a 51% higher mortality risk during the remainder of the first year post-injury compared with those with normal weight, after adjusting for demographic and injury-related factors. Consistent with previous SCI studies,6,9,12,40,41 we also found a higher mortality rate among males and those of older age, unmarried, injured by falls and medical/surgical complications, and severe injuries.
In general, excess accumulation of adipose tissue in the body inhibits fatty acid oxidation and glucose regulation, which promotes the development of chronic diseases, such as metabolic syndrome, diabetes and cardiovascular diseases.22,42–46 It is possible that people with obesity in this study had more preexisting medical conditions or comorbidities (sicker than people of other BMI status), which subsequently increased their risk of dying during the first year after SCI. This finding was corroborated by a recent study that reported the highest mortality rate among people with medical complication-related SCI, as compared with other etiologies.12
Because of reduced metabolism after injury, people experience neurogenic obesity that could contribute to infections, including urinary tract infection, pneumonia, and pressure injuries.46–51 Being obese at the time of injury may enhance the risk of infections due to the overproduction of proinflammatory mediators by excess adipose tissue (tumor necrosis factors-α, interleukin-1, interleukin-6, and C-reactive protein),45,46,52 which contribute to an increased risk of dying from respiratory diseases (primary pneumonia) and infective and parasitic diseases (primary septicemia) among people with SCI and obesity.53
Our study findings suggest that a greater percentage of deaths are related to pulmonary circulation diseases (such as pulmonary embolism and deep vein thrombosis) among people with obesity when compared with people with other BMI statuses. This is consistent with findings in the general population that obesity, beyond physical inactivity, is a risk factor of developing venous thrombosis.54,55
Because our study focused on BMI during initial rehabilitation and its association with one-year mortality, the effect of BMI on long-term mortality in the SCI population is unclear. In the general population, studies suggested that maximum BMI over time is more likely to capture the obesity-death association than BMI at a survey time.24,56–58 The HR of the obesity group relative to the normal weight group increased from 1.18 by using BMI at time of survey to 1.67 by using maximum BMI among 5540 participants.56 Given people tend to gain weight after injury,59–63 researchers should take weight history into consideration, when evaluating the BMI-mortality association in the chronic SCI population.
Similar to the findings of a 10-year mortality study,64 our study findings indicated a tendency of a higher mortality rate among people with underweight. The result did not reach statistical significance perhaps because of a small sample size of people who were underweight. However, the effect of underweight on mortality should not be ignored. People who are underweight have a small percentage of fat mass, suggesting an increase in pressure on the bony prominences, which could heighten the risk of pressure injury. Furthermore, chronic pressure injury is a strong risk factor for death in people with chronic SCI.11,40,41 In the future, larger sample size is needed to validate and precisely estimate the risk of death among people who are underweight.
Limitations
There are several limitations that should be noted. First, because of the study inclusion/exclusion criteria, the reported impact of BMI on one-year mortality may not apply to the first 90 days post-injury. The study findings might also overrepresent people who are employed and injured by falls and sports. Second, readers should be aware of the limited representation of SCIMS Database participants,33 such as a hospital-based study sample and overrepresentation of violent etiologies occurring in young men of minority races due to the urban location of many SCIMS centers. People who have minimal neurological deficits required no rehabilitation or who have too severe injuries to engage in rehabilitation would have been missed in the database. However, this study was not designed to estimate absolute risk in the overall SCI population but rather the relative risk of mortality across BMI categories. As such, bias will only be introduced if the relationship between BMI and mortality is different in persons treated at an SCIMS center compared to persons treated elsewhere after adjusting for demographic and injury characteristics. Third, due to the limitation of secondary data analysis, we cannot assess other important risk factors for mortality, such as smoking and preexisting diseases that are not included in the database. Fourth, BMI in this study is based on measured weight and self-reported height. As people tend to overreport height, BMI could be underestimated.65 Finally, 20.6% of causes of death were unknown and could be meaningfully different from the known causes of death. Future studies with a larger sample size are needed to estimate the relationship between BMI and cause-specific mortality.
Conclusion
Given people with obesity have a high risk of mortality within the first year post-injury, health professionals should target people with obesity at the acute care setting for weight management to prevent premature deaths in the SCI population. Future studies are needed to explore the factors that contribute to a higher death rate in people with obesity and SCI, such as preexisting diseases and comorbidities. Additional studies are warranted to examine the association between BMI and long-term mortality.
Acknowledgements
NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this manuscript do not necessarily represent the policy of NIDILRR, ACL, HHS, and you should not assume endorsement by the Federal Government.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Disclaimer statements
Contributors None.
Funding This work was funded by the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR) (90DP0083).
Conflicts of interest The authors declare no conflicts of interest.
References
- 1.National Spinal Cord Injury Statistical Center . Annual Statistical Report for the Spinal Cord Injury Model Systems. Birmingham, AL: University of Alabama at Birmingham. 2018. [cited 2018 December 1]. Available from https://www.nscisc.uab.edu/Public_Pages/ReportsStats. [Google Scholar]
- 2.Hall OT, McGrath RP, Peterson MD, Chadd EH, DeVivo MJ, Heinemann AW, et al. The burden of traumatic spinal cord injury in the United States: disability-adjusted life years. Arch Phys Med Rehabil . 2019;100(1):95–100. [DOI] [PubMed] [Google Scholar]
- 3.Selassie AW, Varma A, Saunders LL, Welldaregay W.. Determinants of in-hospital death after acute spinal cord injury: a population-based study. Spinal Cord . 2013;51(1):48–54. [DOI] [PubMed] [Google Scholar]
- 4.Jain NB, Ayers GD, Peterson EN, Harris MB, Morse L, O'Connor KC, et al. Traumatic spinal cord injury in the United States, 1993-2012. JAMA. 2015;313(22):2236–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Macias CA, Rosengart MR, Puyana JC, Linde-Zwirble WT, Smith W, Peitzman AB, et al. The effects of trauma center care, admission volume, and surgical volume on paralysis after traumatic spinal cord injury. Ann Surg . 2009;249(1):10–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DeVivo MJ, Krause JS, Lammertse DP.. Recent Trends in mortality and causes of death among persons with spinal cord injury. Arch Phys Med Rehabil . 1999;80(11):1411–9. [DOI] [PubMed] [Google Scholar]
- 7.National Center for Health Statistics, Centers for Disease Control and Prevention . Leading causes of death. [cited 2019 August 5]. Available from https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm.
- 8.Krause JS, Saunders LL.. Do risk factors for mortality after spinal cord injury parallel those from the general USA population? Top Spinal Cord Inj Rehabil . 2012;18(2):113–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cao Y, Krause JS, DiPiro N.. Risk factors for mortality after spinal cord injury in the USA. Spinal Cord . 2013;51(5):413–8. [DOI] [PubMed] [Google Scholar]
- 10.Krause JS, Saunders LL, DiPiro ND, Reed KS.. Theoretical risk and prevention model for secondary health conditions and mortality after SCI: 15 years of research. Top Spinal Cord Inj Rehabil . 2013;19(1):15–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krause JS, Zhai Y, Saunders LL, Carter RE.. Risk of mortality after spinal cord injury: an 8-year prospective study. Arch Phys Med Rehabil . 2009;90(10):1708–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McGrath R, Hall O, Peterson M, DeVivo M, Heinemann A, Kalpakjian C.. The association between the etiology of a spinal cord injury and time to mortality in the United States: A 44-year investigation. J Spinal Cord Med . 2019;42(4):444–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Selvarajah S, Hammond ER, Haider AH, Abularrage CJ, Becker D, Dhiman N, et al. The burden of acute traumatic spinal cord injury among adults in the United States: an update. J Neurotrauma . 2014;31(3):228–38. [DOI] [PubMed] [Google Scholar]
- 14.Varma A HE, Nicholas J, Selassie A.. Predictors of early mortality after traumatic spinal cord injury: a population-based study. Spine . 2010;35(7):778–83. [DOI] [PubMed] [Google Scholar]
- 15.Chen Y, DeVivo MJ.. Epidemiology of spinal cord injury. In: Kirshblum S, Lin VW, (eds.) Spinal Cord Medicine. 3rd ed. New York: Demos Medical; 2018. p. 44–62. [Google Scholar]
- 16.Flegal KM, Kit BK, Orpana H, Graubard BI.. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309:71–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berrington de Gonzalez A, Hartge P, Cerhan JR, Flint AJ, Hannan L, Maclnnis RJ, et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med . 2010;363(23):2211–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Flegal KM, Kit BK, Graubard BI.. Body mass index categories in observational studies of weight and risk of death. Am J Epidemiol . 2014;180(3):288–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee DH, Giovannucci EL.. Body composition and mortality in the general population: a review of epidemiologic studies. Exp Biol Med (Maywood) . 2018;243(17–18):1275–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Prospective Studies Collaboration . Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373(9669):1083–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Flegal KM, Kit BK, Graubard BI.. Bias in hazard ratios arising from misclassification according to self-reported weight and height in observational studies of body mass index and mortality. Am J Epidemiol . 2018;187(1):125–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Flegal KM GB, Williamson DF, Gail MH.. Cause-specific excess deaths associated with underweight, overweight, and obesity. JAMA . 2007;298(17):2028–37. [DOI] [PubMed] [Google Scholar]
- 23.Flegal KM, Graubard BI, Williamson DF, Gail MH.. Excess deaths associated with underweight, overweight, and obesity. JAMA . 2005;293(15):1861–7. [DOI] [PubMed] [Google Scholar]
- 24.Yu E, Ley SH, Manson JE, Willet W, Satija A, Hu B, et al. Weight history and all-cause and cause-specific mortality in three prospective cohort studies. Ann Intern Med. 2017;166(9):613–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rajan S, McNeely MJ, Goldstein B, Weaver F.. Association between obesity and diabetes mellitus in veterans with spinal cord injuries and disorders. Am J Phys Med Rehabil. 2010;89(5):353–61. [DOI] [PubMed] [Google Scholar]
- 26.Weaver FM, Collins EG, Kurichi J, Miskevics S, Smith B, Rajan S, et al. Prevalence of obesity and high blood pressure in veterans with spinal cord injuries and disorders. Am J Phys Med Rehabil . 2007;86(1):22–9. [DOI] [PubMed] [Google Scholar]
- 27.Gater DR Jr, Farkas GJ, Berg AS, Castillo C.. Prevalence of metabolic syndrome in veterans with spinal cord injury. J Spinal Cord Med . 2019;42(1):86-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen Y, Cao Y, Allen V, Richards JS.. Weight matters: physical and psychosocial well being of persons with spinal cord injury in relation to body mass index. Arch Phys Med Rehabil . 2011;92(3):391–8. [DOI] [PubMed] [Google Scholar]
- 29.Tian W, Hsieh CH, DeJong G, Backus D, Groah S, Ballard PH.. Role of body weight in therapy participation and rehabilitation outcomes among individuals with traumatic spinal cord injury. Arch Phys Med Rehabil . 2013;94(4 Suppl):S125–36. [DOI] [PubMed] [Google Scholar]
- 30.Stenson KW, Deutsch A, Heinemann AW, Chen D.. Obesity and inpatient rehabilitation outcomes for patients with a traumatic spinal cord injury. Arch Phys Med Rehabil . 2011;92(3):384–90. [DOI] [PubMed] [Google Scholar]
- 31.Cragg JJ, Noonan VK, Dvorak M, Krassioukov A, Mancini GB, Borisoff JF.. Spinal cord injury and type 2 diabetes: results from a population health survey. Neurology . 2013;81(21):1864–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cragg JJ, Noonan VK, Krassioukov A, Borisoff J.. Cardiovascular disease and spinal cord injury: results from a national population health survey. Neurology. 2013;81(8):723–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen Y, DeVivo MJ, Richards JS, SanAgustin TB.. Spinal cord injury model systems: review of Program and National Database from 1970 to 2015. Arch Phys Med Rehabil . 2016;97(10):1797–804. [DOI] [PubMed] [Google Scholar]
- 34.DeVivo MJ, Stover SL, Black KJ.. Prognostic factors for 12-year survival after spinal cord injury. Arch Phys Med Rehabil . 1992;73(2):156–2. [PubMed] [Google Scholar]
- 35.Instructions for classifying the underlying cause of death. 2017. [cited 2019 April 19]. Available from https://www.cdc.gov/nchs/data/dvs/2a_2017.pdf.
- 36.U.S. Department of Health and Human Services, National Institutes of Health, National Heart, Lung and Blood Institute . Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report (NIH Publication No. 98-4083). 1998. [cited 2019 April 19]. Available from http://www.nhlbi.nih.gov/guidelines/obesity/ob_gdlns.pdf.
- 37.Biering-Sorensen F, DeVivo MJ, Charlifue S, Chen Y, New PW, Noonan V, et al. International Spinal Cord Injury Core Data Set (version 2.0)-including standardization of reporting. Spinal Cord . 2017;55(8):759–64. [DOI] [PubMed] [Google Scholar]
- 38.Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, Johansen M, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med . 2011;34(6):535–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Allison PD. Survival Analysis Using the SAS System: A Practical Guide. Gary, NC: SAS Institute Inc.; 1995. p. 292. [Google Scholar]
- 40.Cao Y, DiPiro N, Krause JS.. Health factors and spinal cord injury: a prospective study of risk of cause-specific mortality. Spinal Cord . 2019;57(7):594–602. [DOI] [PubMed] [Google Scholar]
- 41.Krause JS, Cao Y, DeVivo MJ, DiPiro ND.. Risk and protective factors for cause-specific mortality after spinal cord injury. Arch Phys Med Rehabil . 2016;97(10):1669–78. [DOI] [PubMed] [Google Scholar]
- 42.Yamauchi T, Kamon J, Minokoshi Y, Ito Y, Waki H, Uchida S, et al. Adiponectin stimulates glucose utilization and fatty-acid oxidation by activating AMP-activated protein kinase. Nat Med . 2002;8(11):1288–95. [DOI] [PubMed] [Google Scholar]
- 43.Nigro E, Scudiero O, Monaco ML, Palmieri A, Mazzarella G, Costagliola C, et al. New insight into adiponectin role in obesity and obesity-related diseases. Biomed Res Int . 2014;2014:658913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Charlifue S, Tate D, Biering-Sorensen F, Burns S, Chen Y, Chun S, et al. Harmonization of databases: a step for advancing the knowledge about spinal cord injury. Arch Phys Med Rehabil . 2016;97(10):1805–18. [DOI] [PubMed] [Google Scholar]
- 45.Karastergiou K, Mohamed-Ali V.. The autocrine and paracrine roles of adipokines. Mol Cell Endocrinol . 2010;318(1–2):69–78. [DOI] [PubMed] [Google Scholar]
- 46.Farkas GJ, Gater DR.. Neurogenic obesity and systemic inflammation following spinal cord injury: a review. J Spinal Cord Med . 2018;41(4):378–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Garcia-Arguello LY, O'Horo JC, Farrell A, Blakney R, Sohail MR, Evans CT, et al. Infections in the spinal cord-injured population: a systematic review. Spinal Cord . 2017;55(6):526–34. [DOI] [PubMed] [Google Scholar]
- 48.Togan T, Azap OK, Durukan E, Arslan H.. The prevalence, etiologic agents and risk factors for urinary tract infection among spinal cord injury patients. Jundishapur J Microbiol . 2014;7(1):e8905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chen Y, Devivo MJ, Jackson AB.. Pressure ulcer prevalence in people with spinal cord injury: age-period-duration effects. Arch Phys Med Rehabil . 2005;86(6):1208–13. [DOI] [PubMed] [Google Scholar]
- 50.Cowan LJ, Ahn H, Flores M, Yarrow J, Barks LS, Garvan C, et al. Pressure ulcer prevalence by level of paralysis in patients with spinal cord injury in long-term care. Adv Skin Wound Care. 2019;32(3):122–30. [DOI] [PubMed] [Google Scholar]
- 51.Stillman MD, Barber J, Burns S, Williams S, Hoffman JM.. Complications of spinal cord injury over the first year after discharge from inpatient rehabilitation. Arch Phys Med Rehabil . 2017;98(9):1800–5. [DOI] [PubMed] [Google Scholar]
- 52.Dobner J, Kaser S.. Body mass index and the risk of infection – from underweight to obesity. Clin Microbiol Infect . 2018;24(1):24–8. [DOI] [PubMed] [Google Scholar]
- 53.National Spinal Cord Injury Statistical Center . Facts and Figures at a Glance. Birmingham, AL: University of Alabama at Birmingham. 2019. [cited 2019 April 19]. Available from https://www.nscisc.uab.edu/Public/Facts%20and%20Figures%202019%20-%20Final.pdf. [Google Scholar]
- 54.Kim J, Kraft P, Hagan KA, Harrington LB, Lindstroem S, Kabrhel C.. Interaction of a genetic risk score with physical activity, physical inactivity, and body mass index in relation to venous thromboembolism risk. Genet Epidemiol . 2018;42(4):354–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Severinsen MT, Kristensen SR, Johnsen SP, Dethlefsen C, Tjonneland A, Overvad K.. Anthropometry, body fat, and venous thromboembolism: a Danish follow-up study. Circulation . 2009;120(19):1850–7. [DOI] [PubMed] [Google Scholar]
- 56.Stokes A. Using maximum weight to redefine body mass index categories in studies of the mortality risks of obesity. Popul Health Metr. 2014;12(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Howell CR, Fontaine K, Ejima K, Ness KK, Cherrington A, Mehta T.. Maximum lifetime body mass index and mortality in Mexican American adults: the National Health and Nutrition Examination Survey III (1988-1994) and NHANES 1999-2010. Prev Chronic Dis . 2017;14:E67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Stokes A, Preston SH.. Revealing the burden of obesity using weight histories. Proc Natl Acad Sci USA . 2016;113(3):572–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wen H, Chen Y, He Y, Bickel CS, Robinson-Whelen S, Heinemann AW.. Racial differences in weight gain: a 5-year longitudinal study of persons with spinal cord injury. Arch Phys Med Rehabil . 2018;99(10):1957–64. [DOI] [PubMed] [Google Scholar]
- 60.Powell D, Affuso O, Chen Y.. Weight change after spinal cord injury. J Spinal Cord Med . 2017;40(2):130–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Crane DA, Little JW, Burns SP.. Weight gain following spinal cord injury: a pilot study. J Spinal Cord Med . 2011;34(2):227–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.de Groot S, Post MW, Postma K, Sluis TA, van der Woude LH.. Prospective analysis of body mass index during and up to 5 years after discharge from inpatient spinal cord injury rehabilitation. J Rehabil Med . 2010;42(10):922–8. [DOI] [PubMed] [Google Scholar]
- 63.Hatchett PE, Mulroy SJ, Eberly VJ, Haubert LL, Requejo PS.. Body mass index changes over 3 years and effect of obesity on community mobility for persons with chronic spinal cord injury. J Spinal Cord Med . 2016;39(4):421–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Krause JS, Saunders LL.. Socioeconomic and behavioral risk factors for mortality: do risk factors observed after spinal cord injury parallel those from the general USA population? Spinal Cord . 2012;50(8):609–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Isasi CR, Ayala GX, Sotres-Alvarez D, Madanat H, Penedo F, Loria CM, et al. Is acculturation related to obesity in Hispanic/Latino adults? Results from the Hispanic community health study/study of Latinos. J Obes . 2015;2015:186276. [DOI] [PMC free article] [PubMed] [Google Scholar]