Abstract
Objectives:
To investigate the incidence of and contributing factors to open gingival embrasures between the central incisors after orthodontic treatment.
Materials and Methods:
One hundred posttreatment patients (29 men and 71 women; mean age, 24.7 years) were divided retrospectively into occurrence and nonoccurrence groups based on intraoral photographs. Based on the severity, the occurrence group was further divided into mild, moderate, and severe groups. Parameters from periapical radiographs, superimposed lateral cephalograms, and study models were compared between the occurrence and the nonoccurrence groups by using independent t-tests and were also analyzed on the basis of severity via analysis of variance. Logistic regression analysis was performed to identify the contributing factors to open gingival embrasures.
Results:
The incidence of open gingival embrasures between the central incisors was 22% and 36% in the maxilla and the mandible, respectively. Lingual movement of the incisors, distance from the contact point to the alveolar crest after treatment, antero-posterior overlap of the two central incisors before treatment in the maxilla, and distance from the contact point to the alveolar crest after treatment in the mandible were significantly associated with the occurrence of open gingival embrasures (P < .05). In the mandible, the amount of intrusion was significantly related to severity (P < .05).
Conclusions:
The incidence of open gingival embrasures following orthodontic tooth movement is high. Therefore, attention should be paid to the contributing factors to prevent or reduce the occurrence of open gingival embrasures.
Keywords: Open gingival embrasure, Black triangle, Orthodontic treatment
INTRODUCTION
Open gingival embrasures, also known as “black triangles,” refer to empty space below the interproximal contact when the space is not filled with gingiva.1,2 They cause not only esthetic but also periodontal problems related to chronic food retention.1 Despite the high esthetic demands of adult orthodontic patients, previous studies reported a relatively high incidence of 38 to 43.7% of open gingival embrasures.1–4 Several causes, such as stretching of the interdental transseptal gingival fibers during orthodontic treatment, have been suggested.1,3 In addition, other factors, including periodontal response, tooth form, amount of crowding, alveolar bone height, angle formed between the roots of adjacent teeth, and age, could contribute to open gingival embrasures.1 Open gingival embrasures are most commonly located between the maxillary central incisors.5 Stripping or root axis control can be used for treatment.3 Hyaluronic acid filler has been shown to be able to fill open gingival embrasures in an in vivo model.6
Most previous studies have not taken the complex implications of tooth movement into consideration when evaluating open gingival embrasures. Recent studies have reported that the movement of teeth during orthodontic treatment could also affect the occurrence of open gingival embrasures.7–9 Unfortunately, in these studies, the occurrence was investigated only with consideration of the parameters of tooth movement and not in combination with other predisposing factors such as crowding, alveolar bone height, position of the contact point, tooth shape, and others.
Therefore, the purpose of this study was to determine the incidence of open gingival embrasures after orthodontic treatment and to examine the predisposing factors in combination with orthodontic treatment.
MATERIALS AND METHODS
Subjects
Subjects were selected retrospectively from a pool of patients who completed comprehensive orthodontic treatment between July 2010 and May 2011 in the Department of Orthodontics, Gangnam Severance Dental Hospital. The inclusion criteria were as follows: presence of before (T1) and after (T2) treatment records including frontal intraoral photographs, lateral cephalograms, periapical radiographs taken with a 4-mm metal bead, and study models. Of 320 patients, 100 subjects were selected (29 men and 71 women; mean age, 24.7 ± 7.6 years) based on the following exclusion criteria: disagreement of classification by four examiners, absence of the central incisor, periodontal disease, history of previous orthodontic treatment, open gingival embrasures or restorations between the central incisors before treatment, stripping of the central incisors during treatment, and frontal photographs that were distorted or contained foreign substances, such as saliva and food debris. The mean treatment duration was 23.6 ± 10.7 months, and prophylaxis and oral hygiene instructions were given regularly during treatment. This study was approved by the Institutional Review Board of Gangnam Severance Hospital (No. 3-2014-0125). Because of the retrospective nature of this study, the institutional review board waived the requirement for written informed patient consent.
Classification of Open Gingival Embrasures According to Severity
Frontal intraoral photographs taken before and 1 week after orthodontic treatment were examined to determine the presence and severity of open gingival embrasures between the maxillary and mandibular central incisors. The interdental papilla area was divided into four regions according to the Jemt index (Figure 1).10 The subjects were divided into nonoccurrence and occurrence groups; the occurrence group was further subdivided into mild, moderate, and severe groups. Two orthodontists and two periodontists independently classified the subjects, and 22 subjects were excluded because of disagreement.
Figure 1.
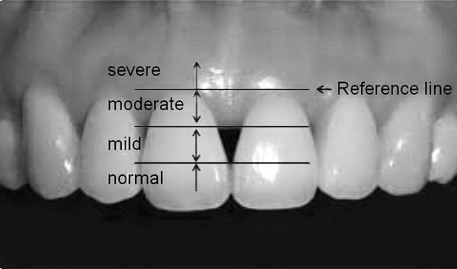
Classification of open gingival embrasures according to severity.10 Two lines parallel to the reference line (tangent line to the highest gingival curvature of the crown) were constructed: a line passing through the most cervical contact point and a line bisecting the distance between the reference line and the contact point line. According to the position of the incisive papilla tip in the four areas constructed by the three parallel lines, the severity of the groups (normal, mild, moderate, and severe) was determined.
Measurements of Tooth Movement on Lateral Cephalograms
After superimposition of lateral cephalograms before and after treatment by the “best fit” method, the amount of vertical and horizontal movement of the maxillary and mandibular incisal tips was measured parallel and perpendicular to the Sella-Nasion (SN) and mandibular planes, respectively (Figure 2). Changes in the maxillary and mandibular incisor inclination relative to the SN and mandibular planes were also measured by subtracting the T1 measurements from the T2 measurements.
Figure 2.
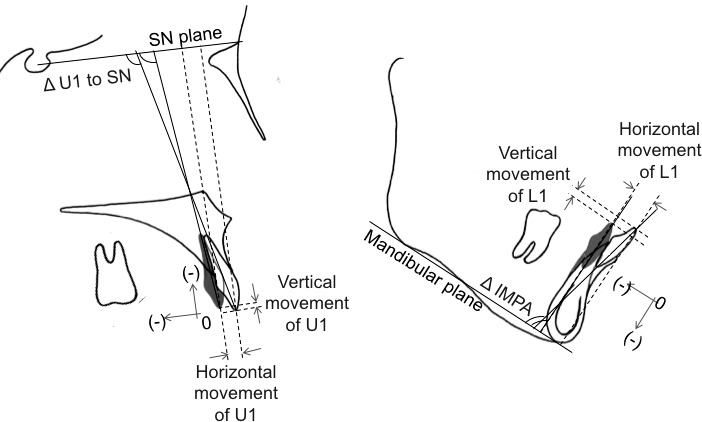
Superimposition of lateral cephalograms shows measurements of tooth movement. SN indicates Sella-Nasion; U1, the maxillary central incisor; L1, the mandibular central incisor; IMPA, incisor mandibular plane angle. Positive values denote extrusive and labial movements, while negative values denote intrusive and lingual movements. Δ U1 to SN and Δ IMPA refer to the changes in measurements between before (T1) and after (T2) treatment (Δ = T2 – T1).
Measurements of Tooth Shape, Tooth Axis, and Alveolar Crest on Periapical Radiographs
To measure the lengths and angulations of the teeth, the ImageJ program (National Institutes of Health, Bethesda, MD) was used. In terms of the magnification error, a metal bead 4 mm in diameter was attached to periapical films to confirm and adjust the radiographic images.
The tooth shape of the central incisor was determined by calculating the ratio of the perpendicular distance from the mesial cementoenamel junction (CEJ) and the interproximal contact point (ICP) to the tooth long axis, which was defined as the crown ratio (Figure 3).11 The most gingival point of the interproximal contact surface between the central incisors was defined as the ICP, and the left central incisor was used for measurement of the crown ratio. The measurement was performed at T2, because no change was expected during treatment and the measurement would be difficult to record in the presence of crowding. The angle between the long axes of the adjacent central incisors was measured and defined as the root angulation. The distance between the mesial CEJs of two central incisors at T2 was also measured. The distance from the ICP to the alveolar bone crest (ABC) was measured at TI and T2, and the change in this distance during treatment (Δ = T2 − T1) was calculated. The ABC was defined as the most coronal area where the periodontal ligament space retained its normal width.12
Figure 3.
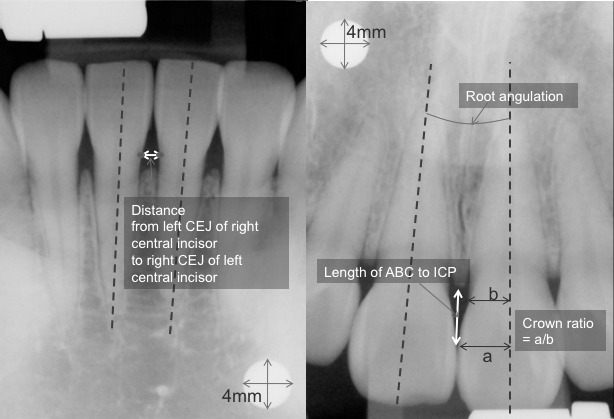
Periapical radiographic measurements. CEJ indicates cementoenamel junction; ABC, alveolar bone crest; ICP, interproximal contact point; a, perpendicular distance from the mesial ICP to the tooth long axis; b, perpendicular distance from the mesial CEJ to the tooth long axis.
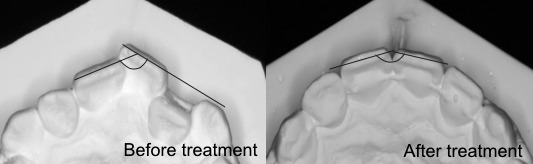
Measurements of Crowding on Study Models
The antero-posterior (A-P) and transverse distances and the angle between the two incisal edges were measured on occlusal photographs taken of the maxillary and mandibular study models before and after treatment. The midpalatal raphe in the maxilla and the perpendicular bisector to the line connecting the mesial surfaces of the first molars in the mandible were used as reference lines. The A-P and transverse overlap between the most mesial points of the two incisal edges were measured parallel and perpendicular to the reference lines, respectively (Figure 4). Rotation was defined as the angle between the two incisal edges (Figure 5).
Figure 4.
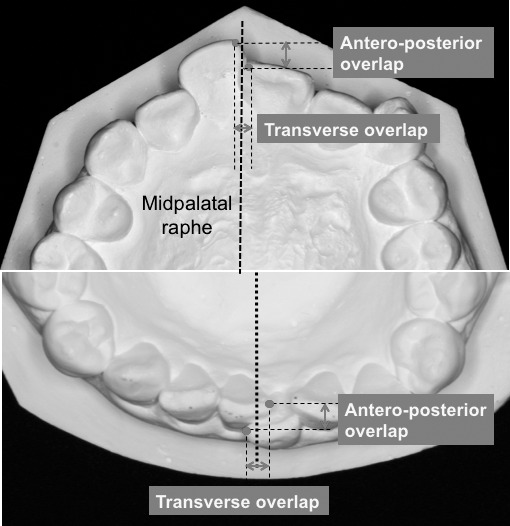
Measurements of the antero-posterior and transverse overlap of the two central incisors.
Figure 5.
Measurement of the angle formed by the incisal edges of the two central incisors.
Statistical Analysis
The SAS program (version 9.1.3, SAS Institute Inc, Cary, NC) was used for statistical analysis, and the level of significance was set at P < .05. One examiner performed all measurements and repeated the measurements on 20 randomly selected patients at 2-week intervals. The intraclass correlation coefficient was >.908, indicating high reliability.
The incidence of open gingival embrasures was calculated, and the difference in incidence between men and women was analyzed by the chi-square test. An independent t-test was used to make comparisons between the occurrence and nonoccurrence groups. Analysis of variance was used to make comparisons among the different severity groups.
Logistic regression analysis was used to identify associations among multiple variables. Only statistically significant variables found through simple ordinary logistic regression were reanalyzed by multiple ordinary logistic regression. The odds ratio was calculated using the beta coefficient, which was measured using the multiple ordinary logistic regression analysis.
RESULTS
The incidence of open gingival embrasures after orthodontic treatment was 22% between the maxillary central incisors and 36% between the mandibular central incisors (Table 1). In the maxilla, moderate and severe groups were not observed, while in the mandible, the severe group was not observed. Gender was not significantly associated with the occurrence of open gingival embrasures (P > .05; Table 2).
Table 1.
Incidence of Open Gingival Embrasure Spaces
| Nonoccurrence |
Occurrence |
|||
| Mild |
Moderate |
Severe |
||
| Maxilla (n = 100) | 78 | 22 | 0 | 0 |
| Mandible (n = 100) | 64 | 23 | 13 | 0 |
Table 2.
Comparison Between Men and Women in the Occurrence Groupa
| Men (n = 29) |
Women (n = 71) |
Significance |
|
| Maxilla (n = 22) | 7 | 15 | NS |
| Mandible (n = 36) | 9 | 27 | NS |
NS indicates not significant. Chi-square test was used to compare the incidence between male and female.
Table 3 shows comparisons between the occurrence and nonoccurrence groups. In the maxilla, the amount of lingual movement of the incisors, distance between the ABC and ICP after treatment, and A-P overlap were significantly greater in the occurrence group than in the nonoccurrence group (P < .05). In the mandible, the lingual tipping of the incisors, amount of intrusion, distance from the ABC to the ICP before and after treatment, and changes in the distance during treatment were significantly greater in the occurrence group than in the nonoccurrence group. In addition, the crown shape was more triangular in the occurrence group (P < .05). When evaluating open gingival embrasures according to severity in the mandible (Table 4), only the amount of incisor intrusion was significantly smaller in the mild group than in the moderate group (P < .05).
Table 3.
Comparison of Open Gingival Embrasure Spaces Between the Nonoccurrence and Occurrence Groups in the Maxilla and Mandiblea
| Measurement |
Maxilla |
Mandible |
||||
| Nonoccurrence | Occurrence | Significance |
Nonoccurrence | Occurrence | Significance |
|
| (n = 78) |
(n = 22) |
(n = 64) |
(n = 36) |
|||
| Treatment duration, mo | 23.10 ± 2.00 | 28.12 ± 2.31 | NS | 24.67 ± 3.51 | 24.10 ± 1.41 | NS |
| Age, y | 23.91 ± 7.30 | 27.77 ± 8.63 | NS | 23.97 ± 6.04 | 26.17 ± 10.07 | NS |
| Δ U1 to SN/Δ IMPA, ° | −6.60 ± 9.33 | −10.45 ± 9.43 | NS | −2.21 ± 6.29 | −6.75 ± 6.43 | * |
| Horizontal movement of U1/L1, mm | −2.74 ± 3.70 | −4.94 ± 3.80 | * | −2.18 ± 3.60 | −3.51 ± 3.11 | NS |
| Vertical movement of U1/L1, mm | −0.29 ± 1.66 | −0.80 ± 1.97 | NS | −0.37 ± 2.66 | −1.66 ± 1.84 | * |
| Crown ratio (tooth shape) | 1.24 ± 0.12 | 1.28 ± 0.10 | NS | 1.25 ± 0.14 | 1.33 ± 0.09 | * |
| Root angulation at T2, ° | −2.21 ± 6.12 | −3.55 ± 6.03 | NS | −2.26 ± 4.63 | −2.71 ± 5.19 | NS |
| Right CEJ–left CEJ distance at T2, mm | 1.60 ± 0.49 | 1.70 ± 0.40 | NS | 1.45 ± 0.36 | 1.59 ± 0.43 | NS |
| Distance from ICP to ABC at T1, mm | 4.67 ± 0.80 | 5.04 ± 0.91 | NS | 4.42 ± 0.63 | 4.90 ± 0.87 | * |
| Distance from ICP to ABC at T2, mm | 5.06 ± 0.79 | 5.51 ± 0.95 | * | 4.97 ± 0.53 | 5.85 ± 1.05 | *** |
| Δ Distance from ICP to ABC, mm | −0.39 ± 0.61 | −0.47 ± 0.84 | NS | −0.56 ± 0.49 | −0.95 ± 1.03 | * |
| Crowding | ||||||
| A-P overlapped distance, mm | 0.55 ± 0.66 | 0.91 ± 0.71 | * | 0.30 ± 0.58 | 0.31 ± 0.50 | NS |
| Transverse overlapped distance, mm | 0.21 ± 0.09 | 0.21 ± 0.78 | NS | 0.38 ± 0.43 | 0.63 ± 0.88 | NS |
| Rotation, ° | 8.43 ± 6.00 | 9.23 ± 8.53 | NS | 10.96 ± 4.97 | 10.25 ± 7.47 | NS |
Independent t-tests were used to compare between the nonoccurrence and occurrence groups, and Bonferroni correction was performed. Regarding root angulation, a negative value indicates that the two roots diverge apically.
NS indicates not significant; U1, maxillary incisor; L1, mandibular incisor; SN, Sella-Nasion; IMPA, incisor mandibular plane angle; T1, before treatment; T2, after treatment; Δ, T2-T1; CEJ, cementoenamel junction; ICP, interproximal contact point; ABC, alveolar bone crest; A-P, antero-posterior.
P < .05; *** P < .001.
Table 4.
Comparison Between the Mild and Moderate Groups in the Mandiblea
| Measurement |
Mild (n = 23) |
Moderate (n = 13) |
Significance |
| Duration, mo | 23.15 ± 2.94 | 24.49 ± 4.60 | NS |
| Age, y | 26.85 ± 11.04 | 24.96 ± 8.33 | NS |
| Δ IMPA, ° | −6.45 ± 7.13 | −7.28 ± 5.21 | NS |
| Horizontal movement of L1, mm | −3.19 ± 3.14 | −4.05 ± 3.11 | NS |
| Vertical movement of L1, mm | −1.03 ± 1.94 | −2.76 ± 0.95 | * |
| Crown ratio (tooth shape) | 1.32 ± 0.09 | 1.34 ± 0.08 | NS |
| Root angulation at T2, ° | −2.69 ± 5.55 | −2.76 ± 4.68 | NS |
| Right CEJ–left CEJ distance at T2, mm | 1.49 ± 0.34 | 1.75 ± 0.53 | NS |
| Distance from ICP to ABC at T1, mm | 4.89 ± 0.69 | 4.93 ± 1.14 | NS |
| Distance from ICP to ABC at T2, mm | 5.60 ± 0.91 | 6.30 ± 1.16 | NS |
| Δ Distance from ICP to ABC, mm | −0.72 ± 0.98 | −1.37 ± 1.04 | NS |
| Crowding | |||
| A-P overlapped distance. mm | 0.31 ± 0.50 | 0.29 ± 0.51 | NS |
| Transverse overlapped distance, mm | 0.49 ± 0.74 | 0.87 ± 1.00 | NS |
| Rotation, ° | 10.36 ± 7.49 | 10.00 ± 7.73 | NS |
Independent t-tests were used to compare between the mild and moderate groups, and Bonferroni correction was performed. Regarding root angulation, a negative value indicates that the two roots diverge apically. NS indicates not significant; IMPA, incisor mandibular plane angle; L1, mandibular incisor; T1, before treatment; T2, after treatment; Δ, T2-T1; CEJ, cementoenamel junction; ICP, interproximal contact point; ABC, alveolar bone crest; A-P, antero-posterior.
P < .05.
Using simple regression analysis, the following measurements were found to be significant contributing factors in the maxilla: age, horizontal movement of the incisor, distance from the ABC to the ICP after treatment, and A-P overlap between the incisors. In the mandible, the following were significant contributing factors: the change in incisor to mandibular plane angle, vertical movement of the incisor, distance from the ABC to the ICP before and after treatment, changes in the distance during treatment, and crown ratio (Table 5).
Table 5.
Relationship Between Severity of Open Gingival Embrasure and Parameters Related to Treatment by Simple Ordinary Logistic Regression Analysis
| Maxilla |
Mandible |
|||||
| B |
SE |
Significance |
B |
SE |
Significance |
|
| Duration, mo | 0.001 | 0.001 | NS | 0.001 | 0.001 | NS |
| Age, y | 0.058 | 0.029 | * | 0.036 | 0.027 | NS |
| Δ U1 to SN/Δ IMPA, ° | −0.043 | 0.026 | NS | −0.110 | 0.350 | * |
| Horizontal movement of U1/L1, mm | −0.153 | 0.066 | * | −0.110 | 0.061 | NS |
| Vertical movement of U1/L1, mm | 0.170 | 0.141 | NS | −0.224 | 0.091 | * |
| Crown ratio | 3.435 | 2.089 | NS | 4.886 | 1.725 | * |
| Root angulation at T2, ° | −0.037 | 0.040 | NS | −0.020 | 0.043 | NS |
| Right CEJ–left CEJ distance at T2, mm | 0.528 | 0.514 | NS | 0.853 | 0.549 | NS |
| Distance from ICP to ABC at T1, mm | 0.545 | 0.301 | NS | 0.883 | 0.302 | * |
| Distance from ICP to ABC at T2, mm | 0.610 | 0.284 | * | 1.442 | 0.354 | ** |
| Δ Distance from ICP to ABC, mm | −0.179 | 0.353 | NS | −0.741 | 0.314 | * |
| Crowding | ||||||
| A-P overlapped distance, mm | 0.702 | 0.334 | * | 0.008 | 0.380 | NS |
| Transverse overlapped distance, mm | 0.004 | 0.248 | NS | 0.591 | 0.332 | NS |
| Rotation, ° | 0.018 | 0.035 | NS | −0.021 | 0.036 | NS |
B indicates beta coefficient; SE, standard error; NS, not significant; U1, maxillary incisor; L1, mandibular incisor; SN, Sella-Nasion; IMPA, incisor mandibular plane angle; T1, before treatment; T2, after treatment; Δ, T2-T1; CEJ, cementoenamel junction; ICP, inteproximal contact point; ABC, alveolar bone crest; A-P, antero-posterior.
P < .05.
A multiple regression analysis showed that in the maxilla, the lingual movement of the incisor, distance from the ABC to the ICP after treatment, and the A-P overlap were significantly related to the occurrence of open gingival embrasures (P < .05), while only the distance from the ABC to the ICP after treatment was significantly related in the mandible (P < .05; Table 6).
Table 6.
Main Contributing Factors to Open Gingival Embrasure Spaces by Multiple Ordinary Logistic Regression Analysisa
| B |
SE |
Significance |
OR |
|
| Maxilla | ||||
| Age, y | 0.064 | 0.033 | NS | 1.066 |
| Horizontal movement of U1, mm | −0.169 | 0.072 | * | 0.845 |
| Distance from ICP to ABC at T2, mm | 0.693 | 0.331 | * | 1.999 |
| A-P overlapped distance, mm | 0.791 | 0.397 | * | 2.206 |
| Mandible | ||||
| Δ IMPA, ° | −0.073 | 0.039 | NS | 0.93 |
| Vertical movement of L1, mm | −0.111 | 0.106 | NS | 0.89 |
| Distance from ICP to ABC at T1, mm | 0.189 | 0.410 | NS | 1.21 |
| Distance from ICP to ABC at T2, mm | 1.133 | 0.457 | * | 3.10 |
| Δ Distance from ICP to ABC, mm | 0.907 | 0.610 | NS | 2.48 |
| Crown ratio | 3.127 | 1.937 | NS | 22.81 |
Multiple ordinary logistic regression analysis was used. B indicates beta coefficient; SE, standard error; OR, odds ratio; NS, not significant; U1, maxillary incisor; ICP, inteproximal contact point; ABC, alveolar bone crest; T1, before treatment; T2, after treatment; Δ, T2-T1; A-P, antero-posterior; IMPA, incisor mandibular plane angle; L1, mandibular incisor.
P < .05.
DISCUSSION
In this study, the incidence of open gingival embrasures following orthodontic treatment was 22%–36%. Gender, treatment duration, and age were not significantly associated with the occurrence of open gingival embrasures. Reports on the relationship between age and the occurrence of open gingival embrasures remain inconsistent, with some studies reporting age as a contributing factor,9,13,14 while others do not.15,16 This difference may be a result of the varying inclusion/exclusion criteria between studies. As patients with periodontitis were excluded from this study, the effect of age might have been underestimated.
Reports on the effect of initial crowding on the occurrence of open gingival embrasures is also inconsistent.1,3,8 Stretching of the gingival fibers or a decrease of gingival thickness during tooth alignment can influence the occurrence.3,8 The possibility of open gingival embrasures increases when the arch length discrepancy is larger than 4 mm,8 while there is a report that crowding was not a significant contributing factor.1 In the present study, A-P overlap was the only contributing factor among the variables related to crowding. The odds ratio was 2.2, indicating that the occurrence of open gingival embrasures increases by 2.2 times when the A-P overlap increases by 1 mm. In terms of transverse overlap, the effect of crowding may have been underestimated. As the most mesial point of the incisal edge, which is usually away from the contact surface, was used to measure crowding, the measured transverse overlap may have been less than the actual overlap, as seen in Figure 4.
Orthodontic tooth movement is another factor that may cause open gingival embrasures.7,8 In previous studies, only nonextraction patients were included,8 or other contributing factors such as age, tooth shape, and alveolar bone crest were not considered.7,8 To overcome these limitations, this study included extraction and nonextraction patients and analyzed various other factors in combination, including tooth movement. Among multiplanar orthodontic movements, the multiple logistic regression analysis revealed that only lingual movement of the maxillary incisors was a significant factor (P < .05). The odds ratio for lingual movement was 0.845, meaning that for every 1 mm of lingual movement of the maxillary central incisor, the risk for open gingival embrasures increases by 1.18 times. Labial movement was also previously reported to increase the occurrence of open gingival embrasures,8 because gingival recession could occur easily as the height of the marginal gingiva lowers and thins with labial orthodontic movement.17 In this study, only 19 subjects exhibited labial movement of the maxillary incisors, which was 1.58 mm on average. Most of these subjects belonged to the nonoccurrence group, with only one showing a moderate open gingival embrasure. Therefore, the insignificant relationship between open gingival embrasures and labial movement may be a result of the small amount of labial movement in the subjects involved in the current study.
According to multiple regression analysis, the distance between the ABC and ICP after orthodontic treatment had a significant effect on the occurrence of open gingival embrasures in the maxilla and mandible (P < .05). In this study, the average distance from the ABC to the ICP in the nonoccurrence group was 5.06 mm and 4.97 mm between the maxillary and mandibular central incisors, respectively, compared with 5.51 mm and 5.85 mm in the occurrence group. These results support a previous finding that open gingival embrasures are likely to occur if the distance from the ABC to the ICP is more than 5 mm.18 Lowering of the ABC during orthodontic treatment was reported in several studies: alveolar bone resorption was 0.29 mm on average in the maxillary anterior segment,19 alveolar bone support decreased by 2.24% on average,20 or a decrease of the interdental alveolar bone height was observed around at least one of the six anterior teeth, which occurred in 36% of orthodontic patients.12 Most subjects in this study showed a decrease in ABC height after treatment, with the exception of a minor increase in a couple of subjects. Therefore, orthodontic treatment can result in open gingival embrasures if the ABC undergoes resorption, causing an increase in the distance between the ABC and the ICP.
In the mandible, intrusive movement of the incisor seemed to cause open gingival embrasures. Although it was not a contributing factor according to the multiple regression analysis, the amount of intrusion was larger in the occurrence group than in the nonoccurrence group and larger in the moderate group than in the mild group (P < .05). When a tooth was intruded, the ABC position was affected by oral hygiene.21 On the mandibular anterior teeth, dental calculus is easily deposited, which may have an indirect effect during intrusion as well.21 Therefore, open gingival embrasures are likely to occur as the mandibular incisors are intruded, which calls for clinicians' attention.
The occurrence of open gingival embrasures was also influenced by embrasure morphology. Open gingival embrasures were observed in the long-wide, long-narrow, and short-wide group, indicating that a long distance from the ABC to the ICP plays a more important role than a wide interdental distance between the adjacent proximal CEJs in the occurrence of embrasures.22 Root angulation can also have an effect on open gingival embrasures,1 although the finding was not confirmed in the present study. This was possibly because most patients finished orthodontic treatment with parallel roots. Therefore, factors related to embrasure morphology, such as distance from the ABC to the ICP, tooth shape, distance between adjacent CEJs, and root angulation, need to be considered together.
Despite the esthetic importance of open gingival embrasures around the lateral incisors, this study focused on the central incisors because of distortion and poor reproducibility of the lateral areas in intraoral photographs. Additional studies that evaluate the thickness and biotype of the gingiva would be useful to investigate the cause of open gingival embrasures. Clinically, open gingival embrasures may be less noticeable if hidden by saliva. However, an understanding of the contributing factors and proper management can prevent or reduce the occurrence of open gingival embrasures in orthodontic patients.
CONCLUSIONS
The incidence of open gingival embrasures following orthodontic treatment was 22%–36%. Consideration should be given to the various contributing factors identified in this study to prevent or reduce the occurrence of open gingival embrasures after orthodontic treatment.
Lingual movement of the incisors, a large distance from the contact point to the alveolar crest after treatment, large A-P overlap between the two central incisors before treatment in the maxilla, and large distance from the contact point to the alveolar crest after treatment in the mandible can cause open gingival embrasures after orthodontic treatment.
A large amount of intrusion of the mandibular incisors can aggravate the severity of open gingival embrasures.
REFERENCES
- 1.Kurth JR, Kokich VG. Open gingival embrasures after orthodontic treatment in adults: prevalence and etiology. Am J Orthod Dentofacial Orthop. 2001;120:116–123. doi: 10.1067/mod.2001.114831. [DOI] [PubMed] [Google Scholar]
- 2.Tanaka OM, Furquim BD, Pascotto RC, Ribeiro GL, Bosio JA, Maruo H. The dilemma of the open gingival embrasure between maxillary central incisors. J Contemp Dent Pract. 2008;9:92–98. [PubMed] [Google Scholar]
- 3.Burke S, Burch JG, Tetz JA. Incidence and size of pretreatment overlap and posttreatment gingival embrasure space between maxillary central incisors. Am J Orthod Dentofacial Orthop. 1994;105:506–511. doi: 10.1016/S0889-5406(94)70013-3. [DOI] [PubMed] [Google Scholar]
- 4.Ko-Kimura N, Kimura-Hayashi M, Yamaguchi M, et al. Some factors associated with open gingival embrasures following orthodontic treatment. Aust Orthod J. 2003;19:19–24. [PubMed] [Google Scholar]
- 5.Hasanreisoglu U, Berksun S, Aras K, Arslan I. An analysis of maxillary anterior teeth: facial and dental proportions. J Prosthet Dent. 2005;94:530–538. doi: 10.1016/j.prosdent.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 6.Pi S, Choi YJ, Hwang S, et al. Local injection of hyaluronic acid filler improves open gingival embrasure: validation through a rat model. J Periodontol. 2017;88:1221–1230. doi: 10.1902/jop.2017.170101. [DOI] [PubMed] [Google Scholar]
- 7.Kozai Y, Tamaki Y, Nomura Y, Kaida K. The factors of open gingival embrasure space between central incisors after orthodontic treatment in adult patients. Orthodontic Waves. 2010;69:39. [Google Scholar]
- 8.Kandasamy S, Goonewardene M, Tennant M. Changes in interdental papillae heights following alignment of anterior teeth. Aust Orthod J. 2007;23:16–23. [PubMed] [Google Scholar]
- 9.Uribe F, Holliday B, Nanda R. Incidence of open gingival embrasures after mandibular incisor extractions: a clinical photographic evaluation. Am J Orthod Dentofacial Orthop. 2011;139:49–54. doi: 10.1016/j.ajodo.2009.03.049. [DOI] [PubMed] [Google Scholar]
- 10.Jemt T. Regeneration of gingival papillae after single-implant treatment. Int J Periodontics Restorative Dent. 1997;17:326–333. [PubMed] [Google Scholar]
- 11.Taylor RM. Variation in form of human teeth: I. An anthropologic and forensic study of maxillary incisors. J Dent Res. 1969;48:5–16. doi: 10.1177/00220345690480012501. [DOI] [PubMed] [Google Scholar]
- 12.Nelson PA, Artun J. Alveolar bone loss of maxillary anterior teeth in adult orthodontic patients. Am J Orthod Dentofacial Orthop. 1997;111:328–334. doi: 10.1016/s0889-5406(97)70192-6. [DOI] [PubMed] [Google Scholar]
- 13.Ikeda T, Yamaguchi M, Meguro D, Kasai K. Prediction and causes of open gingival embrasure spaces between the mandibular central incisors following orthodontic treatment. Aust Orthod J. 2004;20:87–92. [PubMed] [Google Scholar]
- 14.Prato GP, Rotundo R, Cortellini P, Tinti C, Azzi R. Interdental papilla management: a review and classification of the therapeutic approaches. Int J Periodontics Restorative Dent. 2004;24:246–255. [PubMed] [Google Scholar]
- 15.Sheridan JJ, Hastings J. Air-rotor stripping and lower incisor extraction treatment. J Clin Orthod. 1992;26:18–22. [PubMed] [Google Scholar]
- 16.Hugoson A, Norderyd O. Has the prevalence of periodontitis changed during the last 30 years? J Clin Periodontol. 2008;35:338–345. doi: 10.1111/j.1600-051X.2008.01279.x. [DOI] [PubMed] [Google Scholar]
- 17.Wennstrom JL. Mucogingival considerations in orthodontic treatment. Semin Orthod. 1996;2:46–54. doi: 10.1016/s1073-8746(96)80039-9. [DOI] [PubMed] [Google Scholar]
- 18.Tarnow DP, Magner AW, Fletcher P. The effect of the distance from the contact point to the crest of bone on the presence or absence of the interproximal dental papilla. J Periodontol. 1992;63:995–996. doi: 10.1902/jop.1992.63.12.995. [DOI] [PubMed] [Google Scholar]
- 19.Hamp SE, Lundstrom F, Nyman S. Periodontal conditions in adolescents subjected to multiband orthodontic treatment with controlled oral hygiene. Eur J Orthod. 1982;4:77–86. doi: 10.1093/ejo/4.2.77. [DOI] [PubMed] [Google Scholar]
- 20.Artun J, Urbye KS. The effect of orthodontic treatment on periodontal bone support in patients with advanced loss of marginal periodontium. Am J Orthod Dentofacial Orthop. 1988;93:143–148. doi: 10.1016/0889-5406(88)90292-2. [DOI] [PubMed] [Google Scholar]
- 21.Melsen B. Tissue reaction following application of extrusive and intrusive forces to teeth in adult monkeys. Am J Orthod. 1986;89:469–475. doi: 10.1016/0002-9416(86)90002-3. [DOI] [PubMed] [Google Scholar]
- 22.Chang LC. The association between embrasure morphology and central papilla recession: a noninvasive assessment method. Chang Gung Med J. 2007;30:445–452. [PubMed] [Google Scholar]


