Abstract
Objectives:
To compare the failure pattern of four different bracket types and to assess its effect on treatment duration.
Materials and Methods:
A total of 78 white patients (28 male, 50 female) with a mean age of 12.6 years were included in this retrospective cohort study and treated for a mean period of 30.6 months. The patients were treated in a private practice with stainless steel conventionally ligated brackets, ceramic conventionally ligated brackets, stainless steel self-ligating brackets, or nickel-free self-ligating brackets. The loss of at least one bracket during the course of treatment was analyzed with Cox proportional hazards survival analyses and generalized linear regression.
Results:
The overall bracket failure rate at the tooth level was 14.1% (217 brackets), with significant differences according to tooth type (between 8.0%–23.4%) and bracket type (between 11.2%–20.0%). After taking confounders into account, patients treated with ceramic brackets lost more brackets (hazard ratio = 1.62; 95% confidence interval = 1.14–2.29; P = .007) than patients with stainless steel brackets. On average, treatment time increased by 0.6 months (95% confidence interval = 0.21–1.05; P = .004) for each additional failed bracket.
Conclusions:
Bracket failure was more often observed with ceramic brackets and was associated with increased treatment duration.
Keywords: Bracket failure, Treatment duration, Treatment efficiency, Survival analysis, Clinical study
INTRODUCTION
Clinical efficiency and treatment duration in orthodontics can be compromised by bond failure.1–3 Indeed, bracket failure is ranked as one of the most important predictors of fixed appliance treatment duration, along with patient compliance, treatment variations such as office-related treatment approaches, multiple phases, extractions, appliance selection, and underlying malocclusions.1–3 An extension of treatment by 0.3 months for every bracket failure and up to 1.5 months for 3 or more failures has been reported, as the clinician may have to temporarily delay the originally planned succession of wires, and multiple failures might reflect a low level of patient compliance.2,3 Additionally, keeping the fixed appliance phase as short as possible is in the best interest of both the patient and orthodontist. Therefore, it is prudent to control effectively all factors that could prolong treatment duration.4,5
Considerable focus has been placed in the past decades on enhancing the efficiency of orthodontic treatment through the stimulation of patient compliance, modification of orthodontic appliances or bonding techniques, and the use of various adjuncts.6–8 However, existing evidence behind many of these measures is still lacking, and there is often insufficient support for their use to improve treatment efficiency.9,10 Studies have shown that the bonding performance of orthodontic appliances differs depending on factors such as tooth type and position, type of bonding agents and curing methods, and bracket mesh types and materials as well as aging and attrition of the bond in oral conditions. Among the various study designs to evaluate the effect and interaction of these factors, in vivo clinical studies are probably best suited for the formulation of clinical recommendations of efficacy. This is because the complex influencing factors cannot be simulated satisfactorily in in vitro and ex vivo studies, leading consequently to conflicting results, and being ultimately of little clinical significance.11,12
The aim of the present retrospective clinical cohort study was to assess, in a clinically relevant way, the failure patterns of different bracket systems and their effect on orthodontic treatment with fixed appliances. The effect of bracket failure on treatment duration was also assessed as a secondary outcome.
MATERIALS AND METHODS
As a result of the retrospective character of this study, the Ethical Committee of the University of Bonn raised no ethical concerns.
This study was based on a convenience sample from the clinical archives of patients consecutively treated by the same doctors with fixed appliances during a span of 5 years (2011–2016) in a private orthodontic practice in Bergheim, Germany. Patient eligibility was based on (1) clear medical history, (2) complete permanent dentition (with the possible exception of third molars), (3) no cases that were transferred from other practices, (4) complete documentation, (5) achievement of treatment goals (no early termination/drop-outs), and (6) loss of at least one bracket. The latter was set, as the aim of the study was to assess the failure patterns of brackets according to individual patient characteristics and not absolute survival.
A total of 78 patients (28 male/50 female) were recruited who received fixed appliance treatment with bonded attachments on all teeth except molars that were banded and were not assessed. The following four bracket systems (0.022″ slot) were used: (1) conventionally ligated stainless steel (SS) brackets (Mini Master, McLaughlin-Bennett-Trevisi (MBT) prescription, American Orthodontics, Sheboygan, WI, USA) in 25 patients, (2) conventionally ligated ceramic brackets (Clear Comfort, MBT prescription, West Ortho, Bergheim, Germany) in 20 patients, (3) self-ligating SS brackets (Damon 3MX, Ormco, Orange, CA, USA) in 25 patients, and (4) self-ligating Ni-free SS brackets (Bio Quick LP, MBT prescription, Forestadent, Pforzheim, Germany) in 8 patients. Patients included in this study were presented during treatment planning with information regarding all available bracket systems in the practice in the form of brochures and personalized consultation based on the patient's input (such as nickel allergy or esthetic concerns), and the bracket system used was chosen by the patient.
The same bonding protocol was used in all cases according to the manufacturer's instructions. Enamel surfaces were pumiced and then etched with 37% orthophosphoric acid for 30 seconds, thoroughly rinsed with water for 10 seconds, and dried. The same bonding adhesive and resin were employed (Light Bond Filled Sealant & Light Bond Composite, Reliance Orthodontics Products, Itasca, IL, USA). The brackets were placed by three doctors (including the practice owner), while bracket placement and all treatment phases were supervised by the practice owner. All conventionally ligated brackets were ligated using elastomeric ties.
Outcomes
The primary study outcome was the number of failed brackets at the patient level based on the patient's files. Secondarily, time to failure was extracted at the tooth level to assess the pattern of bracket failure. Only first-time failures for each bracket were assessed, because multiple failures of the same bracket might be a result of parafunction, detrimental habits, or flawed bonding protocol.8 Finally, the duration of active treatment in months was extracted at the patient level and measured from the time of insertion to the removal of appliances.
Statistical Analysis
Means and standard deviations (medians and interquartile ranges for non-normally distributed data) were calculated for continuous outcomes and frequencies for binary outcomes after normality checks. Generalized linear negative binomial regression was used to identify factors associated with the number of failed brackets per patient. Time-to-bracket failure was explored with survival analysis, and the bracket failure hazard ratios adjusted for confounders were calculated with Cox proportional hazards regression with shared frailty, accounting for the clustering of brackets within patients. Proportional hazard assumptions were assessed using log-log plots, comparing fitted and predicted Kaplan–Meier plots, and on the basis of Schoenfeld residuals. Finally, treatment duration and the effect of bracket failure (among others) on treatment duration were assessed with linear regression.
For all regression analyses, an initial univariable model with each factor was run and only variables with P ≤ .2 in the univariable model were included in a multivariable model adjusting for confounders such as patient age, sex, and tooth-, treatment-, or malocclusion-related characteristics. Malocclusion-related characteristics, including the presence of deepbite, crossbite, or anterior crowding, were extracted qualitatively by visual inspection of the pretreatment documents. All analyses were conducted with STATA SE 14.0 (StataCorp, College Station, Tex) with α = 0.05 and calculating 95% confidence intervals (CI).
RESULTS
The demographics of the sample are shown in Table 1. Mean treatment duration was 30.6 months, and overall first-time failure for the sample was 14.1% (217 from 1328 attachments; Appendix 1). Considerable differences existed according to tooth type, with an 8.0% failure of canines, followed by 11.3% for first premolars, 13.1% for central incisors, 14.4% for lateral incisors, and 23.4% for second premolars. In addition, significant differences existed according to bracket type, with 11.2% failures for SS self-ligated brackets, followed by 12.3% for SS conventionally ligated brackets, 13.8% for Ni-free self-ligated brackets, and 20.0% for ceramic conventionally ligated brackets.
Table 1.
Descriptive Characteristics of the Patient Sample Included in the Present Study and Treated With Each Bracket Typea
| Category |
Factor |
Category |
Overall |
SSCL |
CeramicCL |
SSSL |
Ni-freeSL |
||||||
| n |
(%) |
n |
(%) |
n |
(%) |
n |
(%) |
n |
(%) |
P |
|||
| Overall | 78 | (100) | 25 | (100) | 20 | (100) | 25 | (100) | 8 | (100) | |||
| General | |||||||||||||
| Gender | Female | 50 | (64) | 14 | (56) | 15 | (75) | 16 | (64) | 5 | (63) | .63 | |
| Male | 28 | (36) | 11 | (44) | 5 | (25) | 9 | (36) | 3 | (38) | |||
| Age | Mean (SD) | 78 | (12.6)(1.9) | 25 | (12.2)(1.5) | 20 | (13.3)(1.9) | 25 | (12.4)(2.3) | 8 | (12.8)(1.5) | .25 | |
| Malocclusion | |||||||||||||
| Deepbite | No | 37 | (47) | 9 | (36) | 8 | (40) | 14 | (56) | 6 | (75) | .18 | |
| Yes | 41 | (53) | 16 | (64) | 12 | (60) | 11 | (44) | 2 | (25) | |||
| Crossbite | No | 66 | (85) | 22 | (88) | 18 | (90) | 20 | (80) | 6 | (75) | .65 | |
| Yes | 12 | (15) | 3 | (12) | 2 | (10) | 5 | (20) | 2 | (25) | |||
| Anterior crowding | No | 15 | (19) | 3 | (12) | 7 | (35) | 2 | (8) | 3 | (38) | .05 | |
| Yes | 63 | (81) | 22 | (88) | 13 | (65) | 23 | (92) | 5 | (63) | |||
| Extraction case | No | 70 | (90) | 23 | (92) | 18 | (90) | 21 | (84) | 8 | (100) | .58 | |
| Yes | 8 | (10) | 2 | (8) | 2 | (10) | 4 | (16) | 0 | (0) | |||
| Auxiliary appliances used | No | 72 | (92) | 24 | (96) | 19 | (95) | 23 | (92) | 6 | (75) | .26 | |
| Compliance | Yes | 6 | (8) | 1 | (4) | 1 | (5) | 2 | (8) | 2 | (25) | ||
| Missed appointments | Mean (SD) | 78 | (2.5)(2.7) | 25 | (1.8)(2.4) | 20 | (3.0)(2.5) | 25 | (2.8)(2.8) | 8 | (2.8)(3.4) | .50 | |
| Hygiene warning given | No | 37 | (47) | 13 | (52) | 10 | (50) | 10 | (40) | 4 | (50) | .84 | |
| Yes | 41 | (53) | 12 | (48) | 10 | (50) | 15 | (60) | 4 | (50) | |||
SS indicates stainless steel; CL, conventionally ligated; SL, self-ligated; SD, standard deviation.
As far as the primary outcome was concerned, a median of three failed brackets per patient was observed (Table 2). Treatment duration and bracket type were significantly associated with the number of bracket failures (Table 3). After adjusting for confounders, only treatment duration was associated with increased failure, with 0.1 failure for each additional month of treatment (95% CI = 0.01–0.19 brackets), which may be extrapolated to an additional bracket failure every 10 months.
Table 2.
Summary Statistics of the Non-normally Distributed Outcome Number of Failed Brackets Per Patient for Different Variablesa
| Factor |
Category |
n |
Median (IQR) |
Range |
Pb |
| Overall | 78 | 3.0 (2.0–5.0) | 1.0–24.0 | ||
| Gender | Female | 50 | 3.0 (1.0–5.0) | 1.0–21.0 | .72 |
| Male | 28 | 3.0 (2.0–4.5) | 1.0–24.0 | ||
| Deepbite | No | 37 | 3.0 (2.0–5.0) | 1.0–13.0 | .78 |
| Yes | 41 | 3.0 (2.0–5.0) | 1.0–24.0 | ||
| Crossbite | No | 66 | 3.0 (1.0–5.0) | 1.0–24.0 | .38 |
| Yes | 12 | 3.5 (3.0–5.5) | 1.0–7.0 | ||
| Anterior crowding | No | 15 | 4.0 (2.0–7.0) | 1.0–24.0 | .27 |
| Yes | 63 | 3.0 (1.0–5.0) | 1.0–13.0 | ||
| Bracket type | SSCL | 25 | 3.0 (2.0–4.0) | 1.0–10.0 | .14 |
| CeramicCL | 20 | 5.0 (2.5–8.0) | 1.0–24.0 | ||
| SSSL | 25 | 3.0 (1.0–5.0) | 1.0–21.0 | ||
| Ni-freeSL | 8 | 2.5 (2.0–4.0) | 1.0–6.0 | ||
| Extraction case | No | 70 | 3.0 (2.0–5.0) | 1.0–24.0 | .75 |
| Yes | 8 | 2.5 (2.0–4.0) | 1.0–13.0 | ||
| Auxiliary appliances used | No | 72 | 3.0 (2.0–5.0) | 1.0–24.0 | .78 |
| Yes | 6 | 3.0 (2.0–3.0) | 1.0–9.0 | ||
| Missed appointments, binary | No | 25 | 2.0 (1.0–3.0) | 1.0–13.0 | .03 |
| Yes | 53 | 4.0 (2.0–6.0) | 1.0–24.0 | ||
| Hygiene warning received | No | 37 | 3.0 (2.0–5.0) | 1.0–24.0 | .63 |
| Yes | 41 | 3.0 (2.0–5.0) | 1.0–11.0 |
IQR indicates interquartile range; SS, stainless steel; CL, conventionally ligated; SL, self-ligated.
P values from Kruskal–Wallis tests.
Table 3.
Results of the Negative Binomial Bi- and Multivariable Regression for the Identification of Factors Important for the Number of Failed Brackets Per Patienta
| Factor |
Category |
Bivariable |
Multivariable |
||
| Coefficient (95% CI) |
P |
Coefficient (95% CI) |
P |
||
| Gender | Female | Referent | NT | ||
| Male | 0.05 (−2.13, 2.23) | .96 | NT | ||
| Age | Per year | −0.05 (−0.68, 0.58) | .87 | NT | |
| Deepbite | No | Referent | NT | ||
| Yes | 1.08 (−0.99, 3.16) | .31 | NT | ||
| Crossbite | No | Referent | NT | ||
| Yes | −0.36 (−3.09, 2.38) | .80 | NT | ||
| Anterior crowding | No | Referent | Referent | ||
| Yes | −2.45 (−5.99, 1.08) | .17 | −1.14 (−4.20, 1.92) | .47 | |
| Bracket type | SSCL | Referent | Referent | ||
| CeramicCL | 2.97 (−0.33, 6.27) | .08 | 1.96 (−1.22, 5.15) | .23 | |
| SSSL | 0.64 (−1.62, 2.90) | .58 | −0.17 (−2.15, 1.82) | .87 | |
| Ni-freeSL | −0.28 (−3.09, 2.53) | .85 | −1.53 (−4.48, 1.43) | .31 | |
| Extraction case | No | Referent | NT | ||
| Yes | −0.38 (−3.59, 2.83) | .82 | NT | ||
| Auxiliary appliances used | No | Referent | NT | ||
| Yes | −0.78 (−4.14, 2.58) | .65 | NT | ||
| Missed appointment | Per appointment | 0.32 (−0.15, 0.93) | .16 | 0.12 (−0.24, 0.59) | .41 |
| Hygiene warning received | No | Referent | NT | ||
| Yes | −0.61 (−2.72, 1.49) | .57 | NT | ||
| Treatment duration | Per month | 0.14 (0.03, 0.23) | .009 | 0.10 (0.01, 0.19) | .03 |
Results are given as unstandardized coefficients with their 95% confidence intervals. CI indicates confidence interval; NT, not tested; SS, stainless steel; CL, conventionally ligated; SL, self-ligated.
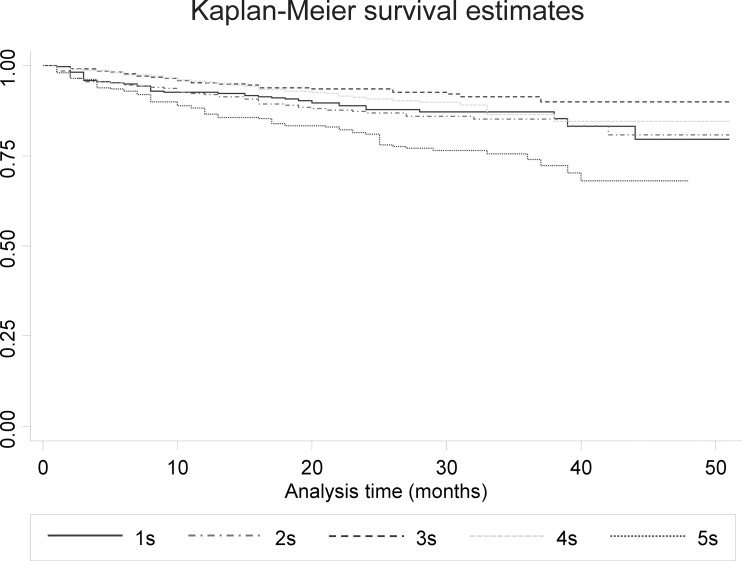
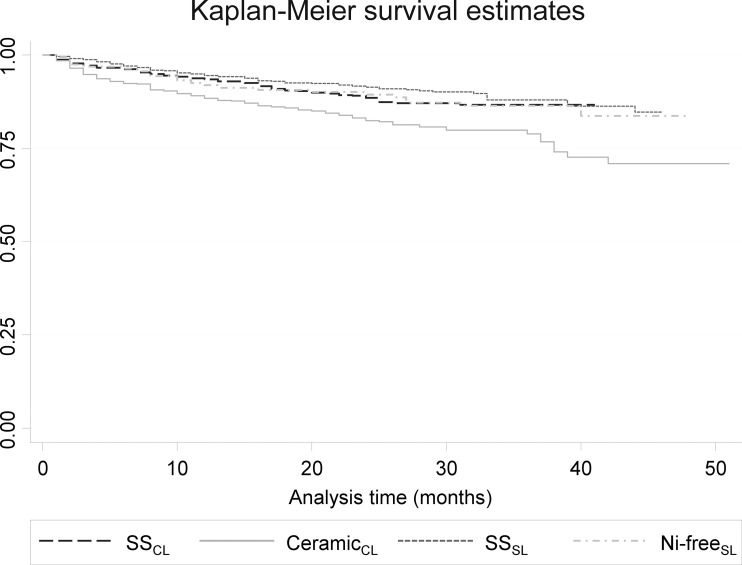
To take into account the differences in treatment duration among patients, bracket failure was analyzed as a time-to-event variable (Table 4). When compared with canine brackets (which showed the lowest failure rate), brackets at the central incisors (hazard ratio [HR] = 1.7; 95% CI = 1.1–2.9), lateral incisors (HR = 1.9; 95% CI = 1.2–3.1), and second premolars (HR = 3.2; 95% CI = 2.0–5.0) were at any particular time more prone to failure (Figure 1). In addition, the ceramic conventionally ligated brackets were 60% more prone to failure at any time when compared with the SS conventionally ligated brackets (HR = 1.6; 95% CI = 1.1–2.3; Figure 2).
Table 4.
Results of the Cox Bi- and Multivariable Regression for the Identification of Factors Important for the Survival of Bracketsa
| Factor |
Category |
Bivariable |
Multivariable |
||
| HR (95% CI) |
P |
HR (95% CI) |
P |
||
| Gender | Female | Referent | NT | ||
| Male | 1.00 (0.73–0.38) | .98 | NT | ||
| Age | Per year | 1.00 (0.92–1.08) | .93 | NT | |
| Jaw | Mandible | Referent | Referent | ||
| Maxilla | 1.30 (0.99–1.69) | .06 | 1.30 (1.00–1.70) | .05 | |
| Deepbite | No | Referent | NT | ||
| Yes | 1.24 (0.91–1.67) | .17 | 1.14 (0.85–1.52) | .38 | |
| Crossbite | No | Referent | NT | ||
| Yes | 0.89 (0.58–1.37) | .60 | NT | ||
| Anterior crowding | No | Referent | NT | ||
| Yes | 0.92 (0.63–1.34) | .66 | NT | ||
| Mouth side | Left | Referent | NT | ||
| Right | 1.15 (0.88–1.51) | .30 | NT | ||
| Tooth | Central incisor | 1.72 (1.05–2.83) | .03 | 1.74 (1.06–2.87) | .03 |
| Lateral incisor | 1.87 (1.15–3.05) | .01 | 1.89 (1.16–3.08) | .01 | |
| Canine | Referent | Referent | |||
| First premolar | 1.43 (0.85–2.40) | .17 | 1.45 (0.86–2.43) | .16 | |
| Second premolar | 3.22 (2.04–5.08) | <.001 | 3.19 (2.03–5.03) | <.001 | |
| Tooth category | Posterior, canines-premolars | Referent | NT | ||
| Anterior, incisors | 0.98 (0.74–1.28) | .86 | NT | ||
| Bracket type | SSCL | Referent | Referent | ||
| CeramicCL | 1.64 (1.15–2.32) | .006 | 1.62 (1.14–2.29) | .007 | |
| SSSL | 0.79 (0.54–1.15) | .21 | 0.80 (0.55–1.18) | .26 | |
| Ni-freeSL | 0.96 (0.58–1.60) | .89 | 1.01 (0.60–1.69) | .98 | |
| Extraction case | No | Referent | NT | ||
| Yes | 0.85 (0.51–1.42) | .54 | NT | ||
| Auxiliary appliances used | No | Referent | NT | ||
| Yes | 1.00 (0.57–1.75) | 1.00 | NT | ||
| Missed appointment | Per appointment | 1.03 (0.98–1.09) | .24 | NT | |
| Hygiene warning received | No | Referent | NT | ||
| Yes | 0.99 (0.73–1.35) | .96 | NT | ||
Results are given as hazard ratios with their 95% confidence intervals. HR indicates hazard ratio; CI, confidence interval; NT, not tested; SS, stainless steel; CL, conventionally ligated; SL, self-ligated.
Figure 1.
Kaplan–Meier plot for bracket survival according to tooth category. When compared with canine brackets (lowest bracket failure rate observed), brackets at the central incisors (hazard ratio = 1.7; 95% confidence interval = 1.1–2.9), lateral incisors (hazard ratio = 1.9; 95% confidence interval = 1.2–3.1), and second premolars (hazard ratio = 3.21; 95% confidence interval = 2.0–5.0) were significantly more prone to failure at any particular time. 1s, upper/lower central incisors; 2s, upper/lower lateral incisors; 3s, upper/lower canines; 4s, upper/lower first premolars; 5s, upper/lower second premolars.
Figure 2.
Kaplan–Meier plot for bracket survival according to bracket system. Ceramic conventionally ligated brackets were 60% more prone to failure at any time when compared with SS conventionally ligated brackets (hazard ratio = 1.6; 95% confidence interval = 1.1–2.3). SS indicates stainless steel; CL, conventionally ligated; SL, self-ligated; Ni-free, nickel free.
Finally, the factors influencing treatment duration were analyzed (Table 5; Appendix 2). Prolonged treatment duration was associated with the use of nickel-free self-ligating brackets when compared with the SS conventionally ligated brackets (by 6.5 months; 95% CI = 0.6–12.4 months) and with extraction treatment when compared with nonextraction treatment (by 7.3 months; 95% CI = 1.8–12.9 months). Furthermore, treatment duration was significantly prolonged by 0.8 months for each additional missed patient appointment (95% CI = 0.2–1.5 months) and by 0.6 months for each additional failed bracket (95% CI = 0.2–1.1 months).
Table 5.
Results of the Linear Bi- and Multivariable Regression for the Identification of Factors Important for Treatment Durationa
| Factor |
Category |
Bivariable |
Multivariable |
||
| Coefficient (95% CI) |
P |
Coefficient (95% CI) |
P |
||
| Gender | Female | Referent | NT | ||
| Male | 1.69 (−2.23, 5.62) | .39 | NT | ||
| Age | Per year | −0.19 (−1.18, 0.80) | .70 | NT | |
| Deepbite | No | Referent | NT | ||
| Yes | −1.17 (−4.95, 2.61) | .54 | NT | ||
| Crossbite | No | Referent | Referent | ||
| Yes | 4.08 (−1.08, 9.24) | .12 | 1.35 (−3.33, 6.03) | .57 | |
| Anterior crowding | No | Referent | NT | ||
| Yes | −1.12 (−5.92, 3.67) | .64 | NT | ||
| Bracket type | SSCL | Referent | Referent | ||
| CeramicCL | 1.38 (−3.50, 6.26) | .58 | −1.53 (−6.03, 2.98) | .50 | |
| SSSL | 4.60 (0.00, 9.20) | .05 | 2.75 (−1.38, 6.87) | .19 | |
| Ni-freeSL | 6.63 (0.03, 13.23) | .05 | 6.47 (0.57, 12.36) | .03 | |
| Extraction case | No | Referent | Referent | ||
| Yes | 7.10 (1.08, 13.12) | .02 | 7.31 (1.77, 12.86) | .01 | |
| Auxiliary appliances used | No | Referent | NT | ||
| Yes | 1.49 (−5.61, 8.58) | .68 | NT | ||
| Missed appointments | Per appointment | 1.02 (0.34, 1.69) | .004 | 0.82 (0.19, 1.46) | .01 |
| Hygiene warning received | No | Referent | NT | ||
| Yes | −0.96 (−4.75, 2.82) | .61 | Referent | ||
| Number of bracket failures | Per failure | 0.58 (0.14, 1.03) | .01 | 0.63 (0.21, 1.05) | .004 |
Results are given as unstandardized coefficients with their 95% confidence intervals. CI indicates confidence interval; NT, not tested; SS, stainless steel; CL, conventionally ligated; SL, self-ligated.
DISCUSSION
This retrospective cohort study assessed the pattern of bracket failure during fixed-appliance treatment and treatment duration. This study indicated that the majority of patients lost more than one bracket during treatment (median of three failures; Table 2), whereas only 18 of 78 patients (23%) lost only one bracket, which is consistent with previous studies.3,7 The overall bracket failure rate at the tooth level was 14.1%, which is higher when compared with previously reported failure rates of 6% to 8%.11,13,14 However, this might be a result of the inclusion of only patients with ≥1 failed bracket to explore the relative bracket failure pattern among patients.
In addition, the mean treatment duration of 30.6 months found in the present study might be longer than the average duration found in the literature.5 This could be explained by a wide malocclusion spectrum that is usually excluded from controlled trials or by the use of bracket failure as an eligibility criterion.
As far as the pattern of failed brackets is concerned, significant differences were found according to tooth type, with canines being the least prone to failure, followed by central incisors (+74% higher failure rate), lateral incisors (+89% higher failure rate), and second premolars (+219% higher failure rate; Table 4), which is in agreement with the patterns observed in other studies.8,14–16 Tooth-specific differences in the bracket failure rate have been attributed to the increased risk of moisture contamination at certain sites, increased masticatory loads, and larger amounts of aprismatic enamel.13,17,18 The higher incisor bracket failure when compared with canines could possibly be explained by either increased activation forces as a result of anterior crowding or by increased mastication forces received during biting food.
As far as the appliance's influence is concerned, significant differences were found between SS and ceramic brackets, with the latter being significantly more prone to failure at any time during treatment (Table 4). This might be explained by the lower structural integrity of ceramic brackets compared to the more deformable SS brackets,19 thus leading to material failure more easily.
Furthermore, a proportional relationship was found between additional bracket failure rate and treatment duration, with 0.1 more failed brackets for each additional month of treatment (or inversely, one additional bracket failure for every 10 months of treatment). This may be because a longer exposure of a bracket to the oral environment corresponds to longer exposure to various degrading factors to the bond surface, such as continuous, multivector occlusal forces, by-products of complex bacterial activity, possibly extreme pH conditions, and variations in temperature.12,20
In addition, bracket failure was found to significantly affect treatment duration, with an extra 0.6 month for each additional bracket failure (Table 5). Taking into account the median number of three failed brackets per patient (interquartile range = 2–5 brackets), excessive bracket failure alone might lead to prolonged treatment by 1.8 months (interquartile range = 1.2–3.0 months), which given the great efforts being made to accelerate orthodontic treatment in any way4,9 might be of importance.
Increased treatment duration was also observed in extraction treatment and on the basis of missed patient appointments; both of these factors are straightforward and can be easily explained. Although temporal trends have been observed in the incidence of orthodontic tooth extractions, the choice of whether to extract teeth should be founded on systematic appraisal of the diagnostic records, treatment plan, and sound biological principles, which are evaluated on a case-by-case level.21,22
Missed appointments are a close proxy to patient compliance, with documented impact on bracket failure and treatment duration.1,3 Interestingly, interventions aimed at improving patient compliance during orthodontic treatment have been found to reduce observed bracket failure and could lead to improved treatment efficiency.6,23
Finally, prolonged treatment duration was associated with the use of nickel-free SL brackets compared to SS conventionally ligated brackets (Table 5), which could not be explained by an increased bracket failure rate for the former and was consistent with previous evidence from randomized trials.10 It might be that the SL brackets used were less effective during the various treatment phases such as finishing or torque application, which have been reported to be problematic with certain SL brackets.24,25 Another possible explanation is the possible wear-out of the SL bracket's clips that, in turn, might have reduced the bracket's efficiency.26 However, caution is warranted with the interpretation of this, because of the nonrandomized nature of the present study. Although the inclusion of nonrandomized studies may be acceptable for assessing the adverse effects of interventions (such as bracket failure), randomization is more critical when judging the therapeutic effects of interventions (such as treatment duration), where randomized clinical trials are the gold standard.27
The strength of the present study includes the use of objective and transparent eligibility criteria to select patients from a pool of consecutively treated patients and the detailed extraction of patient-, appliance-, and treatment-related characteristics, which were appropriately analyzed to assess bracket failure and its effect on treatment duration. However, several limitations were also present. First, this was a nonrandomized historical (retrospective) cohort study, a design that has been shown to be more prone to bias than prospective clinical studies and especially randomized studies.27–29 Therefore, explorative inferences can be drawn from the present study as far as demographic patient- or tooth-specific characteristics related to bracket failure are concerned, but no sound evidence can be attained regarding the comparative effectiveness of the various brackets in treating malocclusions. In addition, the included patients were treated by three different clinicians, which might have influenced the study's results. However, all clinicians had been trained and were working in the same practice using the same bonding and treatment approach for the past 5 years, and all treatment phases were directly supervised by the practice owner (Dr Kirsch). Finally, no sample size calculation was performed because this study was based on the application of a priori set eligibility criteria on a convenience sample of all available patients treated in the past 5 years by the same doctors. Therefore the results, especially for the subgroup of Ni-free brackets or extraction cases, should be viewed as having potentially low statistical power.
The results of the present study could be generalized to the average white patient being treated mostly nonextraction with a wide array of directly bonded buccal fixed appliances in an orthodontic specialty practice by experienced clinicians. They might be less applicable to patients treated in university clinics or patients treated with indirect bonded, lingual, or custom-made appliances.
CONCLUSIONS
Based on the results of the present retrospective cohort study with its inherent limitations, the following conclusions can be drawn:
Multiple bracket failures are clustered in certain patients with a median of three failed brackets per patient.
Tooth-specific differences in bracket failure rate were seen, with canines having the lowest failure rate, followed by incisors and premolars.
Ceramic conventionally ligated brackets were more prone to failure at any time than SS brackets, whether they were conventionally ligated or self-ligated.
Bracket failure was directly associated with prolonged treatment time by 0.6 months for every additional failed bracket.
Appendix 1.
Summary Statistics of Bracket Failure by Characteristica
| Factor |
Category |
Failure, first time, n (%) |
Pb |
|
| No |
Yes |
|||
| Overall | 1328 (86.0) | 217 (14.1) | ||
| Gender | Female | 856 (86.2) | 137 (13.8) | .706 |
| Male | 472 (85.5) | 80 (14.5) | ||
| Jaw | Mandible | 677 (87.6) | 96 (12.4) | .066 |
| Maxilla | 651 (84.3) | 121 (15.7) | ||
| Deepbite | No | 640 (87.2) | 94 (12.8) | .182 |
| Yes | 688 (84.8) | 123 (15.2) | ||
| Crossbite | No | 1125 (85.9) | 184 (14.1) | .976 |
| Yes | 203 (86.0) | 33 (14.0) | ||
| Anterior crowding | No | 254 (85.0) | 45 (15.1) | .578 |
| Yes | 1074 (86.2) | 172 (13.8) | ||
| Mouth side | Left | 670 (86.9) | 101 (13.1) | .286 |
| Right | 658 (85.0) | 116 (15.0) | ||
| Tooth | Central incisor | 271 (86.9) | 41 (13.1) | <.001 |
| Lateral incisor | 267 (85.6) | 45 (14.4) | ||
| Canine | 287 (92.0) | 25 (8.0) | ||
| First premolar | 267 (88.7) | 34 (11.3) | ||
| Second premolar | 236 (76.6) | 72 (23.4) | ||
| Tooth category | Posterior, canines-premolars | 790 (85.8) | 131 (14.2) | .806 |
| Anterior, incisors | 538 (86.2) | 86 (13.8) | ||
| Bracket type | SSCL | 436 (87.7) | 61 (12.3) | .001 |
| CeramicCL | 316 (80.0) | 79 (20.0) | ||
| SSSL | 438 (88.8) | 55 (11.2) | ||
| Ni-freeSL | 138 (86.3) | 22 (13.8) | ||
| Extraction case | No | 1204 (86.0) | 196 (14.0) | .873 |
| Yes | 124 (85.5) | 21 (14.5) | ||
| Auxiliary appliances used | No | 1227 (86.0) | 199 (14.0) | .724 |
| Yes | 101 (84.9) | 18 (15.1) | ||
| Missed appointments, binary | No | 442 (89.1) | 54 (10.9) | .014 |
| Yes | 886 (84.5) | 163 (15.5) | ||
| Hygiene warning received | No | 628 (85.7) | 105 (14.3) | .764 |
| Yes | 700 (86.2) | 112 (13.8) | ||
SS indicates stainless steel; CL, conventionally ligated; SL, self-ligated.
P values from chi-square tests.
Appendix 2.
Summary Statistics of Treatment Duration by Characteristica
| Factor |
Category |
n |
Mean (SD) |
Pb |
| Overall | 78 | 30.6 (8.3) | ||
| Gender | Female | 50 | 30.0 (8.6) | .393 |
| Male | 28 | 31.7 (7.8) | ||
| Deepbite | No | 37 | 31.2 (8.6) | .540 |
| Yes | 41 | 30.1 (8.2) | ||
| Crossbite | No | 66 | 30.0 (7.8) | .119 |
| Yes | 12 | 34.1 (10.4) | ||
| Crowding | No | 15 | 31.5 (9.3) | .643 |
| Yes | 63 | 30.4 (8.2) | ||
| Bracket type | SSCL | 25 | 28.1 (6.8) | .102 |
| CeramicCL | 20 | 29.5 (9.7) | ||
| SSSL | 25 | 32.7 (7.9) | ||
| Ni-freeSL | 8 | 34.8 (8.8) | ||
| Extraction case | No | 70 | 29.9 (8.2) | .022 |
| Yes | 8 | 37.0 (6.8) | ||
| Auxiliary appliances used | No | 72 | 30.5 (8.2) | .678 |
| Yes | 6 | 32.0 (10.9) | ||
| Missed appointments, binary | No | 25 | 28.5 (8.9) | .126 |
| Yes | 53 | 31.6 (7.9) | ||
| Hygiene warning received | No | 37 | 31.1 (8.9) | .613 |
| Yes | 41 | 30.2 (7.9) |
SD indicates standard deviation; SS, stainless steel; CL, conventionally ligated; SL, self-ligated.
P values from 1-way analysis of variance and t-tests.
REFERENCES
- 1.Beckwith FR, Ackerman RJ, Cobb CM, Tira DE. An evaluation of factors affecting duration of orthodontic treatment. Am J Orthod Dentofacial Orthop. 1999;115:7439–7447. doi: 10.1016/s0889-5406(99)70265-9. [DOI] [PubMed] [Google Scholar]
- 2.Popowich K, Nebbe B, Heo G, Glover KE, Major PW. Predictors for class II treatment duration. Am J Orthod Dentofacial Orthop. 2005;127:293–300. doi: 10.1016/j.ajodo.2003.12.025. [DOI] [PubMed] [Google Scholar]
- 3.Skidmore KJ, Brook KJ, Thomson WM, Harding WJ. Factors influencing treatment time in orthodontic patients. Am J Orthod Dentofacial Orthop. 2006;129:230–238. doi: 10.1016/j.ajodo.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 4.Mavreas D, Athanasiou AE. Factors affecting the duration of orthodontic treatment: a systematic review. Eur J Orthod. 2008;30:386–395. doi: 10.1093/ejo/cjn018. [DOI] [PubMed] [Google Scholar]
- 5.Papageorgiou SN, Höchli D, Eliades T. Outcome assessment of comprehensive fixed appliance treatment: a systematic review with meta-analysis and methodological overview of studies using the American Board of Orthodontists Objective Grading System. Korean J Orthod. 47:401–413. doi: 10.4041/kjod.2017.47.6.401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li X, Xu ZR, Tang N, et al. Effect of intervention using a messaging app on compliance and duration of treatment in orthodontic patients. Clin Oral Investig. 2016;20:1849–1859. doi: 10.1007/s00784-015-1662-6. [DOI] [PubMed] [Google Scholar]
- 7.Ziebura T, Hohoff A, Flieger S, Stamm T. Accidental debondings: buccal vs fully individualized lingual multibracket appliances. Am J Orthod Dentofacial Orthop. 2014;145:649–654. doi: 10.1016/j.ajodo.2013.12.030. [DOI] [PubMed] [Google Scholar]
- 8.O'Dywer L, Littlewood SJ, Rahman S, Spencer RJ, Barber SK, Russell JS. A multi-center randomized controlled trial to compare a self-ligating bracket with a conventional bracket in a UK population: part 1: treatment efficiency. Angle Orthod. 2016;86:142–148. doi: 10.2319/112414837.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fleming PS, Fedorowicz Z, Johal A, El-Angbawi A, Pandis N. Surgical adjunctive procedures for accelerating orthodontic treatment. Cochrane Database Syst Rev. 2015;6:CD010572. doi: 10.1002/14651858.CD010572.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Papageorgiou SN, Konstantinidis I, Papadopoulou K, Jäger A, Bourauel C. Clinical effects of pre-adjusted edgewise orthodontic brackets: a systematic review and meta-analysis. Eur J Orthod. 2014;36:350–363. doi: 10.1093/ejo/cjt064. [DOI] [PubMed] [Google Scholar]
- 11.Linklater RA, Gordon PH. Bond failure patterns in vivo. Am J Orthod Dentofacial Orthop. 2003;123:534–539. doi: 10.1067/mod.2003.S0889540602000252. [DOI] [PubMed] [Google Scholar]
- 12.Eliades T, Brantley WA. The inappropriateness of conventional orthodontic bond strength assessment protocols. Eur J Orthod. 2000;22:13–23. doi: 10.1093/ejo/22.1.13. [DOI] [PubMed] [Google Scholar]
- 13.Millett DT, Gordon PH. A 5-year clinical review of bond failure with a no-mix adhesive (Right On) Eur J Orthod. 1994;16:203–211. doi: 10.1093/ejo/16.3.203. [DOI] [PubMed] [Google Scholar]
- 14.Sunna S, Rock WP. Clinical performance of orthodontic brackets and adhesive systems: a randomized clinical trial. Br J Orthod. 1998;25:283–287. doi: 10.1093/ortho/25.4.283. [DOI] [PubMed] [Google Scholar]
- 15.Trimpeneers LM, Dermaut LR. A clinical trial comparing the failure rates of two orthodontic bonding systems. Am J Orthod Dentofacial Orthop. 1996;110:547–550. doi: 10.1016/s0889-5406(96)70064-1. [DOI] [PubMed] [Google Scholar]
- 16.Kula K, Schreiner R, Brown J, Glaros A. Clinical bond failure of pre-coated and operator-coated orthodontic brackets. Orthod Craniofac Res. 2002;5:161–165. doi: 10.1034/j.1600-0544.2002.02199.x. [DOI] [PubMed] [Google Scholar]
- 17.Whitakker DK. Structural variations in the surface zone of human tooth enamel observed by scanning electron microscopy. Arch Oral Biol. 1982;27:383–392. doi: 10.1016/0003-9969(82)90147-9. [DOI] [PubMed] [Google Scholar]
- 18.Zachrisson BU. A post-treatment evaluation of direct bonding in orthodontics. Am J Orthod. 1977;71:173–189. doi: 10.1016/s0002-9416(77)90394-3. [DOI] [PubMed] [Google Scholar]
- 19.Reddy YG, Sharma R, Singh A, Agrawal V, Agrawal V, Chaturvedi S. The shear bond strengths of metal and ceramic brackets: an in-vitro comparative study. J Clin Diagn Res. 2013;7:1495–1497. doi: 10.7860/JCDR/2013/5435.3172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Matasa CG. Microbial attack of orthodontic adhesives. Am J Orthod Dentofacial Orthop. 1995;108:132–141. doi: 10.1016/s0889-5406(95)70075-7. [DOI] [PubMed] [Google Scholar]
- 21.Jackson TH, Guez C, Lin FC, Proffit WR, Ko CC. Extraction frequencies at a university orthodontic clinic in the 21st century: demographic and diagnostic factors affecting the likelihood of extraction. Am J Orthod Dentofacial Orthop. 2017;151:456–462. doi: 10.1016/j.ajodo.2016.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peck S. Extractions, retention and stability: the search for orthodontic truth. Eur J Orthod. 2017;39:109–115. doi: 10.1093/ejo/cjx004. [DOI] [PubMed] [Google Scholar]
- 23.Wright NS, Fleming PS, Sharma PK, Battagel J. Influence of supplemental written information on adolescent anxiety, motivation and compliance in early orthodontic treatment. Angle Orthod. 2010;80:329–335. doi: 10.2319/042809-138.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harradine NW, Birnie DJ. The clinical use of Activa self-ligating brackets. Am J Orthod Dentofacial Orthop. 1996;109:319–328. doi: 10.1016/s0889-5406(96)70155-5. [DOI] [PubMed] [Google Scholar]
- 25.Huang Y, Keilig L, Rahimi A, et al. Numeric modeling of torque capabilities of self-ligating and conventional brackets. Am J Orthod Dentofacial Orthop. 2009;136:638–643. doi: 10.1016/j.ajodo.2009.04.018. [DOI] [PubMed] [Google Scholar]
- 26.Pandis N, Bourauel C, Eliades T. Changes in the stiffness of the ligating mechanism in retrieved active self-ligating brackets. Am J Orthod Dentofacial Orthop. 2007;132:834–837. doi: 10.1016/j.ajodo.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 27.Papageorgiou SN, Xavier GM, Cobourne MT. Basic study design influences the results of orthodontic clinical investigations. J Clin Epidemiol. 2015;68:1512–1522. doi: 10.1016/j.jclinepi.2015.03.008. [DOI] [PubMed] [Google Scholar]
- 28.Papageorgiou SN, Kloukos D, Petridis H, Pandis N. Publication of statistically significant research findings in prosthodontics & implant dentistry in the context of other dental specialties. J Dent. 2015;43:1195–1202. doi: 10.1016/j.jdent.2015.08.005. [DOI] [PubMed] [Google Scholar]
- 29.Papageorgiou SN, Koretsi V, Jäger A. Bias from historical control groups used in orthodontic research: a meta-epidemiological study. Eur J Orthod. 2017;39:98–105. doi: 10.1093/ejo/cjw035. [DOI] [PubMed] [Google Scholar]