Abstract
A 3-dimensional printed model derived from a computed tomography dataset was obtained in a patient with tetralogy of Fallot and major aortopulmonary collaterals. The virtual and solid 3-dimensional heart models provided intuitive representation of such complex and highly individual pathologies and allowed comprehensive spatial conceptualization of the cardiac structures. (Level of Difficulty: Advanced.)
Key Words: 3-dimensional printing, computed tomography, congenital heart defect
Abbreviations and Acronyms: 3D, 3-dimensional; MAPCA, major aortopulmonary collateral artery; VSD, ventricular septal defect
Graphical abstract
A 3-dimensional printed model derived from a computed tomography dataset was obtained in a patient with tetralogy of Fallot and major aortopulmonary…
A 36-year-old male patient came to our noninvasive laboratory for a pre-employment visit. He had a history of congenital heart disease with a surgical procedure in early infancy in his home country; however, no details were available. At physical examination, he was cyanotic with clubbing; a medial sternotomy scar was present, and the auscultation revealed a harsh 3/6 pansystolic murmur at the left sternal edge. His oxygen saturation in room air was 83%. An electrocardiogram showed sinus rhythm and marked right ventricular hypertrophy. A chest x-ray revealed cardiomegaly with bilateral prominent vascular markings. His hemoglobin was 16.8 g/dl, and his hematocrit was 48.2%.
A transthoracic echocardiogram showed a right-sided aortic arch and a large ventricular septal defect (VSD) with an over-riding aorta. The main pulmonary artery was hypoplastic, and there was right ventricular hypertrophy. Contrast cardiac computed tomography was performed (Video 1, Supplemental Figure 1), which provided data for subsequent 3-dimensional (3D) printing in end diastole (Materialise Inc., Leuven, Belgium) (Video 2). The virtual model and 3D solid printouts confirmed and visualized the over-riding aorta and the hypoplastic right ventricular outflow tract (Figures 1A and 1B). The large VSD was seen in real anatomy, and its size and relationships with the adjacent structures were easily appreciated (Figures 1C and 1D). A central shunt was identified connecting the ascending aorta to the hypoplastic main pulmonary artery, and the course of the left and right pulmonary arteries was clearly appreciated using interactive views (Figures 1E and 1F). Major aortopulmonary collateral arteries (MAPCAs) were visible, and 3D reconstruction was able to identify the origin from the descending aorta and to render their spatial relationship with the pulmonary arteries (Figures 1G and 1H). The patient refused other investigations, including angiographic study, and eventually returned to his home country.
Online Video 1.
Axial computed tomography cuts for the chest (mediastinal window) from the apex of the lung until the upper abdomen. The images demonstrate a right-sided aortic arch, large ventricular septal defect with an over-riding aorta, main pulmonary artery atresia with a hypoplastic right ventricular outflow tract, a central shunt connecting the ascending aorta (AAo) to the hypoplastic main pulmonary artery, and major aortopulmonary collaterals.
Online Video 2.
Three-Dimensional Printed Model
The model is cut at the midventricular level for in-depth visualization of the cardiac structures, which allows optimal visualization of the over-riding aorta. The spatial relationships of the ventricular septal defect with the adjacent structures and the overriding aorta are clearly appreciated.
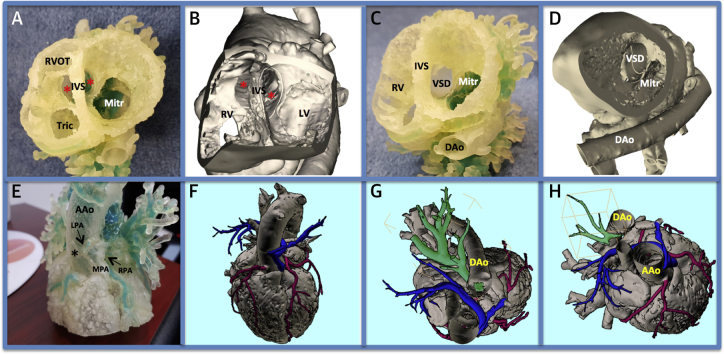
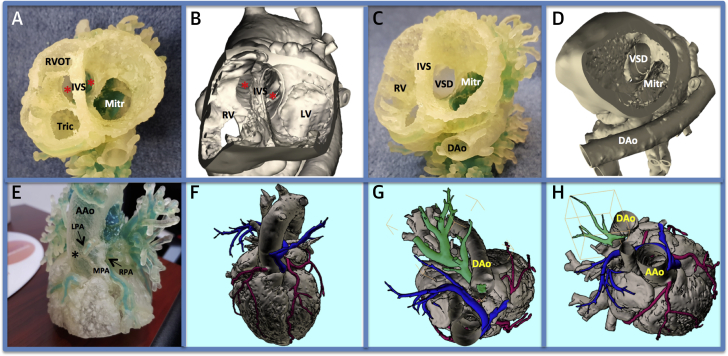
Figure 1.
3-Dimensional Solid Printouts and Virtual Heart Models
(A) A comparison of the 3-dimensional (3D) printed heart model and (B) the virtual 3D reconstruction model. The model is cut at the midventricular level with a viewpoint toward the base of the heart, which allows optimal visualization of the over-riding aorta (asterisks). The hypoplastic right ventricular outflow tract (RVOT) is also visible. (C and D) A tangential view from the left clearly reveals the ventricular septal defect (VSD) and its relationship with the mitral orifice. (E and F) A solid printout of the personalized 3D heart model, anterior view. A central shunt (asterisk) connects the ascending aorta (AAo) with the hypoplastic pulmonary artery (MPA). The right pulmonary artery (RPA) and left pulmonary artery (LPA) are also hypoplastic, and their course can be followed (displayed in blue) in the virtual model. The coronary arteries are displayed in red. (G and H) The 3D virtual model with different off-axis cut planes. Several major aortopulmonary collateral arteries are displayed in green, with clear appreciation of their origin from the descending aorta. See Videos 1 and 2. Dao = descending aorta; IVS = interventricular septum; LV = left ventricle; Mitr = mitral orifice; RV = right ventricle; Tric = tricuspid orifice.
The cardinal features of tetralogy of Fallot (pulmonary infundibular stenosis, an interventricular communication, biventricular connection of the aorta, and right ventricular hypertrophy) can be associated with a wide spectrum of associated anomalies, including pulmonary atresia, atrioventricular septal defect, abnormal branching of the coronary arteries, a right aortic arch, and persistence of left superior vena cava (1). Pulmonary atresia, VSD, and MAPCAs are rare variants of tetralogy of Fallot in which surgical management is tailored to the anatomy of each individual patient and depends on the presence and caliber of true pulmonary arteries and the anatomy of the MAPCAs. Therefore, pre-operative imaging should be focused on variants that have implications for operative repair.
Three-dimensional printing has the potential to convey the anatomic arrangement and to provide a comprehensive spatial conceptualization of the cardiac structures of such complex and highly individual pathologies (2). In the present case, solid printouts of the personalized 3D heart model were able to provide accurate anatomic representation of the pathologic structures, including pulmonary atresia, MAPCAs, and the right aortic arch. Although randomized data and recommendations on the use of 3D printing in congenital heart disease are still lacking, significant advantages in pre-operative and pre-procedural planning may be anticipated (3).
Footnotes
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Informed consent was obtained for this case.
Appendix
For a supplemental figure and videos, please see the online version of this paper.
Appendix
References
- 1.Khan S.M., Drury N.E., Barron D.J. Tetralogy of Fallot: morphological variations and implications for surgical repair. Eur J Cardiothorac Surg. 2019;56:101–109. doi: 10.1093/ejcts/ezy474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bartel T., Rivard A., Jimenez A., Mestres C.A., Müller S. Medical three-dimensional printing opens up new opportunities in cardiology and cardiac surgery. Eur Heart J. 2018;39:1246–1254. doi: 10.1093/eurheartj/ehx016. [DOI] [PubMed] [Google Scholar]
- 3.Sun Z., Lau I., Wong Y.H., Yeong C.H. Personalized three-dimensional printed models in congenital heart disease. J Clin Med. 2019;8:522–539. doi: 10.3390/jcm8040522. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.