Abstract
This report highlights the importance of recognizing, managing, and predicting the risk of ventricular fibrillation in patients presenting with pre-excited atrial fibrillation. (Level of Difficulty: Beginner.)
Key Words: atrial fibrillation, palpitations, ventricular fibrillation
Abbreviations and Acronyms: AF, atrial fibrillation; AV, atrioventricular
Graphical abstract
This report highlights the importance of recognizing, managing, and predicting the risk of ventricular fibrillation in patients presenting…
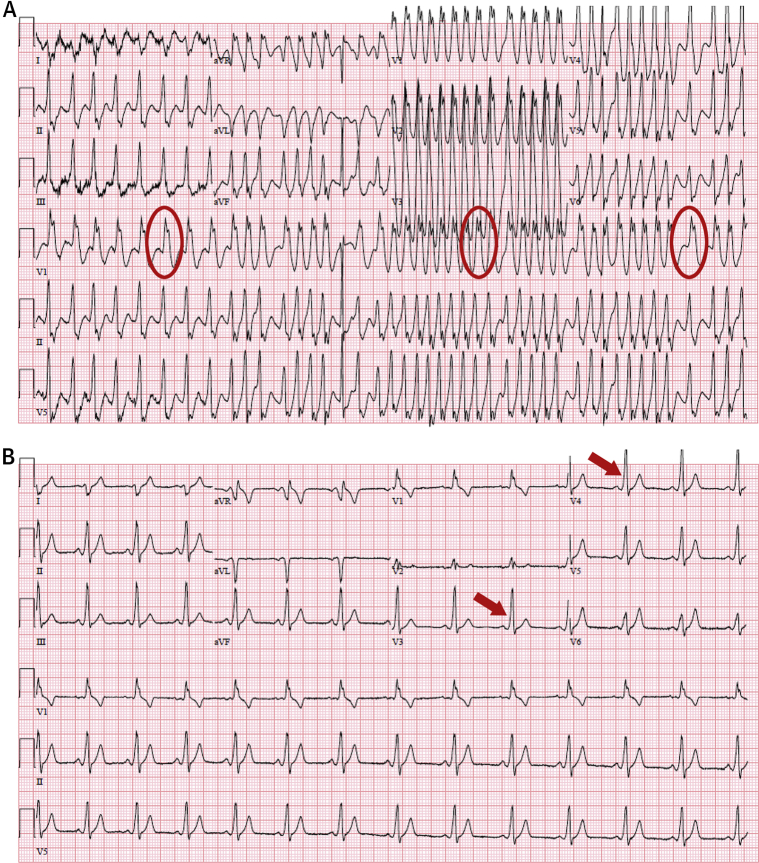
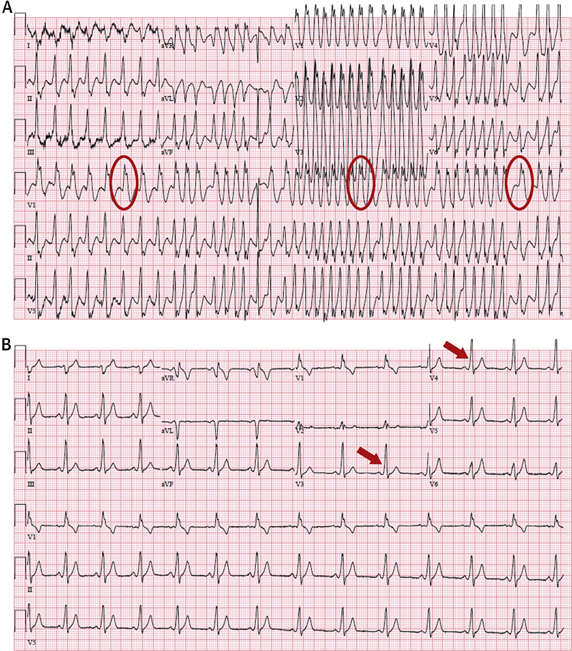
A 25-year-old man presented to the emergency department with a report of sudden-onset palpitations and lightheadedness. The initial electrocardiogram demonstrated an irregular, wide QRS complex tachycardia (Figure 1A, circles) consistent with Wolff-Parkinson-White syndrome with pre-excited atrial fibrillation (AF), with the shortest pre-excited RR interval being 160 ms. The patient became hypotensive and diaphoretic, so synchronized direct-current cardioversion was performed. Normal sinus rhythm with pre-excitation (Figure 1B, arrows) suggestive of a left lateral accessory pathway was then noted on his electrocardiogram, and catheter ablation was performed. AF with an antegrade conducting accessory pathway increases the risk of sudden cardiac death by rapid conduction over the accessory pathway. A shortest pre-excited RR interval of <250 ms during AF predicts an increased risk of degeneration to ventricular fibrillation. Atrioventricular (AV) nodal blocking agents should be avoided because they increase the risk of preferential conduction down the accessory pathway with degeneration to ventricular fibrillation (1). Verapamil, in particular, can be detrimental because of its added vasodilatory properties. Patients with pre-excited AF who are hemodynamically stable may be treated with intravenous ibutilide (prolongs refractoriness of both AV node and accessory pathways) or procainamide (because of its effects on the atrial myocardium) (2). Intravenous amiodarone can be used if ibutilide or procainamide is unavailable, but these patients should be monitored closely because of the effects of amiodarone on the AV node. Hemodynamically unstable patients should undergo immediate cardioversion.
Figure 1.
Atrial Fibrillation in Wolff-Parkinson-White Syndrome
(A) Initial electrocardiogram showing atrial fibrillation with a rapid pre-excited ventricular response. The shortest pre-excited RR interval was 160 ms, indicating the potential of degeneration to ventricular fibrillation. Red circles show multiple different QRS complex configurations suggestive of conduction through an accessory pathway. (B) Electrocardiogram after synchronized direct-current cardioversion which showed sinus rhythm with a QRS complex configuration and delta waves (red arrows) typical of pre-excitation from a left lateral accessory pathway.
Footnotes
Both authors have reported that they have no relationships relevant to the contents of this paper to disclose.
References
- 1.Klein G.J., Bashore T.M., Sellars T.D., Pritchett E.L., Smith W.M., Gallagher J.J. Ventricular fibrillation in the Wolff-Parkinson-White syndrome. N Engl J Med. 1979;301:1080–1085. doi: 10.1056/NEJM197911153012003. [DOI] [PubMed] [Google Scholar]
- 2.Pediatric and Congenital Electrophysiology Society (PACES), Heart Rhythm Society (HRS), American College of Cardiology Foundation (ACCF) PACES/HRS expert consensus statement on the management of the asymptomatic young patient with a Wolff-Parkinson-White (WPW, ventricular preexcitation) electrocardiographic pattern. Heart Rhythm. 2012;9:1006–1024. doi: 10.1016/j.hrthm.2012.03.050. [DOI] [PubMed] [Google Scholar]