Supplemental Digital Content is available in the text.
Keywords: emergency department, erythroblasts, hematologic test, mortality, prognosis, sepsis
Abstract
OBJECTIVES:
Increase of nucleated RBCs in peripheral blood has been shown to be predictive of mortality in ICU patients. The aim of this study was to explore the prognostic value of nucleated RBCs in the first blood sample taken at admission to the emergency department from patients with suspected sepsis.
DESIGN:
Single-center prospective cohort study.
SETTING:
Emergency department.
PATIENTS:
One-thousand two-hundred thirty-one consecutive adult patients with suspected sepsis were included in a prospective quality register-based cohort study. Inclusion criteria were as follows: patients received in rapid response team with blood cultures taken and immediate antibiotics given in the emergency department.
Intervention:
Not applicable.
MEASUREMENT AND MAIN RESULTS:
Nucleated RBCs, Sequential Organ Failure Assessment score, Quick Sequential Organ Failure Assessment, Charlson Comorbidity Index, and commonly used laboratory tests measured in the emergency department were compared with 30-day mortality. Nvaucleated RBC counts were divided into five groups, called “Nucleated RBC score,” according to nucleated RBC count levels and analyzed with logistic regression together with the Sequential Organ Failure Assessment score and Charlson Comorbidity Index. Of the 262 patients with nucleated RBCs equal to or higher than the detection limit (0.01 × 109/L), 26% died within 30 days, compared with 12% of the 969 patients with nucleated RBCs below the detection limit (p < 0.0001). Mortality was significantly higher for each increase in Nucleated RBC score, except from score 2 to 3, and was 62% in the highest group. In multivariate logistic regression, odds ratios for 30-day mortality were as follows: Nucleated RBC score: 1.33 (95% CI, 1.13–1.56), Sequential Organ Failure Assessment score: 1.32 (1.29–1.56), and Charlson Comorbidity Index: 1.17 (1.09–1.25).
CONCLUSIONS:
Most patients with suspected sepsis in emergency department had undetectable nucleated RBCs at admission to the emergency department. However, increased nucleated RBCs significantly predicted 30-day mortality. Nucleated RBCs may provide additional prognostic information to Sequential Organ Failure Assessment score and other laboratory tests.
Sepsis is defined as life-threatening organ dysfunction caused by a dysregulated host response to infection (1). Sequential Organ Failure Assessment (SOFA) is a quantitative measure of organ dysfunction, using routinely measured variables (2). Six organs or organ systems are included in the score: respiratory, cardiovascular, coagulation, liver, renal, and CNS. Mortality increases with increasing SOFA score, both within the specific organ system and for total SOFA score (3, 4).
Nucleated RBCs (NRBCs) are RBC precursors that are normally not present at a detectable concentration in peripheral blood in adults. NRBCs are normally retained in the bone marrow (5) but may be released during severe hematopoietic stress and can be detected in the circulation during compensating hematopoiesis after severe blood loss or hemolysis (6, 7). However, in absence of acute anemia, their presence in peripheral blood appears to reflect pathophysiologic processes in bone marrow homeostasis. This may be mediated by hypoxemia and inflammation (8), the latter suggested by its association with proinflammatory cytokines (9), but no association with liver or renal failure (10).
Currently, circulating NRBCs can be measured reliably by some automated hematology analyzers at very low concentrations (11), and this development has opened renewed interest in NRBCs as a potential prognostic biomarker. Studies have described an association between circulating NRBCs and mortality in ICU patients (10, 12, 13), mortality after hospital discharge for ICU patients (14), and for mortality in ICU patients with surgical sepsis (15) and ARDS (16). However, most of these studies have analyzed the highest NRBC value found during the admittance, which is not necessarily useful as a predictor early in the admission. We hypothesized that NRBCs measured at a single time point in the emergency department (ED) would also be predictive of mortality.
Thus, the aim of this study was to investigate the prognostic value of circulating NRBCs in patients with suspected sepsis in the ED and to compare it with SOFA score, Charlson Comorbidity Index (CCI), and commonly used laboratory tests.
MATERIALS AND METHODS
Study Design and Participants
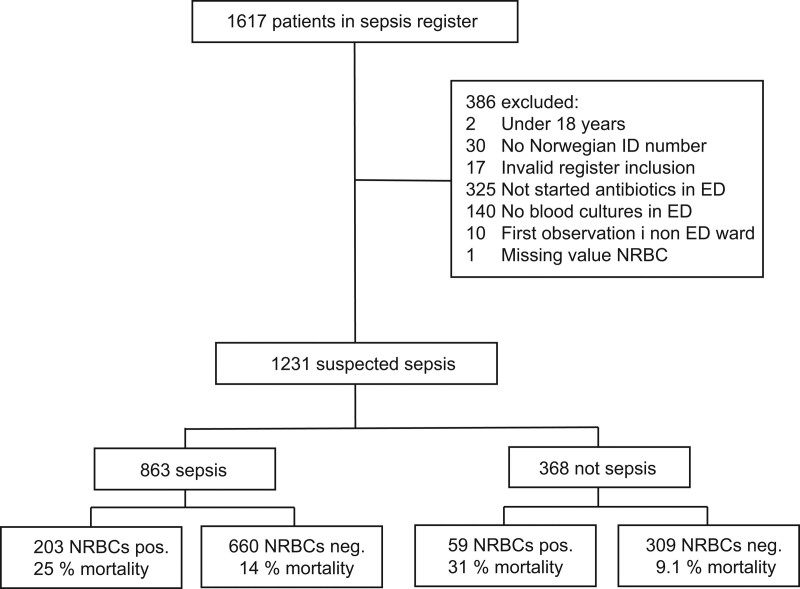
In the ED of an urban university hospital, all adult patients assessed in sepsis rapid response teams and patients with possible infections assessed in medical rapid response teams were consecutively included between May 15, 2017, and June 30, 2020, in a prospective quality register. As shown in Figure 1, patients 18 years or older with severe disease and suspected infection (defined as blood cultures taken and antibiotics given in the ED) were included in this study. Only variables from the first recorded contact of each patient were included. Mortality information was collected from the Norwegian National registry for up to 100 days after admittance; thus, foreign citizens without a Norwegian national identity number were excluded as postdischarge mortality could not be assessed. Incorrectly registered patients, or patients who had their primary clinical evaluation outside the ED, were excluded.
Figure 1.
Inclusion of patients. Confirmed sepsis from post hoc analysis (see Methods section). Invalid register inclusion: patients not assessed by the sepsis or medical rapid response teams. Nucleated RBCs (NRBCs) positive (pos.): greater than or equal to 0.01 × 109/L. ED = emergency department, neg. = negative.
Ethics Approval and Consent to Participate
The study was approved by the Regional Committee for Medical and Health Research Ethics of South-East Norway (approval number 30652). Informed consent was waived because of the strictly observational nature of the study. The sepsis quality register is approved by the hospital’s Data Protection Official (reference 2017/5382).
Diagnostic Assessments and Outcome
SOFA and Quick SOFA (qSOFA) were calculated based on the worst values from the first hour in the ED. The CNS assessment was based on the patients’ actual Glasgow Coma Scale (GCS), independent of cause. For example, patients sedated for intubation were scored to GCS3. The renal assessment was based solely on creatinine, not on urinary output, since the latter required longer observational time than possible in the ED. Furthermore, the highest SOFA score during the hospitalization was recorded and used in the classification of sepsis. Comorbidity was classified with CCI (17). Based on a post hoc evaluation, the patients were classified into four categories of 1) no infection, 2) possible infection but other diagnosis more probable, 3) probable infection, and 4) definite infection confirmed by microbiological findings (18). Patients classified with probable or definite infection with a maximum SOFA score during the hospital stay of greater than or equal to 2 were classified as confirmed sepsis. The outcome was 30-day mortality.
Laboratory Measurements
Blood was collected in Vacuette tubes (Greiner Bio One, Rainbach, Austria) by venipuncture or arterial cannulas mostly within 15 minutes of arrival at the ED and analyzed within 3 hours. Results from later blood collections were not included. NRBCs, hemoglobin, thrombocytes, and leukocytes were analyzed on Sysmex XN9000 (Sysmex, Kobe, Japan) in K2EDTA tubes. NRBC levels were not reported to the treating physician. However, it was laboratory procedure to report the presence of NRBCs as a comment when it exceeded 0.5% of the leukocyte count. There were no protocols for diagnostic or treatment actions following report of the presence of NRBCs, and we assume that it had no effect on the clinical decision-making. Serum tubes were analyzed on Roche Cobas 8000 c702 instruments (Roche Diagnostics, Risch-Rotkreuz, Switzerland) with reagents and calibrators from Roche. Reagents: Creatinine: creatinine plus v2. CRP: C-reactive protein gen3. Albumin: Albumin gen2reagent. Bilirubin: BIL-T Gen.3. LD: LDHI2. Lactate was analyzed in a heparinized blood gas syringe on a Roche Cobas b221 instrument (Roche Diagnostics), in most cases from arterial blood. d-dimer was measured in citrated plasma with STA-Liatest on STA-R evolution instruments (Diagnostica Stago, Asnières-sur-Seine, France) with upper reported limit 4 mg/L fibrinogen equivalent unit (FEU) up until April 5, 2020, and afterward with Innovance d-dimer (Siemens, Erlangen, Germany) on Sysmex CS-5100 (Sysmex) instruments with upper reported limit 35 mg/L FEU.
Statistics
The SOFA score of each organ system is scored in five categories by severity, with 0 representing normal organ function. We constructed a similar score for NRBCs with the following groups: score 0: 0.00 × 109/L, score 1: 0.01 × 109/L, score 2: 0.02 × 109/L, score 3: 0.03–0.07 × 109/L, score 4: greater than 0.07 × 109/L. The groups were adapted after initial data review with the aim of having a sufficient number of patients in each group. NRBCs were described as detectable when the concentration was greater than or equal to 0.01 × 109/L. Survival analysis was performed in Graphpad Prism 8 (Graphpad Software, San Diego, CA) with logrank test (Mantel Cox) test and logrank test for trend. Thirty-day survival rates in the NRBC groups were also compared with chi-square (Fisher exact test). Receiver operation characteristics (ROC) analysis was performed in MedCalc Statistical Software v16.1 (MedCalc Software, Ostend, Belgium) using the DeLong method, analysis was performed for one variable at a time. Patients with missing values were excluded from ROC analysis. The number of missing values for predictors is described in Supplemental Table 1 (http://links.lww.com/CCX/A733). Since the number of missing values was very low for the most important predictors, missing values were not imputed. Medians for demographic, clinical, and laboratory variables for patients with NRBC greater than or equal to 0.01 × 109/L and less than 0.01 × 109/L were compared with Mann-Whitney U tests and proportions with chi-square test in Graphpad Prism 8 (Graphpad Software). The presented p values were not corrected for multiple testing. Logistic regression was performed in MedCalc without removal of nonsignificant variables. All figures were made with Graphpad Prism.
RESULTS
Patient Characteristics
In total, 1,617 consecutive episodes from unique patients with suspected severe disease were included in the quality register in the study period. Of these, 1,231 patient episodes with suspected infection met all the inclusion criteria (Fig. 1). One-hundred eighty-nine patients died within 30 days of inclusion (15.4%), and 863 patients (70.0%) were classified as having confirmed sepsis, with probable or definite infection and SOFA score greater than or equal to 2 in a post hoc assessment. The patients without sepsis had infections without organ failure or various noninfectious conditions. The study participant characteristics are described in Table 1. One-hundred thirty-eight patients died in hospital, whereas 51 died after discharge within 30 days from admission. Three-hundred ninety-four patients (32%) were admitted to ICU during the hospital stay.
TABLE 1.
Demographic, Clinical, and Laboratory Variables
| Variables | NRBCs < 0.01× 109/L, n = 969 | NRBCs ≥ 0.01 × 109/L, n = 262 | pa |
|---|---|---|---|
| Women (%) | 44.6 | 42.4 | 0.52 |
| Age | 73 (56–73) | 72 (61–83) | 0.32 |
| Charlson Comorbidity Index | 2 (1–4) | 3 (1–5) | < 0.0001 |
| Hematologic disease (%) | 3.8 | 8.8 | 0.0009 |
| Malignancy (%) | 14.6 | 25.6 | < 0.0001 |
| SOFA score | 3 (2–4) | 4 (3–6) | < 0.0001 |
| qSOFA | 1 (1–2) | 2 (1–2) | < 0.0001 |
| Admitted to ICU (%) | 28.5 | 47.0 | < 0.0001 |
| Mechanical ventilation (%) | 6.2 | 10.3 | 0.018 |
| Bacteremia (%) | 22.4 | 26.0 | 0.23 |
| Confirmed sepsis (%) | 68.1 | 77.5 | 0.003 |
| 30-d mortality (%) | 12.4 | 26.4 | < 0.0001 |
| Platelets × 109/L | 232 (181–300) | 229 (174–317) | 0.75 |
| Bilirubin | 10 (7–16) | 12 (7–17) | 0.03 |
| Albumin, g/L | 39 (35–42) | 37 (32–40) | < 0.0001 |
| C-reactive protein, mg/L | 80 (29–187) | 84 (35–205) | 0.22 |
| Neutrophils × 109/L | 10.0 (7.0–13.7) | 9.55 (5.9–14.2) | 0.18 |
| Lymphocytes × 109/L | 0.9 (0.5–1.4) | 0.8 (0.4–1.4) | 0.38 |
| Neutrophil/lymphocyte ratio | 11.9 (6.5–20.4) | 11.2 (5.2–20.3) | 0.21 |
| Creatinine, µmol/L | 87 (67–121) | 110 (78–169) | < 0.0001 |
NRBC = nucleated RBC, SOFA = Sequential Organ Failure Assessment.
aMedians were compared with Mann-Whitney U tests and proportions with χ2.
Continuous variables expressed as medians (interquartile range). The following variables were missing for the included patients: Charlson Comorbidity Index n = 4, bilirubin (and SOFA liver) n = 6, platelets (and SOFA coagulation) n = 3, albumin n = 2, C-reactive protein n = 1, leukocyte differential count n = 46, and creatinine (and SOFA renal) n = 1.
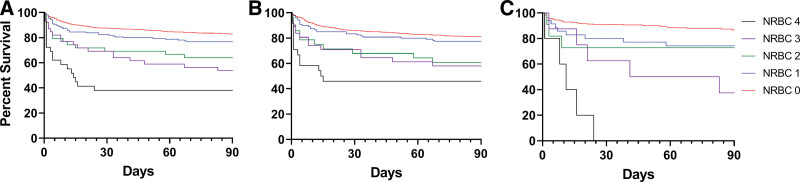
NRBCs in Relation to 30-Day Mortality
Mortality for patients grouped according to different levels of NRBCs is shown in Figure 2A for the whole cohort, and in Figure 2B and C for patients with and without confirmed sepsis, respectively. Mortality was significantly increased with higher NRBC levels in all patient groups (logrank test for trend p < 0.0001). There was no statistical difference for the 30-day mortality for patients with sepsis compared with patients without sepsis (logrank test p = 0.51). The 30-day mortality for patients with suspected sepsis with and without detectable NRBCs was 26.4% and 12.4%, respectively (p < 0.0001 Fisher exact test). The mortality rate in the highest NRBC group was 62.1%.
Figure 2.
Survival analysis according to concentration of nucleated RBC (NRBC) by NRBC score groups, defined as group 0 = 0.00 × 109/L, group 1 = 0.01 × 109/L, group 2 = 0.02 × 109/L, group 3 = 0.03–0.07 × 109/L, and group 4 = greater than 0.07 × 109/L. A, All patients suspected sepsis (n = 1231), (B) confirmed sepsis (n = 863), (C) not sepsis (n = 368).
The area under the curve (AUC) in ROC analysis for prediction of mortality with continuous NRBC results was 0.60 (95% CI, 0.57–0.63) for the whole study cohort and 0.58 (95% CI, 0.55–0.62) for patients with confirmed sepsis.
There were 60 patients with pre-existing hematologic disease of whom seven died (11.7%). There was no difference between NRBCs for survivors and nonsurvivors (Mann-Whitney U p = 0.54) for these patients. Since the proportion of patients with hematologic disease was only 4.9%, these patients had little impact on overall test characteristics of NRBCs. Thus, further analysis was performed without exclusion of patients with hematologic disease.
ROC analysis for 30-day mortality was also performed for the whole population of patients with suspected sepsis for SOFA, qSOFA, and laboratory tests previously described to have predictive power for mortality for patients with sepsis (Supplemental Table 1, http://links.lww.com/CCX/A733). The highest discrimination power (AUC, ROC) was found for SOFA score (0.73; 95% CI, 0.71–0.76), qSOFA (0.67; 0.65–0.70), CCI (0.65; 0.62–0.68), lactate (0.68; 0.65–0.70), lactate dehydrogenase (0.68; 0.65–0.70), d-dimer (0.66; 0.64–0.69), albumin (0.66; 0.63–0.69), and GCS (0.67; 0.64–0.69). The discrimination power of NRBCs was somewhat lower, but higher than for some of the laboratory tests underlying the SOFA score such as platelets (0.56, 0.53–0.59) and bilirubin (0.54, 0.51–0.57). In order to further examine the potential added value of NRBCs to SOFA and established laboratory tests predictive for mortality, we plotted individual results for variables with AUC greater than or equal to 0.55 grouped according to NRBC score in Supplemental Figure 1 (http://links.lww.com/CCX/A733); none of the variables had a high degree of association to NRBCs.
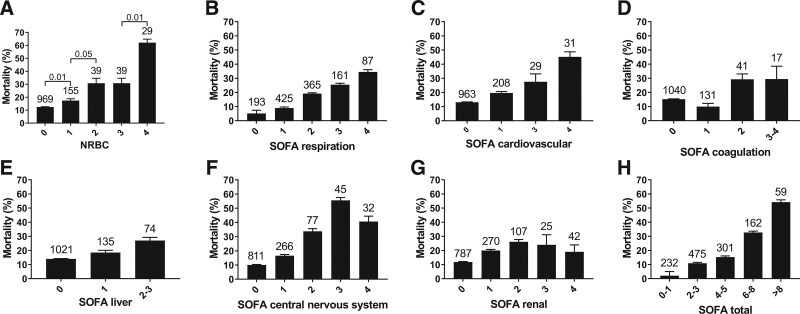
NRBCs Compared With SOFA for Prediction of Mortality
In the SOFA score, each organ system is scored from 0 to 4, where 0 represents normal organ function. We constructed a similar score for NRBCs (see Methods section). The 30-day mortality rate of the NRBC and the SOFA score groups are shown in Figure 3. Mortality was significantly higher for each increase in NRBC score, except from score 2 to 3. The mortality in the uppermost NRBC score 4 was 62.1%, which was considerably higher than in the score 4 categories of any of the SOFA components.
Figure 3.
A, Mean mortality grouped according to Nucleated RBC (NRBC) score. NRBC score 0 = 0.00 × 109/L, 1 = 0.01 × 109/L, 2 = 0.02 × 109/L, 3 = 0.03–0.07 × 109/L, 4 = greater than 0.07 × 109/L. B–G, Components of the Sequential Organ Failure Assessment (SOFA) score. H, Total SOFA score. Error bars represent 95% CIs for the percentage. Numbers above the bars show the number of patients in each group. Groups that contained less than 10 patients were classified together with a neighboring score category.
Logistic Regression Analysis of NRBC Score, SOFA, and CCI for Mortality
In Table 1, we showed that SOFA and CCI scores were higher for patients with detectable levels of NRBCs than for patients without detectable NRBCs. To investigate whether NRBC score had prognostic value independently of SOFA and CCI, we performed univariate logistic regression and multivariate logistic regression. In multivariate logistic regression, the NRBC categories (NRBC scores 0–4) were used as predictive variables in order for NRBCs to be on the same scale as the SOFA score (Table 2).
TABLE 2.
Logistic Regression Analysis
| Variables | SOFA Total/NRBC Score/CCI | |
|---|---|---|
| OR | ||
| Univariate | Multivariate | |
| SOFA (total) | 1.38 (1.30–1.47) | 1.32 (1.24–1.41) |
| CCI | 1.22 (1.15–1.30) | 1.17 (1.09–1.25) |
| NRBC score | 1.68 (1.46–1.94) | 1.33 (1.13–1.56) |
CCI = Charlson Comorbidity Index, NRBC = nucleated RBC, OR = odds ratio, SOFA = Sequential Organ Failure Assessment.
Univariate and multivariate ORs with 95% CIs from logistic regression to predict 30-d mortality.
In the univariate analysis, the odds ratio for NRBC score was 1.68 (95% CI, 1.46–1.94) which was higher than the SOFA score (1.38 [1.30–1.47]).
In the multivariate model, all variables (SOFA total, CCI, and NRBC scores) were retained with odds ratios that were significantly higher than 1.00. In this model, 1 point increase in the NRBC score had about the same predictive value as any other increase of 1 point in the SOFA score.
In the ROC analysis (Supplemental Table 1, http://links.lww.com/CCX/A733), the AUC for SOFA score was 0.73 (95% CI, 0.71–0.76). The AUC for the logistic regression model 1 was 0.77 (0.75–0.80). Thus, indicating that NRBCs and CCI might add prognostic information to SOFA score.
DISCUSSION
In this study, we investigated the prognostic value of NRBCs for 30-day mortality in patients with suspected sepsis in the ED. Although most patients had nondetectable levels of NRBCs, patients with elevated NRBCs had a markedly increased mortality risk. To our knowledge, this is the first study of NRBCs in patients with suspected sepsis in the ED. The prognostic value of NRBCs was greater than for several components of the SOFA score, with a relative mortality risk of 4.7 for the highest NRBC group compared with patients with nondetectable NRBCs (< 0.01 × 109/L). This increase in risk was of a similar magnitude to that previously found in ICU patients (10, 12).
Notably, our study indicated that the prognostic information from NRBCs is to a large extent independent both of components of the SOFA score, CCI, and commonly used laboratory tests. Thus, NRBCs appeared to add prognostic value to clinical scores and commonly used laboratory test in the ED, as previously described for later NRBC assessments in ICU patients (10, 12). The logistic regression analysis indicated slightly improved discrimination for a multivariable model combining SOFA score, CCI, and NRBC score compared with SOFA score alone. However, logistic regression is only one of many ways to combine predictive variables into multivariable predictive models. Development and validation of multivariable predictive models require a different study design (19). There are several suggested multivariable predictive models for patients with sepsis (20, 21), but to our knowledge none that include NRBCs. Thus, inclusion of NRBCs might improve existing predictive models.
There was no significant difference in the predictive value of NRBCs for patients who had sepsis confirmed in a post hoc evaluation, compared with patients who had other infectious or noninfectious condition. Thus, NRBC seems to be general prognostic marker, not specific for sepsis.
Various explanations for the association between NRBCs and mortality have been suggested: RBC production or release could increase due to hematopoietic signaling or hypoxia, or extramedullary production in the spleen could increase due to excessive inflammation-related signaling (10, 14). The SOFA score comprises evaluation of six organ systems but does not include the hematopoietic system. Bone marrow–derived platelets in septic patients are frequently low but usually related to activation of the coagulation system (22). Notably, we found no association between platelets and NRBCs in our study. Even though the pathophysiology is not clearly understood, we propose that NRBCs could be seen as a marker for a dysregulated hematopoietic system including RBC homeostasis. Increased NRBCs were not predictive of mortality in patients with previously known hematologic disease. Thus, NRBCs should not be used as a predictor for this group.
These new findings could have implications for future treatment of sepsis patients. The high mortality risk for patients with markedly elevated NRBCs in general at admittance could indicate need for close surveillance, perhaps even early admission to the ICU. Notably, one study argued that ICU patients with increased NRBCs should not be discharged to regular wards (12). If the mechanisms of the association between detectable NRBCs and mortality can be elucidated, new potential targets for specific management may be identified.
Our study has several strengths. It includes a large number of consecutive patients admitted with suspected sepsis with NRBCs measured at admission to the ED. Although data analysis was done retrospectively, all variables were entered consecutively into the quality register and with minimal missing data. There were few exclusion criteria, a high percentage of inclusion, and no patients lost to follow-up. The definition of suspicion of sepsis and sepsis was similar to that used in other studies. Thus, this cohort is likely to be representative of patients admitted with suspected sepsis elsewhere. To our knowledge, our study is the first to demonstrate the predictive value of NRBCs at a single measurement point at hospital admission. Previous studies from the ICU setting have classified patients into NRBC positive or negative by using NRBC results from the whole ICU stay and, in some cases, analyzed the predictive value using the highest NRBCs during the ICU stay (10, 12, 13).
There are also some weaknesses and questions on the generalizability of our findings. First, NRBCs are analyzed every time a sample is run on several common hematology instruments and is therefore in principle free of extra cost. However, clinicians and investigators should be aware that instruments may differ in the ability to count very low levels of NRBCs, and results may not be standardized across different instruments (11). With the increasing body of evidence for the importance of quantitative measurement of NRBCs, instrument manufacturers should be encouraged to improve and standardize NRBC measurements. Second, no serial measurements of NRBCs were performed as in some previous studies (23, 24). Thus, we were not able to investigate whether day-to-day changes in NRBCs affect the mortality risk.
CONCLUSIONS
Elevated levels of NRBCs were highly predictive for 30-day mortality in patients admitted to the ED with suspected sepsis. In hospitals with the NRBC method available, laboratories should be encouraged to report NRBCs to facilitate more studies of this biomarker. Future prospective observational and possibly interventional studies may be warranted, where level of care could be based on predicted risk estimates that include NRBCs.
ACKNOWLEDGMENTS
We would like to thank all collaborators in the study. The sepsis registry was initiated in close collaboration with Anders B. Martinsen (MD) and has been maintained by Elisabet Trydal and Marianne Leegaard. Valeria Vitelli (Department of Biostatistics, University of Oslo) was consulted for the statistical analysis; any errors are the responsibility of the authors.
Supplementary Material
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccejournal).
Drs. Amundsen and Holten contributed to conceptualization. Drs. Amundsen, Binde, Christensen, and Holten contributed to formal analysis and investigation. Drs. Amundsen and Binde contributed to writing—original draft preparation. All authors contributed to writing—review and editing. Drs. Amundsen, Klingenberg, Kvale, and Holten contributed to resources. All authors read and approved the final article.
Supported, in part, by Oslo University Hospital.
The authors have disclosed that they do not have any conflicts of interest.
Due to the nature of this research, with data from a quality register with waived consent, data are not available to do ethical and legal restrictions. Parts of the dataset can be made available from the corresponding author on reasonable request.
This work was performed at Oslo University Hospital.
REFERENCES
- 1.Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016; 315:801–810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vincent JL, Moreno R, Takala J, et al. The SOFA (sepsis-related organ failure assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996; 22:707–710 [DOI] [PubMed] [Google Scholar]
- 3.Vincent JL, de Mendonça A, Cantraine F, et al. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: Results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med. 1998; 26:1793–1800 [DOI] [PubMed] [Google Scholar]
- 4.Raith EP, Udy AA, Bailey M, et al. ; Australian and New Zealand Intensive Care Society (ANZICS) Centre for Outcomes and Resource Evaluation (CORE). Prognostic accuracy of the SOFA score, SIRS criteria, and qSOFA score for in-hospital mortality among adults with suspected infection admitted to the intensive care unit. JAMA. 2017; 317:290–300 [DOI] [PubMed] [Google Scholar]
- 5.Schwartz SO, Stansbury F. Significance of nucleated red blood cells in peripheral blood; analysis of 1,496 cases. J Am Med Assoc. 1954; 154:1339–1340 [DOI] [PubMed] [Google Scholar]
- 6.Danise P, Maconi M, Barrella F, et al. Evaluation of nucleated red blood cells in the peripheral blood of hematological diseases. Clin Chem Lab Med. 2011; 50:357–360 [DOI] [PubMed] [Google Scholar]
- 7.May JE, Marques MB, Reddy VVB, et al. Three neglected numbers in the CBC: The RDW, MPV, and NRBC count. Cleve Clin J Med. 2019; 86:167–172 [DOI] [PubMed] [Google Scholar]
- 8.Kuert S, Holland-Letz T, Friese J, et al. Association of nucleated red blood cells in blood and arterial oxygen partial tension. Clin Chem Lab Med. 2011; 49:257–263 [DOI] [PubMed] [Google Scholar]
- 9.Stachon A, Bolulu O, Holland-Letz T, et al. Association between nucleated red blood cells in blood and the levels of erythropoietin, interleukin 3, interleukin 6, and interleukin 12p70. Shock. 2005; 24:34–39 [DOI] [PubMed] [Google Scholar]
- 10.Stachon A, Holland-Letz T, Kempf R, et al. Poor prognosis indicated by nucleated red blood cells in peripheral blood is not associated with organ failure of the liver or kidney. Clin Chem Lab Med. 2006; 44:955–961 [DOI] [PubMed] [Google Scholar]
- 11.Da Rin G, Vidali M, Balboni F, et al. Performance evaluation of the automated nucleated red blood cell count of five commercial hematological analyzers. Int J Lab Hematol. 2017; 39:663–670 [DOI] [PubMed] [Google Scholar]
- 12.Stachon A, Segbers E, Holland-Letz T, et al. Nucleated red blood cells in the blood of medical intensive care patients indicate increased mortality risk: A prospective cohort study. Crit Care. 2007; 11:R62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Macichová M, Grochová M, Rácz O, et al. Improvement of mortality prediction accuracy in critically ill patients through combination of SOFA and APACHE II score with markers of stress haematopoiesis. Int J Lab Hematol. 2020; 42:796–800 [DOI] [PubMed] [Google Scholar]
- 14.Purtle SW, Horkan CM, Moromizato T, et al. Nucleated red blood cells, critical illness survivors and postdischarge outcomes: A cohort study. Crit Care. 2017; 21:154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Desai S, Jones SL, Turner KL, et al. Nucleated red blood cells are associated with a higher mortality rate in patients with surgical sepsis. Surg Infect (Larchmt). 2012; 13:360–365 [DOI] [PubMed] [Google Scholar]
- 16.Menk M, Giebelhäuser L, Vorderwülbecke G, et al. Nucleated red blood cells as predictors of mortality in patients with acute respiratory distress syndrome (ARDS): An observational study. Ann Intensive Care. 2018; 8:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987; 40:373–383 [DOI] [PubMed] [Google Scholar]
- 18.Klein Klouwenberg PM, Cremer OL, van Vught LA, et al. Likelihood of infection in patients with presumed sepsis at the time of intensive care unit admission: A cohort study. Crit Care. 2015; 19:319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moons KG, Altman DG, Reitsma JB, et al. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): Explanation and elaboration. Ann Intern Med. 2015; 162:W1–73 [DOI] [PubMed] [Google Scholar]
- 20.Liaw PC, Fox-Robichaud AE, Liaw KL, et al. Mortality risk profiles for sepsis: A novel longitudinal and multivariable approach. Crit Care Explor. 2019; 1:e0032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seo MH, Choa M, You JS, et al. Hypoalbuminemia, low base excess values, and tachypnea predict 28-day mortality in severe sepsis and septic shock patients in the emergency department. Yonsei Med J. 2016; 57:1361–1369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bedet A, Razazi K, Boissier F, et al. Mechanisms of thrombocytopenia during septic shock: A multiplex cluster analysis of endogenous sepsis mediators. Shock. 2018; 49:641–648 [DOI] [PubMed] [Google Scholar]
- 23.Shah R, Reddy S, Horst HM, et al. Getting back to zero with nucleated red blood cells: Following trends is not necessarily a bad thing. Am J Surg. 2012; 203:343–345 [DOI] [PubMed] [Google Scholar]
- 24.Stachon A, Kempf R, Holland-Letz T, et al. Daily monitoring of nucleated red blood cells in the blood of surgical intensive care patients. Clin Chim Acta. 2006; 366:329–335 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.