Abstract
Chest pain is commonly reported in emergency departments, and a thorough clinical history is important in distinguishing the etiology. This case highlights Kounis syndrome, a histamine-mediated coronary vasospasm leading to myocardial injury, due to scombroid fish poisoning. (Level of Difficulty: Beginner.)
Key Words: coronary vasospasm, fish allergy, Kounis syndrome, myocardial infarction with nonobstructive coronary arteries, scombrotoxicosis
Abbreviations and Acronyms: ECG, electrocardiogram; IgE, immunoglobulin E; SFP, scombroid fish poisoning
Graphical abstract
Chest pain is commonly reported in emergency departments, and a thorough clinical history is important in distinguishing the etiology. This case highlights…
A 53-year-old man presented to the emergency department with reports of severe substernal chest pain with radiation to the back and acute nonexertional dyspnea of 2 h duration. Symptoms also included facial flushing, subjective warmth, and acute-onset profuse watery diarrhea. His symptoms started ∼1 h after ingestion of home-cooked tuna steaks. His wife consumed a small portion of tuna and also experienced mild abdominal bloating and diarrhea. Initial vital signs revealed hypotension (88/48 mm Hg) and tachypnea. Physical examination revealed facial erythema, diffuse nonurticarial rash of the upper torso, clear lung sounds without stridor, and a normal cardiac examination. His abdomen was soft but distended with diffuse tenderness to palpation and tympanic to percussion.
Learning Objectives
-
•
To consider rare etiologies in the differential diagnosis of chest pain in the appropriate clinical context.
-
•
To recognize Kounis syndrome in patients presenting with angina and allergy-like symptoms.
Medical History
The patient’s medical history was significant for hypertension, alcohol use disorder (red wine), and obstructive sleep apnea; he had no known food allergies. He did not take any medications, and he denied any tobacco or illicit substance use history. His family history was noncontributory.
Differential Diagnosis
Severe allergic reaction, acute coronary syndrome, acute aortic syndrome, anaphylaxis, scombroid reaction, septic shock, and illicit substance intoxication were considered in the differential diagnosis at initial presentation.
Investigations
Results of the patient’s initial blood work were significant for lactatemia (6.7 mmol/l), absence of leukocytosis or eosinophilia, negative initial cardiac troponin-T, and an ethanol level of 0.14 mg/dl. Whole blood histamine levels obtained 6 h after the tuna ingestion were elevated to 1,347 nmol/l. Urine toxicology was negative for any illicit substances. The patient’s initial electrocardiogram (ECG) showed diffuse ST-segment depressions, with an augmented vector right elevation of 1.5 mm (Figure 1). A computed tomography scan of the aorta ruled out aortic dissection.
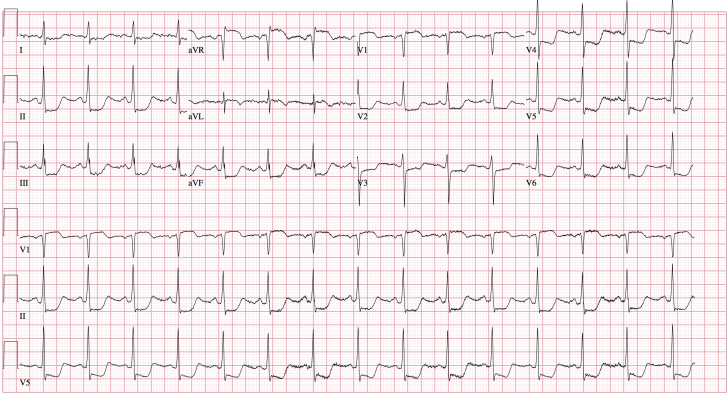
Figure 1.
Initial ECG on Patient Presentation
Electrocardiogram (ECG) showing diffuse ST-segment deviations, in the setting of chest pain, resulted in the patient receiving urgent coronary angiography. This ECG was obtained before administration of intramuscular epinephrine.
Management
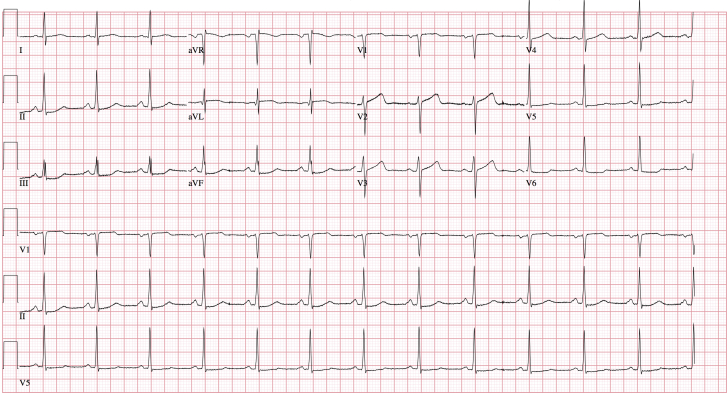
In the emergency department, the patient received intravenous fluid resuscitation, famotidine, and intravenous steroids for assumed allergic reaction. Despite fluid resuscitation, the patient remained hypotensive and subsequently received 0.3 mg of intramuscular epinephrine for anaphylaxis. Although the patient’s blood pressure improved to 121/58 mm Hg, his chest pain continued to worsen. Given the concern for acute coronary syndrome, the patient was taken for urgent coronary angiography, which showed nonobstructed coronary arteries (Figure 2) without visualized coronary spasms. During hospitalization, his ECGs showed improving ST-segment deviations and eventual normalization (Figure 3). In addition, results of the patient’s laboratory testing were significant for a troponin-T level that peaked at 0.19 ng/ml and a histamine level that normalized (222 nmol/l) by the next morning. All symptoms resolved within 18 h of presentation. His pre-discharge echocardiogram demonstrated a left ventricular ejection fraction of 69% with no wall motion abnormalities.
Figure 2.

Coronary Angiography
Right anterior oblique (RAO)–cranial view demonstrating nonobstructed left coronary arteries.
Figure 3.
ECG With Normalization
ST-segment deviations regressed without interventions, electrocardiogram (ECG) taken pre-discharge (∼36 h after tuna ingestion).
The patient’s final diagnosis was vasospastic angina secondary to scombroid fish poisoning (SFP). More specifically, he was determined to have a myocardial infarction with nonobstructive coronary arteries categorized as a type 2 myocardial infarction secondary to coronary vasospasm (1). He was initiated on amlodipine for hypertension, counseled on safe alcohol use, and discharged home with outpatient follow-up.
Discussion
This case report highlights a rare manifestation of SFP presenting as chest pain. SFP is a foodborne illness occurring after ingestion of improperly stored histamine-contaminated fish that results in symptoms similar to that of seafood allergies, and it is often misdiagnosed as such (2). Scombroid fish species (including tuna, mackerel, skipjack, bonito, and marlin) were initially implicated in this food toxemia; however, it is now recognized that non-scombroid species can also cause scombrotoxicosis. The U.S. Food and Drug Administration has mandated regulations for rapid cooling of captured fish to ensure seafood safety; however, SFP remains the most common fish-related illness worldwide. The pathophysiology of SFP involves bacterial overgrowth in fish leading to rapid bacterial conversion of histidine to heat-stable histamine (resistant to cooking, canning, or freezing). After ingestion of a large quantity of histamine, diamine oxidase (the enzyme responsible for histamine deactivation) can be overwhelmed, leading to elevated levels of histamine in the blood and subsequent symptoms. Symptoms of SFP usually include flushing, rash, abdominal pain, diarrhea, headache, palpitations, chest tightness, and a peppery or metallic taste, and they can rarely manifest as hypotension, anaphylaxis, or myocardial infarction (3). The severity of symptoms depends on the quantity of histamine ingested, rate of inactivation, and individual sensitivity. Furthermore, alcohol (particularly red wine) can increase histamine levels due to histamine content and inhibition of diamine oxidase (4). The diagnosis of SFP is primarily made based on clinical presentation such as exposure to potentially spoiled fish, cluster of individuals with similar complaints, and allergy-like symptoms with no previous allergy to fish, consistent with the current case. In addition, the patient had an elevated alcohol level that likely compounded his histaminosis and contributed to the severity of his symptoms. Although the gold standard of diagnosis is histamine quantification in the suspected fish, no samples were available from either the patient or his local market in this case. Management of mild scombroid toxicity focuses on supportive care, and the duration of illness is typically <24 h (2). For moderate symptoms, histamine (H1- and H2-receptor) antagonists can be used for symptom relief. No recommendations exist for management of severe SFP, and patients are usually treated as in anaphylaxis. Intramuscular epinephrine is a first-line agent for anaphylaxis (including anaphylactoid reactions) per consensus guidelines (5). Notably, because SFP is a non–immunoglobulin E (IgE)-mediated phenomenon, fish abstention is not needed, and the patient should not be labeled with a fish allergy.
The patient’s cluster of symptoms is consistent with Kounis syndrome. Allergic angina (later renamed Kounis syndrome) was first characterized in 1991 as a spectrum of disease with concomitant occurrence of acute coronary syndrome with the presence of a hypersensitivity reaction (6). The definitions, etiologies, and pathophysiology were further expanded and now include 3 distinct variants. Type I variant, as with the current case, is characterized as coronary spasm (endothelial dysfunction or microvascular angina) in patients with normal or nearly normal coronary arteries, with a subset of individuals progressing to myocardial injury and raised cardiac enzymes levels. The underlying pathogenesis in Kounis syndrome typically revolves around IgE-mediated stimulation of inflammatory cells (e.g., mast cells, basophils) with subsequent degranulation and release of various cellular mediators, including histamine, chemokines, neutral proteases, tryptase, cytokines, and various arachidonic acid products. Although SFP is not an IgE-mediated process, the causative agent of symptoms is histamine, which is closely associated with coronary vasoconstriction (7). Exogenous histamine, as in scombrotoxicosis, plays a critical role in the same proposed pathophysiology of Kounis syndrome (6). The postulated mechanism of the ECG changes seen in the current case, consistent with ischemia, is due to elevated histamine levels leading to diffuse coronary vasoconstriction.
Follow-Up
The patient remained asymptomatic with no further anginal symptoms at 6-week follow-up in the outpatient setting. His blood pressure was controlled, and he made lifestyle modifications to reduce his risk for future cardiovascular disease.
Conclusions
This case report is a reminder to consider rare etiologies of chest pain with an appropriate clinical history. Although SFP is a common foodborne illness worldwide, it is rarely associated with chest pain. It is proposed that the histamine ingestion (from SFP) led to coronary vasospasm resulting in the patient’s symptoms and diffuse ST-segment depressions and augmented vector right elevation as seen on his initial ECG. Subsequently, the patient was taken urgently for coronary angiography, which revealed nonobstructive coronary arteries. This case underscores the importance of recognizing anaphylactic (and anaphylactoid) reactions accompanied by angina that may represent Kounis syndrome. Further research needs to be conducted regarding the efficacy of therapies in Kounis syndrome, particularly when caused by scombroid poisoning due to its unique pathophysiology. Elucidation of the exact mechanism of scombroid poisoning and its varying effects on the cardiovascular system (peripheral vasodilation, vascular permeability, and coronary vasospasm) may help improve our understanding of cardiovascular collapse as seen in anaphylaxis (8).
Footnotes
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
References
- 1.Thygesen K., Alpert J.S., Jaffe A.S. Fourth universal definition of myocardial infarction (2018) J Am Coll Cardiol. 2018;72:2231–2264. doi: 10.1016/j.jacc.2018.08.1038. [DOI] [PubMed] [Google Scholar]
- 2.Feng C., Teuber S., Gershwin M.E. Histamine (scombroid) fish poisoning: a comprehensive review. Clin Rev Allergy Immunol. 2016;50:64–69. doi: 10.1007/s12016-015-8467-x. [DOI] [PubMed] [Google Scholar]
- 3.Hungerford J.M. Scombroid poisoning: a review. Toxicon. 2010;56:231–243. doi: 10.1016/j.toxicon.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 4.Maintz L., Novak N. Histamine and histamine intolerance. Am J Clin Nutr. 2007;85:1185–1196. doi: 10.1093/ajcn/85.5.1185. [DOI] [PubMed] [Google Scholar]
- 5.Simons F.E.R., Ebisawa M., Sanchez-Borges M. 2015 update of the evidence base: World Allergy Organization anaphylaxis guidelines. World Allergy Organiz J. 2015;8:32. doi: 10.1186/s40413-015-0080-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kounis N.G. Kounis syndrome: an update on epidemiology, pathogenesis, diagnosis and therapeutic management. Clin Chem Lab Med. 2016;54:1545–1559. doi: 10.1515/cclm-2016-0010. [DOI] [PubMed] [Google Scholar]
- 7.Sakata Y., Komamura K., Hirayama A. Elevation of the plasma histamine concentration in the coronary circulation in patients with variant angina. Am J Cardiol. 1996;77:1121–1126. doi: 10.1016/s0002-9149(96)00147-6. [DOI] [PubMed] [Google Scholar]
- 8.Kounis N.G., Cervellin G., Koniari I. Anaphylactic cardiovascular collapse and Kounis syndrome: systemic vasodilation or coronary vasoconstriction? Ann Transl Med. 2018;6:332. doi: 10.21037/atm.2018.09.05. [DOI] [PMC free article] [PubMed] [Google Scholar]