Abstract
We discuss an unusual case of a patient who initially presented with apparent commotio cordis but returned several months later with spontaneous wide complex tachycardia. This case highlights the importance of investigation of survivors of commotio cordis, especially if atypical, to determine if there is underlying cardiac disease. (Level of Difficulty: Beginner.)
Key Words: commotio cordis, electrophysiological study, implantable cardioverter-defibrillator, ventricular tachycardia
Abbreviations and Acronyms: CMR, cardiac magnetic resonance; EPS, electrophysiological study; ICD, implantable cardioverter-defibrillator; LGE, late gadolinium enhancement; LV, left ventricular; VF, ventricular fibrillation; VT, ventricular tachycardia
Graphical abstract

We discuss an unusual case of a patient who initially presented with apparent commotio cordis but returned several months later with recurrent wide…
History of Presentation
A 35-year-old professional soccer player was struck in the chest by a ball from a close distance while playing in a practice game. He experienced dizziness but remained conscious for several minutes before he collapsed. A staff member immediately started cardiopulmonary resuscitation until an emergency medical team arrived. The first documented rhythm was sustained monomorphic ventricular tachycardia (VT), which deteriorated to ventricular fibrillation (VF) (Figure 1). Four electrical shocks were delivered with restoration of sinus rhythm and full neurological recovery.
Learning Objectives
-
•
To understand the importance of performing a comprehensive evaluation for underlying cardiac pathology in survivors of apparent commotio cordis, including CMR and EPS if a scar exists.
-
•
To recognize an additional possible mechanism for atypical commotio cordis, in which a blunt trauma to the chest triggers ventricular arrhythmia within an existing myocardial scar. In patients presenting with this type of mechanism, ICD implantation may be required.
Figure 1.
Initial Cardiac Rhythm Upon Arrival of the Emergency Medical Team
Sustained monomorphic ventricular tachycardia that deteriorated into ventricular fibrillation.
On admission to the intensive cardiac care unit, the patient was alert and oriented. His physical examination and vital signs were normal.
Medical History
The patient is a professional healthy athlete, without any significant medical history and no family history of cardiac disease or sudden cardiac death. A routine echocardiography performed 2 years earlier was within normal limits.
Differential Diagnosis
The differential diagnoses are commotio cordis, contusio cordis, and other causes of sudden cardiac death among athletes, including hypertrophic cardiomyopathy, arrhythmogenic right ventricular dysplasia, ischemic heart disease, anomalous coronaries, myocarditis, and inherited arrhythmia disorders (e.g., congenital long QT syndrome, Brugada syndrome, Wolff-Parkinson-White syndrome).
Investigations
An electrocardiogram showed sinus rhythm, incomplete right bundle branch block, and ST-T changes in the inferior and precordial leads that normalized in the following days. Results of blood tests revealed elevated high-sensitivity cardiac troponin-T of 283 ng/l (normal range, 0 to 14 ng/l). Transthoracic echocardiography demonstrated moderate left ventricular (LV) systolic dysfunction with an ejection fraction of 40%, minimal segmental variation, mildly hypokinetic right ventricular apex, and minimal pericardial effusion around the right ventricular apex. Coronary angiography revealed normal coronary arteries.
Cardiac magnetic resonance (CMR) performed 5 days later revealed mild biventricular dilatation, normal LV wall thickness with mild systolic dysfunction (LV ejection fraction 49%), and inferolateral wall hypokinesis. The right ventricle was mildly hypokinetic, with no evidence of dyskinesia or aneurysm. CMR criteria for arrhythmogenic right ventricular dysplasia were not fulfilled. Confluent subepicardial late gadolinium enhancement (LGE) was noted in the lateral and inferolateral walls of the left ventricle, corresponding with the wall motion abnormality.
Management
During hospitalization, the patient remained asymptomatic with no further documented arrhythmias. Implantable cardioverter-defibrillator (ICD) implantation was considered but was ultimately not performed due to the apparent clinical diagnosis of commotio cordis, despite the evidence of LGE. The patient was instructed to avoid intense exercise and refrain from competitive sports. Upon discharge, he began a cardiac rehabilitation program.
History of Presentation–continued
Nine months after the initial presentation, while the patient was walking on the soccer field as an assistant coach, he suddenly felt palpitations, along with weakness and dizziness. An emergency medical team was immediately called, documenting regular wide complex tachycardia of 230 beats/min that terminated after 3 consecutive rapid premature ventricular contractions, followed by atrial fibrillation and spontaneous conversion to sinus rhythm (Figure 2). A 12-lead electrocardiogram was normal, and results of blood tests revealed a mildly elevated high-sensitivity cardiac troponin T level of 36 ng/l. Transthoracic echocardiography showed normal biventricular systolic function with mild hypokinesis of the posterior wall.
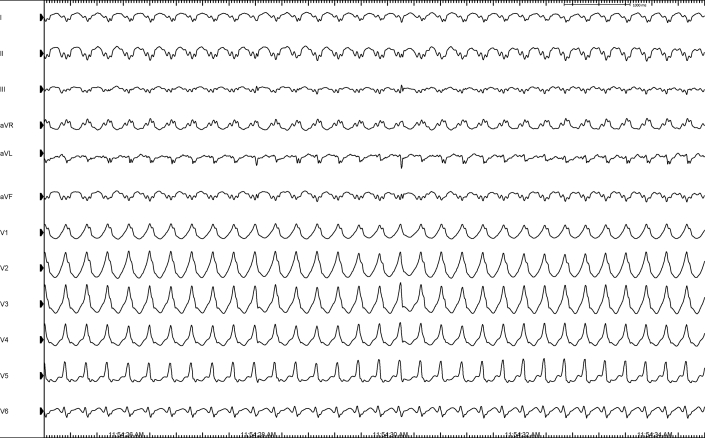
Figure 2.
Initial Electrocardiogram of the Second Event
Wide complex tachycardia at a cycle length of 280 ms, terminated after 3 consecutive premature complexes. Atrial fibrillation is noted afterward.
Given a wide complex tachycardia and the patient’s history, an electrophysiological study (EPS) was performed, with induction of sustained monomorphic VT by double extrastimuli delivered from the right ventricular apex at a basic cycle length of 500 ms and 2 extrastimuli of 230 and 220 ms, terminated by right ventricular overdrive pacing. The arrhythmia was consistent with the clinical arrhythmia documented by the emergency medical team (Figure 3). Subsequently, a dual chamber ICD was implanted concomitant with beta-blocker treatment. During 9 months of follow-up, he remained asymptomatic with no evidence of further arrhythmias.
Figure 3.
Sustained Monomorphic VT Induced by Programmed Electrical Stimulation
Note the similarity between lead II of the inducible ventricular tachycardia (VT) and lead II of the spontaneous arrhythmia (see Figure 2).
Discussion
The rare phenomenon, in which a nonpenetrating blow to the chest results in sudden cardiac death in the absence of cardiac damage, is known as commotio cordis. It is a significant cause of sudden cardiac death in athletes, mainly in adolescent male subjects (1).
An experimental model of commotio cordis has shown that the typical arrhythmia induced by a chest blow is VF. Self-limited VF and transient heart block were also observed. Transient heart block is typically seen with higher velocity impacts that cause structural damage (2). There are several critical variables in the induction of the arrhythmia, including the location, velocity, and shape of the impact object. The most important variable is the timing of impact relative to the cardiac cycle. Only impacts occurring during the 20- to 40-ms window on the upslope of the T-wave cause VF (1,2). In a suggested mechanism, the adenosine triphosphate–sensitive potassium channel is activated by the chest blow, causing alteration in repolarization and eventually VF. It is debatable if there is a component of individual susceptibility to commotio cordis (3).
Commotio cordis is to be distinguished from contusio cordis, in which a significant blunt chest trauma causes structural cardiac damage such as contusion of myocardial muscle, rupture of a cardiac chamber, or disruption of a heart valve, mostly due to motor vehicle accidents.
In the current case, there was no significant structural cardiac or chest injury. The transient ventricular dysfunction could be consistent with post-resuscitation myocardial dysfunction that develops after successful resuscitation from cardiac arrest as previously described. Furthermore, CMR performed a few days later did not show any evidence of acute myocardial changes that represent cardiac contusion, such as myocardial edema or focal delayed hyperenhancement (4).
In this unique case, the initial documented arrhythmia was sustained monomorphic VT that deteriorated into VF (Figure 1), followed by a second episode of spontaneous sustained monomorphic VT 9 months later (Figure 2). The negative QRS complexes in the inferior and lateral leads during the VT, are indicative of the VT origin, which is consistent with the areas of LGE seen in the CMR. Given a monomorphic VT, inducibility by ventricular extrastimuli in EPS, and evidence of LGE, it seems that the mechanism of arrhythmia in the current case is re-entrant arrhythmia within an old myocardial scar, rather than a typical commotio cordis.
Notably, there are also several clinical features that are not consistent with typical commotio cordis. The patient was 35 years old, which is older than the common age range in commotio cordis (1). Furthermore, whereas the classic presentation in commotio cordis is immediate collapse, this patient remained conscious for several minutes before collapsing, which is consistent with the presenting arrhythmia that was not VF. Ultimately, although first presented with a ventricular arrhythmia following a direct hit to the chest, he experienced a second spontaneous ventricular arrhythmia several months later (5).
Because the initial documented arrhythmia was sustained monomorphic VT that deteriorated to VF, the authors hypothesize that the mechanism of the arrhythmia in this case is a re-entrant VT originating from an old myocarditis-related scar, triggered by a blunt hit to the chest.
Follow-Up
The patient had no further arrhythmias over the 1-year follow-up.
Conclusions
The current case shows another possible mechanism for the phenomenon in which a nonpenetrating blow to the chest results in sudden cardiac arrest. The mechanism involved a re-entrant VT originating from an old myocardial scar, triggered by a blunt hit to the chest.
It also highlights the importance of performing a comprehensive evaluation for underlying cardiac pathology in survivors of commotio cordis, especially if atypical, including EPS if there are signs of myocardial scar. ICD implantation should be considered in these cases.
Footnotes
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Informed consent was obtained for this case.
References
- 1.Maron B.J., Estes N.A., 3rd Commotio cordis. N Engl J Med. 2010;362:917. doi: 10.1056/NEJMra0910111. [DOI] [PubMed] [Google Scholar]
- 2.Link M.S. Commotio cordis: ventricular fibrillation triggered by chest impact-induced abnormalities in repolarization. Circ Arrhythm Electrophysiol. 2012;5:425. doi: 10.1161/CIRCEP.111.962712. [DOI] [PubMed] [Google Scholar]
- 3.Alsheikh-Ali A.A., Madias C., Supran S., Link M.S. Marked variability in susceptibility to ventricular fibrillation in an experimental commotio cordis model. Circulation. 2010;122:2499. doi: 10.1161/CIRCULATIONAHA.110.955336. [DOI] [PubMed] [Google Scholar]
- 4.Vago H., Toth A., Apor A., Maurovich-Horvat P., Toth M., Merkely B. Images in cardiovascular medicine. Cardiac contusion in a professional soccer player: visualization of acute and late pathological changes in the myocardium with magnetic resonance imaging. Circulation. 2010;121:2456–2461. doi: 10.1161/CIRCULATIONAHA.109.917724. [DOI] [PubMed] [Google Scholar]
- 5.Maron B.J., Link M.S. Recurrent commotio cordis: déjà vu. Heart Rhythm Case Rep. 2015;1:249. doi: 10.1016/j.hrcr.2015.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]