Abstract
Human hydatid disease is still endemic in pastoral and rangeland areas, with temperate climate, mainly in the southern shore of the Mediterranean, particularly in the Maghreb countries. Renal localization is rare although it is the most frequent site of the urinary tract. Its clinical evolution remains silent for long time, and the diagnosis is often elusive for years. Renal hydatid cysts may pose a problem of differential diagnosis. Our case concerns a renal hydatidosis misdiagnosed as a xanthogranulomatous pyelonephritis, treated by total nephrectomy.
INTRODUCTION
Hydatidosis is a cosmopolitan anthropozoonosis caused by a tapeworm eggs (Echinococcus granulosis), living in the gut of the dogs and wild canines. Renal hydatidosis is rare, even in endemic countries, and may come across diagnostic difficulties. Histopathological study is sometimes the only way to have a certain diagnosis of the hydatid origin of some renal lesions.
CASE REPORT
A 36-year-old woman, working as a teacher, and living in an urban zone with prolonged contact with a domestic dog, has presented right lumbar pain with fever evolving for 10 days. No hydaturia was reported. The patient had no significant medical history.
Clinical examination revealed fever, and right lumber sensibility, with no palpable mass or right lumber contact.
Laboratory investigations revealed raised inflammatory markers. Renal function was normal and there was no hyper-eosinophilia. Cytobacteriological examination of the urine was positive to Escherishia coli.
An abdominal computed tomography (CT) scan revealed an obstructive right staghorn calculus measuring 27 mm with homolateral hydronephrosis and infiltration of perirenal fat. Renal and para renal multilocular collections were described: one pararenal collection measuring 50 mm, a second collection was located in the right paracolic gutter and measuring 23 × 20 mm. An exophytic multilocular renal collection was also described, with calcifications and well-defined wall measuring 67 mm (Fig. 1).
Figure 1 .
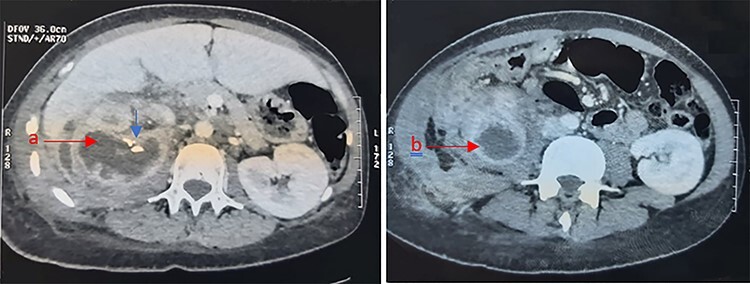
Abdominal CT showing a right renal multilocular collection, measuring 67 mm (a) with calcifications (Blue arrow) and a right para renal collection measuring 50 mm (b).
The radiologists concluded to a xanthogranulomatous pyelonephritis with renal abscess.
Antibiotic therapy was initiated and the patient had percutaneous drainage of the superficial abscess. The drained liquid was purulent and its bacterial analysis revealed the same bacteria: E. coli. Clinical and biological evolution was uneventful. The patient was discharged after 6 days on oral antibiotics and analgesics.
Three months later, the patient was hospitalized. An abdominal CT was performed and the right kidney was described by as non-functional with regression of the renal abscess. Nephrectomy of the right kidney was performed. The surgical procedure was performed by lumbotomy. The nephrectomy was difficult since the peri renal fat was infiltrated because of the history of pyelonephritis, 3 months ago.
Interstingly, anatomopathological examination of the operative specimens reported the aspect of hydatid renal cyst (Fig. 2a and b).
Figure 2 .
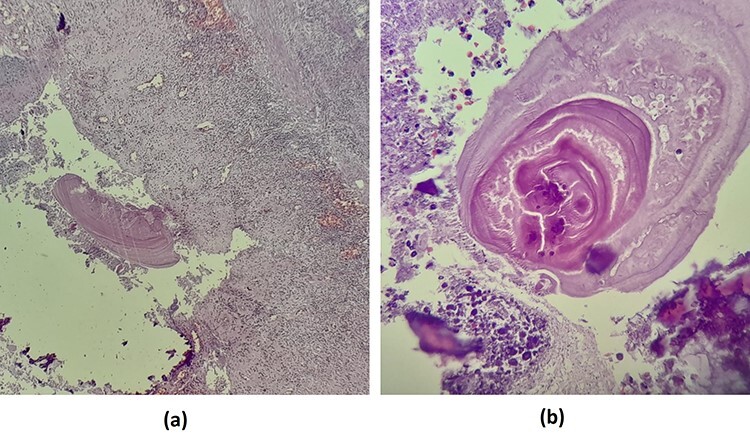
(a) Renal parenchyma with inflammatory reaction containing hydatid membranes (×10). (b) Eosinophil hydatid membranes and laminated acellular layers (×40).
The post-operative course was uneventful. Albendazole was prescribed post-operatively.
During a 6-month follow-up, the patient was asymptomatic with sterile cytobacteriological examination. Hydatid serology was negative. No hydatid recurrence was detected so far.
DISCUSSION
Renal hydatidosis is the first urological location of echinococcal disease, and ranks third, all visceral locations involved, even in endemic countries where raising of stockbreeding and cattle is widely present [1]. This disease is more common in women [2].
The first problem in the presence of a kidney cyst is to confirm its hydatid origin. In endemic countries, echinococcosis should be highly suspected for renal cystic lesions.
The diagnosis is often delayed, given the silent clinical evolution and the lack of specificity of the symptoms. The most frequent symptom is dull flank pain. Hematuria, lumber mass and sometimes fever may be observed. The only symptom that can reliably confirm the hydatid origin is hydaturia, which is found in 13% of cases [1, 2]. Ultrasound is of decisive importance, as it is the first-line diagnostic tool. It classifies hydatid cysts into five types, according to the imaging classification of Gharbi et al. [3]. Types II, III and V do not pose a diagnostic problem. Type I may be misdiagnosed as a simple serous renal cyst, polycystic kidney disease or renal tuberculosis. Calcifications are highly suggestive of hydatid origin in endemic areas; however, it lacks specificity since it may be found in renal carcinomas, renal tuberculosis or xanthogranulomatous pyelonephritis [4], especially in its focal form that does not involve a large renal sinus stone [5], as the present case.
Xanthogranulomatous pyelonephritis, as the name suggests, is a chronic granulomatous process believed to be the result of chronic infection inciting a chronic but incomplete immune reaction. The kidney is eventually replaced by a mass of reactive tissue surrounding the usually present inciting staghorn calculus with possible associate hydronephrosis [5]. The inflammatory process eventually extends into the perinephric tissues and adjacent organs, which is the basis of the radiological staging of this disease: Stage I when the affection is limited to the renal parenchyma only. Stage II involves renal parenchyma as well as an extension to perirenal fat. Stage III defined by the extension into perirenal and pararenal spaces or diffuse retroperitoneum [5].
Thus, hydatid renal cysts can be taken for xanthogranulomatous pyelonephritis in some litigious cases, due to very close and similar radiological findings and description. Sometimes, the differential is narrow and only histological examination can bring a certain diagnosis [2]. Furthermore, inadequate or over treatment may happen even in a controlled situation. No conservative therapy exists for certain forms of xanthogranulomatous pyelonephritis. Nephrectomy is usually performed. If hydatid origin is suspected, nephrectomy is rarely needed. Some specific precautions are required during surgical treatment of renal hydatidosis to prevent dissemination and seeding of the surgical field [2]. The area around the cyst should be carefully isolated by surgical fields soaked in a scolicidal agent (hypertonic saline or hydrogen peroxide). Anaphylactic shocks resulting from intra-operative spillage after a mistaken diagnosis of a retroperitoneal tumor are possible, sometimes deadly [2].
Chemotherapy with antihelmintics of benzimidazole family might be used adjunctively with surgery to prevent recurrence.
More attention should be paid to the differential diagnosis of renal cystic lesions, mainly in endemic areas. If the possibility of a hydatid cyst were considered in the present case, a different approach could have been considered, and the kidney could have been preserved.
CONCLUSION
Hydatid cysts at unusual sites, such as the kidney, especially in non-endemic areas, can lead to difficulties in the diagnosis and management of this diseade, possibly leading to complications or overtreatment. Although hydatid cysts of the kidney are relatively rare, this disease must be considered in people with renal cystic masses from endemic countries.
Contributor Information
Amine Hermi, Faculty of Medicine Tunis, Department of Urology, La Rabta Hospital, University Tunis Manar, Tunis, Tunisia.
Yassine Ouanes, Faculty of Medicine Tunis, Department of Urology, La Rabta Hospital, University Tunis Manar, Tunis, Tunisia.
Abdoulkader Tapsoba, Department of Urology, University of Joseph Ki-Zerbo, Ouagadougou, Burkina Faso.
Alia Kassar Zehani, Faculty of Medicine Tunis, Department of Pathology, La Rabta Hospital, University Tunis Manar, Tunis, Tunisia.
Kays Chaker, Faculty of Medicine Tunis, Department of Pathology, La Rabta Hospital, University Tunis Manar, Tunis, Tunisia.
Mokhtar Bibi, Faculty of Medicine Tunis, Department of Urology, La Rabta Hospital, University Tunis Manar, Tunis, Tunisia.
Kheireddine Mrad Daly, Faculty of Medicine Tunis, Department of Urology, La Rabta Hospital, University Tunis Manar, Tunis, Tunisia.
Ahmed Sellami, Faculty of Medicine Tunis, Department of Urology, La Rabta Hospital, University Tunis Manar, Tunis, Tunisia.
Sami Ben Rhouma, Faculty of Medicine Tunis, Department of Urology, La Rabta Hospital, University Tunis Manar, Tunis, Tunisia.
Yassine Nouira, Faculty of Medicine Tunis, Department of Urology, La Rabta Hospital, University Tunis Manar, Tunis, Tunisia.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no competing interests.
FUNDING
No funding was received.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The approval of the current study has been granted by the medical committee of research ethics of La Rabta Hospital. Written informed consent was obtained from the patient for publication of this study. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient for publication of this study. A copy of the written consent is available for review by the Editor on request.
References
- 1. Hermi A, Ichaoui H, Yaiche R, Hedhli H, Khiari R, Ghozzi S. Multiple unusual urological locations of hydatic cysts including kidney, retrovesical and spermatic cord. A new case report. Urol Case Rep 2019;25:100896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Horchani A, Nouira Y, Kbaier I, Attyaoui F, Zribi AS. Hydatid cyst of the kidney. A report of 147 controlled cases. Eur Urol 2000;38:461–7. [DOI] [PubMed] [Google Scholar]
- 3. Gharbi HA, Hassine W, Brauner MW, Dupuch K. Ultrasound examination of the hydatic liver. Radiology 1981;139:459–63. [DOI] [PubMed] [Google Scholar]
- 4. Von Sinner WN, Hellström M, Kagevi I, Norlen BJ. Hydatid disease of the urinary tract. J Urol mars 1993;149:577–80. [DOI] [PubMed] [Google Scholar]
- 5. Zalaquett E, Menias C, Garrido F, Vargas M, Olivares JF, Campos D, et al. Imaging of hydatid disease with a focus on extrahepatic involvement. Radiographics 2017;37:901–23. [DOI] [PubMed] [Google Scholar]


