Abstract
Background
Pregnancy is an immune-suppressed state which makes pregnant women generally more susceptible to COVID-19 infection and severe illness. Extensive precautions have been recommended to avoid exposure to the virus. Knowledge and attitude toward the disease play an integral role in readiness to accept public health measures. This study aimed to assess the knowledge, attitude and practice towards COVID-19 among pregnant women attending antenatal clinics in three Wollega zones, Ethiopia.
Methods
Institution-based cross-sectional study was employed among 415 pregnant women attending antenatal care at public hospitals in three Wollega zones, Ethiopia from July to August 2020. The data were collected using an interviewer-administered structured questionnaire. The level of knowledge was assessed using 12 multiple choice questions; the score of above or equal to mean was considered as adequate knowledge. Binary logistic regression was performed and the adjusted odds ratio with P-value ≤0.05 at 95% CI was taken as statistically significant.
Results
This study indicates that more than two-thirds (75.4%; 95% CI: 71.1–79.3%) and 43.6% of the pregnant women had adequate knowledge and good practice about the coronavirus pandemic, respectively. The pregnant women who attended secondary school and above and were urban residents were more likely to have good knowledge, AOR = 2.99 (1.7–5.0) and 1.6 (1.2–2.7), respectively. Maternal age ≤ 25 yearsand being an urban resident were the two predictors of good practice of preventive measures, AOR = 1.7 (1.2–2.6) and 2.3 (1.3–4.0), respectively.
Conclusions and Recommendations
The target population demonstrated acceptable knowledge and poor practice toward COVID-19. Health-care providers should give more attention to educating pregnant women at any point of contact; legal enforcement should be implemented to improve practice of preventive measures. Special consideration should be given to those who are from rural areas, and to less-educated pregnant women.
Keywords: pregnant women, Ethiopia, knowledge, attitude, corona virus infection
Introduction
COVID-19 was spreading globally at an accelerated rate and had spread to over 110 countries including Ethiopia when the World Health Organization (WHO) declared it to be a pandemic disease on March 11, 2020.1 The pandemic is posing a serious threat to global public health with more than 6 million cases on May 30, 2020.2 The pandemic had its first wave between December and January 2020 in Asia, and then went through to Europe and America, recording its second wave from February to date. The third wave of the pandemic may increase in the global spread.2
Even though everybody is at risk of becoming infected, pregnant women are more prone to become the victims of COVID-19 compared with the general population.3 It is transmitted by airborne droplets; thus is easily inhaled by pregnant women and is difficult to remove due to the change in anatomical structure of the respiratory system during pregnancy.4 Furthermore pregnancy is an immune suppressed state and pregnant women are generally more susceptible to viral respiratory infections and their complications. Pregnant women are at an increased risk for severe illness from COVID-19.5 The rate of morbidity, cesarean section delivery and preterm birth were also found to be increased.6 Vertical transmission is a matter of debate.2
The available data reporting the impact of COVID-19 on pregnancy outcome are not sufficient and are limited to small case series. In the absence of more robust evidence they were identified as a vulnerable group and were advised to take additional precautions as the COVID-19 pandemic unfolded.7 Pregnant women are considered to be high risk and extensive precautions have been recommended in order not to be exposed to the virus.5,8 COVID-19 public health responses such as social distancing, frequent hand washing and use of protective equipment are critical in preventing and containing the spread of coronavirus.9 Failure to apply these important public health measures might result in poor control and increase likelihood of infection.15
Knowledge and attitude towards the disease plays an integral role in determining a society’s readiness to accept public health measures. Studies have shown that socio-demographic factors including age, ethnicity, front line job, and obstetrics care and history influence the knowledge, attitude and precaution practice toward COVID-19 among pregnant women.11 On the other hand, poor knowledge and practices of preventive measures against COVID-19 among pregnant women have been reported particularly in developing countries.3
A study conducted in northern Ethiopia showed that less than 50% of the studied pregnant women were knowledgeable and had good practice against coronavirus infection.11 The available literature on the level of knowledge, attitude and practice toward COVID-19 among pregnant women in Ethiopia is limited: as far as we are aware there was no study conducted in the study area. The finding of this study will be used as baseline data by policymakers to design appropriate strategies used to tackle the pandemic effect in this vulnerable population. It will used by health professionals when they provide services to pregnant women. It will also be used by scholars who will conduct research on similar topics in the future.
Materials and Methods
Study Area and Period
The study was conducted at randomly selected public hospitals in three Wollega zones (East Wollega, West Wollega and Horo Guduru Wollega zone), western Ethiopia. There are around 12 public hospitals in these three Wollega zones of which one is a referral hospital, one is a comprehensive specialized hospital and the rests are zonal and district hospitals. Accordingly, Nekemte referral hospital, Wollega university specialized hospital, Shambu general hospital, Nedjo general hospital and Arjo hospital were randomly selected and included in the study. The data were collected for one full month from July 1 to August 30, 2020.
Study Design
The institutional-based cross-sectional study was employed among the selected public health institutions.
Population
Source population
All pregnant women who were attending antenatal care (ANC) at public hospitals in East, West and Horo Guduru Wollega zones were the source population for this study.
Study Population
Those pregnant women who were attending ANC at selected public hospital during the data collection period were the study population.
Eligibility Criteria
Inclusion Criteria
All pregnant women who were on antenatal care were included in the study irrespective of trimester, absence or presence of comorbidity, and number of ANC visits.
Exclusion Criteria
Mothers who were unable to communicate were excluded from the study.
Sample Size Determination
Sample size was determined by single population proportion with the following assumptions: Since this study was the first of its type in Ethiopia P = 50% was taken, with 5% margin of error, and 95% confidence interval. Accordingly the calculated sample size was 384 and after adding a 10% allowance for a non-response rate, the final sample size was 422 pregnant women.
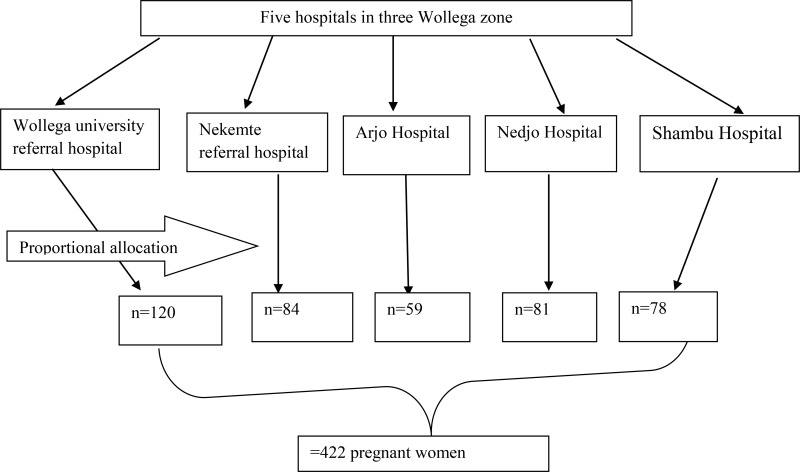
Sampling Procedure
The three zones of Wollega district were purposely selected then the lottery method was used to select five public hospitals from the total of hospitals found in the three zones. Systematic random sampling technique was used to select the representative pregnant women from those who attend ANC. The sample size was proportionally distributed to each hospital depending on the number of pregnant women attending ANC at each hospital (see Figure 1).
Figure 1.
Diagrammatic presentation of the sampling procedure for the study on knowledge, attitude and practice toward COVID-19 among pregnant women in three Wollega zones, Ethiopia.
Variable
Dependent variables
Knowledge towards COVID 19
Practice towards COVID 19 prevention measure.
Independent Variables
Socio-demographic (age, residency, marital status, occupational status, family monthly income, ethnicity, religion), obstetric and reproductive factors (parity, gravidity, history of ANC).
Data Collection Tools and Procedure
The questionnaire was adopted from different articles published in English and contextualized to local situations. The adopted questionnaire was translated to locally spoken Oromo language and pre-tested. The validity of the tool was evaluated by comparing the consistency between the original and re-translated version of the tool. After the pre-test, the order of questions was rearranged, modified by replacing and adding more choice. The questionnaires contain five parts: socio-demographic data, obstetric and reproductive data, knowledge, attitude and practice questions. The questionnaires have a 12-item scale for knowledge assessment questions and a 10-item scale for practice questions. The scoring system of women’s knowledge and practice were either 1 (for correct answer) or 0 (for incorrect answer). The maximum score was 12 for knowledge and 10 for the practice component of the question whereas the minimum score was 0 for both. Data were collected by four trained BSc midwives using an interviewer-administered structured questionnaire.
Data Quality Assurance
The questionnaires were prepared in English and translated to Afan Oromo and re-translated to English. The tools were pre-tested before the actual data collection among 30 pregnant women at Gida hospital, who were not included in the final study. Training was given for data collectors and supervisors for one day. The data collection process was supervised by principal investigators and trained supervisors. The filled questionnaires were randomly checked for completeness and consistency.
Data Processing and Analysis
The collected data were manually entered into Epi-data and exported to SPSS version 22 for statistical software analysis and were cleaned and transformed before analysis. Frequency and percentage were used to describe socio-demographic, reproductive and obstetric characteristics, knowledge, practice and attitude of the participants. Binary logistic regression analysis was conducted to determine the association of pregnant women’s knowledge and practice with some explanatory variables. In multivariable binary logistic regression the AOR with P-value < 0.05 at 95% CI was taken as statistically significant predictors of the outcome variable.
Operational Definition
Awareness: whether women had heard or not about COVID 19.
Good knowledge: Participants who scored ≥ mean (which was 11 for this study).
Inadequate knowledge: Women who scored < mean score for knowledge question.
Good practice: Women who scored 100% (score of 12) on the practice of COVID-19 disease preventive measures questionnaire.
Poor practice: Women who scored < 100% (score below 12) on the practice of COVID-19 disease preventive measures questionnaire.
Ethical Considerations
Written ethical clearance that allows using verbal consent for this study was obtained from the WURERC (Wollega University Research Ethics Review Committee). All the study participants were fully informed about the purpose of the study. Verbal consent was obtained from all respondents who were greater or equal to 18 years old and oral consent was obtained from the legal guardian for those respondents who were less than 18 years old. The interview was undertaken after the respondents completed their ANC examination in a separate area from the other participants. All the information was kept confidential and used only for research purposes. Health education about coronavirus infection was given briefly for every participant at the end of the interview.
Results
Socio-Demographic Characteristics
Data from a total of 415 pregnant women were used in this analysis (98.1% response rate). The minimum and maximum age of the study participant was 17 and 50 respectively, with mean age of 25.46 ± 4.67 years. The majority (71.1%) of the study participants were in the age group 21–30 years followed by those within the age group 17–20 years (15.2%). The study participants were predominantly from an urban area (80.9%) and predominantly (94.7%) married. More than 35.3% of the study participants had attended college or higher educational level (Ssee Table 1).
Table 1.
Socio-Demographic Distribution of the Pregnant Women Attending ANC at Public Health Institutions (n = 415) in East, West and Horo Guduru Wollega Zones, Western Ethiopia
| Character (n = 358) | Category | Frequency | Percentage (%) |
|---|---|---|---|
| Age group | 17–20 | 63 | 15.2 |
| 21–30 | 295 | 71.1 | |
| >30 | 57 | 13.7 | |
| Residence | Urban | 336 | 81.0 |
| Rural | 79 | 19.0 | |
| Marital status | Married | 393 | 94.7 |
| Other | 22 | 5.3 | |
| Educational status | Cannot read and write | 36 | 8.7 |
| Primary school | 89 | 21.4 | |
| Secondary school | 144 | 34.7 | |
| College and above | 146 | 35.2 | |
| Occupation | Government Employee | 83 | 20 |
| NGO Employee | 5 | 1.2 | |
| Private job | 231 | 55.8 | |
| Others | 95 | 22.9 | |
| Religion | Protestant | 291 | 70.1 |
| Orthodox | 84 | 20.2 | |
| Muslim | 36 | 8.7 | |
| Others | 4 | 1 | |
| Number of family member | ≤2 | 175 | 42.2 |
| 3–4 | 174 | 41.9 | |
| ≥5 | 66 | 15.9 |
Obstetric Characteristics of the Pregnant Women
In this study the majority (63.1%) of the participants were multigravida and the remaining 36.9% were primigravida. More than half (61.9%) of the pregnant women had fewer than three alive children while only 6% had four or more alive children. In more than three-quarters (83.6%) of the women the current pregnancy was wanted and planned. Sixty-seven (16.1%) of the study participants had some complications associated with the current pregnancy and more than two-thirds (83.9%) had no previous history of chronic disease and obstetrics complication (see Table 2).
Table 2.
Obstetrics and Reproductive Characteristics of Pregnant Women Attending Antenatal Care, Western Ethiopia 2020 (N=415)
| Variable | Frequency | Percentage | |
|---|---|---|---|
| Gravidity | Primigravida | 153 | 36.9 |
| Multigravida | 262 | 63.1 | |
| Number of alive children | Nulliparous | 133 | 32 |
| 1–3 | 257 | 61.9 | |
| 4 and above | 25 | 6 | |
| Current pregnancy condition | Wanted and planned | 68 | 16.4 |
| Unwanted | 347 | 83.6 | |
| Number of current ANC visit | 1–2 visit | 352 | 84.8 |
| 3 and above | 63 | 15.2 | |
| Gestational at booking | Before 3 month | 81 | 19.5 |
| 3–6 month | 296 | 71.3 | |
| After 6 month | 38 | 9.2 | |
| Obstetrics complication in current pregnancy | YES | 67 | 16.1 |
| NO | 348 | 83.9 | |
Knowledge of the Pregnant Women About COVID-19
All of the 415 study participants (100%) reported that they had ever heard about the coronavirus pandemic. The majority (96.4%) of the pregnant women responded that they knew at least one common symptom of COVID-19 infection. Of the total respondents 87.2% knew that currently COVID-19 had no effective treatment, 83.1% knew that everybody can be infected by COVID-19, and 95.9% knew that wearing a mask can reduce the risk of infection. The vast majority (96.4%) of the pregnant women knew at least one common symptom of COVID-19 (see Table 3).
Table 3.
Distribution of Studied Pregnant Women According to Their Knowledge Towards Coronavirus Infection (n = 415)
| s/n | Variable | Response | |
|---|---|---|---|
| YES | NO | ||
| 1 | Heard about COVID-19 | 415(100%) | 0(0%0 |
| 2 | Do you know the symptom of COVID-19 infection | 400(96.4%) | 15(3.6%) |
| 3 | COVID-19 has effective treatment presently | 53 (12.8%) | 362(87.2%) |
| 4 | Everybody can be infected by COVID-19 | 345 (83.1%) | 70 (16.9%) |
| 5 | COVID-19 is severe in Co-morbid and elderly people | 373 (89.9%) | 42(10.1 |
| 6 | Re-infection can occur with COVID-19 | 349 (84.1%) | 66(15.9%) |
| 7 | COVID-19 infection can be transmitted by air droplets | 401(96.6%) | 14 (3.4%) |
| 8 | Avoiding touching eyes and nose prevents COVID-19 | 375(90.4%) | 40(9.6%) |
| 9 | Ordinary people should use mask to prevent COVID-19 | 398(95.9%) | 17(4.1%) |
| 10 | Avoiding crowding can decrease risk of COVID-19 | 402(96.9%) | 13(3.1%) |
| 12 | Isolation is important after contact with infected person | 405(97.6%) | 10(2.4%) |
| 13 | Reporting the suspected symptom is recommended | 379(91.3%) | 36(8.7%) |
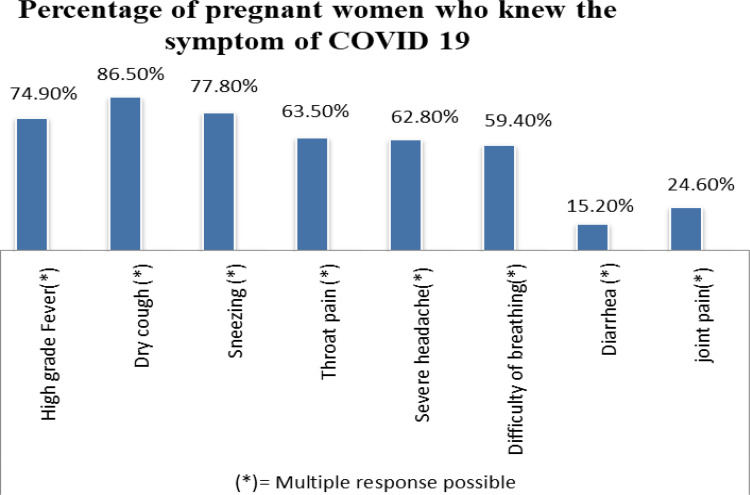
From those who knew the common symptoms of COVID-19: 86.5% knew the dry cough and more than 70% knew sneezing and dry cough as common symptoms of coronavirus disease. Just more than 60% of participants knew that throat pain was a symptom of coronavirus infection (see Figure 2).
Figure 2.
Diagrammatic presentation of percentage of pregnant women who knew the symptoms of COVID-19 in three Wollega zones, west Ethiopia.
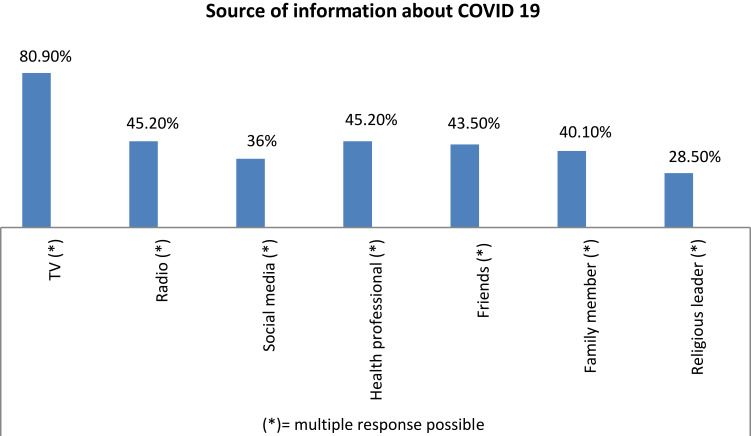
Primary Source of Information About COVID-19
This study revealed that more than two-thirds (75.4%; 95% CI: 71.1–79.3%) of the total respondents had good knowledge about COVID-19. Among the participants the majority (80.9%) stated that their primary source of information about COVID-19 was television followed by health professionals and radio (see Figure 3).
Figure 3.
Diagrammatic presentation of primary source of information about COVID-19 among pregnant women in three Wollega zones, west Ethiopia.
Attitude and Perception Toward COVID-19
Among the studied pregnant women the majority (68.2%) thought that COVID-19 is a curse from God/Allah. More than half (61.2%) believe that the pandemic will be successfully contained. In this study 61.7% thought they are more high risk of developing complications than non-pregnant women if infected with COVID-19; however only 15% of them fear that they will lose their life or a family member due to COVID 19 (see Table 4).
Table 4.
Distribution of Studied Pregnant Women According to Their Attitude and Perception Towards Coronavirus Infection (n = 415)
| s/n | Attitude and Perception Statement | Response | |
|---|---|---|---|
| Agree | Disagree | ||
| 1 | COVID-19 is curse from God | 283 (68.2%) | 132 (31.8%) |
| 2 | COVID-19 will eventually be successfully controlled | 256 (61.2%) | 159 (38.8%) |
| 3 | Do you think a pregnant woman is at higher risk of complication from COVID-19 compared with non-pregnant | 256 (61.7%) | 159 (38.3%) |
| 4 | Do you fear that you may lose your life/family member by COVID-19 | 64 (15.4%) | 351(84.6%) |
Practice of COVID-19 Public Health Measure
This study revealed that less than 43.6% of the study participants had good practice of preventive measures of COVID-19 infection and a large number (56.4%) of the women had poor practice. The women’s responses regarding practice of preventive measures against COVID-19 infection was covering mouth with flexed elbow while coughing or sneezing (91.8%), frequent hand washing (90.6%), wearing face mask (88.2%), avoid hand shaking with others (87.7%) and keeping physical distancing (73.7%) (see Table 5).
Table 5.
Distribution of the Studied Pregnant Women According to Their Practice of Preventive Measures of COVID-19 Infection (n = 415)
| S/N | Practice Question | Response | |
|---|---|---|---|
| YES | NO | ||
| 1 | Wash hand with soap/use sanitizer | 376(90.6%) | 39(9.4%) |
| 2 | Covering mouth with elbow while sneezing | 381(91.8%) | 34(8.2%) |
| 3 | Keeping physical distancing | 306(73.7%) | 109(26.3%) |
| 4 | Wearing face mask when go out | 366(88.2%) | 49(11.8%) |
| 5 | Changing travel | 285(68.7%) | 130(31.3%) |
| 6 | Staying at home /working from home | 226(54.5%) | 189(45.5%) |
| 7 | Reporting COVID-19 symptom to health facility | 325(78.3%) | 90(21.7%) |
| 8 | Stop hand shaking with people | 364(87.7%) | 51(12.3%) |
| 9 | Health care seeking when get ill | 375(90.4%) | 40(9.6%) |
| 10 | Avoiding going to social gathering | 344(82.9%) | 71(17.1%) |
Factors Associated with Knowledge of COVID-19
In the single variable logistic regression educational status of college and above and being an urban resident was associated with having good knowledge about COVID-19 infection. In the multivariate logistic regression analysis those pregnant women who attend secondary school were 1.6 times more likely to have adequate knowledge about the pandemic when compared with their counterparts. Those who were urban residents were nearly 3 times more likely to have good knowledge about coronavirus infection when compared with those who were from rural areas (see Table 6).
Table 6.
Bivariate and Multivariate Logistic Regression of Factors Associated with Knowledge of Coronavirus Infection Among the Studied Pregnant Women
| Covariant | Knowledge Status | COR | AOR | P value | ||
|---|---|---|---|---|---|---|
| Poor | Good | |||||
| Educational status | Below secondary school | 44(35.2%) | 81(64.8%) | 1 | 1 | |
| Secondary school and above | 58 (20%) | 232(80%) | 2.2(1.4–3.5) | 1.6(1–2.7) | 0.05* | |
| Residency | Rural | 36(45.6%) | 43(54.4%) | 1 | 1 | |
| Urban | 66(19.6%) | 270(80.4%) | 3.4(2.0–5.8) | 2.99(1.7–5.0) | 0.000*** | |
Notes: Key: 1 = Reference category, *PV≤ 0.05, ***P<0.0001.
Abbreviations: COR, Crude Odds Ratio; AOR, Adjusted Odds Ratio; CI, confidence interval.
Factors Associated with Practice Against COVID-19
In the single variable logistic regression maternal age of less than or equal to 25 years and being an urban resident was associated with good practice toward preventive measures of COVID-19 infection. Then when the above variables were subjected to multivariate logistic regression analysis those pregnant women who were less than or equal to 25 years of age were 1.7 times more likely to have good practice of preventive measures toward the pandemic when compared with those who were greater than 25 years old. Those pregnant women who were urban residents were about 2.3 times more likely to practice a good level of preventive measures toward coronavirus infection (see Table 7).
Table 7.
Bivariate and Multivariate Logistic Regression of Factors Associated with Practice of Preventive Measures Against Coronavirus Infection Among the Studied Pregnant Women
| Covariant | Practice Status | COR | AOR | P value | ||
|---|---|---|---|---|---|---|
| Poor | Good | |||||
| Age | Below 25 | 122(50.2%) | 121(49.8%) | 1.8(1.3–2.8) | 1.7(1.2–2.6) | 0.008* |
| ≥25 | 112(65.1%) | 60(34.9%) | 1 | 1 | ||
| Residency | Rural | 58(73.4%) | 21(26.6%) | 1 | 1 | |
| Urban | 176(52.4%) | 160(47.6%) | 2.5(1.5–4.3) | 2.3(1.3–4.0) | 0.002* | |
Notes: Key: 1 = Reference category, *P<0.05.
Abbreviations: COR, Crude Odds Ratio; AOR, Adjusted Odds Ratio; CI, confidence interval.
Discussion
This study was interested in ascertaining the knowledge, attitude and practice of pregnant women in Wollega zone toward COVID-19. In this study more than two-thirds of the study participants had adequate knowledge about coronavirus infection. This shows that coronavirus awareness creation campaigns across the country have made a positive impact on the knowledge of the disease. However the practice of COVID-19 public health measures among the pregnant women was low in the area. This implies that having adequate knowledge will not always lead to the adoption of a new practice. The government will need to follow a regulatory strategy on COVID-19 preventive measures despite the health education campaign to improve the knowledge among target population.
In this study, out of all the studied pregnant women two-thirds (75.4%; 95% CI: 71.1–79.3%) of them had good knowledge about the coronavirus pandemic. The current study finding was consistent with a report from studies conducted in India and China in which 75.3% and 76.4% of the study participants had satisfactory level of knowledge about coronavirus infection, respectively.11,12 The possible reason may be that the disease is a global public health problem and is heard about all over the world in a similar manner.
However, this finding was much higher than the finding from community-based cross sectional studies conducted in other parts of Ethiopia at Debra Tabor town and Gurage zone in which only 46.8% and 54.8% of the pregnant women were knowledgeable about COVID-19, respectively.11,13 The current level of knowledge of pregnant women about COVID-19 was also higher than found in research conducted in Egypt which showed that 57.6% of women had a satisfactory level of knowledge.14 The possible reason may be that all the former studies were conducted during the earlier stage of the pandemic compared with the current study and coronavirus risk communication across the world may have made a positive impact on the knowledge of the target population. The nature of the study could be the possible reason for the discrepancy; the level of health-related knowledge is expected to be high among the populations which are on follow up at health facility.
In the current study more than half of the study participants had poor practice about COVID-19 infection. This finding was similar with the findings reported from studies conducted in North West Ethiopia and Nigeria which reported that only 47.6% and 30.3% of pregnant women had good practice of coronavirus preventive measures, respectively.10,11 This can be justified since those public health measures are new and it may take time to adapt to new norms.
In this study, the odds of having good knowledge of COVID 19 was higher among women who had secondary and above education compared with those who attended below primary school. This finding is supported with the findings from the studies conducted in Debra Tabor,11 China12 and Iran16 where a higher proportion of pregnant women who had higher educational status were found to have good knowledge. The reason for this might be that educated women are more likely to be exposed to different mass media and social media including access to the internet to get information about COVID-19. They are also more likely to comprehend the information they obtained.
In this study, the odds of having good knowledge of COVID-19 was higher among women who were from urban areas compared with those pregnant women who were from rural areas. This finding is supported with the finding from the study of pregnant women in low income countries which found that being from a rural area was associated with poor knowledge among pregnant women.16 This may be due to those pregnant women who were living in urban areas getting more information from different social media.
In this study, those pregnant women who were young (<25 years) were more likely to have good practice of COVID-19 preventive measures. This finding was consistent with that reported from the study conducted in Debra Tabor city in Ethiopia which showed that younger women were more likely to have good knowledge and practice about COVID-19.11 This may be due to a younger population being more likely to adopt a new lifestyle.
Strength and Limitation of the Study
This study was an institutional-based study; thus it may not explain the level of knowledge and practice at the community level. On the other hand only individual level factors that may be associated with knowledge and practice toward COVID 19 were identified.
Despite these limitations, our study had some prominent strengths. The present study was at the time when coronavirus infection disease was at its peak in Ethiopia; so it can be used as baseline data for those who are working on the problem. Moreover, factors associated with knowledge and practice of COVID-19 among pregnant women were identified so it gives a direction to follow during health intervention.
Conclusion and Recommendation
In this study most of the study participants had adequate knowledge however the practice of preventive measures were low in the area. Maternal educational status and place of residency were important predictors of adequate knowledge, whereas maternal age and place of residence were important factors associated with good practice of preventive measures toward COVID-19 infection among pregnant women. Core recommendations to assist pregnant women of different aspects in the current pandemic can be made.
Health-care providers should give more attention on educating pregnant women at any point of contact.
Health education campaigns should be implemented to improve knowledge as well as practice of preventive measures for COVID-19.
Legal enforcement should be implemented to improve practice of preventive measures toward COVID-19.
During health education special consideration should be given to those who are from rural areas, and to less-educated pregnant women.
Acknowledgment
First and foremost my special thanks go to Wollega University for allowing me to conduct this study as well as for fully funding it. Next, I extend my deep gratitude to the data collectors, supervisor and study participants. I would also like to thank the administrative and all other staff of the selected hospitals for their cooperation.
Acronyms and Abbreviations
ANC, Antenatal care; AOR, Adjusted Odds Ratio; CI, Confidence Interval; FMOH, Federal Ministry of Health of Ethiopia; HEW, Health Extension Workers; GA, Gestational age; MMR, Maternal Mortality Ratio; PIH, Pregnancy Induced Hypertension; CS, Cesarian section; UNICEF, United Nation International Children’s Emergency Fund; WHO, World Health Organization.
Data Sharing Statement
The data sets used during the current study are available from the corresponding author on reasonable request.
Ethics Approval
This study was conducted in accordance with WMA Declaration of Helsinki. Ethical approval was obtained from the Internal Review Board of Wollega University Institute of Health Science. All the information was kept confidential and used only for research purposes.
Consent to Participate
Verbal informed consent was obtained from all respondents who were greater or equal to 18 years old and oral informed consent was obtained from the legal guardian or the respondents who were less than 18 years old before starting interview. The consent process was approved by the Internal Review Board of Wollega University Institute of Health Science.
Declarations
I declare that this study is my original work and the used references are acknowledged through citation.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Sohrabi C, Alsafi Z, O’Neill N, et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anjorin AA. The coronavirus disease 2019 (COVID-19) pandemic: a review and an update on cases in Africa. Asian Pac J Trop Med. 2020;13. [Google Scholar]
- 3.Cheng S, Khan S, Alsafi Z. Maternal death in pregnancy due to COVID-19. Ultrasound Obstet Gynecol. 56(1):122. doi: 10.1002/uog.22111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhao X, Jiang Y, Zhao Y, et al. Analysis of the susceptibility to COVID-19 in pregnancy and recommendations on potential drug screening. Eur J Clin Microbiol Infect Dis. 2020;39(7):1209–1220. doi: 10.1007/s10096-020-03897-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tanjuakio J. COVID-19, pregnancy, and breastfeeding: what is the current medical consensus on how COVID-19 may affect pregnant individuals who contract the virus? Likewise, what is the current medical consensus on COVID-19 and breastfeeding? Available from: https://www.womenslawproject.org/ Accessed July 9, 2021 [Google Scholar]
- 6.Tug N, Yassa M, Köle E, et al. Pregnancy worsens the morbidity of COVID-19 and this effect becomes more prominent as pregnancy advances. Turkish J Obstet Gynecol. 2020;17(3):149. doi: 10.4274/tjod.galenos.2020.38924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wastnedge EA, Reynolds RM, van Boeckel SR, et al. Pregnancy and COVID-19. Physiol Rev. 2021;101(1):303–318. doi: 10.1152/physrev.00024.2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liang H, Acharya G. Novel corona virus disease (COVID‐19) in pregnancy: what clinical recommendations to follow? Acta Obstet Gynecol Scand. 2020;99(4):439–442. doi: 10.1111/aogs.13836 [DOI] [PubMed] [Google Scholar]
- 9.Carter C. Glutamine, glutamine synthetase and Huntington’s disease. Lancet. 1981;317(8235):1427–1428. doi: 10.1016/S0140-6736(81)92611-8 [DOI] [PubMed] [Google Scholar]
- 10.Ayele AD, Mihretie GN, Belay HG, Teffera AG, Kassa BG, Amsalu BT. Knowledge and practice to prevent COVID-19 and its associated factors among pregnant women in Debre Tabor Town Northwest Ethiopia, a community-based cross-sectional study. BMC pregnancy and childbirth. 2021 Dec;21(1):1–2.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kamal D, Thakur VD, Swain SK, Vikneshram CR. Knowledge, attitude, and practice toward COVID-19 among pregnant women in a tertiary care hospital during the COVID-19 outbreak. Journal of Marine Medical Society. 2020;22(3):66. [Google Scholar]
- 12.Lee T-Y. The outbreak of coronavirus disease in China: risk perceptions, knowledge, and information sources among prenatal and postnatal women. Women Birth. 2020;1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fikadu Y, Yeshaneh A, Melis T, et al. COVID-19 preventive measure practices and knowledge of pregnant women in guraghe zone hospitals. Int J Women’s Health. 13: 39. doi: 10.2147/IJWH.S291507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Metwally HMS, Desoky MMAEM. Knowledge, practice and attitudes of preventive measures against coronavirus infection among pregnant women in Egypt. Saudi Journal of Nursing and Health Care. doi: 10.36348/sjnhc.2020.v03i06.001 [DOI] [Google Scholar]
- 15.Nwafor JI. Knowledge and practice of preventive measures against COVID-19 infection among pregnant women in a low-resource African setting. medRxiv. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maharlouei N, Asadi N, Bazrafshan K. et al. Knowledge and attitude regarding COVID-19 among pregnant women in southwestern iran in the early period of its outbreak: a Cross-Sectional Study. Am J Trop Med Hyg;2020. tpmd200608. doi: 10.4269/ajtmh.20-0608 [DOI] [PMC free article] [PubMed] [Google Scholar]