Abstract
Patients with polycythemia vera are at high risk for vaso-occlusive events including cerebral ischemia and hemorrhage. Cerebral ischemic events are due to increased blood viscosity and platelet activation within the central nervous system arterial vessels. We present a case of a 65-year-old woman who presented to the emergency department with seizures followed by left-sided weakness. Hematologic investigations revealed a hyperviscous state, and magnetic resonance imaging (MRI) was consistent with bilateral hemorrhagic infarction. Genetic studies were positive for polycythemia vera mutation. Symptoms improved with phlebotomy and antiplatelet agents. Through this case, we aim to highlight polycythemia vera as a cause of hemorrhagic stroke and the importance of blood counts in the routine evaluation of the same.
Keywords: polycythemia vera, hemorrhagic stroke, hypercoagulable state
Introduction
Polycythemia vera (PV) is a myeloproliferative disease characterized by clonal proliferation of hematopoietic stem cells, leading to abnormal increases in circulating red blood cells, white blood cells, and platelets, resulting in an increase in blood viscosity and reduction in blood flow velocity. 1 These disorders of hemorheology are contributing factors for thrombosis, resulting in cerebral infarction. In some situations, the condition is associated with cerebral hemorrhage due to dysfunction in platelet aggregation and the prolongation of activated partial prothrombin time. 2 3 Stroke may be the first presenting symptom of PV in 15% or more of those affected by the disease. 4 Here, we present a case of a 65-year-old patient who presented with bilateral hemorrhagic infarcts.
Case Report
A 65-year-old woman with a history of diabetes and hypertension presented to the emergency department with an episode of generalized seizures, followed by weakness of left upper and lower extremities and altered sensorium. On examination, the patient was noted to be in the postictal state with left hemiparesis. Her blood pressure was 180/100 mm Hg. Imaging studies showed areas of infarction in bilateral parieto-occipital, right thalamic, right basal ganglia, and frontal white matter ( Figs 1 2 3 4 – 5 ). Hemorrhagic transformation was seen in bilateral parieto-occipital regions. Magnetic resonance angiography (MRA) of the brain showed hypoplastic right vertebral artery. On laboratory evaluation, she was noted to have a hemoglobin level of 16.1 g/dL associated with elevated total white blood count of 49,390/mm 3 and platelet count of 8.35 lakhs/mm 3 . We considered the possibility of a myeloproliferative neoplasm. Genetic work-up revealed a JAK2 V617F mutation, which is characteristically seen in patients with PV. She was started on antiplatelet agents. We also performed therapeutic phlebotomy to reduce the hemoglobin to a goal of less than 14.5 g/dL. Subsequently, both her sensorium and motor power improved with physiotherapy. To keep her platelet count to a goal of less than 5 lakhs/mm 3 , we also started her on hydroxyurea.
Fig. 1.
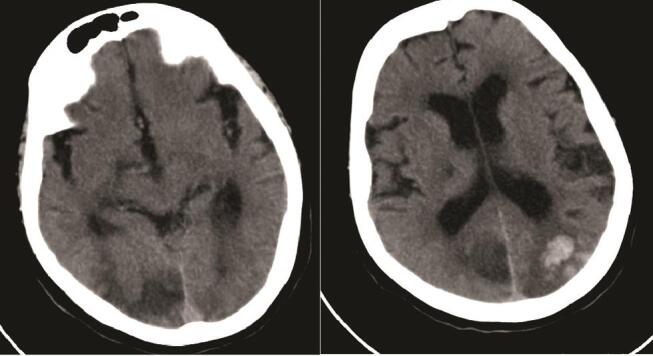
CT brain showing bilateral hemorrhagic infarction in the parieto-occipital lobes.
Fig. 2.
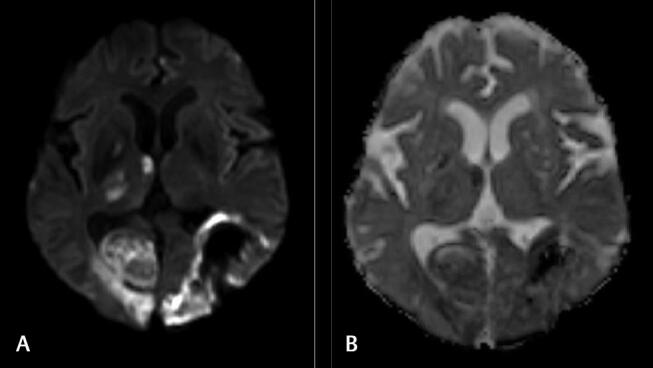
( A ) Diffusion-weighted imaging (DWI) and ( B ) apparent diffusion coefficient (ADC) images showing areas of restricted diffusion on DWI involving right thalamus, bilateral parieto-occipital lobes, and corresponding areas on ADC.
Fig. 3.
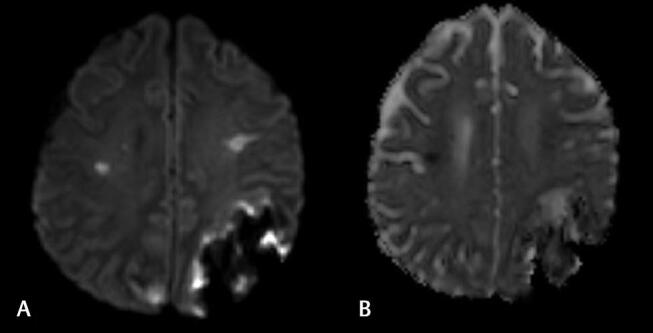
( A ) Diffusion-weighted imaging and ( B ) apparent diffusion coefficient images showing bilateral frontal and occipital infarcts.
Fig. 4.
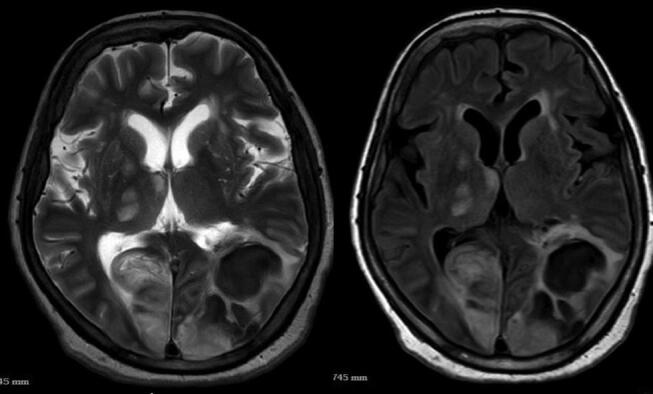
T2/FLAIR (fluid-attenuated inversion recovery) images showing bilateral hemorrhagic infarcts involving parieto-occipital lobes.
Fig. 5.
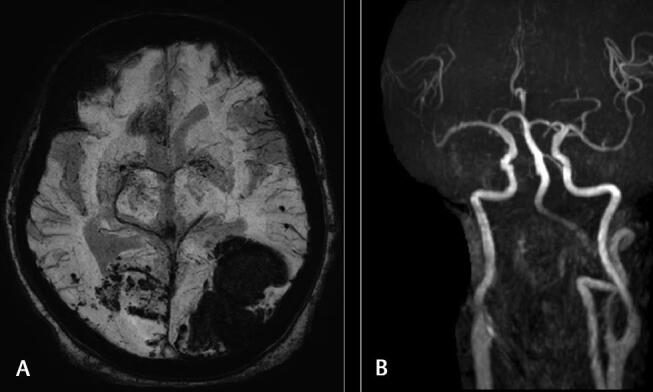
( A ) Susceptibility-weighted imaging (SWI) images showing hemorrhagic areas in both parieto-occipital lobes. ( B ) Magnetic resonance angiography (MRA) showing hypoplastic right vertebral artery on MRA.
Discussion
PV is a rare cause of both cerebral thrombosis and hemorrhage. The etiology of PV is attributed to a gain of function mutation of the JAK2 domain (Janus Activated Kinase (JAK)2 V617F mutation) found in more than 95% of patients. 5 Chemotherapy with hydroxyurea and anagrelide, a medication that inhibits the maturation of platelets, may also be used in conjunction with phlebotomy and antiplatelet agents. 6 PV should be considered in the differential diagnosis of stroke in multiple territories. It is imperative to pay close attention to routine blood investigation, which in this case turned out to be anything but routine.
Acknowledgments
The authors wish to thank their friends and family for their support.
Funding Statement
Funding None.
Footnotes
Conflict of interest None declared.
References
- 1.Spivak J L. Polycythemia vera. Curr Treat Options Oncol. 2018;19(02):12. doi: 10.1007/s11864-018-0529-x. [DOI] [PubMed] [Google Scholar]
- 2.Lim Y, Lee J O, Kim S H et al. Prediction of thrombotic and hemorrhagic events during polycythemia vera or essential thrombocythemia based on leukocyte burden. Thromb Res. 2015;135(05):846–851. doi: 10.1016/j.thromres.2015.02.023. [DOI] [PubMed] [Google Scholar]
- 3.Marchioli R, Finazzi G, Specchia G et al. CYTO-PV Collaborative Group. Cardiovascular events and intensity of treatment in polycythemia vera. N Engl J Med. 2013;368(01):22–33. doi: 10.1056/NEJMoa1208500. [DOI] [PubMed] [Google Scholar]
- 4.Gruppo Italiano Studio Policitemia . Polycythemia vera: the natural history of 1213 patients followed for 20 years. Ann Intern Med. 1995;123(09):656–664. doi: 10.7326/0003-4819-123-9-199511010-00003. [DOI] [PubMed] [Google Scholar]
- 5.Levine R L, Wadleigh M, Cools J et al. Activating mutation in the tyrosine kinase JAK2 in polycythemia vera, essential thrombocythemia, and myeloid metaplasia with myelofibrosis. Cancer Cell. 2005;7(04):387–397. doi: 10.1016/j.ccr.2005.03.023. [DOI] [PubMed] [Google Scholar]
- 6.Landolfi R, Marchioli R, Kutti J et al. European Collaboration on Low-Dose Aspirin in Polycythemia Vera Investigators. Efficacy and safety of low-dose aspirin in polycythemia vera. N Engl J Med. 2004;350(02):114–124. doi: 10.1056/NEJMoa035572. [DOI] [PubMed] [Google Scholar]


