Abstract
Introduction
The MPFL reconstruction is performed either via a single-bundle (SB) or double-bundle (DB) procedure. The purpose of this study is to perform a systematic review comparing SB versus DB graft for recurrent patellofemoral instability, to summarize current evidence, and to clarify the role of both techniques. We focused on clinical scores, physical examination, complications, revision surgeries, and failures.
Material and methods
In May of 2019 the main online databases were accessed. All the clinical studies treating isolated MPFL reconstruction for patellofemoral instability through a single and/or double-bundle graft were enrolled in the present systematic review. Only articles reporting primary isolated MPFL reconstruction, reporting a minimum of 12-months follow-up were considered for inclusion.
Results
The scores of interest were in favour of the DB cohort: Kujala (+ 3.2, P = 0.03), Lysholm (+ 5.1, P = 0.001), Tegner (+ 0.3, P = 0.2), IKDC (+ 5.4, P = 0.01), VAS (+ 0.8, P = 0.3), ROM (+ 9.96, P = 0.04). In the DB graft, a reduction of overall complications (OR 0.59; P = 0.1), further surgeries (OR 0.64; P = 0.12) and re-dislocations (OR 0.61; P = 0.16) was observed. The SB group reported a reduction in the post-operative apprehension test (OR 2.42; P = 0.24).
Conclusion
Current study support the use of double-bundle tendon graft for isolated MPFL reconstruction in selected patients with recurrent patellofemoral instability.
Keywords: Patellofemoral instability, Dislocation, MPFL, Reconstruction, Graft, Single bundle, Double bundle
Introduction
Patellofemoral instability is a multifactorial disorder that affects young active patients [1]. Regardless of the cause of dislocation, up to 94% of knees reported damage to the medio patellofemoral ligament (MPFL) [2]. The MPFL is the most important restraint to lateral displacement of the patella during the first 30° of knee flexion [3]. In up to 44% of patients, conservative treatment resulted in recurrent patellar dislocation [4]. Surgical reconstruction of the MPFL reported excellent outcomes in terms of patient satisfaction, quality of life, and knee scores, in addition to a very low rate of re-dislocations and complications [5]. It has been supposed that isolated MPFL reconstruction may even achieve satisfactory results in patients with mild to moderate patho-anatomical risk factors thus avoiding more invasive procedures [6]. During MPFL reconstruction, for a correct femoral ligament insertion, the radiographic method described by Schöttle et al. [7]. For the patellar ligament insertion, both medial retinaculum and native MPFL are dissected from the patella, leaving the capsule layer intact. Patellar insertion can be performed either via a single (SB) or a double-bundle (DB) procedure. Several techniques are described for MPFL reconstruction either via single and double bundles. The DB was developed to simulate anatomical stress distribution [8] and was designed to reduce the rate of failures and complications [9, 10]. However, results are controversial, and debates are still ongoing [11–14].
Hence, the purpose of this study is to perform a systematic review comparing SB versus DB grafts for recurrent patellofemoral instability, to summarize the current evidence, and clarify the role of both the techniques. We focused on the clinical scores, physical examination, complications, revision surgeries and failures.
Material and methods
Search strategy
This systematic review was conducted according to the Preferred reporting items for systematic reviews and meta-analyses (PRISMA) [15]. A preliminary protocol was drafted to outline the search parameters:
P (population): recurrent patellofemoral instability;
I (intervention): isolated MPFL reconstruction;
C (comparison): double versus single bundle tendon graft;
O (outcome): clinical scores and examination, complications, surgical revision and failure.
Literature search
The search was conducted by two independent authors (FM, JE) in May 2019. The following databases were accessed: Pubmed, Scopus, Embase, and Google scholar. The following keywords were used in combination: patellofemoral, recurrent, patellar, instability, dislocation, syndrome, luxation, MPFL, reconstruction, isolated, tear, rupture, graft, single, double, bundle, semitendinosus, gracilis, hamstring, synthetic, failure, apprehension test, Kujala, Lysholm. If the title and subsequent abstract matched the topic, the full-text of the article was accessed. The bibliographies of the included articles were also screened to find potentially missed articles. Disagreements between the authors were debated and mutually resolved.
Eligibility criteria
All articles treating MPFL reconstruction for recurrent patellofemoral instability through a single and/ or double-bundle graft were enrolled in the present systematic review. According to the authors language capabilities, only articles in Italian, German, English, French, Spanish were included. According to the Oxford Centre of Evidenced-Based Medicine [16], articles with the level of evidence I to IV were considered for inclusion. Only articles reporting primary MPFL reconstruction were included in the present study. Only articles reporting isolated MPFL reconstruction were considered. Comments, techniques, editorials, letters, protocols, expert opinion, and guidelines were excluded. Biomechanical, animal, and cadaveric studies were also excluded. Only articles reporting a minimum of 12-months follow-up were considered. Studies treating patellofemoral instability after total knee arthroplasty were also rejected. Only articles that reported quantitative data concerning the endpoints of interest were included. Disagreements between the authors were debated and mutually resolved.
Outcomes of interest
Two independent authors (FM, JE) recorded the following data: study generalities (author, year, type of study), patient baselines (mean age, duration of the follow-up, time injury to surgery), type of instability (recurrent and/ or acute), presence of risk factors (trochlear dysplasia, patella alta, elevated TT-TG), and surgical graft fixation. Data concerning the following parameters were also recorded: Kujala Anterior Knee Pain Scale [17], Lysholm Knee Scoring Scale [18], Tegner Activity Scale [19], International Knee Documentation Committee (IKCD) [20], visual analogic scale (VAS) and knee range of motion (ROM). In addition, clinical examination, complications, further re-operations, and failures were recorded.
Methodological quality assessment
For the methodological quality assessment, the PEDro score was performed. This score was evaluated by two independent authors (FM, JE). This score analyses the included articles under several points of view: statement of the eligibility criteria, allocation, randomization and blinding methods, duration of follow-up, intention to treat, point estimates, and variability. The final value ranks from 0 (poor quality) to 10 (excellent quality). Value > 6 points are considered acceptable.
Statistical analysis
The statistical analyses were performed through the IBM SPSS Statistic software. Continuous data were analysed via arithmetic mean, standard deviation and range of interval. Binary data were analysed through the odd ratio (OR) effect measure. The confidence interval was set at 95% in all the comparisons. The unpaired t-test was performed in all the comparisons. A P value < 0.05 was considered statistically significant.
Results
Search result
From the initial search, we obtained a total of 1105 articles. From this pool, 301 were rejected due to duplication. Another 478 articles were excluded due to discrepancies in meeting eligibility criteria. A further 275 articles were rejected due to the lack of quantitative data concerning the outcomes of interest. This left 51 articles for inclusion. Of them, another 6 articles were excluded due to uncertain data. Ultimately, a total of 46 studies were included, 29 performing double-bundle MPFL reconstruction, 16 using the single-bundle technique, 1 comparing both the techniques. We enrolled four randomized clinical trials (RCT), 19 prospective cohort studies (PCS), 19 retrospective cohort studies (RCS), four case series (CS). The type of the included studies according to the grafts are shown in Table 1. The flow-chart of the literature search is shown in Fig. 1.
Table 1.
Generalities, demographic data and related PEDro scores of the included studies concerning the DB graft
| Author, year | Type of study | PEDro score | Knees (n) | Mean age | Time injury to surgery | Mean follow-up (months) |
|---|---|---|---|---|---|---|
| Astur et al. 2015 [11] | RCT | 8 | 28 | 28.32 | 60.00 | |
| Bitar et al. 2012 [21] | PCS | 7 | 56 | 23.00 | 19.30 | |
| Christiansen et al. 2008 [22] | PCS | 6 | 32 | 22.00 | 84.00 | 22.00 |
| Csintalan et al. 2014 [23] | CS | 5 | 56 | 24.30 | 86.40 | 51.00 |
| Deie et al. 2011 [24] | RCS | 5 | 31 | 22.20 | 39.00 | |
| Feller et al. 2014 [25] | RCS | 5 | 26 | 24.40 | 88.80 | 42.00 |
| Fink et al. 2014 [26] | PCS | 7 | 17 | 21.50 | 12.00 | |
| Goncaives et al. 2011 [27] | PCS | 6 | 22 | 28.60 | 141.00 | 26.20 |
| Hinterwimmer et al. 2013 [28] | RCS | 6 | 19 | 23.00 | 16.00 | |
| Kang et al. 2013 [29] | RCT | 8 | 82 | 28.75 | 24.00 | |
| Kita et al. 2015 [30] | PCS | 7 | 44 | 25.40 | 156.00 | 39.00 |
| Krishna Kumar et al. 2014 [31] | PCS | 7 | 30 | 18.00 | 33.53 | 25.00 |
| Kumahashi et al. 2012 [32] | PCS | 6 | 5 | 13.60 | 19.00 | 27.80 |
| Kumahashi et al. 2016 [33] | PCS | 7 | 17 | 22.00 | 61.00 | 45.00 |
| Li et al. 2014 [34] | PCS | 7 | 65 | 29.40 | 78.50 | |
| Lind et al. 2016 [35] | PCS | 8 | 24 | 12.50 | 39.00 | |
| Lind et al. 2016 [35] | PCS | 8 | 179 | 23.00 | 41.00 | |
| Lin et al. 2015 [36] | RCS | 5 | 18 | N/R | 35.00 | |
| Lippacher et al. 2014 [37] | RCS | 7 | 68 | 18.30 | 24.70 | |
| Ma et al. 2013 [38] | RCT | 8 | 32 | 28.40 | 26.00 | 40.00 |
| Matsushita et al. 2014 [39] | RCS | 6 | 21 | 22.10 | 44.00 | |
| Matsushita et al. 2014 [39] | RCS | 6 | 18 | 23.50 | 38.00 | |
| Niu et al. 2017 [40] | PCS | 7 | 30 | 25.00 | 55.10 | |
| Panni et al. 2011 [41] | CS | 5 | 48 | 25.00 | 12.00 | 33.00 |
| Ronga et al. 2009 [42] | PCS | 5 | 37 | 28.00 | 37.00 | |
| Sadigursky et al. 2016 [43] | PCS | 7 | 31 | 29.38 | 12.00 | |
| Smith et al. 2014 [44] | RCS | 6 | 21 | 23.00 | 95.00 | 12.00 |
| Suganuma et al. 2016 [45] | RCS | 6 | 18 | 20.70 | 51.60 | |
| Suganuma et al. 2016 [45] | RCS | 6 | 28 | 20.30 | 48.00 | |
| Thaunat et al. 2007 [46] | RCS | 5 | 23 | 22.00 | 28.00 | |
| Toritsuka et al. 2011 [47] | CS | 6 | 20 | 23.80 | 30.00 | |
| Wang et al. 2013 [46] | RCS | 7 | 44 | 26.00 | 48.00 | |
| Wang et al. 2016 [48] | RCS | 6 | 26 | 26.30 | 38.20 | |
| Wantabe et al. 2008 [49] | RCS | 7 | 29 | 19.00 | 43.20 | 51.60 |
| Zhang et al. 2019 [50] | PCS | 7 | 60 | 21.00 | 12.00 | 96.00 |
RCT randomized clinical trial, PCS prospective cohort study, RCS retrospective cohort study, CS case series
Fig. 1.
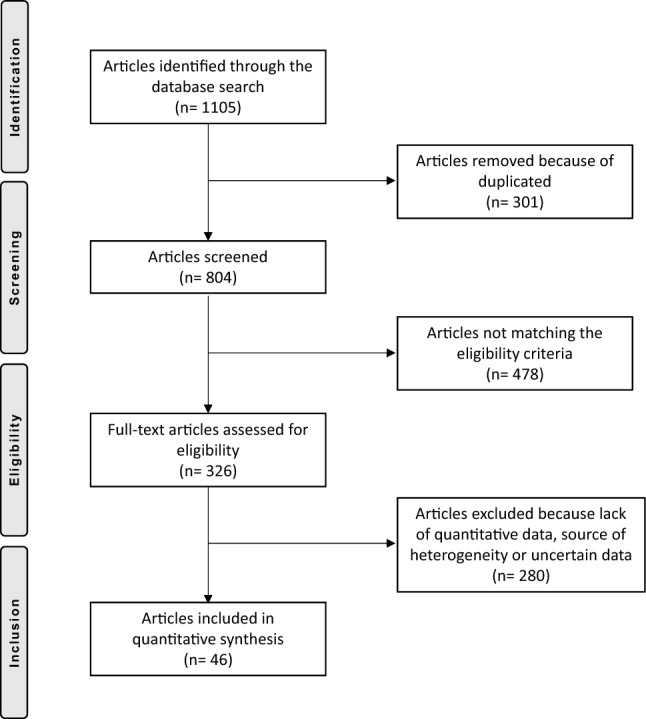
PRISMA flow-chart of the literature search
Methodological quality assessment
The PEDro score evidenced some weakness of this systematic review. Only 9% of the articles provided randomization. None of the included articles provided blinding methods. However, the overall quality of the included papers, the follow-up duration, and the number of included patients were acceptable. In total, the PEDro score resulted in 6.34 ± 1.1 points, attesting to the good methodological quality assessment of this systematic review. The results of the PEDro score assigned for each study are shown in Tables 1 and 2.
Table 2.
Generalities, demographic data and related PEDro scores of the included studies concerning the SB graft
| Author, year | Type of study | PEDro score | Knees (n) | Mean age | Time surgery to injury | Mean follow-up (months) |
|---|---|---|---|---|---|---|
| Ahmad et al. 2009 [51] | CS | 5 | 20 | 23.00 | 31.00 | |
| Amin et al. 2015 [52] | RCS | 6 | 8 | 22.00 | 9.00 | 24.00 |
| Astur et al. 2015 [11] | RCT | 8 | 30 | 31.06 | 60.00 | |
| Bitar et al. 2011 [53] | RCT | 8 | 21 | NR | 24.00 | |
| Calapodopulos et al. 2016 [54] | PCS | 5 | 22 | 23.10 | 30.00 | |
| Ellera Gomes et al. 1992 [55] | RCS | 5 | 30 | 28.00 | 90.00 | 39.00 |
| Ellera Gomes et al. 2004 [56] | PCS | 6 | 16 | 26.70 | 1.00 | 60.00 |
| Gomes et al. 2008 [57] | PCS | 7 | 12 | 19.30 | 53.00 | |
| Goyal et al. 2013 [58] | RCS | 5 | 32 | 25.00 | 38.00 | |
| Han et al. 2011 [59] | RCS | 6 | 59 | 24.30 | 45.60 | 68.40 |
| Hiemstra et al. 2017 [60] | RCS | 5 | 155 | 25.40 | 24.40 | |
| Howells et al. 2012 [61] | PCS | 7 | 155 | 26.00 | 16.00 | |
| Howells et al. 2012 [61] | PCS | 7 | 55 | 26.00 | 16.00 | |
| Nomura et al. 2000 [62] | PCS | 7 | 27 | 21.00 | 55.20 | 70.80 |
| Nomura et al. 2006 [63] | RCS | 6 | 12 | 24.80 | 122.40 | 51.00 |
| Nomura et al. 2007 [64] | RCS | 5 | 24 | 22.50 | 142.80 | |
| Pinheiro et al. 2018 [65] | RCS | 7 | 16 | 27.10 | 31.20 | |
| Pinheiro et al. 2018 [65] | RCS | 7 | 21 | 26.40 | 34.80 | |
| Raghuveer et al. 2012 [66] | PCS | 7 | 15 | 29.20 | 141.60 | 42.00 |
| Sillanpaa et al. 2008 [67] | RCS | 6 | 18 | 20.20 | 121.20 | |
| Slenker et al. 2013 [68] | RCS | 6 | 35 | 20.60 | 57.60 | 21.00 |
| Steiner et al. 2006 [69] | CS | 6 | 34 | 27.00 | 66.50 | |
| Vavalle et al. 2015 [70] | RCS | 5 | 16 | 22.00 | 38.00 | |
| Wang et al. 2013 [12] | RCS | 7 | 26 | 23.00 | 48.00 | |
| Wang et al. 2010 [71] | RCS | 7 | 28 | 29.00 | 30.00 | 42.00 |
RCT randomized clinical trial, PCS prospective cohort study, RCS retrospective cohort study, CS case series
Patient demographic
Data from 2204 patients were obtained. The patients at the time of surgery had a mean age of 23.66 ± 3.7 years. The mean duration of the follow-up was 45.02 ± 22.1 months. 24% of the studies harvested the gracilis tendon for the reconstruction, 60% the semitendinosus. Other grafts were the adductor magnus, quadriceps, patellar, hamstring, tibialis anterior, and five synthetic tendons. In the DB group, a total of 1305 patients were enrolled, with a mean age of 23.01 ± 4.0 years. The time between the first dislocation and surgery in this group was 65.99 ± 47.5 months (Table 1). In the SB group, a total of 899 patients were enrolled, with a mean age of 24.53 ± 3.3 years. The time between the first dislocation and surgery in this group was 61.38 ± 48.3 months (Table 2). No significant discrepancies between the two groups concerning age and time injury to surgery were detected (P = 0.07 and P = 0.4, respectively).
Outcomes of interest
The DB group reported a mean Kujala score of 89.84% (range 71.0–97.7, SD 5.9), mean Lysholm score of 91.79% (range 87.9–96.4, SD 2.7), mean Tegner score of 5.36 (range 4.0–7.8, SD 1.1), mean IKDC of 81.58% (range 76.3–91.3, SD 6.0), mean VAS of 21.30% (range 1.40–3.90, SD 1.0) and mean ROM of 137.70° (range 145.0–125.9, SD 6.4). The SB group reported a mean Kujala score of 86.62% (range 75.2–96.0, SD 5.6), mean Lysholm score of 86.67% (range 79.1–92.1, SD 4.3), mean Tegner score of 5.06 (range 4.0–5.6, SD 0.6), mean IKDC of 76.18% (range 68.9–82.3, SD 6.8), mean VAS of 20.50% (range 1.0–4.3, SD 2.3), and mean ROM 127.73° (range 117.2–141, SD 12.1). All these endpoints scored in favour of the DB group: Kujala (+ 3.2, P = 0.03), Lysholm (+ 5.1, P = 0.001), Tegner (+ 0.3, P = 0.2), IKDC (+ 5.4, P = 0.01), VAS (+ 0.8, P = 0.3), ROM (+ 9.96, P = 0.04). In the DB graft, a reduction of overall complications (OR 0.59; 95% CI 0.37–0.89 P = 0.1), further surgeries (OR 0.64; 95% CI 0.35–1.14; P = 0.12) and re-dislocations (OR 0.61; 95% CI 0.31–1.21; P = 0.16) was observed. The SB group reported a reduction in the post-operative apprehension test (OR 2.42; 95% CI 1.42–4.12; P = 0.24).
Discussion
According to the main findings of this systematic review, the DB graft scored greater in terms of mean ROM, Kujala, IKDC, and Lysholm scores. Tegner score and VAS, further complications, revisions, and re-dislocations rate were remarkably in favour of the DB graft group, however, no statistically significance was found.
Recently, Kang et al. [72], performed a systematic review comparing SB versus DB using exclusively the hamstring tendon. They analysed 1116 knees (254 SB versus 862 DB), and focused on the Kujala score, apprehension test, re-dislocations, and overall complications. An increased risk of post-operative apprehension test in the SB group and of joint stiffness in the DB group was shown. No other relevant differences between the two grafts were detected. Lee et al. [73] performed recently a meta-analysis analysing the surgical techniques for patellofemoral instability. They reviewed even two clinical trials [12, 14] that compared DB vs SB, founding reduced instability, revisions and better clinical scores result in the DB group [73]. Two biomechanical studies [74, 75], comparing the two bundle methods, revealed that both reconstructions are able to restore adequate patellar stability. Placella et al. [75] stated that the ultimate load was 213 ± 90 N and 171 ± 51 N for the DB and SB, respectively. It was shown that the DB is more anatomical with better physiological stress distribution and, therefore, simulates the ultimate load more so than the SB graft [75], and better mimics the MPFL track at reduced flexion angles [74]. Furthermore, Wang et al. [74] found that the DB generates greater resistance to lateral displacement at the first 15° of knee flexion. Recently, Kang et al. [76] performed a systematic review of over 691 procedures comparing the techniques for patellar fixation in DB-MPFL reconstruction. They found a similarity between bone tunnel, suture anchors and suture techniques in terms of Kujala score, apprehension test, dislocation rate and further complications [76]. They stated that all these techniques achieve satisfactory patellar fixation for DB-MPFL reconstruction [76].
In the present systematic review, all scores of interests were remarkably in favour of the DB graft, with a good homogeneity of values in all comparisons. The range of values was narrow, especially for the Lysohlm score and IKDC. The standard deviation was small in all comparisons, detecting low data dispersion and feasible results. Similar observations were seen for the comparison of ROM, which reports a considerable improvement in favour of the DB graft. As such, these results are trustworthy and reliable. The Tegner score and visual analogic scale reported minimally improved values in the DB graft group. Data from these scores were reported by few studies and are not sufficient to draft reliable conclusions. Additionally, the level of significance according to the t-test is poor, detecting similarity between the techniques. Concerning the other outcomes of interest, no statistically significant result was obtained among all the comparisons. The t test detected marked similarity between the techniques in all the comparisons. However, the results of the comparisons of further surgeries and re-dislocations were considerably in favour of the SB graft. The analysis of the overall complications detected remarkable risk in the SB graft group, and the value of the t test was closer to the cut-off. All other comparisons detected minimal differences between the two groups.
Limitations of this work are several. First, most of the enrolled studies had poor level of evidence, being mostly retrospective. Few studies randomized samples, while none took advantage of blinding methods. Therefore, the overall quality was remarkably reduced, and data from this work must be interpreted with caution. Heterogeneous inclusion and exclusion criteria, along with the poor analysis reported by some of the enrolled studies, were other important limitations. Data analysis were performed regardless of the type of graft (autografts, allografts, synthetics). Further studies should be addressed to clarify the role of each grafts and related potential advantages. However, the comprehensive nature of the literature search, along with the strict eligibility criteria represent important points of strength of this systematic review. Furthermore, the good quality of the methodological assessment and the optimal baseline comparability decreased the risk of publication bias, improving the overall reliability of this work.
Conclusion
The main findings of this systematic review support that a double bundle graft achieves statistically significant improvement in joint function in patients with patellofemoral instability who undergo MPFL reconstruction. Improvement was evidenced in the range of motion, Kujala, IKDC, and Lysholm scores compared to a single bundle graft.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study informed consent is not required.
Footnotes
The original online version of this article was revised due to a retrospective Open Access order.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
7/19/2021
A Correction to this paper has been published: 10.1007/s00402-021-04012-w
References
- 1.Sillanpää PMV, Iivonen T, et al. Incidence and risk factors of acute traumatic primary patellar dislocation. Med Sci Sports Exerc. 2008;40(4):606–611. doi: 10.1249/MSS.0b013e318160740f. [DOI] [PubMed] [Google Scholar]
- 2.Sallay PI, Poggi J, Speer KP, Garrett WE. Acute dislocation of the patella. A correlative pathoanatomic study. Am J Sports Med. 1996;24(1):52–60. doi: 10.1177/036354659602400110. [DOI] [PubMed] [Google Scholar]
- 3.Kaplan EB. Factors responsible for the stability of the knee joint. Bull Hosp Joint Dis. 1957;18(1):51–59. [PubMed] [Google Scholar]
- 4.Trikha SP, Acton D, O'Reilly M, Curtis MJ, Bell J. Acute lateral dislocation of the patella: correlation of ultrasound scanning with operative findings. Injury. 2003;34(8):568–571. doi: 10.1016/S0020-1383(02)00382-0. [DOI] [PubMed] [Google Scholar]
- 5.Longo UG, Berton A, Salvatore G, Migliorini F, Ciuffreda M, Nazarian A, Denaro V. Medial patellofemoral ligament reconstruction combined with bony procedures for patellar instability: current indications, outcomes, and complications. Arthroscopy. 2016;32(7):1421–1427. doi: 10.1016/j.arthro.2016.01.013. [DOI] [PubMed] [Google Scholar]
- 6.Bartsch A, Lubberts B, Mumme M, Egloff C, Pagenstert G. Does patella alta lead to worse clinical outcome in patients who undergo isolated medial patellofemoral ligament reconstruction? A systematic review. Arch Orthop Trauma Surg. 2018;138(11):1563–1573. doi: 10.1007/s00402-018-2971-4. [DOI] [PubMed] [Google Scholar]
- 7.Schottle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(5):801–804. doi: 10.1177/0363546506296415. [DOI] [PubMed] [Google Scholar]
- 8.Kang HJ, Wang F, Chen BC, Su YL, Zhang ZC, Yan CB. Functional bundles of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2010;18(11):1511–1516. doi: 10.1007/s00167-010-1090-8. [DOI] [PubMed] [Google Scholar]
- 9.Schottle PB, Hensler D, Imhoff AB. Anatomical double-bundle MPFL reconstruction with an aperture fixation. Knee Surg Sports Traumatol Arthrosc. 2010;18(2):147–151. doi: 10.1007/s00167-009-0868-z. [DOI] [PubMed] [Google Scholar]
- 10.Stupay KL, Swart E, Shubin Stein BE. Widespread implementation of medial patellofemoral ligament reconstruction for recurrent patellar instability maintains functional outcomes at midterm to long-term follow-up while decreasing complication rates: a systematic review. Arthroscopy. 2015;31(7):1372–1380. doi: 10.1016/j.arthro.2014.12.029. [DOI] [PubMed] [Google Scholar]
- 11.Astur DC, Gouveia GB, Borges JH, Astur N, Arliani GG, Kaleka CC, Cohen M. Medial patellofemoral ligament reconstruction: a longitudinal study comparison of 2 techniques with 2 and 5-years follow-up. Open Orthop J. 2015;9:198–203. doi: 10.2174/1874325001509010198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang CH, Ma LF, Zhou JW, Ji G, Wang HY, Wang F, Wang J. Double-bundle anatomical versus single-bundle isometric medial patellofemoral ligament reconstruction for patellar dislocation. Int Orthop. 2013;37(4):617–624. doi: 10.1007/s00264-013-1788-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mikashima Y, Kimura M, Kobayashi Y, Miyawaki M, Tomatsu T. Clinical results of isolated reconstruction of the medial patellofemoral ligament for recurrent dislocation and subluxation of the patella. Acta Orthop Belg. 2006;72(1):65–71. [PubMed] [Google Scholar]
- 14.Mohammed R, Hunt N, Gibbon AJ. Patellar complications in single versus double tunnel medial patellofemoral ligament reconstruction. J Orthop Surg (Hong Kong) 2017;25(1):2309499017691007. doi: 10.1177/2309499017691007. [DOI] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Howick J CI, Glasziou P, Greenhalgh T, Heneghan C, Liberati A, Moschetti I, Phillips B, Thornton H, Goddard O, Hodgkinson M (2011) The 2011 Oxford levels of evidence. Oxford Centre for evidence-based medicine. https://www.cebm.net/indexaspx?o=5653. Accessed May 2019
- 17.Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9(2):159–163. doi: 10.1016/S0749-8063(05)80366-4. [DOI] [PubMed] [Google Scholar]
- 18.Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10(3):150–154. doi: 10.1177/036354658201000306. [DOI] [PubMed] [Google Scholar]
- 19.Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med. 2009;37(5):890–897. doi: 10.1177/0363546508330143. [DOI] [PubMed] [Google Scholar]
- 20.Higgins LD, Taylor MK, Park D, Ghodadra N, Marchant M, Pietrobon R, Cook C, International Knee Documentation C Reliability and validity of the International Knee Documentation Committee (IKDC) Subjective Knee Form. Joint Bone Spine. 2007;74(6):594–599. doi: 10.1016/j.jbspin.2007.01.036. [DOI] [PubMed] [Google Scholar]
- 21.Bitar AC, Demange MK, D'Elia CO, Camanho GL. Traumatic patellar dislocation: nonoperative treatment compared with MPFL reconstruction using patellar tendon. Am J Sports Med. 2012;40(1):114–122. doi: 10.1177/0363546511423742. [DOI] [PubMed] [Google Scholar]
- 22.Christiansen SE, Jacobsen BW, Lund B, Lind M. Reconstruction of the medial patellofemoral ligament with gracilis tendon autograft in transverse patellar drill holes. Arthroscopy. 2008;24(1):82–87. doi: 10.1016/j.arthro.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 23.Csintalan RP, Latt LD, Fornalski S, Raiszadeh K, Inacio MC, Fithian DC. Medial patellofemoral ligament (MPFL) reconstruction for the treatment of patellofemoral instability. J Knee Surg. 2014;27(2):139–146. doi: 10.1055/s-0033-1360652. [DOI] [PubMed] [Google Scholar]
- 24.Deie M, Ochi M, Adachi N, Shibuya H, Nakamae A. Medial patellofemoral ligament reconstruction fixed with a cylindrical bone plug and a grafted semitendinosus tendon at the original femoral site for recurrent patellar dislocation. Am J Sports Med. 2011;39(1):140–145. doi: 10.1177/0363546510377436. [DOI] [PubMed] [Google Scholar]
- 25.Feller JA, Richmond AK, Wasiak J. Medial patellofemoral ligament reconstruction as an isolated or combined procedure for recurrent patellar instability. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2470–2476. doi: 10.1007/s00167-014-3132-0. [DOI] [PubMed] [Google Scholar]
- 26.Fink C, Veselko M, Herbort M, Hoser C. MPFL reconstruction using a quadriceps tendon graft: part 2: operative technique and short term clinical results. Knee. 2014;21(6):1175–1179. doi: 10.1016/j.knee.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 27.Gonçaives MBJ, Júnior LHdC, Soares LFM, Gonçaives TJ, dos Santos RL, Pereira ML. Medial patellofemoral ligament reconstruction to treat recurrent patellar dislocation. Revista Brasileira de Ortopedia (English Edition) 2011;46(2):160–164. doi: 10.1016/s2255-4971(15)30233-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hinterwimmer S, Imhoff AB, Minzlaff P, Saier T, Rosenstiel N, Hawe W, Feucht MJ. Anatomical two-bundle medial patellofemoral ligament reconstruction with hardware-free patellar graft fixation: technical note and preliminary results. Knee Surg Sports Traumatol Arthrosc. 2013;21(9):2147–2154. doi: 10.1007/s00167-013-2498-8. [DOI] [PubMed] [Google Scholar]
- 29.Kang H, Cao J, Yu D, Zheng Z, Wang F. Comparison of 2 different techniques for anatomic reconstruction of the medial patellofemoral ligament: a prospective randomized study. Am J Sports Med. 2013;41(5):1013–1021. doi: 10.1177/0363546513480468. [DOI] [PubMed] [Google Scholar]
- 30.Kita K, Tanaka Y, Toritsuka Y, Amano H, Uchida R, Takao R, Horibe S. Factors affecting the outcomes of double-bundle medial patellofemoral ligament reconstruction for recurrent patellar dislocations evaluated by multivariate analysis. Am J Sports Med. 2015;43(12):2988–2996. doi: 10.1177/0363546515606102. [DOI] [PubMed] [Google Scholar]
- 31.Krishna Kumar M, Renganathan S, Joseph CJ, Easwar T, Rajan DV. Medial patellofemoral ligament reconstruction in patellar instability. Indian J Orthop. 2014;48(5):501–505. doi: 10.4103/0019-5413.139864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kumahashi N, Kuwata S, Tadenuma T, Kadowaki M, Uchio Y. A "sandwich" method of reconstruction of the medial patellofemoral ligament using a titanium interference screw for patellar instability in skeletally immature patients. Arch Orthop Trauma Surg. 2012;132(8):1077–1083. doi: 10.1007/s00402-012-1516-5. [DOI] [PubMed] [Google Scholar]
- 33.Kumahashi N, Kuwata S, Takuwa H, Egusa N, Uchio Y. Longitudinal change of medial and lateral patellar stiffness after reconstruction of the medial patellofemoral ligament for patients with recurrent patellar dislocation. J Bone Joint Surg Am. 2016;98(7):576–583. doi: 10.2106/JBJS.15.00605. [DOI] [PubMed] [Google Scholar]
- 34.Li J, Li Y, Wei J, Wang J, Gao S, Shen Y. A simple technique for reconstruction of medial patellofemoral ligament with bone-fascia tunnel fixation at the medial margin of the patella: a 6-year-minimum follow-up study. J Orthop Surg Res. 2014;9:66. doi: 10.1186/s13018-014-0066-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lind M, Enderlein D, Nielsen T, Christiansen SE, Fauno P. Clinical outcome after reconstruction of the medial patellofemoral ligament in paediatric patients with recurrent patella instability. Knee Surg Sports Traumatol Arthrosc. 2016;24(3):666–671. doi: 10.1007/s00167-014-3439-x. [DOI] [PubMed] [Google Scholar]
- 36.Lin KY, Lu YC, Renn JH. The double-pulley technique for anatomical double-bundled medial patellofemoral ligament reconstruction. Injury. 2015;46(8):1619–1624. doi: 10.1016/j.injury.2015.04.017. [DOI] [PubMed] [Google Scholar]
- 37.Lippacher S, Dreyhaupt J, Williams SR, Reichel H, Nelitz M. Reconstruction of the medial patellofemoral ligament: clinical outcomes and return to sports. Am J Sports Med. 2014;42(7):1661–1668. doi: 10.1177/0363546514529640. [DOI] [PubMed] [Google Scholar]
- 38.Ma LF, Wang F, Chen BC, Wang CH, Zhou JW, Wang HY. Medial retinaculum plasty versus medial patellofemoral ligament reconstruction for recurrent patellar instability in adults: a randomized controlled trial. Arthroscopy. 2013;29(5):891–897. doi: 10.1016/j.arthro.2013.01.030. [DOI] [PubMed] [Google Scholar]
- 39.Matsushita T, Kuroda R, Oka S, Matsumoto T, Takayama K, Kurosaka M. Clinical outcomes of medial patellofemoral ligament reconstruction in patients with an increased tibial tuberosity-trochlear groove distance. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2438–2444. doi: 10.1007/s00167-014-2919-3. [DOI] [PubMed] [Google Scholar]
- 40.Niu J, Qi Q, Fu K, Duan G, Liu C, Wang F. Medial patellofemoral ligament reconstruction with semi-patellar tunnel fixation: surgical technique and mid-term follow-up. Med Sci Monit. 2017;23:5870–5875. doi: 10.12659/msm.905583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Panni AS, Alam M, Cerciello S, Vasso M, Maffulli N. Medial patellofemoral ligament reconstruction with a divergent patellar transverse 2-tunnel technique. Am J Sports Med. 2011;39(12):2647–2655. doi: 10.1177/0363546511420079. [DOI] [PubMed] [Google Scholar]
- 42.Ronga M, Oliva F, Longo UG, Testa V, Capasso G, Maffulli N. Isolated medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2009;37(9):1735–1742. doi: 10.1177/0363546509333482. [DOI] [PubMed] [Google Scholar]
- 43.Sadigursky D, de Melo Laranjeira MS, Nunes M, Caneiro RJ, Colavolpe PO. Reconstruction of the medial patellofemoral ligament by means of the anatomical double-bundle technique using metal anchors. Rev Bras Ortop. 2016;51(3):290–297. doi: 10.1016/j.rboe.2015.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Smith TO, Mann CJ, Donell ST. Does knee joint proprioception alter following medial patellofemoral ligament reconstruction? Knee. 2014;21(1):21–27. doi: 10.1016/j.knee.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 45.Suganuma J, Mochizuki R, Sugiki T, Inoue Y, Kitamura K, Akutsu S, Ono H. Reconstruction of the medial patellofemoral ligament using a synthetic graft with arthroscopic control of patellofemoral congruence. Arthroscopy. 2016;32(11):2259–2268. doi: 10.1016/j.arthro.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 46.Thaunat M, Erasmus PJ. The favourable anisometry: an original concept for medial patellofemoral ligament reconstruction. Knee. 2007;14(6):424–428. doi: 10.1016/j.knee.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 47.Toritsuka Y, Amano H, Mae T, Uchida R, Hamada M, Ohzono K, Shino K. Dual tunnel medial patellofemoral ligament reconstruction for patients with patellar dislocation using a semitendinosus tendon autograft. Knee. 2011;18(4):214–219. doi: 10.1016/j.knee.2010.05.007. [DOI] [PubMed] [Google Scholar]
- 48.Wang HD, Dong JT, Gao SJ. Medial patellofemoral ligament reconstruction using a bone groove and a suture anchor at patellar: a safe and firm fixation technique and 3-year follow-up study. J Orthop Surg Res. 2016;11(1):138. doi: 10.1186/s13018-016-0473-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Watanabe T, Muneta T, Ikeda H, Tateishi T, Sekiya I. Visual analog scale assessment after medial patellofemoral ligament reconstruction: with or without tibial tubercle transfer. J Orthop Sci. 2008;13(1):32–38. doi: 10.1007/s00776-007-1196-0. [DOI] [PubMed] [Google Scholar]
- 50.Zhang L, Li Z. Long-Term Clinical Results of Double Bundle Reconstruction of the Medial Patellofemoral Ligament for Patellar Instability. J Knee Surg. 2019;32(2):153–159. doi: 10.1055/s-0038-1636913. [DOI] [PubMed] [Google Scholar]
- 51.Ahmad CS, Brown GD, Shubin Stein BE. The docking technique for medial patellofemoral ligament reconstruction: surgical technique and clinical outcome. Am J Sports Med. 2009;37(10):2021–2027. doi: 10.1177/0363546509336261. [DOI] [PubMed] [Google Scholar]
- 52.Amin NH, Lynch TS, Patel RM, Patel N, Saluan P. Medial patellofemoral ligament reconstruction. JBJS Rev. 2015 doi: 10.2106/JBJS.RVW.N.00089. [DOI] [PubMed] [Google Scholar]
- 53.Bitar AC, D'Elia CO, Demange MK, Viegas AC, Camanho GL. Randomized prospective study on traumatic patellar dislocation: conservative treatment versus reconstruction of the medial patellofemoral ligament using the patellar tendon, with a minimum of two years of follow-up. Revista Brasileira de Ortopedia (English Edition) 2011;46(6):675–683. doi: 10.1016/s2255-4971(15)30324-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Calapodopulos CJ, Nogueira MC, Eustaquio JM, Calapodopulos Junior CJ, Rodrigues OA. Reconstruction of the medial patellofemoral ligament using autologous graft from quadriceps tendon to treat recurrent patellar dislocation. Rev Bras Ortop. 2016;51(2):187–193. doi: 10.1016/j.rboe.2016.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ellera Gomes JL. Medial patellofemoral ligament reconstruction for recurrent dislocation of the patella: a preliminary report. Arthroscopy. 1992;8(3):335–340. doi: 10.1016/0749-8063(92)90064-I. [DOI] [PubMed] [Google Scholar]
- 56.Ellera Gomes JL, Stigler Marczyk LR, Cesar de Cesar P, Jungblut CF. Medial patellofemoral ligament reconstruction with semitendinosus autograft for chronic patellar instability: a follow-up study. Arthroscopy. 2004;20(2):147–151. doi: 10.1016/j.arthro.2003.11.006. [DOI] [PubMed] [Google Scholar]
- 57.Gomes JE. Comparison between a static and a dynamic technique for medial patellofemoral ligament reconstruction. Arthroscopy. 2008;24(4):430–435. doi: 10.1016/j.arthro.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 58.Goyal D. Medial patellofemoral ligament reconstruction: the superficial quad technique. Am J Sports Med. 2013;41(5):1022–1029. doi: 10.1177/0363546513477828. [DOI] [PubMed] [Google Scholar]
- 59.Han H, Xia Y, Yun X, Wu M. Anatomical transverse patella double tunnel reconstruction of medial patellofemoral ligament with a hamstring tendon autograft for recurrent patellar dislocation. Arch Orthop Trauma Surg. 2011;131(3):343–351. doi: 10.1007/s00402-010-1173-5. [DOI] [PubMed] [Google Scholar]
- 60.Hiemstra LA, Kerslake S, Lafave M. Medial patellofemoral ligament reconstruction femoral tunnel accuracy: relationship to disease-specific quality of life. Orthop J Sports Med. 2017;5(2):2325967116687749. doi: 10.1177/2325967116687749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Howells NR, Barnett AJ, Ahearn N, Ansari A, Eldridge JD. Medial patellofemoral ligament reconstruction: a prospective outcome assessment of a large single centre series. J Bone Joint Surg Br. 2012;94(9):1202–1208. doi: 10.1302/0301-620X.94B9.28738. [DOI] [PubMed] [Google Scholar]
- 62.Nomura E. Classification of lesions of the medial patello-femoral ligament in patellar dislocation. Int Orthop. 1999;23(5):260–263. doi: 10.1007/s002640050366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nomura E, Inoue M. Hybrid medial patellofemoral ligament reconstruction using the semitendinous tendon for recurrent patellar dislocation: minimum 3 years' follow-up. Arthroscopy. 2006;22(7):787–793. doi: 10.1016/j.arthro.2006.04.078. [DOI] [PubMed] [Google Scholar]
- 64.Nomura E, Inoue M, Kobayashi S. Long-term follow-up and knee osteoarthritis change after medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2007;35(11):1851–1858. doi: 10.1177/0363546507306161. [DOI] [PubMed] [Google Scholar]
- 65.Pinheiro Junior LFB, Cenni MHF, Nicolai OP, Gomes LPH, Leal RS, Coelho DGP. Outcomes of medial patellofemoral ligament reconstruction in patients with patella alta. Rev Bras Ortop. 2018;53(5):570–574. doi: 10.1016/j.rboe.2017.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Raghuveer RK, Mishra CB. Reconstruction of medial patellofemoral ligament for chronic patellar instability. Indian J Orthop. 2012;46(4):447–454. doi: 10.4103/0019-5413.97259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sillanpaa P, Mattila VM, Visuri T, Maenpaa H, Pihlajamaki H. Ligament reconstruction versus distal realignment for patellar dislocation. Clin Orthop Relat Res. 2008;466(6):1475–1484. doi: 10.1007/s11999-008-0207-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Slenker NR, Tucker BS, Pepe MD, Marchetto PA, Cohen SB. Short-/intermediate-term outcomes after medial patellofemoral ligament reconstruction in the treatment of chronic lateral patellofemoral instability. Phys Sportsmed. 2013;41(2):26–33. doi: 10.3810/psm.2013.05.2009. [DOI] [PubMed] [Google Scholar]
- 69.Steiner TM, Torga-Spak R, Teitge RA. Medial patellofemoral ligament reconstruction in patients with lateral patellar instability and trochlear dysplasia. Am J Sports Med. 2006;34(8):1254–1261. doi: 10.1177/0363546505285584. [DOI] [PubMed] [Google Scholar]
- 70.Vavalle G, Capozzi M. Isolated reconstruction of the medial patellofemoral ligament with autologous quadriceps tendon. J Orthop Traumatol. 2016;17(2):155–162. doi: 10.1007/s10195-015-0375-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wang F, Kang HJ, Chen BC, Chen W, Su YL, Zhang YZ. Combination of medial patellofemoral ligament reconstruction with vastus medialis advancement for chronic patellar dislocation. Chin Med J (Engl) 2010;123(21):3024–3029. [PubMed] [Google Scholar]
- 72.Kang H, Zheng R, Dai Y, Lu J, Wang F. Single- and double-bundle medial patellofemoral ligament reconstruction procedures result in similar recurrent dislocation rates and improvements in knee function: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2019;27(3):827–836. doi: 10.1007/s00167-018-5112-2. [DOI] [PubMed] [Google Scholar]
- 73.Lee DY, Park YJ, Song SY, Hwang SC, Park JS, Kang DG. Which technique is better for treating patellar dislocation? A systematic review and meta-analysis. Arthroscopy. 2018;34(11):3082–3093. doi: 10.1016/j.arthro.2018.06.052. [DOI] [PubMed] [Google Scholar]
- 74.Wang Q, Huang W, Cai D, Huang H. Biomechanical comparison of single- and double-bundle medial patellofemoral ligament reconstruction. J Orthop Surg Res. 2017;12(1):29. doi: 10.1186/s13018-017-0530-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Placella G, Speziali A, Sebastiani E, Morello S, Tei MM, Cerulli G. Biomechanical evaluation of medial patello-femoral ligament reconstruction: comparison between a double-bundle converging tunnels technique versus a single-bundle technique. Musculoskelet Surg. 2016;100(2):103–107. doi: 10.1007/s12306-016-0397-0. [DOI] [PubMed] [Google Scholar]
- 76.Kang H, Zheng R, Dong C, Fu K, Wang F. No influence of patellar fixation technique on clinical outcomes of double-bundle medial patellofemoral ligament reconstruction: a systematic review. Arch Orthop Trauma Surg. 2019;139(1):79–90. doi: 10.1007/s00402-018-3008-8. [DOI] [PubMed] [Google Scholar]


