The treatment of complex anal fistula is a challenge, because inappropriate surgery may cause fecal incontinence. Video-assisted anal fistula treatment (VAAFT) and fistula tract laser closure (FiLaC™) are both minimally invasive and sphincter-saving techniques for treating anal fistula. VAAFT can treat fistula tracts under direct vision and FiLaC™ can achieve circular closure of fistula tracts. VAAFT plus FiLaC™ combines the advantages of two technologies and is a promising procedure for complex anal fistula (Figs. 1, 2, 3, 4, 5, 6).
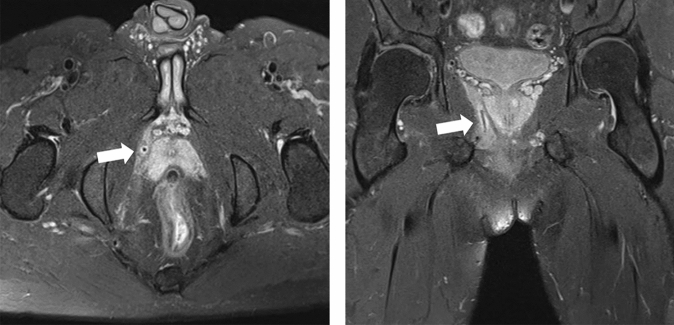
Fig. 1.
Preoperative perianal magnetic resonance imaging shows the long fistula tract (white arrow) located near the prostate and under the levator ani muscle
Fig. 2.
Identification of the fistula tract during the operation. The patient was placed in a lithotomy position under subarachnoid anesthesia. There was a scar and an external opening at 2 cm from the anal verge (white arrow). Exploration with the probe revealed that the fistula tract was about 10 cm long
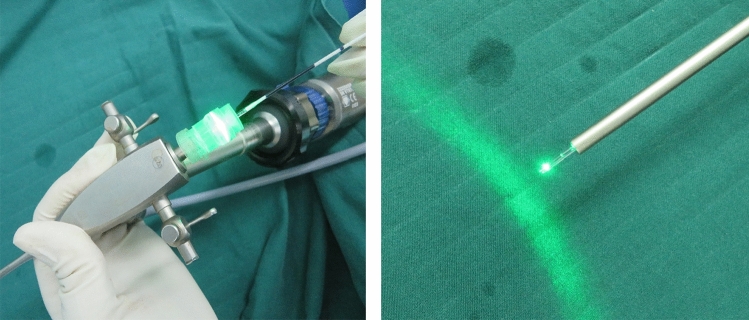
Fig. 3.
Placing laser fibre into the fistuloscope. We replaced unipolar the electrode of VAAFT (Karl Storz GmbH, Tuttlingen, Germany), with the radial laser probe of FiLaC™ (Biolitec Biomedical Technology GmbH, Jena, Germany)
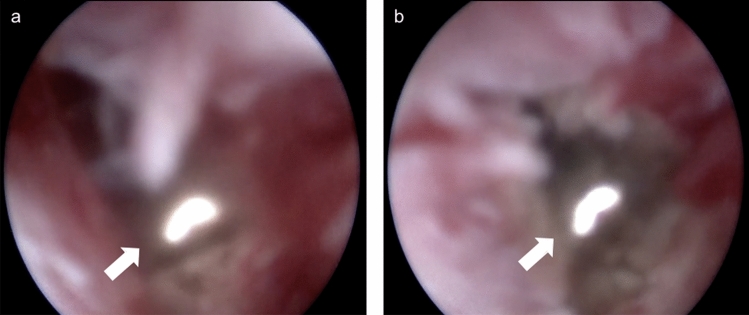
Fig. 4.
Direct vision was provided by the fistuloscope while the radial laser probe (14 W power at wavelength of 1470 nm) was shrinking and sealing the tract (White arrow: radial laser probe). a BEFORE laser closure. b The fistula tract had obviously shrunk after laser closure
Fig. 5.

Wound healing 2 months after the operation
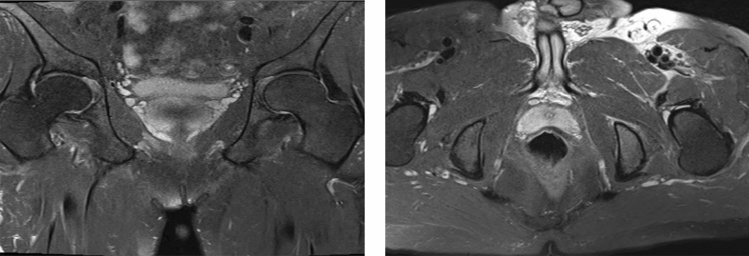
Fig. 6.
Perianal magnetic resonance imaging (MRI) 4 months after the operation. The long fistula tract was disappeared. The perianal MRI shows excellent healing
Authors’ contribution
YBY and CFX wrote the manuscript and prepared the figures (contributed equally to this work). YBY, YQC and Chen Wang drafted the design of the procedure. YBY and CW conducted the procedure. CFX, QTW, HZ and QJD provided postoperative dressing change and follow-up. All authors read and approved the final manuscript.
Funding
Funded by Program for Xinglin Scholar at Shanghai University of Traditional Chinese Medicine (No. RC-2017-02-08); Special General Projects of Clinical Research in Health Industry of Shanghai Municipal Health Commission (No. 202040161); Key Subject Construction Project of Shanghai Municipal Health Commission (Traditional Chinese Medicine Anorectal); Shanghai Famous TCM Doctor Yong-Qing Cao's Studio.
Compliance with ethical standard
Conflict of interest
All authors have nothing to disclose.
Consent for publication
All authors agree to publish. Patient signed informed consent and was willing to submit the information.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yi-Bo Yao and Chang-Fang Xiao contributed equally to this work and are co-first authors.