Abstract
During the present coronavirus disease 2019 (COVID-19) pandemic, transplantation of donor lungs using patients with a history of COVID-19 infection is a critical issue. Donor-derived virus infection and graft dysfunction are possible after transplantation. However use of such lungs could save the lives of patients requiring emergency transplantation. We successfully transplanted lungs from a brain-dead donor who had recovered from severe acute respiratory syndrome coronavirus 2 into a severe respiratory failure patient supported with extracorporeal membrane oxygenation who needed an emergency transplant. At the 3-month follow-up our patient showed no evidence of COVID-19 transmission or graft dysfunction.
As the coronavirus disease 2019 (COVID-19) pandemic continues, many potential organ donors are at risk of infection.1 In particular lung transplantation faces critical challenges in terms of donor-derived infection and graft dysfunction. Unfortunately it is not possible to wait for an optimal brain-dead donor; patients waiting for lung transplants are at high risk for mortality because of donor shortage. Therefore acceptance of a donor must be carefully determined according to the recipient’s condition. To date 1 case of lung transplantation from a previously COVID-19–infected donor has been reported, but an extracorporeal membrane oxygenation (ECMO) bridge was not used before transplantation.2 We successfully transplanted lungs from a brain-dead donor who had recovered from severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pneumonia into a patient supported with ECMO who required an emergency transplant.
A 56-year-old woman with end-stage pleuroparenchymal fibroelastosis underwent venoarterial ECMO because of consistently high pulmonary hypertension combined with right heart failure (maximal tricuspid regurgitation velocity, 3.7 m/s). She had been on home oxygen therapy for 2 years while waiting for a lung transplant. Fortunately a brain-dead donor was allocated to her on day 2 of ECMO.
The donor was a 66-year-old woman who suffered brain death from a traumatic subarachnoid hemorrhage. Three months previously the donor had been hospitalized with pneumonia, and polymerase chain reaction (PCR) confirmed COVID-19 infection (Figure 1 ). After 10 days of conservative treatment she was PCR-negative and discharged home. One month later the pneumonia had completely resolved and she remained PCR-negative. Two months later she was admitted with a traumatic subarachnoid hemorrhage; a nasopharyngeal swab and bronchoalveolar lavage fluid were PCR-negative for SARS-CoV-2. Liver and lung functions were normal but kidney function was lost, requiring continuous renal replacement therapy. After 6 days she was diagnosed with brain death (she was electroencephalogram-negative), and her organs were donated. Preoperative bronchial washing was negative for bacteria, fungi, and SARS-CoV-2 (by PCR test). No pulmonary infiltrate or any sign of interstitial lung disease was evident on chest computed tomography (CT) (Figures 2A and 2B). The partial pressure of arterial oxygen was 584 mm Hg on 100% oxygen and the positive end-expiratory pressure was 5 cm H2O. The donor lungs met the International Society for Heart and Lung Transplantation COVID-19 guidelines.3 The liver was sent elsewhere for urgent transplantation.
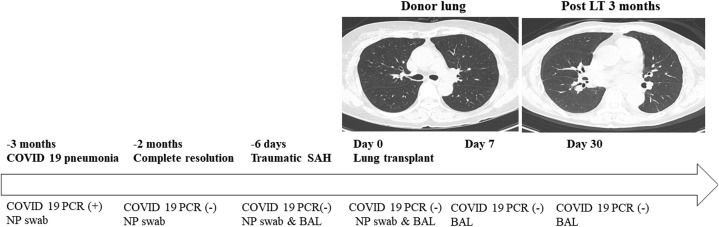
Figure 1.
History of donor lung and transplant results. At the 3-month follow-up our patient showed no evidence of COVID-19 transmission or graft dysfunction. (BAL, bronchoalveolar lavage; COVID-19, coronavirus disease 2019; LT, lung transplantation; NP, nasopharyngeal; PCR, polymerase chain reaction; SAH, subarachnoid hemorrhage.)
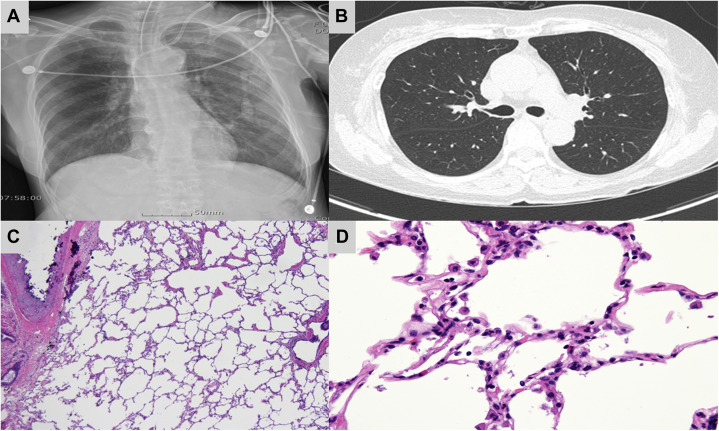
Figure 2.
Imaging of donor lungs. (A) Chest radiograph and (B) chest computed tomography of donor lung before transplantation were normal. (C, D) Histology of the lung biopsy sample was normal (hematoxylin and eosin stain; C, 40×; D, 400×).
Pretransplantation the recipient’s nasopharyngeal swab was PCR-negative for SARS-CoV-2. Bilateral, sequential lung transplantation was performed with an anterolateral thoracotomy under venoarterial ECMO support. Donor lung biopsy samples revealed no sign of COVID-19–induced injury or fibrotic sequelae (Figures 2C and 2D). The lung biopsy sample lacked SARS-CoV-2 RNA, and the viral culture was negative. Standard immunosuppression included basiliximab, tacrolimus, mycophenolate mofetil, and methylprednisolone. The empirical antibiotics were nystatin, sulfamethoxazole-trimethoprim, and voriconazole.
The patient was extubated on postoperative day 3. There were no postoperative complications, and she was discharged on day 44 (Figure 3A). SARS-CoV PCR and viral culture of bronchoalveolar lavage fluid samples collected 7 and 30 days after lung transplantation were negative. Routine chest CT performed on days 7 and 30 showed normal post-transplantation changes without lung injury. On day 90 spirometry and chest CT were both normal (Figure 3B).
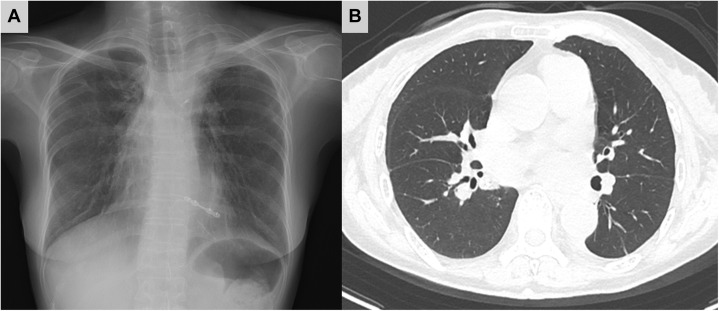
Figure 3.
Imaging after transplant. (A) Chest radiograph at 1 month and (B) chest computed tomography at 3 months showed normal post-transplant changes without fibrosis.
Comment
Although vaccines against COVID-19 are now available, COVID-19 variants are emerging.4 In addition some experts warn that COVID-19 may be like the influenza virus and thus very difficult to eradicate. Therefore an increasing number of donors may be people who have recovered from COVID-19 infection. In patients requiring emergency lung transplantation it is necessary to accept donors with COVID-19 histories after careful evaluation.
First repeated virus PCR tests are required to reduce the risk for donor-derived transmission. To date 1 episode of donor-derived infection has been reported; the donor had not undergone lower respiratory tract testing.1 Because the sensitivity of such a test is higher than that of an upper respiratory tract test, sampling of both the upper and lower respiratory tracts is required. Second donor lung function must be meticulously evaluated. COVID-19 infection can cause acute lung injury, but the long-term lung effects remain unknown.5 Even after the pneumonia resolves alveolar damage, irreversible lung fibrosis, and respiratory dysfunction may remain. Therefore careful CT and blood gas analysis are required. The International Society for Heart and Lung Transplantation states that donor lungs from patients who have recovered from COVID-19 are acceptable if at least 28 days have passed from symptom onset, 2 PCR tests are negative, and no permanent organ damage is detected. In our case the donor had been infected with SARS-CoV-2 3 months before and had recovered after 1 month. SARS-CoV-2 PCR tests of the upper and lower respiratory tracts were repeatedly negative, as was the lung biopsy sample. Thus the risk of donor-derived SARS-CoV-2 transmission was very low.
In conclusion we safely placed lungs from a donor who had recovered from COVID-19 pneumonia in a severe respiratory failure patient supported with ECMO. Before transplantation repeated upper and lower respiratory tract tests were negative for SARS-CoV-2 and chest CT revealed no residual lung injury. The lungs were successfully transplanted; there was no viral transmission or other complication. Although the follow-up period was short, this was the only option to save her life. Further studies are required to determine long-term safety and effectiveness. Acceptance of a donor with a COVID-19 history must depend on the recipient’s condition.
References
- 1.Kaul DR, Valesano AL, Petrie JG, et al. Donor to recipient transmission of SARS-CoV-2 by lung transplantation despite negative donor upper respiratory tract testing. Am J Transplant. 2021;21:2885-2889. [DOI] [PMC free article] [PubMed]
- 2.Ceulemans L.J., Van Slambrouck J., De Leyn P., et al. Successful double-lung transplantation from a donor previously infected with SARS-CoV-2. Lancet Respir Med. 2021;9:315–318. doi: 10.1016/S2213-2600(20)30524-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saima A., Lara D.I., Me-Linh L., et al. Guidance from the International Society of Heart and Lung Transplantation regarding the SARS CoV-2 pandemic. https://ishlt.org/ishlt/media/documents/SARS-CoV-2_Guidance-for-Cardiothoracic-Transplant-and-VAD-center.pdf Available at:
- 4.Krammer F. SARS-CoV-2 vaccines in development. Nature. 2020;586:516–527. doi: 10.1038/s41586-020-2798-3. [DOI] [PubMed] [Google Scholar]
- 5.Richardson S., Hirsch J.S., Narasimhan M., et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323:2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]