Abstract
Objective: This study aimed to explore the impacts of comprehensive care on psychological emotion, postoperative rehabilitation and complications of colorectal cancer patients after colostomy. Methods: From August 2018 to February 2020, a total of sixty colorectal cancer patients undergoing colostomy in our hospital were collected and randomly assigned to a control group to receive conventional care and a research group to receive comprehensive care, with 30 patients in each group. The two groups of patients were compared for postoperative recovery, complications, adverse psychological emotions, self-care ability, quality of life, and nursing satisfaction. Results: The first time of exhaust, food intake and the recovery of bowel sound in the research group were markedly earlier than those in the control group. Besides, the research group had notably lower incidence of postoperative complications, lower self-anxiety scale (SAS) and self-depression scale (SDS) scores at discharge, and higher average self-care ability than the control group, as well as higher quality of life score and nursing satisfaction. Conclusion: Comprehensive care intervention can promote postoperative recovery of colorectal cancer patients after colostomy, relieve their negative emotions, reduce postoperative complications, improve quality of life and nursing satisfaction, which are all important and make this type of care worthy of promotion in clinical practice.
Keywords: Comprehensive nursing, colorectal cancer, colostomy, complication
Introduction
Colorectal cancer is a common malignancy of the gastrointestinal tract, of which the incidence rate is second only to gastric cancer and esophageal cancer, and it has a poor prognosis [1]. With the improvement of people’s living standards and changes in eating habits over the past few years, its incidence is increasing annyally [2]. Despite advances in medical technology and the emergence of many different treatments for colorectal cancer, surgery remains the preferred treatment for patients with colorectal cancer [3]. In radical surgery for colorectal cancer, a permanent colostomy is usually required, which can greatly improve the survival rate of patients [4].
Although colostomy is a mature type of surgery, there is still a high incidence of complications, which not only brings physiological pain to colostomy patients, but also affects their self-efficacy and quality of life [5,6]. Therefore, how to reduce the complications of colostomy and improve the quality of life of colostomy patients through active and effective care intervention is a common concern of colostomy care managers [7]. A study [8] found that a good position of the stoma is the key to reducing related complications and improving patients’ self-care ability and quality of life. However, there is no clear recommendation in medical and nursing textbooks for the positioning of the stoma currently, and there is a relative lack of preoperative positioning intervention by enterstomal therapists in the clinical setting of major hospitals. Some surgeons in China mostly choose the position of stoma during surgery, resulting in a great deviation between the anatomical position of colostomy and the ideal position [9].
The comprehensive care model is a holistic and comprehensive care model that allows for more comprehensive care based on the characteristics of the disease [10]. Therefore, in our research, the nurses were trained in the positioning of stoma, so that they could position it based on the characteristics of colorectal cancer surgery, thus to provide better reference for the choice of care model for patients undergoing colorectal cancer surgery.
Materials and methods
General data
From August 2018 to February 2020, a total of sixty colorectal cancer patients undergoing colostomy in the general surgery department of The Fourth Hospital of Changsha were recruited as research subjects, including 33 males and 27 females. They were divided into a control group (conventional care) and a research group (comprehensive care), with 30 patients in each group. Patients who underwent colostomy for the first time were included in the study. Patients with severe cardiopulmonary or other severe organ diseases, consciousness disorders, communication disorders, or surgical contraindications were excluded. All patients agreed to participate in the experiment and signed the informed consent form. The experiment was approved by the hospital ethics committee and the experiment complied with the Declaration of Helsinki.
Nursing plan
Patients in the control group were treated with the conventional care model. The nursing staff was not involved in stoma positioning, which was performed intraoperatively by the supervising surgeon according to individual surgical habits and convenience of the surgery. Other specific measures included; regular observation of patients’ conditions and colostomy, adjustment of their dietary structure, and relief of adverse emotions. Patients were given detailed answers to their questions, and postoperative care precautions were given so that they could actively cooperate with the follow-up treatment.
Patients in the research group received a comprehensive care model, and the specific measures were as follow: (1) Positioning of colostomy: the nursing staff cooperated with doctors to locate the position of stoma before surgery, discussed this with the enterstomal therapist, surgeons and patients one day before surgery, they asked about the patients’ opinions on the choice of stoma position, understood patients’ daily living habits to avoid the body parts where they were wearing belts on the principle of not affecting their comfort in regard to clothing. The specific methods were as follows: ① The patient was asked to lie completely flat to expose the abdomen. During the process, the nursing staff told the patient to keep warm and to relax; ② The operator stood on one side of the patient’s stoma to observe the outline of the abdomen, and placed the palms of both hands together at the white line of the patient’s abdomen below the umbilicus. The operator asked the patient to hold his/her head with both hands and gradually raised his/her head, with eyes on the toes. Meanwhile, the operator’s fingers were sliding outward to touch a longitudinally contracted muscle, which was the rectus abdominis muscle. The width of rectus abdominis was measured and marked with an oily pen at the edge of rectus abdominis; ③ The operator selected a sigmoidostomy on the 1/3 rectus abdominis muscle connecting the umbilicus and the left iliac spine, took the edge of rectus abdominis muscle as the boundary, and drew a dot as the mark; ④ The operator asked the patient to sit, stand and squat to carefully observe the outline of the abdomen and to make sure that there was a flat enough area on the abdomen to apply the ostomy bag and that the patient could see the stoma site; ⑤ The stoma chassis model was placed at the marked dot to make sure it was placed flat against the abdomen when the patient was lying down, sitting, standing, or squatting; ⑥ After verifying the correct position, the area was disinfected with iodophor and 75% alcohol. Then, a circle with a diameter of 2 to 3 cm was drawn with oil, and the hollow circle was painted as a solid dot and covered with a 3 M transparent sticker. (2) Close observation of vital signs: after surgery, the nursing staff closely monitored the vital signs of patients, including body temperature, respiration, blood pressure, pulse, etc., and notified the doctor in time if there was any abnormality. (3) Psychological nursing intervention: anxiety, depression and other negative emotions often occurred after colostomy. The nursing staff was required to learn to communicate with patients patiently, encourage patients to express their feelings and listen to them patiently. It was also necessary to educate patients about colostomy knowledge. The nursing staff chose appropriate ways to publicize this according to their knowledge and cultural levels, focused on the important principles, to expect the effects and possible adverse reactions of surgical treatment, explained the processes and functions of colostomy nursing, and helped patients relieve their negative emotions and build up their confidence. (4) Instruction of correct nursing methods: the nursing staff explained the use, replacement and observation methods of the ostomy bag, and informed the patients and their families to observe whether there was edema, ischemic necrosis and the corresponding treatment measures at colostomy. (5) Enhancement in patients’ self-care ability: the knowledge explained by nursing staff about the use of the ostomy bag could not only protect patients from infection and peculiar smells, but also increase their self-confidence in life, and reduce their worries about participating in social activities after surgery.
Outcome measures
(1) The recovery of gastrointestinal functions was recorded and compared between the two groups after surgery, including the first time of exhaust, food intake, and recovery of bowel sounds. (2) The self-care ability of both groups of patients was compared. Each item of the scale scored 0 to 5 (with the total score of 50), and the score was directly proportional to the self-care ability. A total score of less or equal to 10 was regarded as severe dependence, a total score of 11-20 as moderate dependence, a total score of 21-49 as mild dependence, and a total score of 50 as no need for dependence. (3) The Visual Analogue Scale (VAS) score [11] of the two groups three days after surgery was compared. (4) The Self-rating Anxiety Scale (SAS) and Self-rating Depression Scale (SDS) [12] were applied to evaluate the negative psychological emotions of patients in both groups after care. (5) The complications in the two groups were recorded and compared, including fecal dermatitis, prolapse, retraction, stenosis, hernia, and surgical incision infection. (6) A self-made knowledge questionnaire was utilized to assess the mastery of colostomy knowledge of both groups of patients, including 5 items of observation and treatment of complications, indications and methods of anal dilatation, daily life management, peripheral skin care, and replacement of ostomy bags. The score ranged from 0 to 100, and the higher the score, the better the condition. (7) The Quality of Life Questionnaire-Core 30 (QLQ-C30) [13] was applied to evaluate the quality of life of patients in both groups before and after care. The scale was divided into 5 items (physical function, role physical, emotional function, social function, cognitive function), with 30 items in total. The score was proportional to the quality of life. (8) Patients’ nursing satisfaction was assessed through a questionnaire survey, which was classified as greatly satisfied, satisfied and dissatisfied.
Statistical methods
Data statistical analysis was conducted with SPSS 20.0 statistical software. Figure illustrations were made using GraphPad 8.0. The measurement data was represented by means ± standard deviation. Comparison between the two groups was conducted by t test. Comparison of counting data adopted Chi-square test. P < 0.05 indicated that the difference was statistically significant.
Results
General data
There was no remarkable difference in gender, age, body mass index (BMI), pathological pattern, pathogenic site, and educational levels between the two groups (P > 0.05), indicating comparability. More details are shown in Table 1.
Table 1.
General data
| Factors | Research group (n=30) | Control group (n=30) | χ2 | P |
|---|---|---|---|---|
| Gender | 0.067 | 0.795 | ||
| Male | 16 (53.33) | 17 (56.67) | ||
| Female | 14 (46.67) | 13 (43.33) | ||
| Age (year) | 0.278 | 0.605 | ||
| ≤ 61 | 13 (43.33) | 15 (50.00) | ||
| > 61 | 17 (56.67) | 15 (50.00) | ||
| BMI (kg/m2) | 0.272 | 0.602 | ||
| ≤ 23 | 18 (60.00) | 16 (53.33) | ||
| > 23 | 12 (40.00) | 14 (46.67) | ||
| Smoking history | 0.067 | 0.795 | ||
| Present | 14 (46.67) | 13 (43.33) | ||
| Absent | 16 (53.33) | 17 (56.67) | ||
| Pathological pattern | 0.067 | 0.795 | ||
| Squamous carcinoma | 17 (56.67) | 16 (53.33) | ||
| Glandular cancer | 13 (43.33) | 14 (46.67) | ||
| Pathogenic site | 0.278 | 0.605 | ||
| Colon cancer | 15 (50.00) | 13 (43.33) | ||
| Rectal cancer | 15 (50.00) | 17 (56.67) | ||
| Educational level | 0.077 | 0.7781 | ||
| Below high school | 20 (66.67) | 21 (70.00) | ||
| High school and above | 10 (33.33) | 9 (30.00) |
Postoperative gastrointestinal function recovery of the two groups
Patients in the research group recovered earlier than those in the control group in terms of the first time of exhaust, the first time of food intake, and the first recovery time of bowel sound, with a statistically significant difference (P < 0.05), as shown in Table 2.
Table 2.
Postoperative gastrointestinal function recovery of the two groups (h)
| Item | Research group (n=30) | Control group (n=30) | t | P |
|---|---|---|---|---|
| First time of exhaust | 42.56 ± 3.41 | 53.71 ± 4.06 | 11.52 | < 0.001 |
| First time of food intake | 8.02 ± 1.03 | 11.13 ± 1.47 | 9.49 | < 0.001 |
| First recovery time of bowel sound | 34.28 ± 3.92 | 40.17 ± 5.42 | 4.82 | < 0.001 |
Comparisons of self-care ability and postoperative VAS scores between the two groups
After care, the self-care ability score and VAS score in the research group were (38.56 ± 2.93) and (1.93 ± 0.41), respectively, and those in the control group were (29.11 ± 2.11) and (2.34 ± 0.41), respectively. The research group exhibited a markedly higher self-care score and a lower VAS score than the control group, with statistical significance (P < 0.05), as shown in Figure 1.
Figure 1.
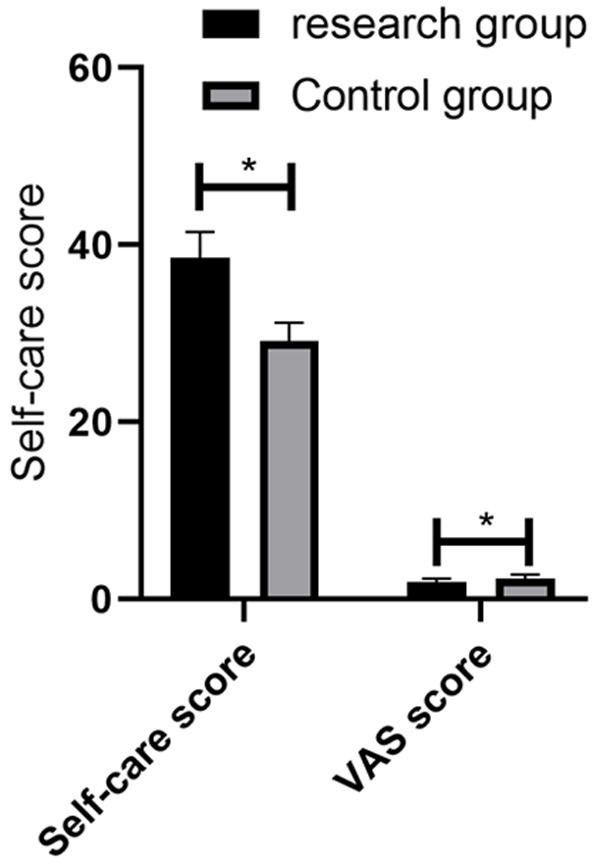
Comparisons of self-care ability and postoperative VAS scores between the two groups. * denotes P < 0.05.
Comparison of incidence of complication between the two groups
Only one patient in the research group developed retraction, with a complication rate of 3.33%. The number of patients in the control group who developed fecal dermatitis, prolapse, retraction, stenosis, hernia, and surgical incision infection were 2, 1, 1, 1, 2, 1, respectively, with a complication rate of 26.67%. The incidence of complications was remarkably lower in the research group than in the control group, with statistical difference (P < 0.05). More details are shown in Table 3.
Table 3.
Comparison of complications
| Complications | Research group (n=30) | Control group (n=30) | X2 | P |
|---|---|---|---|---|
| Fecal dermatitis | 0 (0.93) | 2 (6.67) | - | - |
| Prolapse | 0 (0.93) | 1 (3.33) | - | - |
| Retraction | 1 (3.33) | 1 (3.33) | - | - |
| Stenosis | 0 | 1 (3.33) | - | - |
| Hernia | 0 | 2 (6.67) | - | - |
| Surgical incision infection | 0 | 1 (3.33) | - | - |
| Total incidence | 1 (3.33) | 8 (26.67) | 6.405 | 0.026 |
Comparison of negative emotion score between the two groups
We applied SAS and SDS to evaluate the psychological negative emotions of patients. The results showed no significant difference in SAS and SDS scores between the two groups before care (P > 0.05). After care, the negative emotion scores were markedly improved in both groups compared with those before, and the improvement was more obvious in the research group (P < 0.05). The differences were statistically significant. More details are shown in Figure 2.
Figure 2.
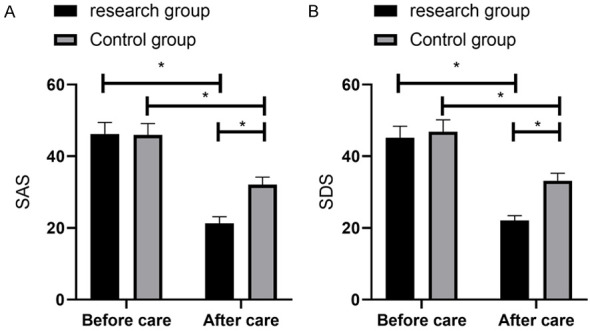
Comparison of negative emotion score between the two groups. A. SAS score of patients in the two groups before and after treatment. B. SDS score of patients in the two groups before and after treatment. * denotes P < 0.05.
Comparison of disease awareness rate between the two groups
The patients in the research group had better knowledge of observation and treatment of complications, indications and methods of anal dilatation, daily life management, peripheral skin care, and replacement of ostomy bags than those in the control group, and the difference was statistically significant (P < 0.05), as shown in Table 4.
Table 4.
Comparison of disease awareness rate between the two groups
| Factors | Research group (n=30) | Control group (n=30) | t | P |
|---|---|---|---|---|
| Observation and treatment of complications | 5.12 ± 0.43 | 3.73 ± 0.21 | 15.91 | < 0.001 |
| Indications and methods of anal dilatation | 4.75 ± 0.22 | 3.35 ± 0.23 | 24.09 | < 0.001 |
| Daily life management | 4.51 ± 0.36 | 4.11 ± 0.17 | 5.50 | < 0.001 |
| Peripheral skin care | 3.84 ± 0.25 | 2.17 ± 0.13 | 32.46 | < 0.001 |
| Replacement of ostomy bag | 4.66 ± 0.23 | 4.14 ± 0.15 | 10.37 | < 0.001 |
Comparison of quality of life between the two groups
Compared with the control group, the quality of life scores in the research group were considerably higher in all dimensions of physical function, role physical, emotional function, social function, and cognitive function after care, and the difference was statistically significant (P < 0.05), as shown in Table 5.
Table 5.
Comparison of quality of life between the two groups
| Factors | Research group (n=30) | Control group (n=30) | t | P |
|---|---|---|---|---|
| Physical function | 91.16 ± 4.32 | 82.15 ± 4.04 | 8.34 | < 0.001 |
| Role physical | 83.25 ± 3.14 | 71.37 ± 2.62 | 15.91 | < 0.001 |
| Emotional function | 84.21 ± 3.67 | 71.23 ± 2.85 | 15.30 | < 0.001 |
| Cognitive function | 91.97 ± 4.31 | 83.22 ± 2.71 | 9.41 | < 0.001 |
| Social function | 63.52 ± 2.11 | 52.57 ± 2.85 | 16.91 | < 0.001 |
Comparison of nursing satisfaction between the two groups
The number of patients in the research group who were greatly satisfied, satisfied and dissatisfied with the care were 24, 5 and 1, respectively, with the nursing satisfaction rate of 98.15%. While the number of patients in the control group who were greatly satisfied, satisfied and dissatisfied with the care were 14, 7 and 9, respectively, with the nursing satisfaction rate of 77.45%. The satisfaction degree in the research group was considerably higher than that in the control group, and the difference was statistically significant (P < 0.05), as shown in Table 6.
Table 6.
Comparison of nursing satisfaction between the two groups [n (%)]
| Group | Research group (n=30) | Control group (n=30) | X2 | P |
|---|---|---|---|---|
| Greatly satisfied | 24 (80.00) | 14 (46.67) | - | - |
| Satisfied | 5 (16.67) | 7 (23.33) | - | - |
| Dissatisfied | 1 (3.33) | 9 (30.00) | - | - |
| Nursing satisfaction | 29 (96.67) | 21 (70.00) | 7.680 | 0.006 |
Discussion
Colorectal cancer, as a malignant tumor with high incidence and lethality, is still treated with radical colon cancer surgery as the preferred treatment option. Despite its good efficacy, the colostomy population is unable to defecate on their own like normal people, which leads to a certain risk of complications and may also produce a series of negative psychological emotions, which is detrimental to the prognosis of patients [14,15]. Therefore, it is necessary to provide appropriate care interventions for these patients to improve their awareness of the disease and treatment motivation, so as to reduce their negative emotions and complications, and improve their quality of life [16,17].
In our research, we analyzed the application effect of a comprehensive care mode in colorectal cancer patients after colostomy. First of all, we recorded and compared the recovery of gastrointestinal functions between the two groups. Patients in the research group experienced earlier first time of exhaust, first time of food intake, and first recovery time of bowel sound than the control group, which suggested that the application of comprehensive care mode could effectively promote the recovery of gastrointestinal functions after surgery. During care, we promoted patients’ blood circulation in the abdominal cavity, improved their blood perfusion and oxygen supply to the abdominal gastrointestinal tract, accelerated their gastrointestinal peristalsis, and facilitated their recovery of gastrointestinal functions by helping them exercise early eating times and shortening their time of eating [18]. Then we compared the postoperative self-care ability, VAS score, and the incidence of complications between the two groups. The results showed notably higher self-care ability and markedly lower VAS scores and incidence of complications in the research group than the control group, indicating that the application of comprehensive care can efficiently improve patients’ self-care ability, alleviate their pain, and reduce the incidence of complications. One of the most important measures in the implementation of our comprehensive care model is the involvement of nursing staff in the preoperative positioning of the enterostomy, that the “doctor, nurse and patient” jointly draw up the position of the stoma, and then jointly go to the patient’s bedside for positioning after the professional enterstomal therapist and surgeons have communicated about the surgical approach and the surgical incision site. A past study [19] pointed out that inviting patients to participate in the positioning of the stoma, informing them about the stoma, respecting their usual habits, and enabling them to see their stoma from different positions can not only effectively avoid the disadvantage of large deviations between the anatomical position of the stoma and the ideal position during intraoperative positioning, but also help reduce postoperative stoma complications and patient self-care. Suggesting that preoperative stoma positioning can reduce stoma complications and improve patients’ quality of life, which is consistent with our observations. In addition, we also provided patients with health information related to colostomy, which also helps patients to improve their self-care skills after surgery.
Then we also analyzed the application effect of comprehensive care model in colorectal cancer patients after colostomy from the aspects of negative emotions, disease awareness rate and postoperative quality of life. The results showed relieved negative emotions of patients in both groups, with more obvious improvement in the research group. Moreover, the disease awareness rate and postoperative quality of life of patients in the research group were significantly superior to those in the control group. Psychological factors are important factors affecting many diseases, especially for colorectal cancer patients after colostomy, who are more likely to have negative psychological emotions due to defecation and other problems, which will further affect their postoperative recovery [20,21]. Comprehensive care measures, however, strengthened the psychological care intervention for patients to eliminate the impact of their negative emotions on postoperative recovery. Moreover, we also provided patients with detailed dietary guidance, so that they consumed more high-protein, high-vitamin, and high-iron foods to ensure adequate nutrition [22]. These above factors have a vital impact on improving the quality of life of patients.
To sum up, comprehensive care intervention can promote postoperative recovery of colorectal cancer patients after colostomy, relieve their negative emotions, reduce postoperative complications, improve quality of life and nursing satisfaction, which is worthy of promotion in clinical practice. However, there are some shortcomings in this study. For example, we did not include more care models for comparison, so whether the comprehensive care model is the most appropriate care model needs to be further demonstrated. Second, due to the insufficient inclusion of number of cases in our study, our conclusions also need to be further demonstrated by expanding the sample size.
Acknowledgements
This study was financially supported by the Hunan Science and Technology Innovation Project (2019JJ80058).
Disclosure of conflict of interest
None.
References
- 1.Takiyama A, Tanaka T, Yamamoto Y, Hata K, Ishihara S, Nozawa H, Kawai K, Kiyomatsu T, Nishikawa T, Otani K, Sasaki K, Watanabe T. Microsatellite status of primary colorectal cancer predicts the incidence of postoperative colorectal neoplasms. Anticancer Res. 2017;37:5785–5790. doi: 10.21873/anticanres.12020. [DOI] [PubMed] [Google Scholar]
- 2.Alagaratnam S, Loizidou M, Yang SY, Fuller B, Ramesh B. Increased expression of IGF-1Ec with increasing colonic polyp dysplasia and colorectal cancer. J Cancer Res Clin Oncol. 2020;146:2861–2870. doi: 10.1007/s00432-020-03345-0. [DOI] [PubMed] [Google Scholar]
- 3.Dai W, Feng H, Lee D. MCCC2 overexpression predicts poorer prognosis and promotes cell proliferation in colorectal cancer. Exp Mol Pathol. 2020;115:104428. doi: 10.1016/j.yexmp.2020.104428. [DOI] [PubMed] [Google Scholar]
- 4.Silva KA, Duarte AX, Cruz AR, de Araujo LB, Pena GDG. Time after ostomy surgery and type of treatment are associated with quality of life changes in colorectal cancer patients with colostomy. PLoS One. 2020;15:e0239201. doi: 10.1371/journal.pone.0239201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Su H, Bao MDL, Wang P, Wang XW, Nie HX, Yun H, Liang JW, Liu Q, Wang XS, Zhou ZX, Zhou HT. Clinical application of enterostomy using running suture of dermis and seromuscular layer in laparoscopic-assisted radical resection for rectal carcinoma. Zhonghua Zhong Liu Za Zhi. 2019;41:553–557. doi: 10.3760/cma.j.issn.0253-3766.2019.07.014. [DOI] [PubMed] [Google Scholar]
- 6.Ling JY, Li YY, Zhong LX, Li WW, Liu H, Cai Y, Hu HB, Zhang JW, Deng YH. Effect of enterostomy on analgesic pattern in patients with advanced digestive tract cancer. Zhonghua Wei Chang Wai Ke Za Zhi. 2019;22:1159–1164. doi: 10.3760/cma.j.issn.1671-0274.2019.12.011. [DOI] [PubMed] [Google Scholar]
- 7.Xian H, Zhang Y, Yang Y, Zhang X, Wang X. A descriptive, cross-sectional study among Chinese patients to identify factors that affect psychosocial adjustment to an enterostomy. Ostomy Wound Manage. 2018;64:8–17. [PubMed] [Google Scholar]
- 8.Liu Y, Li DC, Feng HY, Zhu Y, Liu LY. Effects of enterostomy in treating locally advanced rectal cancer with combined chemoradiotherapy and operation. Zhonghua Wai Ke Za Zhi. 2007;45:455–458. [PubMed] [Google Scholar]
- 9.Maeda C, Hidaka E, Shimada M, Shimada S, Nakahara K, Takayanagi D, Takehara Y, Mukai S, Sawada N, Ishida F, Kudo SE. Transverse colon cancer occurring at a colostomy site 35 years after colostomy: a case report. World J Surg Oncol. 2015;13:171. doi: 10.1186/s12957-015-0593-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hopman P, de Bruin SR, Forjaz MJ, Rodriguez-Blazquez C, Tonnara G, Lemmens LC, Onder G, Baan CA, Rijken M. Effectiveness of comprehensive care programs for patients with multiple chronic conditions or frailty: a systematic literature review. Health Policy. 2016;120:818–832. doi: 10.1016/j.healthpol.2016.04.002. [DOI] [PubMed] [Google Scholar]
- 11.Sutton RM, McDonald EL, Shakked RJ, Fuchs D, Raikin SM. Determination of minimum clinically important difference (MCID) in visual analog scale (VAS) pain and foot and ankle ability measure (FAAM) scores after hallux valgus surgery. Foot Ankle Int. 2019;40:687–693. doi: 10.1177/1071100719834539. [DOI] [PubMed] [Google Scholar]
- 12.Yue T, Li Q, Wang R, Liu Z, Guo M, Bai F, Zhang Z, Wang W, Cheng Y, Wang H. Comparison of hospital anxiety and depression scale (HADS) and zung self-rating anxiety/depression scale (SAS/SDS) in evaluating anxiety and depression in patients with psoriatic arthritis. Dermatology. 2020;236:170–178. doi: 10.1159/000498848. [DOI] [PubMed] [Google Scholar]
- 13.Davda J, Kibet H, Achieng E, Atundo L, Komen T. Assessing the acceptability, reliability, and validity of the EORTC Quality of Life Questionnaire (QLQ-C30) in Kenyan cancer patients: a cross-sectional study. J Patient Rep Outcomes. 2021;5:4. doi: 10.1186/s41687-020-00275-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang J, Ren LJ, Chen XL, Ma L, Chen BJ, Ran SJ, Lu S. Quick rehabilitation nursing improves the recovery of colon cancer patients after laparoscopy. J Biol Regul Homeost Agents. 2017;31:1073–1079. [PubMed] [Google Scholar]
- 15.Hu M, Yu Y, Wu Z, Jin Y, Luo J. The clinical study of fast-track rehabilitation nursing in the perioperative period of therapeutic laparoscopy of colon cancer patients. J Pak Med Assoc. 2020;70:24–30. [PubMed] [Google Scholar]
- 16.Finlayson E, Zhao S, Boscardin WJ, Fries BE, Landefeld CS, Dudley RA. Functional status after colon cancer surgery in elderly nursing home residents. J Am Geriatr Soc. 2012;60:967–973. doi: 10.1111/j.1532-5415.2012.03915.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vendler MMI, Haidari TA, Waage JE, Kleif J, Kristensen B, Gögenur I, Bertelsen CA Copenhagen complete Mesocolic Excision Study group (COMES) Incidence of venous thromboembolic events in enhanced recovery after surgery for colon cancer: a retrospective, population-based cohort study. Colorectal Dis. 2017;19:O393–O401. doi: 10.1111/codi.13910. [DOI] [PubMed] [Google Scholar]
- 18.Parsons HM, Tuttle TM, Kuntz KM, Begun JW, McGovern PM, Virnig BA. Quality of care along the cancer continuum: does receiving adequate lymph node evaluation for colon cancer lead to comprehensive postsurgical care? J Am Coll Surg. 2012;215:400–411. doi: 10.1016/j.jamcollsurg.2012.05.014. [DOI] [PubMed] [Google Scholar]
- 19.Hussain T, Chang HY, Luu NP, Pollack CE. The value of continuity between primary care and surgical care in colon cancer. PLoS One. 2016;11:e0155789. doi: 10.1371/journal.pone.0155789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Castells A, Bessa X, Daniels M, Ascaso C, Lacy AM, Garcia-Valdecasas JC, Gargallo L, Novell F, Astudillo E, Filella X, Pique JM. Value of postoperative surveillance after radical surgery for colorectal cancer: results of a cohort study. Dis Colon Rectum. 1998;41:714–723. doi: 10.1007/BF02236257. discussion 723-714. [DOI] [PubMed] [Google Scholar]
- 21.Duineveld LAM, Molthof H, Wieldraaijer T, van de Ven AWH, Busschers WB, van Weert H, Wind J. General practitioners’ involvement during survivorship care of colon cancer in the Netherlands: primary health care utilization during survivorship care of colon cancer, a prospective multicentre cohort study. Fam Pract. 2019;36:765–770. doi: 10.1093/fampra/cmz028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dixit N, Burke N, Rodriguez G, Sarkar U, Cicerelli B, DeVore JD, Napoles AM. Knowledge and self-efficacy for caring for breast and colon cancer survivors among safety net primary care providers. Support Care Cancer. 2020;28:4923–4931. doi: 10.1007/s00520-019-05277-z. [DOI] [PMC free article] [PubMed] [Google Scholar]


