Abstract
Objective: This study aimed to explore the influence of predictive nursing on the emotions and self-management abilities of post-colostomy rectal cancer patients. Methods: From March 2017 to October 2019, 130 patients with rectal cancer were recruited as the study cohort and placed into a predictive group (the PG) (n=80) that underwent predictive nursing or a normal group (the NG) (n=50) that underwent routine nursing. After the intervention, the operative indications, self-care abilities, nutritional indicators, mental health, postoperative recovery, complications, and nursing satisfaction of the two groups were compared. Results: After the intervention, compared with the NG, the average blood loss, operation times, gastrointestinal tract recovery times and durations of the hospital stays in the PG were shorter, and the self-care ability scores were higher, the nutritional conditions, namely the albumin (ALB), transferrin (TRF), and prealbumin (PAB) levels, were higher, the mental health, namely the self-rating anxiety scale (SAS) and self-rating depression scale (SDS) scores, was better, the total effective rate of the postoperative recovery and the nursing satisfaction were higher, and the incidence of complications was lower. Conclusion: predictive nursing can improve the moods and self-management abilities of post-colostomy rectal cancer patients.
Keywords: Predictive nursing, rectal cancer, postoperative colostomy, self-management abilities
Introduction
Colorectal cancer is the third most frequently diagnosed cancer among men and women all over the world, and it is the fourth largest cause of cancer death, of which rectal cancer accounts for about 30%. Moreover, the clinical results are generally poor [1]. Rectal cancer refers to a malignancy occurring within 15 cm of the anal margin and is generally considered a unique mass. Because of its invasive growth mode, the surgical methods and treatment results have evident uniqueness. Heredity, age, obesity, smoking, and diet are indicators related to rectal cancer [2,3]. Radiation therapy and chemotherapy can reduce large tumors, so they play an indispensable role in the treatment of rectal cancer. However, chemotherapy and radiotherapy have many side effects, such as related toxic reactions, which will affect the patients’ quality of life [4]. In the past 20 years, with the progress in medical technology, the treatment methods have also improved, and the recovery and survival effects of rectal cancer patients after treatment have also been improved [5]. A series of postoperative measures, including postoperative colostomy, are particularly important for the recovery of rectal cancer patients.
In recent years, the frequency of conventional colostomy in rectal cancer resection has increased [6]. Many studies have shown that, compared with the patients without colostomies, the patients who underwent a colostomy have lower anastomotic leakage and a lower risk of reoperation. But correspondingly, the postoperative complications will increase evidently [7,8]. Therefore, the selection of the nursing measures before and after the operation is very important. Predictive nursing is a better choice. Guided by a new medical model, this nursing mode summarizes the characteristics of different diseases and patients’ behaviors. In the postoperative care of cancer, it can minimize all kinds of adverse factors derived from the tumors and the treatment and can improve the patient satisfaction [9-11]. Although there are many studies on predictive nursing in various cancers, there are few studies on its effect after rectal cancer operations, especially its influence on postoperative colostomy patients. Therefore, this study aimed to explore the influence of predictive nursing on the emotions and self-management abilities of post-colostomy rectal cancer patients.
Methods
General information
From March 2017 to October 2019, 130 patients with rectal cancer were recruited as the study cohort and placed in a predictive group (the PG) (n=80) that underwent predictive nursing or the normal group (the NG) (n=50) that underwent routine nursing. Inclusion criteria: patients who were diagnosed with colon cancer, patients who underwent a radical resection of rectal cancer and who received an artificial colostomy, patients without any secondary diseases that would affect this study, patients who could express their feelings normally and had normal mental states. Exclusion criteria: patients with an expected survival period less than 6 months, patients with other diseases that will affect this study, and patients with communication problems. The family members have the relevant agreements. This research was approved by the Ethics Committee.
Methods
The NG underwent routine nursing. After the patients were diagnosed, the medical staff evaluated the patients’ conditions promptly. Before the operations, the patients were educated about intestinal cancer surgery and informed of the key points of artificial colostomy nursing, the key points of ostomy bag replacement, and the related complications of colostomy. Positive psychological counseling was carried out for the patients to pacify their moods, and the family members of the patients were informed of the key points of family nursing.
The PG underwent predictive nursing in addition to the nursing the NG underwent. Active physical examinations were conducted on the patients after their hospitalization. Before the operations, the patients and their families were educated about intestinal cancer, such as knowledge about colostomies and radical resections of rectal cancer, and they were given an introduction to the various colostomy methods. In the process of nursing, the changes in the patients’ psychological states were determined, and the nursing staff actively communicated with the patients in order to eliminate their anxiety, depression, and other emotions caused by the disease and their surgeries. At the same time, the medical staff should encourage the patients to communicate with other patients who had undergone the same surgery. Before the operations, the multimedia mode was used to explain the key points of stoma care and self-care to be carried out after the operations, such as the diet indexes, bathing modes, and exercise modes. The stomas were cleaned, and the patients were trained to defecate and demonstrate actively, so that they could master certain self-care abilities. The medical staff distributed brochures to teach the patients how to replace their ostomy bags correctly, explained the discharge methods of gas and feces, and informed the patients of the characteristics of the postoperative complications and related treatment methods. During the nursing care, the medical staff paid attention in order to observe the patients’ colostomies of patients, selected suitable ostomy bags for them, and explained the proper preservation methods for ostomy bags. At the same time, in terms of the dietary indicators, the medical staff taught the patients to follow correct dietary habits, instructed them to eat regular meals, mainly light meals, with less oil and fewer fat foods, to avoid spicy food, and they ensured that the patients defecate promptly. The principle of clothing selection in the patients’ daily lives was also explained, and attention was paid to the protection of ostomy bags during bathing and daily activities.
Outcome measures
Surgical indications
The surgical indications of the two groups were observed and compared. The indexes examined included intraoperative blood loss, the getting out of bed times, the gastrointestinal tract recovery times, and hospital stay durations.
Self-care ability scores
The patients’ self-care abilities were evaluated using a self-made questionnaire. The indicators we examined included stoma care, stick to the right, and master of disease-related knowledge. The one-hundred percentage point system was applied, and higher score indicated better self-care abilities.
Nutritional indicators
Seven days after the operations, the two groups’ nutritional indexes were compared. The indexes included serum albumin (ALB), transferrin (TRF), and prealbumin (PAB).
Mental health
Self-rating anxiety scale (SAS) [12] and the self-rating depression scale (SDS) [13] were used to evaluate the patients’ mental health in the two groups before and at one month after the nursing. The one-hundred percentage point system was applied in the two scales, and higher scores indicated worse mental health conditions in the patients.
Postoperative recovery
The postoperative recoveries of the two groups were observed. The standards were as follows: 1) Markedly effective: After operation, the patient’s bodily health is normal, all the vital signs are stable, there are no signs of complications, and the stoma is in good condition; 2) Effective: The patients have a better degree of disease recovery and better wound healing. 3) General: The patients still need to be hospitalized for observation. Total effective rate = markedly effective rate+effective rate.
Incidence of complications
The incidence of complications was observed. The indicators included urinary retention, intestinal obstructions, incision infections, artificial pneumoperitoneum, anastomotic leakage, and bleeding.
Treatment satisfaction
A treatment satisfaction questionnaire was used to test the patients’ satisfaction with the treatment, and then the two groups’ treatment satisfaction scores were compared. The test contents and evaluation criteria were developed in house. The total possible score was 100 points, of which 100-85 points were rated as satisfactory, above 70 but below 85 points as basically satisfactory, and below 70 points as unsatisfactory.
Statistical methods
SPSS 25.0 (Asia Analytics Formerly SPSS China) was used for the comprehensive data statistical analysis and figure creation. The count data were tested using X2 tests, and the measurement data were expressed using (Mean ± SD). The two groups at the two time points were analyzed using t tests and multiple time points using a two-factor variance. When P < 0.05, a difference was considered to be significant.
Results
General information
There were no significant differences in the general data such as gender, age, BMI, residence, smoking, or drinking history between the two groups (P > 0.05) (Table 1).
Table 1.
The general patient data
| Classification | PG (n=80) | NG (n=50) | t/X2 | P |
|---|---|---|---|---|
| Gender | 0.12 | 0.729 | ||
| Male | 52 (65.00) | 31 (62.00) | ||
| Female | 28 (35.00) | 19 (38.00) | ||
| Age (years) | 55.78±4.61 | 55.27±5.02 | 0.59 | 0.554 |
| BMI (kg/m2) | 26.92±3.67 | 27.16±3.23 | 0.38 | 0.705 |
| Residence | 0.11 | 0.739 | ||
| Rural | 36 (45.00) | 24 (48.00) | ||
| Urban | 44 (55.00) | 26 (52.00) | ||
| Smoking history | 0.09 | 0.765 | ||
| Yes | 54 (67.50) | 35 (70.00) | ||
| No | 26 (32.50) | 15 (30.00) | ||
| Drinking history | 0.05 | 0.818 | ||
| Yes | 61 (76.25) | 39 (78.00) | ||
| No | 19 (23.75) | 11 (22.00) | ||
| High blood lipid | 0.02 | 0.875 | ||
| Yes | 68 (85.00) | 43 (86.00) | ||
| No | 12 (15.00) | 7 (14.00) | ||
| Hypertension | 0.07 | 0.796 | ||
| Yes | 67 (83.75) | 41 (82.00) | ||
| No | 13 (16.25) | 9 (18.00) |
The surgical indicators in the PG were better than they were in the NG
All the surgical indicators were compared. The intraoperative blood loss, the getting out of bed times, the gastrointestinal tract recovery times, and the hospital stay durations in the PG were shorter than they were in the NG (P < 0.05) (Figure 1). This showed that, compared with the NG, the PG had a better surgical effect.
Figure 1.
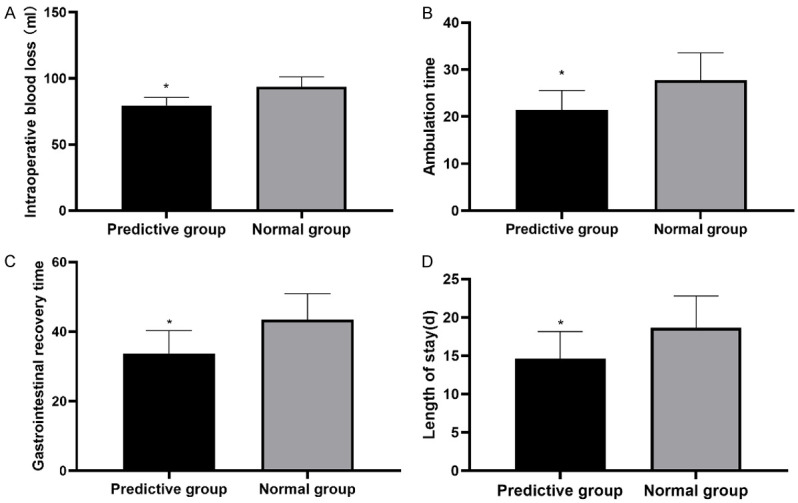
The operative indications of the two groups of patients. A. Intraoperative blood loss: the intraoperative blood loss in the PG was less than it was in the NG (P < 0.05); B. The getting out of bed times: the getting out of bed times in the PG were shorter than they were in the NG (P < 0.05); C. Gastrointestinal tract recovery times: the gastrointestinal tract recovery times of the patients in the PG were shorter than they were in the NG (P < 0.05); D. Lengths of stay: the durations of the hospital stay of the patients in the PG were shorter than they were in the NG (P < 0.05). Note: *means compared with the NG, P < 0.05.
The self-management ability scores in the PG were better than they were in the NG
The self-care ability scores were compared. The stoma care, stick to the right diet, active medication, and master of disease-related knowledge scores in the PG were all higher than they were in the NG (P < 0.05) (Figure 2). After the nursing intervention, the PG patients’ self-management abilities recovered better.
Figure 2.
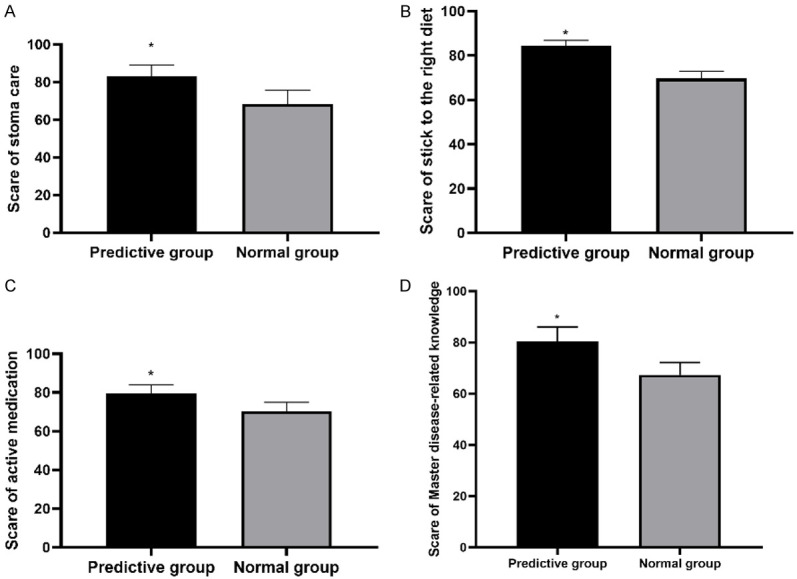
The cores of self-care ability scores of the patients in the two groups. A. Stoma care: the intraoperative stoma care scores in the PG were higher than they were in the NG (P < 0.05); B. Stick to the right diet: The stick to the right diet scores in the PG were higher than they were in the NG (P < 0.05); C. Active medication: The patients in the PG scored higher than the patients in the NG (P < 0.05); D. Master of disease-related knowledge: the master disease-related knowledge scores in the PG were higher than they were in the NG (P < 0.05). Note: *means compared with the NG, P < 0.05.
The nutritional status of the PG was better than of the nutritional status in the NG
The nutritional indexes of the two groups were compared. The ALB, TRF, and PAB levels in the PG were higher than they were in the NG (P < 0.05) (Figure 3). This showed that predictive nursing can better restore patients’ nutritional conditions.
Figure 3.
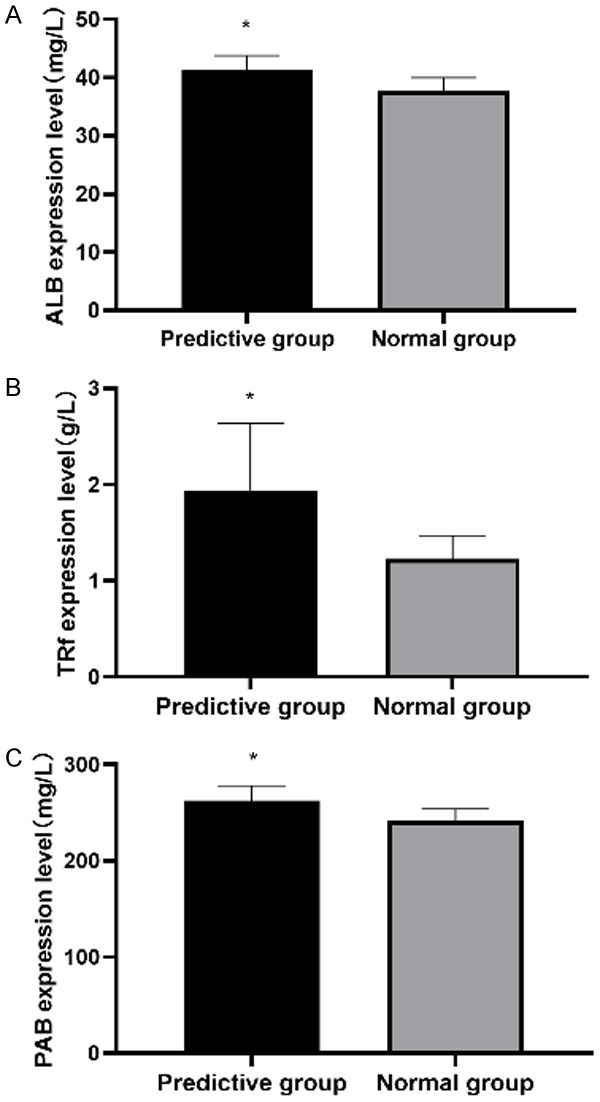
The expression levels of the patients’ nutritional indicators in two groups. A. ALB expression level: The ALB in the PG was higher than it was in the NG (P < 0.05); B. TRF expression level: The TRF levels in the PG were higher than they were in the NG (P < 0.05); C. The PAB expression levels: The PAB levels in the PG were higher than they were in the NG (P < 0.05). Note: *means compared with the preoperative value, P < 0.05.
The mental health scores in the PG were lower than they were in the NG
The two groups’ SAS and SDS scores were compared. The SAS and SDS scores in both groups were decreased at one month after the nursing, and the patients’ scores in the PG were lower than they were in the NG (P < 0.05) (Figure 4). This indicated that predictive nursing can better maintain patients’ mental health levels.
Figure 4.
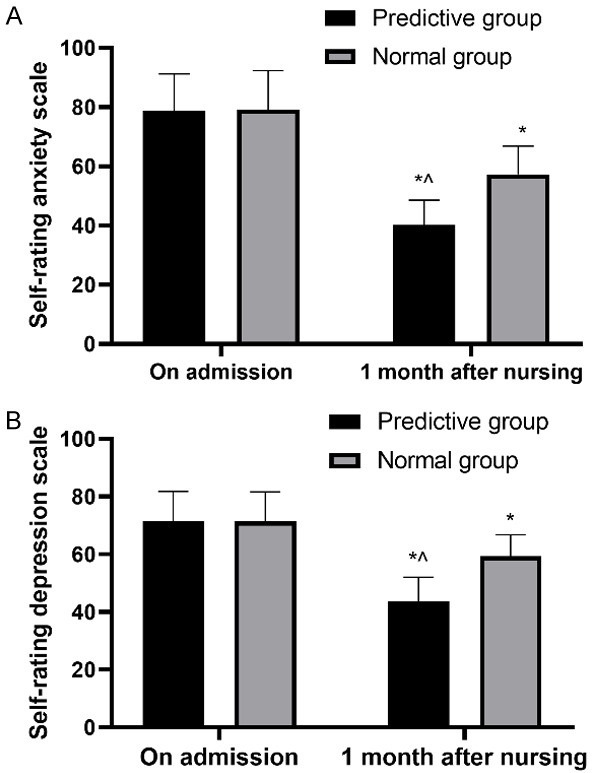
The patients’ mental health in two groups. A. SAS: the scores ion both groups were decreased after one month of admission, and the SAS scores of the patients in the PG were lower than they were in the NG (P < 0.05); B. SDS: both groups’ scores decreased at one month after admission, and the SDS scores of the patients in the PG were lower than the scores in the NG (P < 0.05). Note: *means compared with admission, P < 0.05; ^means compared with the NG, P < 0.05.
The total effective rate in the PG was higher than it was in the NG
Comparing the postoperative recovery between the two groups, the patients’ total effective rate in the PG was higher than the total effective rate in the NG (P < 0.05) (Table 2). The total effective rate in the PG was higher, which indicated that the postoperative recovery in the PG was better than it was in the NG.
Table 2.
The total effective rates
| Classification | PG (n=80) | NG (n=50) | X2 | P |
|---|---|---|---|---|
| Markedly effective | 58 (72.50) | 29 (58.00) | - | - |
| Effective | 18 (22.50) | 11 (22.00) | - | - |
| General | 4 (5.00) | 10 (20.00) | - | - |
| Total effective rate (%) | 76 (95.00) | 40 (80.00) | 7.20 | 0.007 |
The incidence of complications in the PG was lower than it was in the NG
Comparing the incidences of complications, the incidence of postoperative complications in the PG was lower than it was in the NG (P < 0.05) (Table 3). This showed that predictive nursing can reduce the incidence of complications and make patients safer during their operations.
Table 3.
The incidences of complications
| Classification | PG | NG | X2 | P |
|---|---|---|---|---|
| Urinary retention | 1 (2.00) | 5 (10.00) | ||
| Intestinal obstruction | 1 (2.00) | 5 (10.00) | ||
| Incision infection | 0 (0.00) | 3 (6.00) | ||
| Artificial pneumoperitoneum | 1 (2.00) | 2 (4.00) | ||
| Anastomotic leakage and bleeding | ||||
| Incidence of complications (%) | 3 (6.00) | 15 (30.00) | 9.76 | 0.002 |
The patient satisfaction in the PG was higher than it was in the NG
Comparing the patients’ satisfaction in the two groups, the satisfaction in the PG was higher than the patient satisfaction in the NG (P < 0.05) (Table 4).
Table 4.
The patient satisfaction in the two groups
| Classification | PG (n=80) | NG (n=50) | X2 | P |
|---|---|---|---|---|
| Satisfied | 52 (65.00) | 22 (44.00) | - | - |
| Basically satisfied | 26 (32.50) | 16 (32.00) | - | - |
| Dissatisfied | 2 (2.50) | 12 (24.00) | - | - |
| Satisfaction (%) | 78 (97.50) | 38 (76.00) | 14.80 | < 0.001 |
Discussion
Rectal cancer begins in the rectal tissues, grows slowly into the blood vessels or lymphatic vessels, and finally forms malignant tumors on the rectal wall, which can then easily metastasize [14]. Therefore, for rectal cancer, early detection and early treatment are needed. However, after the treatment, patients’ stomata are easily contaminated, and the incidence of postoperative complications is high, so effective measures are needed to protect the stomata [15,16]. Among many diseases, including rectal cancer, good postoperative stoma and good nursing methods can minimize stomatal complications [17]. Here, we explored the influence of predictive nursing on the emotional and physical recovery of patients who underwent a postoperative stoma.
First, the SAS and SDS scores of the patients in the PG were lower than the corresponding scores in the NG after nursing for one month, indicating that health education and psychological counseling in the PG were effective. The Health education in the PG not only taught the patients about rectal cancer and radical resection of rectal cancer, but it also introduced the patients to stomas and the stoma method, which is more detailed than the health education given in the NG. At the same time, the medical staff in the PG understood the patients’ psychological states and communicated with them frequently. Studies show that more detailed health education gives patients a better chance to restore confidence in cancer treatment [18]. This is similar to the results of this study. Psychological counseling is the main method for relieving patients’ negative emotions. Cancer, especially rectal cancer, will have a great negative impact on patients’ psychology. At the same time, in the nursing process, the problem induced by the ostomy bag can very easily affect the harmonious relationship of the family members. If patients’ confidence is lost and the depressive mood is aggravated, a patient’s condition will further deteriorate [19-21]. Combined with the results of this study, we conclude that psychological counseling and detailed health education can effectively reduce patients’ anxiety and depression.
Health education and psychological counseling can alleviate patients’ anxiety and depression, increase patients’ confidence, and help patients have a better recovery. According to the indications of the operation, the amount of bleeding, the getting out of bed times, the gastrointestinal tract recovery times, and the durations of the hospital stays in the PG were shorter. At the same time, combined with the self-care ability scores, especially the mastering disease-related knowledge scores, the PG had higher scores, indicating that predictive nursing health education and psychological counseling made the patients better understand the operation process and the diseases, and they enhanced their confidence and made the patients form a tacit understanding of the medical care. Therefore, the operation went smoothly, and the patients received better treatment. Rectal cancer is a chronic disease. The treatment will cause a series of side effects such as nausea and vomiting, and a series of complications, thus reducing the patients’ quality of life. Therefore, the patients have the ability to perform self-care, which is conducive to their better recovery from such diseases [22-24]. From this point of view, predictive nursing can improve the patients’ self-care abilities, which makes patients have a better recovery, and this also explains why the incidence of complications in the PG was lower. In addition, predictive nursing has a higher level of nutritional indicators. A nutritional imbalance can easily induce abnormal molecular signal transduction, thus inducing the pathogenesis of rectal cancer [25,26]. Predictive nursing can provide better nutritional support to patients and reduce the causative factors of rectal cancer, so that patients can better fight against such diseases. However, it is a great pity that this study failed to determine some of the related predisposing factors of rectal cancer. In addition, this study failed to determine the cooperation levels in the patients’ treatment and nursing, which is very unfavorable to the improvement of nursing and treatment programs. Therefore, in our future research, we will include the inducing factors in the evaluation indicators, and we will observe and evaluate the nursing statuses of the patients during and after the operations, in order to continuously improve their treatment and nursing.
To sum up, for patients with rectal cancer undergoing a colostomy after their operations, the implementation of predictive nursing can improve the patients’ moods and their self-management abilities, so it is worthy of popularizing clinically.
Acknowledgements
This study was financially supported by Hengyang City Science and Technology Bureau, The Application of Mobile Medical APP in the Health Management of PICC Chemotherapy Patients (S2018G9031021263).
Disclosure of conflict of interest
None.
References
- 1.Dayde D, Tanaka I, Jain R, Tai MC, Taguchi A. Predictive and prognostic molecular biomarkers for response to neoadjuvant chemoradiation in rectal cancer. Int J Mol Sci. 2017;18:573. doi: 10.3390/ijms18030573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Paschke S, Jafarov S, Staib L, Kreuser ED, Maulbecker-Armstrong C, Roitman M, Holm T, Harris CC, Link KH, Kornmann M. Are colon and rectal cancer two different tumor entities? A proposal to abandon the term colorectal cancer. Int J Mol Sci. 2018;19:2577. doi: 10.3390/ijms19092577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Feeney G, Sehgal R, Sheehan M, Hogan A, Regan M, Joyce M, Kerin M. Neoadjuvant radiotherapy for rectal cancer management. World J Gastroenterol. 2019;25:4850–4869. doi: 10.3748/wjg.v25.i33.4850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Couwenberg AM, Burbach JPM, van Grevenstein WMU, Smits AB, Consten ECJ, Schiphorst AHW, Wijffels NAT, Heikens JT, Intven MPW, Verkooijen HM. Effect of neoadjuvant therapy and rectal surgery on health-related quality of life in patients with rectal cancer during the first 2 years after diagnosis. Clin Colorectal Cancer. 2018;17:e499–e512. doi: 10.1016/j.clcc.2018.03.009. [DOI] [PubMed] [Google Scholar]
- 5.Smith JJ, Garcia-Aguilar J. Advances and challenges in treatment of locally advanced rectal cancer. J. Clin. Oncol. 2015;33:1797–1808. doi: 10.1200/JCO.2014.60.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rutegard M, Bostrom P, Haapamaki M, Matthiessen P, Rutegard J. Current use of diverting stoma in anterior resection for cancer: population-based cohort study of total and partial mesorectal excision. Int J Colorectal Dis. 2016;31:579–585. doi: 10.1007/s00384-015-2465-6. [DOI] [PubMed] [Google Scholar]
- 7.Emmanuel A, Chohda E, Lapa C, Miles A, Haji A, Ellul J. Defunctioning stomas result in significantly more short-term complications following low anterior resection for rectal cancer. World J Surg. 2018;42:3755–3764. doi: 10.1007/s00268-018-4672-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ihnat P, Gunkova P, Peteja M, Vavra P, Pelikan A, Zonca P. Diverting ileostomy in laparoscopic rectal cancer surgery: high price of protection. Surg Endosc. 2016;30:4809–4816. doi: 10.1007/s00464-016-4811-3. [DOI] [PubMed] [Google Scholar]
- 9.Reich RR, Lengacher CA, Alinat CB, Kip KE, Paterson C, Ramesar S, Han HS, Ismail-Khan R, Johnson-Mallard V, Moscoso M, Budhrani-Shani P, Shivers S, Cox CE, Goodman M, Park J. Mindfulness-based stress reduction in post-treatment breast cancer patients: immediate and sustained effects across multiple symptom clusters. J Pain Symptom Manage. 2017;53:85–95. doi: 10.1016/j.jpainsymman.2016.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu Q, Zhu H. Application of predictive nursing reduces psychiatric complications in ICU patients after neurosurgery. Iran J Public Health. 2016;45:469–473. [PMC free article] [PubMed] [Google Scholar]
- 11.Yu Y, Hu L, Chen X, Ge M, Zhu H, Yan Y. The impact of the predictive nursing education process on degree of comfort and quality of life for patients in the oncology department. Iran J Public Health. 2017;46:1231–1236. [PMC free article] [PubMed] [Google Scholar]
- 12.Wu JJ, Zhang YX, Du WS, Jiang LD, Jin RF, Yu HY, Liu JM, Han M. Effect of Qigong on self-rating depression and anxiety scale scores of COPD patients: a meta-analysis. Medicine (Baltimore) 2019;98:e15776. doi: 10.1097/MD.0000000000015776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jokelainen J, Timonen M, Keinanen-Kiukaanniemi S, Harkonen P, Jurvelin H, Suija K. Validation of the Zung self-rating depression scale (SDS) in older adults. Scand J Prim Health Care. 2019;37:353–357. doi: 10.1080/02813432.2019.1639923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dekker E, Tanis PJ, Vleugels JLA, Kasi PM, Wallace MB. Colorectal cancer. Lancet. 2019;394:1467–1480. doi: 10.1016/S0140-6736(19)32319-0. [DOI] [PubMed] [Google Scholar]
- 15.Shida D, Tagawa K, Inada K, Nasu K, Seyama Y, Maeshiro T, Miyamoto S, Inoue S, Umekita N. Modified enhanced recovery after surgery (ERAS) protocols for patients with obstructive colorectal cancer. BMC Surg. 2017;17:18. doi: 10.1186/s12893-017-0213-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shang Y, Guo C, Zhang D. Modified enhanced recovery after surgery protocols are beneficial for postoperative recovery for patients undergoing emergency surgery for obstructive colorectal cancer: a propensity score matching analysis. Medicine (Baltimore) 2018;97:e12348. doi: 10.1097/MD.0000000000012348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Steinhagen E, Colwell J, Cannon LM. Intestinal stomas-postoperative stoma care and peristomal skin complications. Clin Colon Rectal Surg. 2017;30:184–192. doi: 10.1055/s-0037-1598159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arnold CL, Rademaker A, Liu D, Davis TC. Changes in colorectal cancer screening knowledge, behavior, beliefs, self-efficacy, and barriers among community health clinic patients after a health literacy intervention. J Community Med Health Educ. 2017;7:497. doi: 10.4172/2161-0711.1000497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kumar V, Kumawat N, Thomas JM, Kumar A, Sharma A, Kamal M. Challenges encountered in placement of ostomy bag for palliative care in a patient with colorectal cancer. Indian J Palliat Care. 2019;25:474–476. doi: 10.4103/IJPC.IJPC_23_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Calderon C, Jimenez-Fonseca P, Jara C, Hernandez R, Martinez de Castro E, Varma S, Ghanem I, Carmona-Bayonas A. Comparison of coping, psychological distress, and level of functioning in patients with gastric and colorectal cancer before adjuvant chemotherapy. J Pain Symptom Manage. 2018;56:399–405. doi: 10.1016/j.jpainsymman.2018.05.010. [DOI] [PubMed] [Google Scholar]
- 21.Vashistha V, Singh B, Kaur S, Prokop LJ, Kaushik D. The effects of exercise on fatigue, quality of life, and psychological function for men with prostate cancer: systematic review and meta-analyses. Eur Urol Focus. 2016;2:284–295. doi: 10.1016/j.euf.2016.02.011. [DOI] [PubMed] [Google Scholar]
- 22.Piamjariyakul U, Williams PD, Prapakorn S, Kim M, Park L, Rojjanasrirat W, Williams AR. Cancer therapy-related symptoms and self-care in Thailand. Eur J Oncol Nurs. 2010;14:387–394. doi: 10.1016/j.ejon.2010.01.018. [DOI] [PubMed] [Google Scholar]
- 23.Gray NM, Hall SJ, Browne S, Macleod U, Mitchell E, Lee AJ, Johnston M, Wyke S, Samuel L, Weller D, Campbell NC. Modifiable and fixed factors predicting quality of life in people with colorectal cancer. Br J Cancer. 2011;104:1697–1703. doi: 10.1038/bjc.2011.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Karimi S, Makhsosi BR, Seyedi-Andi SJ, Behzadi M, Moghofeh Y, Mohammadinasrabadi K, Abdi A, Ahmadi P. Surveying the effect of a self-care education program on severity of nausea and emesis in colorectal cancer patients under chemotherapy. J Multidiscip Healthc. 2017;10:301–307. doi: 10.2147/JMDH.S131111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jiang R, Botma A, Rudolph A, Husing A, Chang-Claude J. Phyto-oestrogens and colorectal cancer risk: a systematic review and dose-response meta-analysis of observational studies. Br J Nutr. 2016;116:2115–2128. doi: 10.1017/S0007114516004360. [DOI] [PubMed] [Google Scholar]
- 26.Zamora-Ros R, Cayssials V, Jenab M, Rothwell JA, Fedirko V, Aleksandrova K, Tjonneland A, Kyro C, Overvad K, Boutron-Ruault MC, Carbonnel F, Mahamat-Saleh Y, Kaaks R, Kuhn T, Boeing H, Trichopoulou A, Valanou E, Vasilopoulou E, Masala G, Pala V, Panico S, Tumino R, Ricceri F, Weiderpass E, Lukic M, Sandanger TM, Lasheras C, Agudo A, Sanchez MJ, Amiano P, Navarro C, Ardanaz E, Sonestedt E, Ohlsson B, Nilsson LM, Rutegard M, Bueno-de-Mesquita B, Peeters PH, Khaw KT, Wareham NJ, Bradbury K, Freisling H, Romieu I, Cross AJ, Vineis P, Scalbert A. Dietary intake of total polyphenol and polyphenol classes and the risk of colorectal cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort. Eur J Epidemiol. 2018;33:1063–1075. doi: 10.1007/s10654-018-0408-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


